Abstract
Purpose of Review
Gallant efforts are ongoing to achieve sustained antiretroviral therapy (ART)–free HIV remission in the HIV-infected person; however, most, if not all, current human clinical studies have primarily focused these efforts on targeting viral persistence in CD4 T cells in blood and tissue sanctuaries. The lack of myeloid centered HIV clinical trials, either as primary or secondary end points, has hindered our understanding of the contribution of myeloid cells in unsuccessful trials but may also guide successes in future HIV eradication clinical strategies.
Recent Findings
Recent advances have highlighted the importance of myeloid reservoirs as sanctuaries of HIV persistence and therefore may partially be responsible for viral recrudescence following ART treatment interruption in several clinical trials where HIV was not detectable or recovered from CD4 T cells. Given these findings, novel innovative therapeutic approaches specifically focused on HIV clearance in myeloid cell populations need to be vigorously pursued if we are to achieve additional cases of sustained ART-free remission.
Summary
This review will highlight new research efforts defining myeloid persistence and recent advances in HIV remission and cure trials that would be relevant in targeting this compartment and make an argument as to their clinical relevancy as we progress towards sustained ART-free HIV remission in all HIV-infected persons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most past and ongoing HIV eradication targeted clinical trials have narrowly focused on evaluating and targeting the long-lived memory CD4+ T cells, as these cellular reservoirs harbor the majority of the cell-associated HIV using current reservoir quantification assays. As treatment interruption of antiretroviral therapy (ART) remains the gold standard in determining the outcome of HIV curative designed clinical trials, the contribution of viral persistence in myeloid cells, such as blood monocytes and tissue macrophages, has not been at the forefront. This partly stems from the debate in the field on the scope of myeloid cells as viral reservoirs or contributors to viral persistence. However, recent studies now provide compelling evidence that blood monocytes and tissue macrophages in the lung [1, 2], adipose tissue [3], gut-associated lymphoid tissue (GALT) [4, 5], genital tract [6], semen [7], and bone marrow [8, 9] as well as central nervous system (CNS) cells including both myeloid originating microglia and astrocytes of the brain [10, 11]; all have been shown to harbor HIV in the setting of suppressive ART. Thus, in order to achieve full remission, we need to rethink the design and implementation of HIV cure-focused trials for elimination of all cellular reservoirs.
Two prominent cases that may shed light on the importance of myeloid cells as viral reservoirs in cure studies may be informative in this regard. In the case of the “Berlin Patient” [12], who received a bone marrow transplant and successfully achieved viral remission after stopping ART without subsequent viremic rebound for over a decade now, the exact mechanisms for this successful trial, which to date has not been replicated, remain undefined and speculative. With respect to monocytes and macrophages in this trial, prior administration of gemtuzumab (a myeloid cell depleting anti-CD33 monoclonal antibody) for his acute myeloid leukemia (AML) may have depleted HIV-infected myeloid reservoirs. It is also unclear whether the lack of a myeloid cell-targeted depletion contributed to the incomplete reservoir elimination and viral reemergence in other human [13] and non-human [14] trials that have attempted to recapitulate the case of the Berlin Patient.
In the case of the infamous “Mississippi baby,” and cases of acute and extremely early administration of ART [15,8,17], where a prolonged period of viral control without ART persisted, the viral reservoir monitoring studies were not designed for interrogation of viral persistence within myeloid cells. Interesting to note that in the case of the Mississippi baby following aggressive ART at birth, virus rebounded after 27 months after ART cessation. At 26 months, plasma virus was undetectable (< 2 copies/ml); however, the monocyte threshold for detection of cell-associated virus was higher than for the memory CD4 T cells, so it is unclear if the use of more sensitive assays would have detected any residual virus in the monocytes. Furthermore, lower monocyte counts were assessed as compared to CD4 T cells and viral outgrowth assays were not performed on monocytes. In our ongoing studies where ART was administered early during acute HIV infection [18], we are pursuing sensitive virological studies to better define the contribution of myeloid reservoirs to viral persistence in the earliest stage of infection.
This review will consider the contribution of HIV persistence in myeloid-derived cells in past, ongoing, and future cure clinical trials. Furthermore, we will review the sensitivity of myeloid reservoir measurement methods and argue for inclusion of monitoring myeloid cells harboring HIV as future primary and secondary end points in future HIV cure studies.
Evidence for Myeloid Cells as Contributors of HIV Persistence
Mounting evidence suggests that cells of the macrophage lineage, including blood monocytes subsets, play a significant role in HIV-1 persistence. Monocytes routinely survey tissues by transmigrating across the vascular endothelium from the bloodstream into tissues sites. Their capacity to harbor HIV DNA and RNA makes them suspect as critical contributors to HIV pathogenesis [19•]. Indeed, a variety of attributes make the monocyte and tissue macrophages, including microglia, ideal candidates for contributing to the HIV reservoir, both as carriers and replenishers of the viral reservoir. The macrophage reservoir half-life has historically been underdetermined, yet in the presence of ART, macrophages from SIV-infected rhesus macaques can sustain viremia for several months [20,13,22]. Furthermore, myeloid cells are relatively more resistant to apoptosis induced by HIV infection [23], and virus produced by macrophages may be more infectious than virus originating from CD4+ T cells [24].
The HIV envelope region undergoes more frequent sequence evolution in blood monocytes as compared to that of resting CD4+ T cells, suggesting a distinct contribution to plasma viremia. Indeed, phylogenetic analyses of HIV-1 sequences indicated that after prolonged ART, viral populations are related or identical to those found only in CD14+ monocytes [25]. The non-classical or patrolling monocyte subset (CD14lowCD16high) expresses higher levels of CCR5, a co-receptor for M-tropic HIV strains, and CD4, making them more susceptible to continual viral infection. Circulating blood monocytes traffic into tissues to later differentiate into tissue macrophages, but have the potential to undergo subsequent differentiation into migratory myeloid dendritic cells, which then traffic to other lymph tissues. Monocytes and macrophages disseminate into most tissues of the body and mediate HIV spread, particularly into the central nervous system and lymphoid tissues. Post-mortem brain tissue analysis has revealed that viral DNA is present in 3 to 19% of astrocytes [26] despite astrocyte infection being both relatively infrequent and unproductive [27]. Moreover, our group has used next-generation in situ hybridization RNAScope to identify HIV RNA in cerebellum macrophages of an infected individual who died with a undetectable plasma viral load [28•]. Perivascular macrophages have a half-life of ∼ 3 months [29] while microglia have a half-life of months-years to years-lifetime [30], and parenchymal microglia have been shown to represent two thirds of the infected cells in brain autopsies of HIV-infected persons with encephalitis [31]. Therefore, both CNS perivascular macrophages and microglia need to be considered as possible long-lived HIV reservoirs.
The extent of monocyte and macrophage tissue reservoir compartments contributing to viral recrudescence is poorly understood. Compared to the vast majority of studies tailored to evaluate the viral reservoir in the CD4 T cell compartment, few studies focus their effort to elucidate the relationship of monocyte/macrophages to HIV reservoir and its persistence. In humanized myeloid-only mice (MoM) infected with HIV, it has been shown that after ART-interruption, one of three mice experienced a delayed viral rebound [19•]. Due to the absence of human T cells in MoM mice, this study showed for the first time, in vivo, that persistent HIV infection exists in tissue macrophages during ART and the myeloid compartment can contribute to viral rebound after treatment interruption. Although investigators reported not being able to detect HIV DNA or viral outgrowth in peripheral monocytes isolated from viremic and ART-suppressed patients [19•, 32•], others have reported detection of HIV in circulating monocyte populations. CD16+ monocytes isolated from the blood of ART-treated individuals have been shown to harbor HIV DNA [33, 34]. In non-human primate studies, SIV was quantifiable in monocytes and macrophages from blood and tissues using a modified quantitative viral outgrowth assay (QVOA). The macrophage-QVOA (Mϕ-QVOA) is specifically tailored to quantify productively infected myeloid cells [35•]. The evidence in these reports stresses a need for HIV curative studies to include a more comprehensive evaluation of HIV persistence in the myeloid compartment in both blood and tissue. In doing this will we begin to fully understand the extent of the viral reservoir and the dynamics of its’ persistence, as well as to ascertain failures in past and current cure studies, which may better inform future curative endeavors (Fig. 1).
Biomarkers and Advances in Quantifying HIV Reservoirs in Myeloid Cells
CD4 T cells have been at the center of understanding HIV persistence dynamics and defining the latent reservoir. However, studies have utilized various HIV persistence and reservoir measurement techniques in characterizing these aspects in the myeloid compartment (Table 1). While there is evidence of HIV persistence in forms of proviral DNA in myeloid cells, measurement of replication-competent proviruses that produce infectious virions during ART-suppression is what will define the myeloid compartment as a reservoir. It is the existence of the latter that results in viral rebound after ART interruption and is a major barrier to curing HIV infection [39, 40]. The QVOA remains the gold standard for quantifying the latent reservoir, and its development was critical in defining resting CD4 T cells as latent reservoirs [39]. Overtime, modifications of the QVOA have been implemented to improve and streamline different steps of the assay. However, the majority of modifications done on the QVOA remained to be T cell centric [41,32,43, 44, 45•, 46, 47, 48•, 49, 50]. Clement et al. have modified the QVOA and tailored the assay to measure the viral reservoir size in monocytes and macrophages, addressing the need to evaluate the potential viral reservoir in myeloid cells [35•]. The Mϕ-QVOA assessed enriched myeloid cells that undergo cellular stimulation with TNF-α, a potent activator of myeloid cells and the U1 HIV latently infected monocytic cell line [51, 52]. Using the Mϕ-QVOA technique, macrophages were not only found to be productively infected in the SIV-infected non-human primate model, but also the number of productively infected macrophages varied throughout different tissue sites. Moreover, despite viral suppression by ART, tissue macrophages isolated from SIV-infected macaques continued to be productively infected [38•].
With the ongoing use of these techniques in myeloid cells, it is of great value to evaluate potential biomarkers of viral persistence and reservoir in this cellular compartment. Much of the biomarkers currently proposed, such as CD2, CD30, CD32, and immune checkpoint receptors TIGIT, PD-1, and LAG-3, are still being investigated, but CD4 T cells were the focused cell type of these discoveries [53,42,43,56, 57•, 58]. The utility of these biomarkers as it directly relates to viral persistence and reservoir in myeloid cells has not been vigorously pursued, although much of the markers are T cell specific and highlight a need to further investigate myeloid-specific candidates. CD16, a Fcγ receptor, expression on myeloid cells has been found to be enriched for HIV DNA [33, 34]. In addition, higher expression of CCR2 on CD14+CD16+ monocytes isolated for ART-suppressed patients correlated with higher HIV DNA levels in peripheral blood mononuclear cells (PBMC) [59•].
Consideration of Myeloid Cells in HIV Cure Trials
Latency Reactivation Agents
The “shock and kill” strategy is currently one of the most widely discussed approaches to eliminate the viral reservoir [60, 61]. In this approach, drugs are administered to reverse HIV latency and induce viral production, ultimately resulting in the death of infected cells by direct viral cytopathic effects or immune-mediated clearance. Latency reversing agents (LRAs) are administered during suppressive ART, thereby preventing reactivated virus from replenishing the reservoir through infection of new cells. Clinical trials involving LRAs such as romidepsin, vorinostat, disulfiram, and panobinostat have failed to demonstrate significant reduction in reservoir size, although transient elevation in plasma viral RNA has been observed [62,51,64, 65•, 66, 67]. Numerous LRAs have been shown in vitro to have implications for driving HIV transcription in myeloid-derived cells, yet primary outcomes of completed clinical trials have thus far been entirely T cell focused, leaving our knowledge of myeloid-driven viral control to be underdeveloped. Below are some LRAs that may have relevance in driving viral transcription in myeloid cells.
Numerous clinical trials have used histone deacetylase inhibitors (HDACi) to reactivate HIV transcription, these include the following: panobinostat, vorinostat, valproic acid, and romidepsin. While HDACi may not alter the initial susceptibility of macrophages to HIV infection, they have been shown to decrease HIV release from macrophages ex vitro [68]. Thus far, there are limited studies that have assessed the impact of LRAs on myeloid contributions to pro-virus reactivation kinetics, although the importance for which has been published. In human primary astrocyte cell lines transfected with patient-derived HIV-1 LTR, treatment with HDACi did activate transcription of HIV LTRs [26, 69]. Furthermore, valproic acid (VPA) has been shown to alter activation states of the myelo-monocytic pathway [70] and therefore may have promise in latency reactivation in myeloid cells. In a separate study using CD34+ myeloid precursor cells, results from RNA microarray analysis revealed altered pathways for myeloid cell differentiation [71]. Pathways altered are implicated in changing homeostatic signals for both sustained cell persistence and pro-inflammatory activation of pre-cursor myeloid cells.
Disulfiram and a protein kinase C activator, bryostatin, are non-HDACi with LRA activity. Although well tolerated in clinical trials (NCT01286259, NCT02269605), HIV-1 reactivation was only considered in T cells. However, interestingly, DSF reactivates latent HIV-1 expression in U1 cells (a monocytic cell line) but not in ACH2 cells (a T cell line) [72]. Bryostatin has had moderate LRA activity in astrocyte cell lines both in vitro and in cultured primary astrocytes by inducing HIV-1 expression through NF-kB activation [73]. These LRAs may thus have value in targeting myeloid HIV reservoirs in the central nervous system. One concern however has been a risk for adverse CNS toxicity with LRA reactivating HIV in the CNS [74•, 75]; however, a recent clinical study has shown no long-term neuro-consequences though additional studies are needed.
Biologics
Immunotherapy with immune checkpoint blocking antibodies has been shown success in oncology through reversing T cell immune exhaustion and may have efficacy in the elimination of HIV. A recent study in patients with metastatic non-small-cell lung carcinoma (NSCLC) and HIV infection, who received multiple doses of PD-1 inhibitors while on suppressive ART, one participant showed a decline in viral reservoirs in CD4 T cells [76]. Moreover, of six HIV-positive individuals on therapy who received the anti-PD-L1 antibody BMS-936559, two patients demonstrated improvements in HIV-1-specific CD8+ T cell responses suggesting blockade of the PD-1–PD-L1 pathway has the potential to improve HIV-1-specific immunity and potentially eliminate HIV [77]. Given that PD-L1 is expressed on myeloid cells, the impact of PD-1:PDL-1 blockade on viral reservoirs in myeloid cells would be of interest to future cure initiatives.
3BNC117 and 10-1074 are two of most potent broadly neutralizing antibodies currently available. 3BNC117 targets the CD4-binding site and 10-1074 targets the base of the V3 loop of HIV-1 gp120. In phase 1 clinical studies (NCT03526848), the combination of 3BNC117 and 10-1074 has additive effects extending the median time-to-viral-rebound by 11–15 weeks than treating with 3BNC117 alone [78•]. However, the protective capacity of bnAbs not only is solely due to virus neutralization but can also be attributable to Fc-mediated function [79, 80]. Indeed, studies in HIV-1-infected humanized mice show that the therapeutic activity of anti-HIV-1 bNAbs requires Fc receptor (FcR) effector function to mediate anti-viral protection [81]. Therefore, investigating the role of FcR phagocytic expressors such as monocytes and macrophages for their capacity in direct sequestration and destruction of HIV but in stimulating the secretion of inflammatory mediators could be key in delineating time-to-rebound kinetics or an actual HIV elimination.
Multiple studies demonstrate that α4β7-expressing gut homing CD4 T cells represent early targets for HIV, and therapy targeting this integrin has been considered in the management of HIV-1 infection. Recent studies in the SIV-infected macaques show that treatment, during acute infection with ART and anti-α4β7 therapy, achieved long-term viremic control following treatment interruption [82•], suggesting this may be a novel therapeutic for HIV remission. While several clinical studies are ongoing targeting α4β7 (NCT03147859, NCT03577782, and NCT02788175), in our recent studies, we have observed significant attenuation of lymphoid aggregates in the terminal ileum in inflammatory bowel disease patients with concomitant HIV-1 infection receiving ART and anti-α4β7 therapy [83•]. While we also observed modest impact on persistent viral reservoirs in the gut of these donors, the study has not initiated ART treatment interruption to determine the extent of immunological control of residual HIV reservoirs. Furthermore, given that α4β7 is expressed on myeloid cells [84], monitoring the effects of α4β7 immunotherapy in myeloid cells should be pursued.
Immune-Based Modification Therapies
CD8 T cells targeting HIV-infected CD4 T cells are well described, but it is apparent that this is more challenging when virus resides in myeloid cells. SIV-specific CD8+ T cells can efficiently kill SIV-infected CD4+ T cells but not SIV-infected macrophages [85]. Clayton et al. recently show that HIV-infected macrophages are more resistant to cytotoxic T lymphocytes (CTLs) killing through a granzyme-B inhibitor–mediated mechanism [86•]. Rainho et al. show that CTL-mediated killing of CD4+ T cells and monocyte derived macrophages infected with SIV nef variants was more efficient when targeting CD4+ T cells than macrophages [87]. Finding strategies to enhance CTL activity against infected macrophages are therefore important. Pegu et al. have shown that a bi-specific immunomodulatory protein that stimulates CD8+ T cell effector function thereby initiating latent-infected cell lysis through recognition of Env [88•] may be retargeted towards HIV-infected macrophages. Studies evaluating immunotherapies targeting negative checkpoint receptors [89•, 90, 91] to improve CTL activity as well as harnessing NK cells [92] could also be needed in concert to overcome myeloid cell resistance to CTL killing. Advances have also been made using chimeric antigen receptors (CAR) to re-engineer CD8 T cells for specific lysis of HIV-infected CD4 T cells [93,82,95]. However, engagement of a CAR T cell to mediate monocyte and macrophage killing of infected cells has not been assessed to date.
Excising the CCR5 locus using zinc finger nucleases was the first-in-human application of genome editing accomplished in both T cells and hematopoietic stem/progenitor cells [96]. However, the CRISPR-Cas9 system has now markedly improved the precision by which direct edits to the host genome can be made. However, no clinical trial in the context of HIV cure has genetically engineered myeloid cells despite the feasibility having been published. Zhang et al. have reported using a dCas9-synergistic activation mediator (dCas9-SAM) system to reactivate HIV-1 in both CD4+ T cell and microglial cell lines [97•]. Other promising results in myeloid cells that are presented by Hu et al. were latently infected microglial, pro-monocytes, and T cell lines; they developed a Cas9/guide RNA system to eradicate the HIV-1 genome and immunize target cells against HIV-1 reactivation [98].
Conclusion: Potential Future Clinical Trials
Promising newer strategies are being pursued including the “block and lock” approach for HIV cure. Didehydro-Cortistatin A (dCA) is one compound that inhibits Tat which has been shown in vitro to decrease chromatin accessibility at the HIV LTR, reducing the transcriptional competence of latent HIV-1 provirus under ART [99, 100]. In mouse models, dCA treatment showed strong reductions in both systemic and brain tissue levels of viral RNA [101•, 102]. This may be particularly relevant for myeloid cells in the CNS. dCA therapy, by reducing low-level viremia and preventing viral reactivation from latent reservoirs, makes it a promising therapeutic for tissue sanctuaries like the CNS and where cell-based cytotoxicity strategies can have irreversible consequences. In the promonocyte cell line U1, dCA had no effect on viral mRNA production [102, 103]; however, because the U1 cell line has two integrated proviruses with Tat mutations, U1 cells are therefore already deficient for processive viral production. Further studies of dCA treatment activity in myeloid cells harboring virus should be pursued. Inclusion of a Tat inhibitor to current ART regimens may contribute to a functional cure in which no further immune cells are infected but would need to be paired with a strategy that eliminates already infected cells.
New therapeutic strategies that place emphasis on targeting HIV in non-CD4+ T cells will be imperative on the road to a successful cure. As shown in Table 2, ongoing HIV cure trials may need to be redesigned to better inform on their impact on myeloid HIV reservoirs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Jambo KC, Banda DH, Kankwatira AM, Sukumar N, Allain TJ, Heyderman RS, et al. Small alveolar macrophages are infected preferentially by HIV and exhibit impaired phagocytic function. Mucosal Immunol. 2014;7(5):1116–26. https://doi.org/10.1038/mi.2013.127.
Cai Y, Sugimoto C, Arainga M, Midkiff CC, Liu DX, Alvarez X, et al. Preferential destruction of interstitial macrophages over alveolar macrophages as a cause of pulmonary disease in simian immunodeficiency virus-infected rhesus macaques. J Immunol. 2015;195(10):4884–91. https://doi.org/10.4049/jimmunol.1501194.
Damouche A, Lazure T, Avettand-Fenoel V, Huot N, Dejucq-Rainsford N, Satie AP, et al. Adipose tissue is a neglected viral reservoir and an inflammatory site during chronic HIV and SIV infection. PLoS Pathog. 2015;11(9):e1005153. https://doi.org/10.1371/journal.ppat.1005153.
Zalar A, Figueroa MI, Ruibal-Ares B, Bare P, Cahn P, de Bracco MM et al. Macrophage HIV-1 infection in duodenal tissue of patients on long term HAART. Antiviral Res. 2010;87(2):269–71. https://doi.org/10.1016/j.antiviral.2010.05.005.
Josefsson L, von Stockenstrom S, Faria NR, Sinclair E, Bacchetti P, Killian M et al. The HIV-1 reservoir in eight patients on long-term suppressive antiretroviral therapy is stable with few genetic changes over time. Proc Natl Acad Sci U S A. 2013;110(51):E4987–96. https://doi.org/10.1073/pnas.1308313110.
Ganor Y, Real F, Sennepin A, Dutertre CA, Prevedel L, Xu L et al. HIV-1 reservoirs in urethral macrophages of patients under suppressive antiretroviral therapy. Nat Microbiol. 2019. https://doi.org/10.1038/s41564-018-0335-z.
Bernard-Stoecklin S, Gommet C, Corneau AB, Guenounou S, Torres C, Dejucq-Rainsford N et al. Semen CD4+ T cells and macrophages are productively infected at all stages of SIV infection in macaques. PLoS Pathog. 2013;9(12):e1003810. https://doi.org/10.1371/journal.ppat.1003810.
Kitagawa M, Lackner AA, Martfeld DJ, Gardner MB, Dandekar S. Simian immunodeficiency virus infection of macaque bone marrow macrophages correlates with disease progression in vivo. Am J Pathol. 1991;138(4):921–30.
Gill V, Shattock RJ, Freedman AR, Robinson G, Griffin GE, Gordon-Smith EC et al. Macrophages are the major target cell for HIV infection in long-term bone marrow culture and demonstrate dual susceptibility to lymphocytotropic and monocytotropic strains of HIV-1. Br J Haematoly. 1996;93(1):30–7.
Cenker JJ, Stultz RD, McDonald D. Brain microglial cells are highly susceptible to HIV-1 infection and spread. AIDS Res Hum Retrovir. 2017;33(11):1155–65. https://doi.org/10.1089/AID.2017.0004.
Eugenin EA, Clements JE, Zink MC, Berman JW. Human immunodeficiency virus infection of human astrocytes disrupts blood-brain barrier integrity by a gap junction-dependent mechanism. J Neurosci. 2011;31(26):9456–65. https://doi.org/10.1523/JNEUROSCI.1460-11.2011.
Hutter G, Nowak D, Mossner M, Ganepola S, Mussig A, Allers K, et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N Engl J Med. 2009;360(7):692–8. https://doi.org/10.1056/NEJMoa0802905.
Henrich TJ, Hu Z, Li JZ, Sciaranghella G, Busch MP, Keating SM, et al. Long-term reduction in peripheral blood HIV type 1 reservoirs following reduced-intensity conditioning allogeneic stem cell transplantation. J Infect Dis. 2013;207(11):1694–702. https://doi.org/10.1093/infdis/jit086.
Mavigner M, Watkins B, Lawson B, Lee ST, Chahroudi A, Kean L, et al. Persistence of virus reservoirs in ART-treated SHIV-infected rhesus macaques after autologous hematopoietic stem cell transplant. PLoS Pathog. 2014;10(9):e1004406. https://doi.org/10.1371/journal.ppat.1004406.
Henrich TJ, Hatano H, Bacon O, Hogan LE, Rutishauser R, Hill A, et al. HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: an observational study. PLoS Med. 2017;14(11):e1002417. https://doi.org/10.1371/journal.pmed.1002417.
Persaud D, Gay H, Ziemniak C, Chen YH, Piatak M Jr, Chun TW, et al. Absence of detectable HIV-1 viremia after treatment cessation in an infant. N Engl J Med. 2013;369(19):1828–35. https://doi.org/10.1056/NEJMoa1302976.
Luzuriaga K, Gay H, Ziemniak C, Sanborn KB, Somasundaran M, Rainwater-Lovett K, et al. Viremic relapse after HIV-1 remission in a perinatally infected child. N Engl J Med. 2015;372(8):786–8. https://doi.org/10.1056/NEJMc1413931.
Colby DJ, Trautmann L, Pinyakorn S, Leyre L, Pagliuzza A, Kroon E, et al. Rapid HIV RNA rebound after antiretroviral treatment interruption in persons durably suppressed in Fiebig I acute HIV infection. Nat Med. 2018;24(7):923–6. https://doi.org/10.1038/s41591-018-0026-6.
• Honeycutt JB, Thayer WO, Baker CE, Ribeiro RM, Lada SM, Cao Y, et al. HIV persistence in tissue macrophages of humanized myeloid-only mice during antiretroviral therapy. Nat Med. 2017;23(5):638–43. https://doi.org/10.1038/nm.4319. Using the myeloid-only mouse model, this group demonstrates HIV infection of tissue macrophages is rapidly suppressed by ART. However remarkably, post treatment interruption, a delayed viral rebound was observed and consistent with the establishment of persistent infection in tissue macrophages.
Crowe S, Zhu T, Muller WA. The contribution of monocyte infection and trafficking to viral persistence, and maintenance of the viral reservoir in HIV infection. J Leukoc Biol. 2003;74(5):635–41. https://doi.org/10.1189/jlb.0503204.
Igarashi T, Brown CR, Endo Y, Buckler-White A, Plishka R, Bischofberger N, et al. Macrophage are the principal reservoir and sustain high virus loads in rhesus macaques after the depletion of CD4+ T cells by a highly pathogenic simian immunodeficiency virus/HIV type 1 chimera (SHIV): implications for HIV-1 infections of humans. Proc Natl Acad Sci U S A. 2001;98(2):658–63. https://doi.org/10.1073/pnas.021551798.
Micci L, Alvarez X, Iriele RI, Ortiz AM, Ryan ES, McGary CS, et al. CD4 depletion in SIV-infected macaques results in macrophage and microglia infection with rapid turnover of infected cells. PLoS Pathog. 2014;10(10):e1004467. https://doi.org/10.1371/journal.ppat.1004467.
Kumar A, Abbas W, Herbein G. HIV-1 latency in monocytes/macrophages. Viruses. 2014;6(4):1837–60. https://doi.org/10.3390/v6041837.
Gaskill PJ, Zandonatti M, Gilmartin T, Head SR, Fox HS. Macrophage-derived simian immunodeficiency virus exhibits enhanced infectivity by comparison with T-cell-derived virus. J Virol. 2008;82(3):1615–21. https://doi.org/10.1128/JVI.01757-07.
Zhu T, Muthui D, Holte S, Nickle D, Feng F, Brodie S, et al. Evidence for human immunodeficiency virus type 1 replication in vivo in CD14(+) monocytes and its potential role as a source of virus in patients on highly active antiretroviral therapy. J Virol. 2002;76(2):707–16.
Churchill MJ, Wesselingh SL, Cowley D, Pardo CA, McArthur JC, Brew BJ, et al. Extensive astrocyte infection is prominent in human immunodeficiency virus-associated dementia. Ann Neurol. 2009;66(2):253–8. https://doi.org/10.1002/ana.21697.
Gonzalez-Scarano F, Martin-Garcia J. The neuropathogenesis of AIDS. Nat Rev Immunol. 2005;5(1):69–81. https://doi.org/10.1038/nri1527.
• Lamers SL, Rose R, Ndhlovu LC, Nolan DJ, Salemi M, Maidji E, et al. The meningeal lymphatic system: a route for HIV brain migration? J Neuro-Oncol. 2015;22:275–81. https://doi.org/10.1007/s13365-015-0399-y. Key publication which directly visualizes, by RNAscope, HIV RNA in macrophages of cerebellum from post-mortem brain tissue of an ART-suppressed HIV-infected individual. Presents compelling evidence for the myeloid compartment as critical contributors, despite the ongoing controversy, in the brain as a latent source of replication-competent virus.
Koppensteiner H, Brack-Werner R, Schindler M. Macrophages and their relevance in human immunodeficiency virus type I infection. Retrovirology. 2012;9:82. https://doi.org/10.1186/1742-4690-9-82.
Soulet D, Rivest S. Bone-marrow-derived microglia: myth or reality? Curr Opin Pharmacol. 2008;8(4):508–18. https://doi.org/10.1016/j.coph.2008.04.002.
Beschorner R, Nguyen TD, Gozalan F, Pedal I, Mattern R, Schluesener HJ, et al. CD14 expression by activated parenchymal microglia/macrophages and infiltrating monocytes following human traumatic brain injury. Acta Neuropathol. 2002;103(6):541–9. https://doi.org/10.1007/s00401-001-0503-7.
• Honeycutt JB, Wahl A, Baker C, Spagnuolo RA, Foster J, Zakharova O, et al. Macrophages sustain HIV replication in vivo independently of T cells. J Clin Investig. 2016;126(4):1353–66. https://doi.org/10.1172/JCI84456. Demonstrates that macrophages can sustain HIV replication in the absence of T cells in the myeloid only mouse model. HIV-infected macrophages were distributed in various tissues including the brain. This publication thus also contributes to evidence for the myeloid compartment as critical contributors, despite the ongoing controversy, in the brain as a latent source of replication-competent virus.
Ellery PJ, Tippett E, Chiu YL, Paukovics G, Cameron PU, Solomon A, et al. The CD16+ monocyte subset is more permissive to infection and preferentially harbors HIV-1 in vivo. J Immunol. 2007;178(10):6581–9. https://doi.org/10.4049/jimmunol.178.10.6581.
Valcour VG, Shiramizu BT, Shikuma CM. HIV DNA in circulating monocytes as a mechanism to dementia and other HIV complications. J Leukoc Biol. 2010;87(4):621–6. https://doi.org/10.1189/jlb.0809571.
• Avalos CR, Price SL, Forsyth ER, Pin JN, Shirk EN, Bullock BT, et al. Quantitation of productively infected monocytes and macrophages of simian immunodeficiency virus-infected macaques. J Virol. 2016;90(12):5643–56. https://doi.org/10.1128/JVI.00290-16. Presents a robust method for modified quantitative virus outgrowth assay to assess the contribution of productively infected monocytes and macrophages to HIV- and SIV-infected cells in vivo.
Castellano P, Prevedel L, Eugenin EA. HIV-infected macrophages and microglia that survive acute infection become viral reservoirs by a mechanism involving Bim. Sci Rep. 2017;7(1):12866. https://doi.org/10.1038/s41598-017-12758-w
Sonza S, Mutimer HP, Oelrichs R, Jardine D, Harvey K, Dunne A, Purcell DF, Birch C, Crowe SM. Monocytes harbour replication-competent, non-latent HIV-1 in patients on highly active antiretroviral therapy. Aids. 2001;15(1):17–22.
• Avalos CR, Abreu CM, Queen SE, Li M, Price S, Shirk EN, et al. Brain macrophages in simian immunodeficiency virus-infected, antiretroviral-suppressed macaques: a functional latent reservoir. MBio. 2017;8(4). https://doi.org/10.1128/mBio.01186-17. This publication demonstrates the presence of the latent macrophage reservoir in brains of SIV-infected ART-treated macaques. Also presents compelling evidence for the myeloid compartment as critical contributors, despite the ongoing controversy, in the brain as a latent source of replication-competent virus.
Finzi D, Hermankova M, Pierson T, Carruth LM, Buck C, Chaisson RE, et al. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science. 1997;278(5341):1295–300.
Finzi D, Blankson J, Siliciano JD, Margolick JB, Chadwick K, Pierson T, et al. Latent infection of CD4+ T cells provides a mechanism for lifelong persistence of HIV-1, even in patients on effective combination therapy. Nat Med. 1999;5(5):512–7. https://doi.org/10.1038/8394.
Patel SS, Duby AD, Thiele DL, Lipsky PE. Phenotypic and functional characterization of human T cell clones. J Immunol. 1988;141(11):3726–36.
Wong JK, Hezareh M, Gunthard HF, Havlir DV, Ignacio CC, Spina CA, et al. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science. 1997;278(5341):1291–5.
Kuzmichev YV, Veenhuis RT, Pohlmeyer CW, Garliss CC, Walker-Sperling VE, Blankson JN. A CD3/CD28 microbead-based HIV-1 viral outgrowth assay. J Virus Erad. 2017;3(2):85–9.
Bullen CK, Laird GM, Durand CM, Siliciano JD, Siliciano RF. New ex vivo approaches distinguish effective and ineffective single agents for reversing HIV-1 latency in vivo. Nat Med. 2014;20(4):425–9. https://doi.org/10.1038/nm.3489.
• Fun A, Mok HP, Wills MR, Lever AM. A highly reproducible quantitative viral outgrowth assay for the measurement of the replication-competent latent HIV-1 reservoir. Sci Rep. 2017;7:43231. https://doi.org/10.1038/srep43231. Novel method streamlining the viral outgrowth assay using a dual co-receptor expressing cell line, SupT1-CCR5, to replace the PBMC co-culture. Reduces the protocol to a single-step resting CD4+ T cell purification with a custom antibody cocktail significantly reduce labour and improves assay reproducibility.
Laird GM, Eisele EE, Rabi SA, Lai J, Chioma S, Blankson JN, et al. Rapid quantification of the latent reservoir for HIV-1 using a viral outgrowth assay. PLoS Pathog. 2013;9(5):e1003398. https://doi.org/10.1371/journal.ppat.1003398.
Rosenbloom DI, Elliott O, Hill AL, Henrich TJ, Siliciano JM, Siliciano RF. Designing and interpreting limiting dilution assays: general principles and applications to the latent reservoir for human immunodeficiency virus-1. Open Forum Infect Dis. 2015;2(4):ofv123. https://doi.org/10.1093/ofid/ofv123.
• Massanella M, Yek C, Lada SM, Nakazawa M, Shefa N, Huang K, et al. Improved assays to measure and characterize the inducible HIV reservoir. EBioMedicine. 2018;36:113–21. https://doi.org/10.1016/j.ebiom.2018.09.036. Excellent review of modified methods to quantify the HIV reservoir, including an optimized quantitative viral outgrowth assay.
Procopio FA, Fromentin R, Kulpa DA, Brehm JH, Bebin AG, Strain MC, et al. A novel assay to measure the magnitude of the inducible viral reservoir in HIV-infected individuals. EBioMedicine. 2015;2(8):874–83. https://doi.org/10.1016/j.ebiom.2015.06.019.
Bruner KM, Wang Z, Simonetti FR, Bender AM, Kwon KJ, Sengupta S, et al. A quantitative approach for measuring the reservoir of latent HIV-1 proviruses. Nature. 2019. https://doi.org/10.1038/s41586-019-0898-8.
Fernandez G, Zaikos TD, Khan SZ, Jacobi AM, Behlke MA, Zeichner SL. Targeting IkappaB proteins for HIV latency activation: the role of individual IkappaB and NF-kappaB proteins. J Virol. 2013;87(7):3966–78. https://doi.org/10.1128/JVI.03251-12.
Gallastegui E, Marshall B, Vidal D, Sanchez-Duffhues G, Collado JA, Alvarez-Fernandez C, et al. Combination of biological screening in a cellular model of viral latency and virtual screening identifies novel compounds that reactivate HIV-1. J Virol. 2012;86(7):3795–808. https://doi.org/10.1128/JVI.05972-11.
Iglesias-Ussel M, Vandergeeten C, Marchionni L, Chomont N, Romerio F. High levels of CD2 expression identify HIV-1 latently infected resting memory CD4+ T cells in virally suppressed subjects. J Virol. 2013;87(16):9148–58. https://doi.org/10.1128/JVI.01297-13.
Fromentin R, Bakeman W, Lawani MB, Khoury G, Hartogensis W, DaFonseca S, et al. CD4+ T cells expressing PD-1, TIGIT and LAG-3 contribute to HIV persistence during ART. PLoS Pathog. 2016;12(7):e1005761. https://doi.org/10.1371/journal.ppat.1005761.
Banga R, Procopio FA, Noto A, Pollakis G, Cavassini M, Ohmiti K, et al. PD-1+ and follicular helper T cells are responsible for persistent HIV-1 transcription in treated aviremic individuals. Nat Med. 2016;22:754–61. https://doi.org/10.1038/nm.4113.
Hogan LE, Vasquez J, Hobbs KS, Hanhauser E, Aguilar-Rodriguez B, Hussien R, et al. Increased HIV-1 transcriptional activity and infectious burden in peripheral blood and gut-associated CD4+ T cells expressing CD30. PLoS Pathog. 2018;14(2):e1006856. https://doi.org/10.1371/journal.ppat.1006856.
• Abdel-Mohsen M, Kuri-Cervantes L, Grau-Exposito J, Spivak AM, Nell RA, Tomescu C, et al. CD32 is expressed on cells with transcriptionally active HIV but does not enrich for HIV DNA in resting T cells. Sci Transl Med. 2018;10(437):eaar6759. https://doi.org/10.1126/scitranslmed.aar6759. Key publication providing critical evidence as a rebuttal for CD32 as an insufficient marker of HIV infection. Demonstrates that although CD32 is expressed on cells with transcriptionally active HIV, the expression does not enrich for HIV DNA in resting T cells.
Cohn LB, da Silva IT, Valieris R, Huang AS, Lorenzi JCC, Cohen YZ, et al. Clonal CD4(+) T cells in the HIV-1 latent reservoir display a distinct gene profile upon reactivation. Nat Med. 2018;24(5):604–9. https://doi.org/10.1038/s41591-018-0017-7.
• Veenstra M, Byrd DA, Inglese M, Buyukturkoglu K, Williams DW, Fleysher L, et al. CCR2 on peripheral blood CD14(+)CD16(+) monocytes correlates with neuronal damage, HIV-associated neurocognitive disorders, and peripheral HIV DNA: reseeding of CNS reservoirs? J NeuroImmune Pharmacol. 2018. https://doi.org/10.1007/s11481-018-9792-7. Critical publication providing evidence of CCR2 expressing CD14+CD16+ monocytes as potential peripheral blood biomarkers of neurocognitive impairment in the context of ART-supressed chronic HIV infection.
Siliciano JD, Siliciano RF. HIV-1 eradication strategies: design and assessment. Curr Opin HIV AIDS. 2013;8(4):318–25. https://doi.org/10.1097/COH.0b013e328361eaca.
Archin NM, Bateson R, Tripathy MK, Crooks AM, Yang KH, Dahl NP, et al. HIV-1 expression within resting CD4+ T cells after multiple doses of vorinostat. J Infect Dis. 2014;210(5):728–35. https://doi.org/10.1093/infdis/jiu155.
Archin NM, Liberty AL, Kashuba AD, Choudhary SK, Kuruc JD, Crooks AM, et al. Administration of vorinostat disrupts HIV-1 latency in patients on antiretroviral therapy. Nature. 2012;487(7408):482–5. https://doi.org/10.1038/nature11286.
Elliott JH, McMahon JH, Chang CC, Lee SA, Hartogensis W, Bumpus N, et al. Short-term administration of disulfiram for reversal of latent HIV infection: a phase 2 dose-escalation study. Lancet HIV. 2015;2(12):e520–9. https://doi.org/10.1016/S2352-3018(15)00226-X.
Elliott JH, Wightman F, Solomon A, Ghneim K, Ahlers J, Cameron MJ, et al. Activation of HIV transcription with short-course vorinostat in HIV-infected patients on suppressive antiretroviral therapy. PLoS Pathog. 2014;10(10):e1004473. https://doi.org/10.1371/journal.ppat.1004473.
• Olesen R, Vigano S, Rasmussen TA, Sogaard OS, Ouyang Z, Buzon M, et al. Innate immune activity correlates with CD4 T cell-associated HIV-1 DNA decline during latency-reversing treatment with panobinostat. J Virol. 2015;89(20):10176–89. https://doi.org/10.1128/JVI.01484-15. Evidence provided for mediators of innate immune activity as critical contributors to modulate the effects of latency-reversing agents on the viral reservoir.
Sogaard OS, Graversen ME, Leth S, Olesen R, Brinkmann CR, Nissen SK, et al. The depsipeptide romidepsin reverses HIV-1 latency in vivo. PLoS Pathog. 2015;11(9):e1005142. https://doi.org/10.1371/journal.ppat.1005142.
Spivak AM, Andrade A, Eisele E, Hoh R, Bacchetti P, Bumpus NN, et al. A pilot study assessing the safety and latency-reversing activity of disulfiram in HIV-1-infected adults on antiretroviral therapy. Clin Infect Dis. 2014;58(6):883–90. https://doi.org/10.1093/cid/cit813.
Lu HK, Gray LR, Wightman F, Ellenberg P, Khoury G, Cheng WJ, et al. Ex vivo response to histone deacetylase (HDAC) inhibitors of the HIV long terminal repeat (LTR) derived from HIV-infected patients on antiretroviral therapy. PLoS One. 2014;9(11):e113341. https://doi.org/10.1371/journal.pone.0113341.
Gray LR, Cowley D, Crespan E, Welsh C, Mackenzie C, Wesselingh SL, et al. Reduced basal transcriptional activity of central nervous system-derived HIV type 1 long terminal repeats. AIDS Res Hum Retrovir. 2013;29(2):365–70. https://doi.org/10.1089/AID.2012.0138.
Chateauvieux S, Eifes S, Morceau F, Grigorakaki C, Schnekenburger M, Henry E, et al. Valproic acid perturbs hematopoietic homeostasis by inhibition of erythroid differentiation and activation of the myelo-monocytic pathway. Biochem Pharmacol. 2011;81(4):498–509. https://doi.org/10.1016/j.bcp.2010.11.011.
De Felice L, Tatarelli C, Mascolo MG, Gregorj C, Agostini F, Fiorini R, et al. Histone deacetylase inhibitor valproic acid enhances the cytokine-induced expansion of human hematopoietic stem cells. Cancer Res. 2005;65(4):1505–13. https://doi.org/10.1158/0008-5472.CAN-04-3063.
Doyon G, Zerbato J, Mellors JW, Sluis-Cremer N. Disulfiram reactivates latent HIV-1 expression through depletion of the phosphatase and tensin homolog. AIDS. 2013;27(2):F7–F11. https://doi.org/10.1097/QAD.0b013e3283570620.
Diaz L, Martinez-Bonet M, Sanchez J, Fernandez-Pineda A, Jimenez JL, Munoz E, et al. Bryostatin activates HIV-1 latent expression in human astrocytes through a PKC and NF-kB-dependent mechanism. Sci Rep. 2015;5:12442. https://doi.org/10.1038/srep12442.
• Gray LR, On H, Roberts E, Lu HK, Moso MA, Raison JA, et al. Toxicity and in vitro activity of HIV-1 latency-reversing agents in primary CNS cells. J Neuro-Oncol. 2016;22(4):455–63. https://doi.org/10.1007/s13365-015-0413-4. Significant investigation of toxicity and potency of a panel of commonly used LRA including: panobinostat, romidepsin, vorinostat, disulfrim. Good evaluation of LRA potential activation of HIV transcription in latently infecteted cells of the CNS.
Rasmussen TA, Tolstrup M, Moller HJ, Brinkmann CR, Olesen R, Erikstrup C, et al. Activation of latent human immunodeficiency virus by the histone deacetylase inhibitor panobinostat: a pilot study to assess effects on the central nervous system. Open Forum Infect Dis. 2015;2(1):ofv037. https://doi.org/10.1093/ofid/ofv037.
Ostios-Garcia L, Faig J, Leonardi GC, Adeni AE, Subegdjo SJ, Lydon CA, et al. Safety and efficacy of PD-1 inhibitors among HIV-positive patients with non-small cell lung cancer. J Thorac Oncol. 2018;13(7):1037–42. https://doi.org/10.1016/j.jtho.2018.03.031.
Gay CL, Bosch RJ, Ritz J, Hataye JM, Aga E, Tressler RL, et al. Clinical trial of the anti-PD-L1 antibody BMS-936559 in HIV-1 infected participants on suppressive antiretroviral therapy. J Infect Dis. 2017;215(11):1725–33. https://doi.org/10.1093/infdis/jix191.
• Mendoza P, Gruell H, Nogueira L, Pai JA, Butler AL, Millard K, et al. Combination therapy with anti-HIV-1 antibodies maintains viral suppression. Nature. 2018;561(7724):479–84. https://doi.org/10.1038/s41586-018-0531-2. Foundational publication in broadly neutralizing antibody efficacy. Combination treatment with 3BNC117 and 10-1074 targeting independent sites on the HIV-1 envelope mediated significant neutralization of HIV-1 infection during analytical treatment interruption.
Hessell AJ, Hangartner L, Hunter M, Havenith CE, Beurskens FJ, Bakker JM, et al. Fc receptor but not complement binding is important in antibody protection against HIV. Nature. 2007;449(7158):101–4. https://doi.org/10.1038/nature06106.
Bournazos S, Klein F, Pietzsch J, Seaman MS, Nussenzweig MC, Ravetch JV. Broadly neutralizing anti-HIV-1 antibodies require Fc effector functions for in vivo activity. Cell. 2014;158(6):1243–53. https://doi.org/10.1016/j.cell.2014.08.023.
Riddler SA, Zheng L, Durand CM, Ritz J, Koup RA, Ledgerwood J, et al. Randomized clinical trial to assess the impact of the broadly neutralizing HIV-1 monoclonal antibody VRC01 on HIV-1 persistence in individuals on effective ART. Open Forum Infect Dis. 2018;5(10):ofy242. https://doi.org/10.1093/ofid/ofy242.
• Byrareddy SN, Arthos J, Cicala C, Villinger F, Ortiz KT, Little D, et al. Sustained virologic control in SIV+ macaques after antiretroviral and alpha4beta7 antibody therapy. Science. 2016;354(6309):197–202. https://doi.org/10.1126/science.aag1276. Seminal publication reporting that ART plus infusions of a primatized monoclonal antibody against the α4β7 integrin conferred effective SIV control and moderate subsequent reconstitution of their immune systems occurred without a need for further therapy.
• Uzzan M, Tokuyama M, Rosenstein AK, Tomescu C, SahBandar IN, Ko HM, et al. Anti-alpha4beta7 therapy targets lymphoid aggregates in the gastrointestinal tract of HIV-1-infected individuals. Sci Transl Med. 2018;10(461):eaau4711. https://doi.org/10.1126/scitranslmed.aau4711. Presents the first human study of anti-α4β7 therapy in a cohort of HIV-1 infected subjects with mild inflammatory bowel disease.
Tiisala S, Paavonen T, Renkonen R. Alpha E beta 7 and alpha 4 beta 7 integrins associated with intraepithelial and mucosal homing, are expressed on macrophages. Eur J Immunol. 1995;25(2):411–7. https://doi.org/10.1002/eji.1830250216.
Vojnov L, Martins MA, Bean AT, Veloso de Santana MG, Sacha JB, Wilson NA, et al. The majority of freshly sorted simian immunodeficiency virus (SIV)-specific CD8(+) T cells cannot suppress viral replication in SIV-infected macrophages. J Virol. 2012;86(8):4682–7. https://doi.org/10.1128/JVI.06324-11.
• Clayton KL, Collins DR, Lengieza J, Ghebremichael M, Dotiwala F, Lieberman J, et al. Resistance of HIV-infected macrophages to CD8(+) T lymphocyte-mediated killing drives activation of the immune system. Nat Immunol. 2018;19(5):475–86. https://doi.org/10.1038/s41590-018-0085-3. An extensive body of compelling evidence for cytolytic failure for CD8 mediated killing of HIV-infected macrophages. Highlights the consequential hyperinflammatory conditions that poor killing of macrophages suggesting a myeloid-driven mechanism for ongoing chronic inflammation.
Rainho JN, Martins MA, Cunyat F, Watkins IT, Watkins DI, Stevenson M. Nef is dispensable for resistance of simian immunodeficiency virus-infected macrophages to CD8+ T cell killing. J Virol. 2015;89(20):10625–36. https://doi.org/10.1128/JVI.01699-15.
• Pegu A, Asokan M, Wu L, Wang K, Hataye J, Casazza JP, et al. Activation and lysis of human CD4 cells latently infected with HIV-1. Nat Commun. 2015;6:8447. https://doi.org/10.1038/ncomms9447. Compelling evidence for synergistic activation when a highly potent broadly neutralizing antibody is linked to an activating anti-human CD3 antibody. Demonstrates the feasibility of targeted activation and reduction in the number of latently infected T cells ex vivo and in non-human primate model.
• Chew GM, Fujita T, Webb GM, Burwitz BJ, Wu HL, Reed JS, et al. TIGIT marks exhausted T cells, correlates with disease progression, and serves as a target for immune restoration in HIV and SIV infection. PLoS Pathog. 2016;12(1):e1005349. https://doi.org/10.1371/journal.ppat.1005349. Indicates a novel role for TIGIT during HIV disease pathogenesis in immune exhaustion. Also investigates TIGIT immune-exhaustive role rhesus macaques providing evidence for feasibility of further investigating TIGIT blockade as a means of improving CD8+ T cell function in non-human primate model of HIV/AIDS.
Fujita T, Burwitz BJ, Chew GM, Reed JS, Pathak R, Seger E, et al. Expansion of dysfunctional Tim-3-expressing effector memory CD8+ T cells during simian immunodeficiency virus infection in rhesus macaques. J Immunol. 2014;193(11):5576–83. https://doi.org/10.4049/jimmunol.1400961.
Bui JK, Mellors JW. Reversal of T-cell exhaustion as a strategy to improve immune control of HIV-1. AIDS. 2015;29(15):1911–5. https://doi.org/10.1097/QAD.0000000000000788.
Tomescu C, Mavilio D, Montaner LJ. Lysis of HIV-1-infected autologous CD4+ primary T cells by interferon-alpha-activated NK cells requires NKp46 and NKG2D. AIDS. 2015;29(14):1767–73. https://doi.org/10.1097/QAD.0000000000000777.
Deeks SG, Wagner B, Anton PA, Mitsuyasu RT, Scadden DT, Huang C, et al. A phase II randomized study of HIV-specific T-cell gene therapy in subjects with undetectable plasma viremia on combination antiretroviral therapy. Mol Ther. 2002;5(6):788–97. https://doi.org/10.1006/mthe.2002.0611.
Mitsuyasu RT, Anton PA, Deeks SG, Scadden DT, Connick E, Downs MT, et al. Prolonged survival and tissue trafficking following adoptive transfer of CD4zeta gene-modified autologous CD4(+) and CD8(+) T cells in human immunodeficiency virus-infected subjects. Blood. 2000;96(3):785–93.
Yang OO, Tran AC, Kalams SA, Johnson RP, Roberts MR, Walker BD. Lysis of HIV-1-infected cells and inhibition of viral replication by universal receptor T cells. Proc Natl Acad Sci U S A. 1997;94(21):11478–83.
Perez EE, Wang J, Miller JC, Jouvenot Y, Kim KA, Liu O, et al. Establishment of HIV-1 resistance in CD4+ T cells by genome editing using zinc-finger nucleases. Nat Biotechnol. 2008;26(7):808–16. https://doi.org/10.1038/nbt1410.
• Zhang Y, Yin C, Zhang T, Li F, Yang W, Kaminski R, et al. CRISPR/gRNA-directed synergistic activation mediator (SAM) induces specific, persistent and robust reactivation of the HIV-1 latent reservoirs. Sci Rep. 2015;5:16277. https://doi.org/10.1038/srep16277. First reporting of successful demonstration for latent HIV-1 provirus reactivation by dCas9-SAM guided by target-specific MS2-mediated single guide RNA. This approach specifically targeted the enhancer of the HIV-1 LTR promoter and may inform next generation LRA or block and lock strategies.
Hu W, Kaminski R, Yang F, Zhang Y, Cosentino L, Li F, et al. RNA-directed gene editing specifically eradicates latent and prevents new HIV-1 infection. Proc Natl Acad Sci U S A. 2014;111(31):11461–6. https://doi.org/10.1073/pnas.1405186111.
Wang S, Huber PW, Cui M, Czarnik AW, Mei HY. Binding of neomycin to the TAR element of HIV-1 RNA induces dissociation of Tat protein by an allosteric mechanism. Biochemistry. 1998;37(16):5549–57. https://doi.org/10.1021/bi972808a.
Mestre B, Arzumanov A, Singh M, Boulme F, Litvak S, Gait MJ. Oligonucleotide inhibition of the interaction of HIV-1 Tat protein with the trans-activation responsive region (TAR) of HIV RNA. Biochim Biophys Acta. 1999;1445(1):86–98.
• Kessing CF, Nixon CC, Li C, Tsai P, Takata H, Mousseau G, et al. In vivo suppression of HIV rebound by didehydro-Cortistatin a, a “block-and-lock” strategy for HIV-1 treatment. Cell Rep. 2017;21(3):600–11. https://doi.org/10.1016/j.celrep.2017.09.080. Excellent first reporting of a compound with “block and lock” efficacy mediating suppression of viral rebound after treatment interruption in a humanized HIV-infected mouse model.
Mousseau G, Kessing CF, Fromentin R, Trautmann L, Chomont N, Valente ST. The Tat inhibitor didehydro-Cortistatin A prevents HIV-1 reactivation from latency. MBio. 2015;6(4):e00465. https://doi.org/10.1128/mBio.00465-15.
Adams M, Sharmeen L, Kimpton J, Romeo JM, Garcia JV, Peterlin BM, et al. Cellular latency in human immunodeficiency virus-infected individuals with high CD4 levels can be detected by the presence of promoter-proximal transcripts. Proc Natl Acad Sci U S A. 1994;91(9):3862–6.
Chatziandreou N, Farsakoglu Y, Palomino-Segura M, D,Antuono R, Pizzagalli DU, Sallusto F, et al. Macrophage death following influenza vaccination initiates the inflammatory response that promotes dendritic cell function in the draining lymph node. Cell Rep. 2017;18(10):2427–40. https://doi.org/10.1016/j.celrep.2017.02.026.
Cohen N, Stolarsky-Bennun M, Amir-Kroll H, Margalit R, Nussbaum G, Cohen-Sfady M, et al. Pneumococcal capsular polysaccharide is immunogenic when present on the surface of macrophages and dendritic cells: TLR4 signaling induced by a conjugate vaccine or by lipopolysaccharide is conducive. J Immunol. 2008;180(4):2409–18. https://doi.org/10.4049/jimmunol.180.4.2409.
Bar-On Y, Gruell H, Schoofs T, Pai JA, Nogueira L, Butler AL, et al. Safety and antiviral activity of combination HIV-1 broadly neutralizing antibodies in viremic individuals. Nat Med. 2018;24(11):1701–7. https://doi.org/10.1038/s41591-018-0186-4.
Li B, Xu L, Pi C, Yin Y, Xie K, Tao F, et al. CD89-mediated recruitment of macrophages via a bispecific antibody enhances anti-tumor efficacy. Oncoimmunology. 2017;7(1):e1380142. https://doi.org/10.1080/2162402X.2017.1380142.
Levine BL, Humeau LM, Boyer J, MacGregor RR, Rebello T, Lu X, et al. Gene transfer in humans using a conditionally replicating lentiviral vector. Proc Natl Acad Sci U S A. 2006;103(46):17372–7. https://doi.org/10.1073/pnas.0608138103.
Acknowledgements
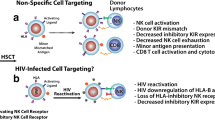
The authors would also like to acknowledge Thomas Premeaux for his construction and design of Fig. 1.
Funding
LCN is supported by the National Institutes of Health (NIH), National Institutes of Mental Health (R01MH112457, R01MH104141), the National Institute of Neurological Disorders and Stroke (R21 NS106970), and the National Institute on Minority Health and Health Disparities (U54 MD007601). The funders of this study had no role in the design of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
LCN has received research support from Tobira Therapeutics and serves as advisory board member for ViiV Healthcare. Brooks I. Mitchell and Elizabeth I. Laws have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Central Nervous System and Cognition
Rights and permissions
About this article
Cite this article
Mitchell, B.I., Laws, E.I. & Ndhlovu, L.C. Impact of Myeloid Reservoirs in HIV Cure Trials. Curr HIV/AIDS Rep 16, 129–140 (2019). https://doi.org/10.1007/s11904-019-00438-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-019-00438-5