Abstract
Purpose of Review
In this review, we present new developments in antiretroviral adherence, focusing on pharmacological measures and real-time adherence monitoring. In addition, new strategies on how to incorporate these new measures into research and clinical care are proposed.
Recent Findings
Antiretroviral drug concentrations in hair and dried blood spots are two novel pharmacological measures of cumulative drug adherence and exposure that have been recently evaluated in HIV treatment and pre-exposure prophylaxis. Real-time adherence monitoring using electronic devices has also proven highly informative, feasible, and well accepted, offering the possibility for an immediate intervention when non-adherence is detected. Both approaches offer considerable advantages over traditional adherence measures in predicting efficacy.
Summary
New methods to objectively monitor adherence in real-time and over long time periods have been developed. Further research is required to better understand how these measures can optimize adherence and, ultimately, improve clinical outcomes in HIV treatment and prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last several decades, the advancements in the efficacy of antiretroviral therapy (ART) have prolonged survival in people living with HIV (PLWH) [1]. Newer medications have become safer and easier to take, most of them are now co-formulated in a single tablet that is taken once-a-day, and long-acting medications with long half-lives, which could facilitate infrequent dosing, are currently in development [2]. However, ART adherence is still challenged by multiple individual (i.e., education, health literacy, poverty, substance use) and community or structural (i.e., stigma, disclosure, access to care) barriers that limit its durability. While adherence to antiretroviral medications continues to be a major predictor of treatment success (and source of variability in outcomes in clinical practice and research studies), we currently do not have a gold standard method to accurately measure ART adherence [3], and the development of new strategies to achieve this goal continues to be a focus in the field. In this review, we discuss some of the most recent methods to objectively measure ART adherence, both in HIV-infection and in pre-exposure prophylaxis (PrEP), their advantages and limitations, and propose new ideas for their possible application in clinical and research settings.
Traditional Measures of Art Adherence: Advantages and Disadvantages
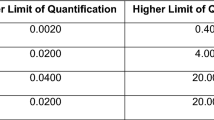
Historically, clinicians and researchers have relied on self-reported measures of ART adherence, which are subject to multiple limitations including recall and social desirability bias, often leading to overestimation of adherence (Table 1) [4,5,6,7]. These methods have been coupled with other measures including pill counts (announced or unannounced) and pharmacy refills. Although more objective than self-report, these measures are still subject to several limitations, including manipulation and the need for a readily available pharmacy staff (Table 1) [8, 9].
Perhaps the most commonly used method for addressing adherence in HIV treatment has been achieving an undetectable HIV viral load (VL), which has been associated with favorable clinical outcomes [10] and prevention of HIV transmission [11]. Because high levels of ART adherence (usually ≥ 95%) were initially required to achieve and sustain and undetectable HIV VL in the early era of ART [12, 13], it has been frequently assumed that a virologically suppressed patient is equivalent to an adherent patient. However, as modern ART has become more potent and pharmacologically forgiving to missed doses, virologic suppression can be achieved with adherence levels around 80–85% [14,15,16,17,18,19], thus making an undetectable HIV VL an imperfect surrogate for high adherence in HIV infection. In addition, HIV VL is not informative of adherence patterns and the development of viremia usually results long after an adherence gap has occurred (Table 1). Lastly, HIV VL as a surrogate marker of adherence is not applicable for PrEP.
Standard electronic adherence monitors (EAMs), such as the medication event monitoring systems (MEMS), and plasma/urine drug concentrations offer a more objective method to quantify adherence and could provide a more comprehensive picture of adherence over a period of time [7, 20]. However, MEMS data can only be made available during a face-to-face encounter and reflects adherence behaviors that have occurred weeks or even months before these data can be evaluated, thus limiting its utility [21] (Table 1). Plasma and urine drug and metabolite concentrations provide proof of drug ingestion and can be predictive of virologic failure in diverse settings [22, 23]. However, their utility is limited by the short half-lives (~ 10–20 h) that most antiretrovirals have in these matrices (Table 1) and by the fact that single-dose concentrations usually match steady-state concentrations [24]. Due to this limitation, plasma and urine drug concentrations are usually only able to detect drug intake within a short period of time (days to 1 week). In addition, they are subject to “white coat” adherence (i.e., improved drug adherence immediately preceding a research or clinical encounter) [25], and threshold concentrations associated with adherence and virologic suppression are only available for few antiretrovirals [26], thus further restricting their broad use in clinical practice.
In response to the limitations of the traditional measures of adherence, new methods that can objectively quantify ART adherence have been developed. These include pharmacological measures of drug exposure and newer EAMs that can measure adherence in real time, both of which are described below.
New Pharmacologic Measures that Quantify Cumulative Drug Exposure
Given the short “look back” period of plasma and urine drug concentrations, new pharmacological methods that can quantify drug adherence and exposure over longer periods of time have been developed, resembling the utility that glycosylated hemoglobin (Hgb A1c) has had in patients with diabetes mellitus [27]. Because they reflect drug intake and metabolism over a period of weeks to months, these new measures provide a picture of cumulative drug exposure as a result of behavior (i.e., drug adherence) and pharmacokinetics (i.e., absorption, distribution, metabolism and excretion) in the same evaluation. To date, the two available matrices in which cumulative ART adherence exposure can be quantified are dried blood spots (DBS) and hair.
Antiretroviral Concentrations in Dried Blood Spots
For over 50 years, DBS have been the method of choice for screening neonates for inborn errors of metabolism and congenital infections (e.g., phenylketonuria, hypothyroidism, and toxoplasmosis) using blood obtained through a needlestick from the heel at the time of birth [28]. This preference for DBS reflects various advantages over traditional plasma blood sampling; it can be collected in small quantities from venipuncture or needlestick, does not require special sample processing, and is associated with a substantial cost benefit [29]. Likewise, DBS samples can be stored for relatively long periods of time after collection and can be shipped without special biohazard precautions [24, 30]. These advantages have led to the use of DBS sampling for analysis beyond the neonatal period, including rapid diagnostics of vector-borne diseases [31], identification of disease-associated genetic mutations [32], diagnosis of HIV infection, and quantification of HIV VL [33,34,35,36], among others.
Recently, the use of DBS for the pharmacokinetic analysis of antiretroviral drugs has become a novel and attractive approach in the research and clinical settings. Early on, multiple DBS methods to measure drug concentrations of various antiretroviral drugs were developed using liquid chromatography, with a primary focus on the quantification of parent drug as an alternative to plasma drug concentrations [37,38,39,40,41,42,43,44,45,46]. A recent example of this approach is the ENCORE1 study, a multicenter, randomized clinical trial that evaluated the safety and efficacy of a reduced dose of efavirenz (EFV) in resource-limited settings. In this study, DBS were used to quantify concentrations of EFV, with an overall good correlation (R2 = 0.904, p < 0.001), albeit underestimation (53 ± 9.5% lower) of plasma drug levels [47]. In another study, drug concentrations of parent tenofovir (TFV) from tenofovir disoproxil fumarate (TDF), lamivudine (3TC) and EFV were evaluated in a pregnant women cohort in rural South Africa, demonstrating an overestimation of adherence in self-report vs. DBS levels, but feasibility of DBS collection in this population [48]. The main limitation of these studies was the focus on parent drug concentrations in DBS, which are expected to also have short half-lives similar to their plasma counterparts, thus restricting their adherence evaluation to a qualitative yes/no information over a short period of time. Additional limitations of DBS sampling, in general, include the potential influence of a variable hematocrit in the setting of anemia (which could under or overestimate drug concentrations [49] and is more prevalent in resource-limited settings and in women), the need of a specialized central laboratory for analysis, and the lack of currently available real-time methods to measure drug concentrations [3].
Parallel to the quantification of antiretroviral parent drug concentrations in DBS, this matrix has also been evaluated for the measurement of intracellular concentrations of antiretroviral anabolites in red blood cells (RBCs), given the abundance of RBCs in DBS [24, 29, 50,51,52]. This area of research has focused on TFV and emtricitabine (FTC), because these nucleoside analogues are also phosphorylated inside of RBCs in a similar fashion to their metabolism in peripheral blood mononuclear cells (PBMCs), where they are phosphorylated to their pharmacologically active moieties TFV diphosphate (TFV-DP) and FTC triphosphate (FTC-TP), respectively [29]. Once phosphorylated, TFV-DP, it is trapped and accumulates 25-fold from first dose to steady state in RBCs, with an intracellular half-life of 17 days [24, 29]. These unique pharmacologic characteristics were used in pharmacokinetic modeling analyses to develop a TFV-DP gradient that can be used to estimate TDF-FTC dosing over a preceding period of approximately 8 weeks [29]. These findings were recently confirmed using directly observed dosing in healthy volunteers, in whom the TFV-DP concentration benchmarks for daily TDF-FTC dosing were established [24]. This methodology has also been extended recently to quantify TFV-DP arising from tenofovir alafenamide (TAF) [52], with an ongoing study to establish the drug concentrations associated with different adherence benchmarks in healthy volunteers (NCT02962739). In contrast to TFV-DP, FTC-TP exhibits an intermediate half-life (~ 35 h) in DBS and can detect a dosing event within the last 7 days, making it a surrogate for plasma drug levels and informative of “white coat” adherence and pre-appointment dosing [24, 51]. Since FTC-TP and TFV-DP are simultaneously quantified in the same DBS sample, the combination of both anabolites can provide comprehensive information on cumulative exposure and recent dosing to TDF-FTC at the same time.
The clinical utility of TFV-DP in DBS has been well established in the PrEP field, where no other surrogate markers of adherence, such as HIV VL, are available. In the iPrEx Open-Label Extension (iPrEx-OLE), TFV-DP in DBS was used as a measure of cumulative exposure to TDF-FTC. In this study, a TFV-DP concentration of ≥ 700 fmol/punch (consistent with four or more doses per week) was associated with 100% protection from HIV infection in men and transgender women who have sex with men [53]. Similar results were observed in PrEP demonstration projects, where high feasibility and acceptability to DBS collection were also confirmed in real-world settings [54, 55]. Currently, DBS are being collected to quantify adherence in various studies evaluating novel PrEP formulations and drug delivery strategies (NCT02720094, NCT03164564, NCT02842086) in the USA and around the world. In addition, DBS sampling has been frequently performed in cases of PrEP breakthrough to determine the role of drug adherence [56,57,58].
In comparison to the extensive data available for PrEP, the utility of TFV-DP in DBS the HIV treatment arena has not been well established. A small study in 35 women with HIV infection in the USA who were taking TFV as part of their ART regimen found that TFV-DP in DBS was negatively correlated with increasing number of days between pharmacy refills, with the lowest TFV-DP concentrations observed in a patient with viremia [59]. Another study explored the utility TFV-DP in DBS in 29 PLWH (90% women) in South Africa. In this study, TFV-DP in DBS showed moderate correlation with electronic real-time adherence monitoring in HIV-infected patients (r = 0.510, p < 0.001) [60]. Of note, none of these studies have evaluated the utility of TFV-DP in DBS to predict viral suppression or other clinical outcomes, which remains a critical gap in the field and is currently being evaluated (NCT02012621).
Antiretroviral Concentrations in Hair
Human hair grows at an average rate of 1 cm per month [61]. This relatively slow growth offers an advantage as an adherence measure in comparison to other biological matrices (i.e., plasma, urine), because the rate of hair growth reflects slow uptake of drugs (and their metabolites) from the systemic circulation over a period of weeks to months [62]. For decades, the use of hair sampling to quantify drug concentrations was limited to the detection of drugs of abuse [63, 64] and was mostly used as a tool in medical criminology [65]. However, a strong body of literature has emerged on the use of hair as a measure of cumulative exposure to a wide variety of therapies [66, 67] and endogenous hormones [68, 69]. Hair collection offers the advantage that it can be obtained in various clinical and non-clinical settings [70, 71], does not require special training or equipment, and can be shipped without biohazard concerns and without the need of a cold chain. It can also be evaluated to determine adherence at different time points in the preceding weeks/months, as the drug concentrations in the proximal vs. the distal segments of the hair strand reflect the effect of time on drug exposure [72]. On the other hand, hair sampling requires a specialized laboratory for processing and could have limited acceptability for sampling in certain patient populations [73, 74].
Antiretroviral hair concentrations have been a matter of research for over a decade [75]. To date, multiple different liquid chromatography-based assays to quantify these drugs have been developed [76,77,78] and utilized as adherence measures in HIV treatment and prevention studies. These methods usually require 50–100 strands of hair that is obtained as close as possible to the scalp [79], which can also be obtained through self-collection, with good correlation with traditional hair collection procedures [80]. In HIV treatment, hair concentrations have been demonstrated to be strong predictors of virologic success in large and diverse prospective clinical cohorts of PLWH, performing better than other traditional adherence measures as predictors of treatment outcomes [79, 81,82,83,84,85]. In comparison to DBS analysis of intracellular anabolites (which is limited to TFV and FTC), hair can be used to quantify drug exposure to multiple antiretrovirals in all drug classes, thus increasing the reach and generalizability of this methodology as a measure of adherence. However, antiretroviral hair concentrations that are associated with known adherence benchmarks using directly observed therapy are only available for TFV (derived from TDF) [86], and additional research in this area is needed to fully characterize the pharmacokinetics of many other antiretrovirals in this matrix.
Drug adherence and exposure in PrEP have also been informed by hair concentrations of antiretrovirals. For example, TFV hair concentrations were recently evaluated in three different PrEP studies which included women (VOICE) and men/transgender women who have sex with men (US PrEP Demonstration Project and iPrEx-OLE). In this analysis, very low cumulative TFV exposure was demonstrated in participants enrolled in the VOICE trial (median intake of 0.2 doses per week) in comparison to participants in iPrEx-OLE (2.9 doses per week) and the PrEP Demo study (6 doses per week) [87], confirming the low adherence rates to TDF observed in the VOICE trial (< 40% of participants had detectable TFV plasma levels) despite high rates of self-reported adherence [88]. In another study that measured adherence and exposure in two randomized, placebo-control studies that evaluated daily and intermittent PrEP in serodiscordant couples and men who have sex with men, TFV and FTC concentrations in hair were strongly correlated with MEMS adherence as well as with plasma and PBMC drug concentrations, but weakly correlated with self-reported adherence [89], highlighting the need for objective and reliable methods of drug adherence in PrEP research. Lastly, in addition to their utility as measures of drug adherence and exposure in PrEP, hair drug concentrations have also been evaluated in the context of drug toxicities associated with TDF, in particular with changes in renal function [90, 91]. Further research is needed to determine the utility of combining hair drug concentrations to prospectively quantify and monitor PrEP adherence and toxicity in future trials and clinical practice.
Measures of Adherence That Can Lead to Actionable Interventions
As new technologies to quantify drug intake and exposure have been developed, better non-pharmacological methods to reliably measure adherence have also emerged. As noted above, EAMs that record medication bottle openings (i.e., MEMS) can provide objective evidence of medication-taking behavior, and have been available for over two decades[3]. However, they are subject to misclassification bias (i.e., “pocket doses” in which multiple doses are removed at one opening of the device for future dosing, as well as “curiosity openings” in which no doses are removed during an opening), which can limit their accuracy [60, 92] and they can only be evaluated at the time of a study or clinic visit, usually long after the adherence gap has occurred [7, 93]. In this regard, EAMs that provide immediate information on dosing events could prove more useful to actively monitor adherence in “real time” between clinical or study visits [94].
Wireless real-time adherence monitoring (RTAM) has been studied in HIV for about a decade, with marked improvements to increase feasibility and reliability in recent years. RTAM devices are electronic pill containers with long battery half-lives, which can usually hold medication supplies for up to 30 days and transmit a time-stamped cellular signal to a central web-based server every time the device is opened (which is recorded as a dosing event) [3]. These adherence data can be monitored in real-time through standard cellular and internet connections, where the data is secure through an encrypted system and available for future use. Other forms of RTAM devices include blister pack holders and larger devices where vaginal microbicides and/or larger quantities of drug supply can be stored [95]. The main advantage that RTAM has over traditional EAMs is that it provides dose-to-dose adherence data that can lead to an intervention at the precise time when it is most likely to be effective (i.e., when non-adherence has been identified), which usually precedes (and could prevent) viral rebound [94, 96]. In addition, RTAM by itself (like standard EAMs) can also improve adherence through Hawthorne effect (a change in behavior in response to the awareness of being observed) [97] and can be perceived as a show of support and extension of care from healthcare providers [98]. A main weakness of RTAM is that it does not confirm medication ingestion [4]. However, RTAM devices have been shown to predict outcomes that are dependent on drug intake, such as viral suppression [99, 100]. In terms of acceptability, RTAM has been well accepted in research studies overall [101, 102], although some concerns about the privacy, autonomy, confidentiality, and/or stigma associated to RTAMs have emerged, in particular in mobile populations who may have difficulty traveling with the device, as well as those who feel marginalized [103, 104]. In addition, because these devices usually depend on a reliable network, the risk for technological failure remains tangible, in particular in areas with intermittent cellular coverage [99, 102, 105]. Modern RTAM devices (and other EAMs) are able to store the dosing events for future network download when a cellular connection becomes available, thus increasing the reliability of these methods [106].
The capability of RTAM to trigger an intervention is an attractive advantage of this adherence monitoring modality. This feature was recently studied in a Ugandan cohort, in which RTAM + 3 different randomized short messaging services (SMS) strategies (scheduled vs. triggered vs. none) resulted in an increase in ART adherence of 11.1% in the scheduled SMS arm, in comparison to the RTAM only arm, with a reduction in > 48 and > 96 h adherence lapses [107]. Notably, participants perceived the SMS as a source of support and motivation in forming good adherence habits [98]. Similar results were found in two studies performed in China and South Africa where RTAM was combined with SMS, even among individuals with high adherence who were virologically suppressed on chronic ART [108, 109]. Various other studies evaluating these and other RTAM-based strategies are currently underway (NCT03086655, NCT02915367, and NCT03292432). In addition, RTAM is planned for a large multinational study of latent tuberculosis treatment in high-risk household contacts of adults with multidrug-resistant pulmonary infection [110].
Potential Uses of New Measures in Research and Clinical Scenarios
Given the unique characteristics of the measures of ART adherence and exposure presented in this review, multiple possible applications of these methods in research studies and clinical care could be considered. Below we propose some strategies that could be implemented in this context.
-
1.
Complementary use of RTAM and pharmacologic measures: Recent studies have demonstrated strong correlation between hair and DBS concentrations of antiretrovirals) [89, 111], which supports their use in combination to monitor adherence to ART and PrEP. While DBS concentrations could be used to estimate average dose intake over a preceding period of time (i.e., ~ 8 weeks), hair drug concentrations could be used to quantify longer drug exposure, including to non TFV/FTC-based regimens. In addition, measures of cumulative and short-term exposure (i.e., plasma drug levels) could also be combined to assess drug intake patterns in ART and PrEP [112]. Furthermore, coupling pharmacologic measures with RTAM is an attractive strategy that remains largely unknown (only available data are with DBS [60]) and should be a focus of future research in the field. Ultimately, an integrated adherence monitoring approach would include RTAM plus a pharmacologic measure, where the adherence data would be used to establish individualized benchmark drug concentrations that could be used to predict virologic failure and/or drug resistance.
-
2.
Assessment of the efficacy of behavioral interventions: As the rollout of ART continues, innovative behavioral interventions to promote optimal and durable adherence in large-scale will be required. Currently, intensive peer support, SMS reminders, and adherence clubs are among some of the interventions that have proven successful [96]. However, not all studies evaluating these (and other) strategies have offered positive results [113], raising the possibility that these interventions do not translate into the expected change in behavior (i.e., adherence). Thus, to fully understand and assess the effect of a behavioral intervention, future studies could benefit from including objective measures of adherence and exposure such as antiretrovirals concentrations in hair and DBS. This approach has already been implemented in a few interventional studies which demonstrated an increase in pre- and postadherence interventions in various settings [114,116,116].
-
3.
Early intervention to improve adherence and exposure-associated clinical outcomes: While virologic suppression has been the ultimate clinical goal of ART to prevent progression to AIDS and transmission of HIV, the forgiveness of new ART combinations has allowed for an increasing tolerance to missed doses that do not result in loss of virologic control. However, it remains unclear whether this forgiveness has any long-term clinical impact. In this context, RTAM and pharmacological measures of adherence could create an opportunity to identify a subset of patients with virologic suppression in whom adherence decreases below a specific threshold (i.e., benchmark for daily dosing) that could be predictive of future or impending treatment failure. This approach could have significant clinical implications for the counseling and evaluation of patients who have an undetectable HIV VL at the time of their study visit and could be used to trigger a targeted intervention in the patients who need one the most. Similarly, it is conceivable that antiretroviral concentrations in hair and DBS could be potentially used to pre-emptively monitor ART and PrEP toxicity, as slow drug accumulation could precede the development of clinically evident toxicities. Further research on the clinical utility of cumulative adherence measures is required.
-
4.
Quantification of adherence in the setting of virologic suppression: An emerging body of literature supports the concept that suboptimal adherence, in the context of virologic suppression, has significant clinical consequences as it relates to residual viral replication [117, 118] and higher levels of biomarkers of inflammation and coagulopathy [119,121,121]. Thus, an objective and reliable estimation of adherence in the virologically suppressed population remains of critical importance. Given the frequent overestimation of adherence based on self-report and other subjective measures [4, 5], RTAM and pharmacological measures could be used to objectively quantify adherence and exposure beyond virologic suppression and identify if variations in adherence result in adverse clinical outcomes.
Conclusions
Optimal and durable adherence to ART and PrEP is required to maximize their therapeutic benefit and assure clinical success. Modern measures that can objectively quantify antiretroviral adherence and exposure have emerged in recent years, increasing our understanding of the adherence patterns that are associated with positive and negative clinical outcomes. To successfully complement the rapidly evolving field of antiretroviral drug development, future research should focus on the feasibility and clinical application of strategies that combine multiple ART adherence methods in clinical practice and research studies.
References
Palella FJ Jr, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, et al. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43(1):27–34. https://doi.org/10.1097/01.qai.0000233310.90484.16.
Margolis DA, Gonzalez-Garcia J, Stellbrink HJ, Eron JJ, Yazdanpanah Y, Podzamczer D, et al. Long-acting intramuscular cabotegravir and rilpivirine in adults with HIV-1 infection (LATTE-2): 96-week results of a randomised, open-label, phase 2b, non-inferiority trial. Lancet. 2017;390(10101):1499–510. https://doi.org/10.1016/S0140-6736(17)31917-7.
Garrison LE, Haberer JE. Technological methods to measure adherence to antiretroviral therapy and preexposure prophylaxis. Curr Opin HIV AIDS. 2017;12(5):467–74. https://doi.org/10.1097/COH.0000000000000393.
Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behav. 2007;11(2):161–73. https://doi.org/10.1007/s10461-006-9133-3.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45. https://doi.org/10.1007/s10461-006-9078-6.
Turner BJ. Adherence to antiretroviral therapy by human immunodeficiency virus-infected patients. J Infect Dis. 2002;185(Suppl 2):S143–51. https://doi.org/10.1086/340197.
Arnsten JH, Demas PA, Farzadegan H, Grant RW, Gourevitch MN, Chang CJ, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-report and electronic monitoring. Clin Infect Dis. 2001;33(8):1417–23. https://doi.org/10.1086/323201.
Okatch H, Beiter K, Eby J, Chapman J, Marukutira T, Tshume O, et al. Brief report: apparent antiretroviral overadherence by pill count is associated with HIV treatment failure in adolescents. J Acquir Immune Defic Syndr. 2016;72(5):542–5. https://doi.org/10.1097/QAI.0000000000000994.
Bisson GP, Gross R, Bellamy S, Chittams J, Hislop M, Regensberg L, et al. Pharmacy refill adherence compared with CD4 count changes for monitoring HIV-infected adults on antiretroviral therapy. PLoS Med. 2008;5(5):e109. https://doi.org/10.1371/journal.pmed.0050109.
Grabar S, Le Moing V, Goujard C, Leport C, Kazatchkine MD, Costagliola D, et al. Clinical outcome of patients with HIV-1 infection according to immunologic and virologic response after 6 months of highly active antiretroviral therapy. Ann Intern Med. 2000;133(6):401–10. https://doi.org/10.7326/0003-4819-133-6-200009190-00007.
Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Curr Opin HIV AIDS. 2012;7(2):99–105. https://doi.org/10.1097/COH.0b013e32834f5cf2.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. https://doi.org/10.7326/0003-4819-133-1-200007040-00004.
Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14(4):357–66. https://doi.org/10.1097/00002030-200003100-00008.
Viswanathan S, Detels R, Mehta SH, Macatangay BJ, Kirk GD, Jacobson LP. Level of adherence and HIV RNA suppression in the current era of highly active antiretroviral therapy (HAART). AIDS Behav. 2015;19(4):601–11. https://doi.org/10.1007/s10461-014-0927-4.
Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41. https://doi.org/10.1086/507526.
Shuter J, Sarlo JA, Kanmaz TJ, Rode RA, Zingman BS. HIV-infected patients receiving lopinavir/ritonavir-based antiretroviral therapy achieve high rates of virologic suppression despite adherence rates less than 95%. J Acquir Immune Defic Syndr. 2007;45(1):4–8. https://doi.org/10.1097/QAI.0b013e318050d8c2.
Martin M, Del Cacho E, Codina C, Tuset M, De Lazzari E, Mallolas J, et al. Relationship between adherence level, type of the antiretroviral regimen, and plasma HIV type 1 RNA viral load: a prospective cohort study. AIDS Res Hum Retrovir. 2008;24(10):1263–8. https://doi.org/10.1089/aid.2008.0141.
Maggiolo F, Airoldi M, Kleinloog HD, Callegaro A, Ravasio V, Arici C, et al. Effect of adherence to HAART on virologic outcome and on the selection of resistance-conferring mutations in NNRTI- or PI-treated patients. HIV Clin Trials. 2007;8(5):282–92. https://doi.org/10.1310/hct0805-282.
Viswanathan S, Justice AC, Alexander GC, Brown TT, Gandhi NR, McNicholl IR, et al. Adherence and HIV RNA suppression in the current era of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2015;69(4):493–8. https://doi.org/10.1097/QAI.0000000000000643.
Thirumurthy H, Siripong N, Vreeman RC, Pop-Eleches C, Habyarimana JP, Sidle JE, et al. Differences between self-reported and electronically monitored adherence among patients receiving antiretroviral therapy in a resource-limited setting. AIDS. 2012;26(18):2399–403. https://doi.org/10.1097/QAD.0b013e328359aa68.
Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med. 2001;134(10):968–77. https://doi.org/10.7326/0003-4819-134-10-200105150-00011.
Marzolini C, Telenti A, Decosterd LA, Greub G, Biollaz J, Buclin T. Efavirenz plasma levels can predict treatment failure and central nervous system side effects in HIV-1-infected patients. AIDS. 2001;15(1):71–5. https://doi.org/10.1097/00002030-200101050-00011.
Gunda DW, Kasang C, Kidenya BR, Kabangila R, Mshana SE, Kidola J, et al. Plasma concentrations of efavirenz and nevirapine among HIV-infected patients with immunological failure attending a tertiary hospital in North-western Tanzania. PLoS One. 2013;8(9):e75118. https://doi.org/10.1371/journal.pone.0075118.
Anderson PL, Liu AY, Castillo-Mancilla JR, Gardner EM, Seifert SM, McHugh C, et al. Intracellular tenofovir-diphosphate and emtricitabine-triphosphate in dried blood spots following directly observed therapy: the DOT-DBS study. Antimicrob Agents Chemother. 2017;62(1):e01710–7. https://doi.org/10.1128/AAC.01710-17.
Podsadecki TJ, Vrijens BC, Tousset EP, Rode RA, Hanna GJ. “White coat compliance” limits the reliability of therapeutic drug monitoring in HIV-1-infected patients. HIV Clin Trials. 2008;9(4):238–46. https://doi.org/10.1310/hct0904-238.
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf.
Koenig RJ, Peterson CM, Jones RL, Saudek C, Lehrman M, Cerami A. Correlation of glucose regulation and hemoglobin AIc in diabetes mellitus. N Engl J Med. 1976;295(8):417–20. https://doi.org/10.1056/NEJM197608192950804.
Lehmann S, Delaby C, Vialaret J, Ducos J, Hirtz C. Current and future use of “dried blood spot” analyses in clinical chemistry. Clin Chem Lab Med. 2013;51(10):1897–909. https://doi.org/10.1515/cclm-2013-0228.
Castillo-Mancilla JR, Zheng JH, Rower JE, Meditz A, Gardner EM, Predhomme J, et al. Tenofovir, emtricitabine, and tenofovir diphosphate in dried blood spots for determining recent and cumulative drug exposure. AIDS Res Hum Retrovir. 2013;29(2):384–90. https://doi.org/10.1089/AID.2012.0089.
Johannessen A. Dried blood spots in HIV monitoring: applications in resource-limited settings. Bioanalysis. 2010;2(11):1893–908. https://doi.org/10.4155/bio.10.120.
Balmaseda A, Saborio S, Tellez Y, Mercado JC, Perez L, Hammond SN, et al. Evaluation of immunological markers in serum, filter-paper blood spots, and saliva for dengue diagnosis and epidemiological studies. J Clin Virol. 2008;43(3):287–91. https://doi.org/10.1016/j.jcv.2008.07.016.
Conroy JM, Trivedi G, Sovd T, Caggana M. The allele frequency of mutations in four genes that confer enhanced susceptibility to venous thromboembolism in an unselected group of New York State newborns. Thromb Res. 2000;99(4):317–24. https://doi.org/10.1016/S0049-3848(00)00254-1.
Snijdewind IJ, van Kampen JJ, Fraaij PL, van der Ende ME, Osterhaus AD, Gruters RA. Current and future applications of dried blood spots in viral disease management. Antivir Res. 2012;93(3):309–21. https://doi.org/10.1016/j.antiviral.2011.12.011.
Lakshmi V, Sudha T, Dandona R, Teja VD, Kumar GA, Dandona L. Application of human immunodeficiency virus type 1 BED enzyme immunoassay on dried blood spots in India. J Med Microbiol. 2009;58(Pt 3):312–7. https://doi.org/10.1099/jmm.0.005249-0.
Chang J, de Sousa A, Sabatier J, Assane M, Zhang G, Bila D, et al. Performance characteristics of finger-stick dried blood spots (DBS) on the determination of human immunodeficiency virus (HIV) treatment failure in a pediatric population in Mozambique. PLoS One. 2017;12(7):e0181054. https://doi.org/10.1371/journal.pone.0181054.
Zeh C, Ndiege K, Inzaule S, Achieng R, Williamson J, Chih-Wei Chang J, et al. Evaluation of the performance of Abbott m2000 and Roche COBAS Ampliprep/COBAS Taqman assays for HIV-1 viral load determination using dried blood spots and dried plasma spots in Kenya. PLoS One. 2017;12(6):e0179316. https://doi.org/10.1371/journal.pone.0179316.
Duthaler U, Berger B, Erb S, Battegay M, Letang E, Gaugler S et al. Automated high throughput analysis of antiretroviral drugs in dried blood spots. J Mass Spectrom. 2017.
Kromdijk W, Mulder JW, Smit PM, ter Heine R, Beijnen JH, Huitema AD. Short communication therapeutic drug monitoring of antiretroviral drugs at home using dried blood spots: a proof-of-concept study. Antivir Ther. 2013;18(6):821–5. https://doi.org/10.3851/IMP2501.
Zheng J-H, Guida LA, Rower C, Castillo-Mancilla J, Meditz A, Klein B, et al. Quantitation of tenofovir and emtricitabine in dried blood spots (DBS) with LC–MS/MS. J Pharm Biomed Anal. 2014;88:144–51. https://doi.org/10.1016/j.jpba.2013.08.033.
Amara AB, Else LJ, Tjia J, Olagunju A, Puls RL, Khoo S, et al. A validated method for quantification of efavirenz in dried blood spots using high-performance liquid chromatography–mass spectrometry. Ther Drug Monit. 2015;37(2):220–8. https://doi.org/10.1097/FTD.0000000000000127.
Koal T, Burhenne H, Roemling R, Svoboda M, Resch K, Kaever V. Quantification of antiretroviral drugs in dried blood spot samples by means of liquid chromatography/tandem mass spectrometry. Rapid Commun Mass Spectrom. 2005;19(21):2995–3001. https://doi.org/10.1002/rcm.2158.
Meesters RJ, van Kampen JJ, Reedijk ML, Scheuer RD, Dekker LJ, Burger DM, et al. Ultrafast and high-throughput mass spectrometric assay for therapeutic drug monitoring of antiretroviral drugs in pediatric HIV-1 infection applying dried blood spots. Anal Bioanal Chem. 2010;398(1):319–28. https://doi.org/10.1007/s00216-010-3952-9.
Ter Heine R, Rosing H, Van Gorp E, Mulder J, Van der Steeg W, Beijnen J, et al. Quantification of protease inhibitors and non-nucleoside reverse transcriptase inhibitors in dried blood spots by liquid chromatography–triple quadrupole mass spectrometry. J Chromatogr B. 2008;867(2):205–12. https://doi.org/10.1016/j.jchromb.2008.04.003.
Ter Heine R, Hillebrand M, Rosing H, van Gorp E, Mulder J, Beijnen J, et al. Quantification of the HIV-integrase inhibitor raltegravir and detection of its main metabolite in human plasma, dried blood spots and peripheral blood mononuclear cell lysate by means of high-performance liquid chromatography tandem mass spectrometry. J Pharm Biomed Anal. 2009;49(2):451–8. https://doi.org/10.1016/j.jpba.2008.11.025.
Ter Heine R, Rosing H, Van Gorp E, Mulder J, Beijnen J, Huitema A. Quantification of etravirine (TMC125) in plasma, dried blood spots and peripheral blood mononuclear cell lysate by liquid chromatography tandem mass spectrometry. J Pharm Biomed Anal. 2009;49(2):393–400. https://doi.org/10.1016/j.jpba.2008.10.040.
Van Schooneveld T, Swindells S, Nelson SR, Robbins BL, Moore R, Fletcher CV. Clinical evaluation of a dried blood spot assay for atazanavir. Antimicrob Agents Chemother. 2010;54(10):4124–8. https://doi.org/10.1128/AAC.00297-10.
Amara AB, Else LJ, Carey D, Khoo S, Back DJ, Amin J et al. A comparison of dried blood spots versus conventional plasma collection for the characterisation of efavirenz pharmacokinetics in a large-scale global clinical trial-The ENCORE1 study. Therapeutic Drug Monitoring. 2017.
Alcaide ML, Ramlagan S, Rodriguez VJ, Cook R, Peltzer K, Weiss SM et al. Self-report and dry blood spot measurement of antiretroviral medications as markers of adherence in pregnant women in rural South Africa. AIDS and Behavior. 2017;1–6.
Wilhelm AJ, den Burger JC, Swart EL. Therapeutic drug monitoring by dried blood spot: progress to date and future directions. Clin Pharmacokinet. 2014;53(11):961–73. https://doi.org/10.1007/s40262-014-0177-7.
Zheng JH, Rower C, McAllister K, Castillo-Mancilla J, Klein B, Meditz A, et al. Application of an intracellular assay for determination of tenofovir-diphosphate and emtricitabine-triphosphate from erythrocytes using dried blood spots. J Pharm Biomed Anal. 2016;122:16–20. https://doi.org/10.1016/j.jpba.2016.01.038.
Castillo-Mancilla J, Seifert S, Campbell K, Coleman S, McAllister K, Zheng JH, et al. Emtricitabine-triphosphate in dried blood spots as a marker of recent dosing. Antimicrob Agents Chemother. 2016;60(11):6692–7. https://doi.org/10.1128/AAC.01017-16.
Castillo-Mancilla J, Coyle RP, Zheng JH, Ellison L, Roon L, Fey J et al. Tenofovir diphosphate arising from TAF is quantifiable in dried blood spots. Poster Presented at CROI 2017 Seattle, WA Abstract 405.
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. https://doi.org/10.1016/S1473-3099(14)70847-3.
Hosek S, Rudy B, Landovitz RJ, Kapogiannis BG, Siberry G, Rutledge B et al. An HIV-pre-exposure prophylaxis (PrEP) demonstration project and safety study for young men who have sex with men in the united states (ATN 110). IAS 2015: 8th IAS Conference on HIV Pathogenesis Treatment and Prevention. 2015.
Liu AY, Cohen SE, Vittinghoff E, Anderson PL, Doblecki-Lewis S, Bacon O, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2016;176(1):75–84. https://doi.org/10.1001/jamainternmed.2015.4683.
Knox DC, Anderson PL, Harrigan PR, Tan DH. Multidrug-resistant HIV-1 infection despite preexposure prophylaxis. N Engl J Med. 2017;376(5):501–2. https://doi.org/10.1056/NEJMc1611639.
Hoornenborg E, Prins M, Achterbergh RC, Woittiez LR, Cornelissen M, Jurriaans S et al. Acquisition of wild-type HIV-1 infection in a patient on pre-exposure prophylaxis with high intracellular concentrations of tenofovir diphosphate: a case report. Lancet HIV. 2017.
Markowitz M, Grossman H, Anderson PL, Grant R, Gandhi M, Horng H et al. Newly acquired infection with multi-drug resistant HIV-1 in a patient adherent to pre-exposure prophylaxis. JAIDS J Acquired Immune Deficiency Syndromes. 2017.
Castillo-Mancilla JR, Searls K, Caraway P, Zheng JH, Gardner EM, Predhomme J, et al. Short communication: tenofovir diphosphate in dried blood spots as an objective measure of adherence in HIV-infected women. AIDS Res Hum Retrovir. 2015;31(4):428–32. https://doi.org/10.1089/AID.2014.0229.
Warne P, Robbins R, Anderson P, Gouse H, Joska J, Leu CS et al. Utility of dried blood spot-derived ARV biomarkers as an objective measure of treatment adherence in South Africa. Poster Presented at IAPAC Adherence 2015 Miami, FL Abstract 241.
LeBeau MA, Montgomery MA, Brewer JD. The role of variations in growth rate and sample collection on interpreting results of segmental analyses of hair. Forensic Sci Int. 2011;210(1):110–6. https://doi.org/10.1016/j.forsciint.2011.02.015.
Beumer J, Bosman I, Maes R. Hair as a biological specimen for therapeutic drug monitoring. Int J Clin Pract. 2001;55(6):353–7.
Balabanova S, Homoki J. Determination of cocaine in human hair by gas chromatography/mass spectrometry. Int J Legal Med. 1987;98(4):235–40.
Mieczowski T, Newel R. Comparing hair and urine assays for cocaine and marijuana. Fed Probat. 1993;57:59.
Gandhi M, Greenblatt RM. Hair it is: the long and short of monitoring antiretroviral treatment. Ann Intern Med. 2002;137(8):696–7. https://doi.org/10.7326/0003-4819-137-8-200210150-00016.
Song SH, Jun SH, Park KU, Yoon Y, Lee JH, Kim JQ, et al. Simultaneous determination of first-line anti-tuberculosis drugs and their major metabolic ratios by liquid chromatography/tandem mass spectrometry. Rapid Commun Mass Spectrom. 2007;21(7):1331–8. https://doi.org/10.1002/rcm.2961.
Williams J, Myson V, Steward S, Jones G, Wilson JF, Kerr MP, et al. Self-discontinuation of antiepileptic medication in pregnancy: detection by hair analysis. Epilepsia. 2002;43(8):824–31. https://doi.org/10.1046/j.1528-1157.2002.38601.x.
Sauvé B, Koren G, Walsh G, Tokmakejian S, Van Uum SH. Measurement of cortisol in human hair as a biomarker of systemic exposure. Clin Invest Med. 2007;30(5):183–91. https://doi.org/10.25011/cim.v30i5.2894.
Gao W, Stalder T, Foley P, Rauh M, Deng H, Kirschbaum C. Quantitative analysis of steroid hormones in human hair using a column-switching LC–APCI–MS/MS assay. J Chromatogr B. 2013;928:1–8. https://doi.org/10.1016/j.jchromb.2013.03.008.
Prasitsuebsai W, Kerr SJ, Truong KH, Ananworanich J, Do VC, Nguyen LV, et al. Using lopinavir concentrations in hair samples to assess treatment outcomes on second-line regimens among Asian children. AIDS Res Hum Retrovir. 2015;31(10):1009–14. https://doi.org/10.1089/aid.2015.0111.
Hickey MD, Salmen CR, Tessler RA, Omollo D, Bacchetti P, Magerenge R, et al. Antiretroviral concentrations in small hair samples as a feasible marker of adherence in rural Kenya. J Acquir Immune Defic Syndr. 1999;66(3):311.
Strano-Rossi S, Bermejo-Barrera A, Chiarotti M. Segmental hair analysis for cocaine and heroin abuse determination. Forensic Sci Int. 1995;70(1–3):211–6. https://doi.org/10.1016/0379-0738(94)01620-K.
Olds PK, Kiwanuka JP, Nansera D, Huang Y, Bacchetti P, Jin C, et al. Assessment of HIV antiretroviral therapy adherence by measuring drug concentrations in hair among children in rural Uganda. AIDS Care. 2015;27(3):327–32. https://doi.org/10.1080/09540121.2014.983452.
Robbins R, Gouse H, Warne P, Mtingeni Y, Henry M, Lopez-Rios J et al. Feasibility and acceptability of hair and dried blood spot derived ARV biomarkers as objective measures of treatment adherence in South Africa. Poster Presented at IAPAC Adherence 2015 Miami, FL Abstract 210.
Bernard L, Vuagnat A, Peytavin G, Hallouin M-C, Bouhour D, Nguyen TH, et al. Relationship between levels of indinavir in hair and virologic response to highly active antiretroviral therapy. Ann Intern Med. 2002;137(8):656–9. https://doi.org/10.7326/0003-4819-137-8-200210150-00009.
Huang Y, Yang Q, Yoon K, Lei Y, Shi R, Gee W, et al. Microanalysis of the antiretroviral nevirapine in human hair from HIV-infected patients by liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem. 2011;401(6):1923–33. https://doi.org/10.1007/s00216-011-5278-7.
Huang Y, Gandhi M, Greenblatt RM, Gee W, Lin ET, Messenkoff N. Sensitive analysis of anti-HIV drugs, efavirenz, lopinavir and ritonavir, in human hair by liquid chromatography coupled with tandem mass spectrometry. Rapid Commun Mass Spectrom. 2008;22(21):3401–9. https://doi.org/10.1002/rcm.3750.
Gandhi M, Yang Q, Bacchetti P, Huang Y. A low-cost method for analyzing nevirapine levels in hair as a marker of adherence in resource-limited settings. AIDS Res Hum Retrovir. 2014;30(1):25–8. https://doi.org/10.1089/aid.2013.0239.
Gandhi M, Ameli N, Bacchetti P, Anastos K, Gange SJ, Minkoff H, et al. Atazanavir concentration in hair is the strongest predictor of outcomes on antiretroviral therapy. Clin Infect Dis. 2011;52(10):1267–75. https://doi.org/10.1093/cid/cir131.
Saberi P, Neilands TB, Ming K, Johnson MO, Kuncze K, Koss CA et al. Strong correlation between concentrations of antiretrovirals in home-collected and study-collected hair samples: implications for adherence monitoring. JAIDS J Acquir Immune Defic Syndr. 2017.
Pintye J, Bacchetti P, Teeraananchai S, Kerr S, Prasitsuebsai W, Singtoroj T et al. Brief report: lopinavir hair concentrations are the strongest predictor of viremia in HIV-infected Asian children and adolescents on second-line antiretroviral therapy. JAIDS J Acquir Immune Defic Syndr. 2017.
Van Zyl GU, Van Mens TE, McIlleron H, Zeier M, Nachega JB, Decloedt E, et al. Low lopinavir plasma or hair concentrations explain second line protease inhibitor failures in a resource-limited setting. J Acquir Immune Defic Syndr. 1999;56(4):333.
Gandhi M, Ameli N, Bacchetti P, Gange SJ, Anastos K, Levine A, et al. Protease inhibitor levels in hair samples strongly predict virologic responses to HIV treatment. AIDS (London, England). 2009;23(4):471–8. https://doi.org/10.1097/QAD.0b013e328325a4a9.
Koss CA, Natureeba P, Mwesigwa J, Cohan D, Nzarubara B, Bacchetti P, et al. Hair concentrations of antiretrovirals predict viral suppression in HIV-infected pregnant and breastfeeding Ugandan women. AIDS (London, England). 2015;29(7):825–30. https://doi.org/10.1097/QAD.0000000000000619.
Baxi SM, Greenblatt RM, Bacchetti P, Jin C, French AL, Keller MJ, et al. Nevirapine concentration in hair samples is a strong predictor of Virologic suppression in a prospective cohort of HIV-infected patients. PLoS One. 2015;10(6):e0129100. https://doi.org/10.1371/journal.pone.0129100.
Liu AY, Yang Q, Huang Y, Bacchetti P, Anderson PL, Jin C, et al. Strong relationship between oral dose and tenofovir hair levels in a randomized trial: hair as a potential adherence measure for pre-exposure prophylaxis (PrEP). PLoS One. 2014;9(1):e83736. https://doi.org/10.1371/journal.pone.0083736.
Koss CA, Bacchetti P, Hillier SL, Livant E, Horng H, Mgodi N et al. Differences in cumulative exposure and adherence to tenofovir in the VOICE, iPrEx OLE, and PrEP demo studies as determined via hair concentrations. AIDS Res Human Retroviruses. 2017.
Dai JY, Hendrix CW, Richardson BA, Kelly C, Marzinke M, Chirenje ZM, et al. Pharmacological measures of treatment adherence and risk of HIV infection in the VOICE study. J Infect Dis. 2015;213(3):335–42. https://doi.org/10.1093/infdis/jiv333.
Baxi SM, Liu A, Bacchetti P, Mutua G, Sanders EJ, Kibengo FM, et al. Comparing the novel method of assessing PrEP adherence/exposure using hair samples to other pharmacologic and traditional measures. J Acquir Immune Defic Syndr. 1999;68(1):13.
Gandhi M, Murnane PM, Bacchetti P, Elion R, Kolber MA, Cohen SE, et al. Hair levels of preexposure prophylaxis drugs measure adherence and are associated with renal decline among men/transwomen. AIDS. 2017;31(16):2245–51. https://doi.org/10.1097/QAD.0000000000001615.
Gandhi M, Glidden DV, Mayer K, Schechter M, Buchbinder S, Grinsztejn B, et al. Association of age, baseline kidney function, and medication exposure with declines in creatinine clearance on pre-exposure prophylaxis: an observational cohort study. Lancet HIV. 2016;3(11):e521–e8. https://doi.org/10.1016/S2352-3018(16)30153-9.
Vreeman RC, Nyandiko WM, Liu H, Tu W, Scanlon ML, Slaven JE et al. Measuring adherence to antiretroviral therapy in children and adolescents in western Kenya. J Int AIDS Soc. 2014;17(1).
Samet JH, Sullivan LM, Traphagen ET, Ickovics JR. Measuring adherence among HIV-infected persons: is MEMS consummate technology? AIDS Behav. 2001;5(1):21–30. https://doi.org/10.1023/A:1009503320498.
Haberer JE. Actionable adherence monitoring to optimise intervention. Lancet HIV. 2017;4(1):e5–6. https://doi.org/10.1016/S2352-3018(16)30191-6.
Gengiah TN, Upfold M, Naidoo A, Mansoor LE, Feldblum PJ, Karim QA, et al. Monitoring microbicide gel use with real-time notification of the container’s opening events: results of the CAPRISA Wisebag study. AIDS Behav. 2014;18(5):833–40. https://doi.org/10.1007/s10461-014-0750-y.
Haberer JE, Sabin L, Amico KR, Orrell C, Galárraga O, Tsai AC et al. Improving antiretroviral therapy adherence in resource-limited settings at scale: a discussion of interventions and recommendations. J Int AIDS Soc. 2017;20(1).
Deschamps AE, Van Wijngaerden E, Denhaerynck K, De Geest S, Vandamme AM. Use of electronic monitoring induces a 40-day intervention effect in HIV patients. J Acquir Immune Defic Syndr. 2006;43(2):247–8. https://doi.org/10.1097/01.qai.0000246034.86135.89.
Ware NC, Pisarski EE, Tam M, Wyatt MA, Atukunda E, Musiimenta A, et al. The meanings in the messages: how SMS reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30(8):1287–94. https://doi.org/10.1097/QAD.0000000000001035.
Haberer JE, Kahane J, Kigozi I, Emenyonu N, Hunt P, Martin J, et al. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav. 2010;14(6):1340–6. https://doi.org/10.1007/s10461-010-9799-4.
Haberer JE, Musinguzi N, Boum Y 2nd, Siedner MJ, Mocello AR, Hunt PW, et al. Duration of antiretroviral therapy adherence interruption is associated with risk of virologic rebound as determined by real-time adherence monitoring in rural Uganda. J Acquir Immune Defic Syndr. 1999;70(4):386–92.
Haberer JE, Robbins GK, Ybarra M, Monk A, Ragland K, Weiser SD, et al. Real-time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptable. AIDS Behav. 2012;16(2):375–82. https://doi.org/10.1007/s10461-011-9933-y.
Haberer JE, Kiwanuka J, Nansera D, Muzoora C, Hunt PW, So J et al. Real-time adherence monitoring of antiretroviral therapy among HIV-infected adults and children in rural Uganda. AIDS (London, England). 2013;27(13).
Bachman DeSilva M, Gifford AL, Keyi X, Li Z, Feng C, Brooks M et al. Feasibility and acceptability of a real-time adherence device among HIV-positive IDU patients in China. AIDS Res Treat. 2013;2013.
Campbell JI, Eyal N, Musiimenta A, Haberer JE. Ethical questions in medical electronic adherence monitoring. J Gen Intern Med. 2016;31(3):338–42. https://doi.org/10.1007/s11606-015-3502-4.
de Sumari-de Boer IM, van den Boogaard J, Ngowi KM, Semvua HH, Kiwango KW, Aarnoutse RE, et al. Feasibility of real time medication monitoring among HIV infected and TB patients in a resource-limited setting. AIDS Behav. 2016;20(5):1097–107. https://doi.org/10.1007/s10461-015-1254-0.
Wisepill Technologies. Real time adherence management. (Accessed November 18, 2017 at https://www.wisepill.com/).
Haberer JE, Musiimenta A, Atukunda EC, Musinguzi N, Wyatt MA, Ware NC, et al. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30(8):1295–300. https://doi.org/10.1097/QAD.0000000000001021.
Sabin LL, Bachman DeSilva M, Gill CJ, Zhong L, Vian T, Xie W, et al. Improving adherence to antiretroviral therapy with triggered real-time text message reminders: the China adherence through technology study. J Acquir Immune Defic Syndr. 2015;69(5):551–9. https://doi.org/10.1097/QAI.0000000000000651.
Orrell C, Cohen K, Mauff K, Bangsberg DR, Maartens G, Wood R. A randomized controlled trial of real-time electronic adherence monitoring with text message dosing reminders in people starting first-line antiretroviral therapy. J Acquir Immune Defic Syndr. 2015;70(5):495–502. https://doi.org/10.1097/QAI.0000000000000770.
Protecting households on exposure to newly diagnosed index multidrug-resistant TB patients. Available at http://impaactnetwork.org/studies/IMPAACT2003B.asp Accessed 7 Nov 2017.
Gandhi M, Team iS, Glidden DV, Team iS, Liu A, Team iS et al. Strong correlation between concentrations of tenofovir (TFV) emtricitabine (FTC) in hair and TFV diphosphate and FTC triphosphate in dried blood spots in the iPrEx open label extension: implications for pre-exposure prophylaxis adherence monitoring. J Infect Dis 2015;212(9):1402–1406, DOI: https://doi.org/10.1093/infdis/jiv239.
Abaasa A, Hendrix C, Gandhi M, Anderson P, Kamali A, Kibengo F et al. Utility of different adherence measures for PrEP: patterns and incremental value. AIDS Behav. 2017:1–9.
Kanters S, Park JJ, Chan K, Socias ME, Ford N, Forrest JI, et al. Interventions to improve adherence to antiretroviral therapy: a systematic review and network meta-analysis. Lancet HIV. 2017;4(1):e31–40. https://doi.org/10.1016/S2352-3018(16)30206-5.
Gwadz M, Cleland CM, Applegate E, Belkin M, Gandhi M, Salomon N, et al. Behavioral intervention improves treatment outcomes among HIV-infected individuals who have delayed, declined, or discontinued antiretroviral therapy: a randomized controlled trial of a novel intervention. AIDS Behav. 2015;19(10):1801–17. https://doi.org/10.1007/s10461-015-1054-6.
Hickey MD, Salmen CR, Omollo D, Mattah B, Fiorella KJ, Geng EH, et al. Implementation and operational research: pulling the network together: quasiexperimental trial of a patient-defined support network intervention for promoting engagement in HIV care and medication adherence on Mfangano Island, Kenya. J Acquir Immune Defic Syndr. 2015;69(4):e127–34. https://doi.org/10.1097/QAI.0000000000000664.
Golub SA, Pena S, Hilley A, Pachankis J, Radix A. Brief behavioral intervention increases PrEP drug levels in a real-world setting. Poster Presented at CROI 2017 Seattle, WA Abstract 965.
Li JZ, Gallien S, Ribaudo H, Heisey A, Bangsberg DR, Kuritzkes DR. Incomplete adherence to antiretroviral therapy is associated with higher levels of residual HIV-1 viremia. AIDS. 2014;28(2):181–6. https://doi.org/10.1097/QAD.0000000000000123.
Podsadecki TJ, Vrijens BC, Tousset EP, Rode RA, Hanna GJ. Decreased adherence to antiretroviral therapy observed prior to transient human immunodeficiency virus type 1 viremia. J Infect Dis. 2007;196(12):1773–8. https://doi.org/10.1086/523704.
Castillo-Mancilla JR, Brown TT, Erlandson KM, Palella FJ Jr, Gardner EM, Macatangay BJ, et al. Suboptimal adherence to combination antiretroviral therapy is associated with higher levels of inflammation despite HIV suppression. Clin Infect Dis. 2016;63(12):1661–7. https://doi.org/10.1093/cid/ciw650.
Castillo-Mancilla JR, Morrow M, Boum Y, Byakwaga H, Haberer JE, Martin JN et al. Higher Art adherence is associated with lower systemic inflammation in treatment-naïve Ugandans who achieve virologic suppression. J Acquir Immune Defic Syndr. 2018. https://doi.org/10.1097/QAI.0000000000001629.
Castillo-Mancilla JR, Phillips AN, Neaton JD, Neuhaus J, Collins S, Mannheimer S, et al. Association of Suboptimal Antiretroviral Therapy Adherence With Inflammation in Virologically Suppressed Individuals Enrolled in the SMART Study. Open Forum Infect Dis. 2017 Dec 22;5(1):ofx275. https://doi.org/10.1093/ofid/ofx275.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jose R. Castillo-Mancilla reports grants K23AI104315 and R21AI124859 from NIH. Jessica E. Haberer reports grants from NIH, Gates Foundation, USAID; has served as a consultant for NIH, Merck, and WHO; and has received stock from Natera.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on HIV Pathogenesis and Treatment
Rights and permissions
About this article
Cite this article
Castillo-Mancilla, J.R., Haberer, J.E. Adherence Measurements in HIV: New Advancements in Pharmacologic Methods and Real-Time Monitoring. Curr HIV/AIDS Rep 15, 49–59 (2018). https://doi.org/10.1007/s11904-018-0377-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-018-0377-0