Abstract
Purpose of Review
Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease characterized by inflammation and fibrosis of the biliary ducts associated with a high risk for hepatobiliary malignancies. Up to 50% of PSC patients develop dominant strictures (DS) and warrant investigations to exclude cholangiocarcinoma (CCA). Most patients undergo endoscopic retrograde cholangiopancreatography (ERCP) with brush cytology, but diagnostic accuracy is suboptimal, with sensitivity varying between 8 and 43% for the detection of CCA. Negative brush cytology often results in repeat ERCPs and need for heightened surveillance.
Recent Findings
The relatively recent introduction of per oral single operator cholangioscopy (SOC) as a safe and efficient complementary tool to ERCP allows for visual characterization and direct targeted forceps biopsy acquisition, with some studies showing sensitivity of up to 90% for overall diagnostic performance. However, most of the data for SOC in PSC comes from retrospective single-center studies.
Summary
SOC allows visual characterization and direct targeted biopsies, with some studies demonstrating superior diagnostic performance for CCA detection in PSC. In addition, SOC may have potential benefit in characterization of different phenotypes of DS in PSC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary sclerosing cholangitis (PSC) is a sporadic, inflammatory condition described by multifocal biliary duct strictures that can lead to chronic liver disease. PSC has a male preponderance and a substantial proportion of affected patients has concomitant inflammatory bowel disease (IBD), either ulcerative colitis or Crohn’s disease [1, 2]. PSC is considered an autoimmune disease; however, the pathogenesis of PSC has not been entirely elucidated and is assumed to be related to a blend of genetic risk factors and environmental triggers [1, 2]. The prevalence is approximately 4–16/100,000 people, and distribution varies according to the geographic area, with the highest frequency described in northern Europe and the lowest in Asia [3,4,5].
Unfortunately, no effective treatment for PSC exists, and the reported median time from diagnosis until the need for liver transplantation (LT) or liver-related death is approximately 13 and 21 years in transplant and community centers, respectively [6]. Several clinical factors have been associated with prognosis. In the largest global cohort of PSC patients, diagnosis at older age was related to a lower LT-free survival, while female sex, presence of Crohn’s disease compared to ulcerative colitis, and small duct PSC compared to classical PSC were associated with a better outcome [7].
As PSC is a heterogeneous disease and its natural history is not similar to other chronic liver diseases, detailed prognostic models have been established. In 2000, the Mayo Clinic established a score integrating bilirubin, age, AST, and albumin as well as variceal bleeding history and patients were classified into three groups as low, intermediate, and high risk for disease progression [8].
More recently, risk estimation tools have been developed using machine learning that demonstrated accurate prediction for decompensation, including the PSC estimate tool (PREsTo) and the United Kingdom (UK-PSC) Risk Scores [9, 10].
Dominant Strictures and Cholangiocarcinoma in PSC
More than half of the patients with PSC develop high-grade or dominant strictures (DS) of the bile ducts during the course of their disease. DS can either represent worsening of the underlying inflammatory response or the progression to malignancy. Development of a DS, therefore, significantly complicates the management of this disease, since precise diagnosis of these indeterminate biliary strictures becomes a difficult clinical task.
Dominant strictures are characterized as a stenosis with a diameter of ≤ 1.5 mm in the common bile duct and/or ≤ 1.0 mm in the right or left hepatic duct within 2 cm of the main hepatic confluence. The investigation for the etiology of DS is pivotal, as PSC is related to 400-fold higher risk of cholangiocarcinoma (CCA) in comparison to the general population [6]. In fact, the yearly risk for CCA in PSC is estimated at 2%, with a cumulative incidence from 6 to 11% at 10 years, and up to 20% at 30 years [6]. Interestingly, the cancer risk in PSC seems to be variable over time, as 27–37% of all the hepatobiliary cancers are detected in the first year of PSC diagnosis [11].
A recent retrospective study evaluating almost 2400 cases of CCA in different anatomical locations (1169 intrahepatic, 995 perihilar, and 231 distal) demonstrated a reverse association between the use of aspirin and the risk of all CCA subtypes, with adjusted odds ratios (AORs) ranging from 0.29 to 0.35 for different anatomical locations (P < 0.001 for all). Association between PSC and the peri-hilar subtype (AOR = 453, 95% CI 104–999), was stronger than the association with intrahepatic (AOR = 93.4, 95% CI 27.1–322) or distal (AOR = 34.0, 95% CI 3.6–323) CCA [12•].
According to the American Association for Gastroenterology (AGA) practice guidelines, patients with PSC and DS should be investigated for CCA using biliary ductal sampling with endoscopic retrograde cholangiopancreatography (ERCP) and simple brush cytology, possibly with the addition of other procedures such as fluorescence in situ hybridization (FISH), and/or the use of per oral single operator cholangioscopy (SOC) with direct targeted biopsies [13••]. Detection rates for CCA with current techniques are suboptimal and negative brush cytology results in the need for close monitoring of these DS. Routine brush cytology obtained with ERCP has demonstrated a wide range of diagnostic performance, with sensitivities ranging between 8 and 43% for the detection of CCA when suspicious results were considered as positive. On the other hand, the reported specificity has been as high as 97% [14, 15]. The addition of sophisticated techniques, including fluorescence in situ hybridization (FISH) and digital image analysis (DIA), has demonstrated an improvement in the sensitivity of CCA detection by 10–15% [16,17,18,19]. However, these techniques are not accessible in many centers, and some patients with negative results will require several ERCPs when CCA suspicion remains high. In fact, up to 20% of DS end up being classified as indeterminate after multiple ERCPs with brush cytology [20].
It should be emphasized that in patients with PSC, the opportune identification of CCA within a biliary stricture is fundamental for management and has a significant impact on clinical outcomes. Prompt identification of CCA is critical in order to enable timely curative surgical resection in patients with preserved liver function but for a majority of patients, the detection of CCA would be a contraindication for LT unless centers have access for special treatment protocols for LT in the setting of perihilar CCA [21].
Effectiveness of Cholangioscopy in PSC
Cholangioscopy is an endoscopic technique used not only for direct visual characterization of the bile duct but also to acquire direct targeted biopsy forceps for diagnostic evaluation of biliary lesions, and if needed, for therapeutic intervention within the bile ducts. Cholangioscopy has recently been transformed by the introduction of a system enabling a single endoscopist to perform the entire procedure. This single-operator cholangioscopy (SOC) system is a significant improvement over the previous 2-endoscopist system using a “mother-daughter” cholangioscope [22, 23]. In SOC, the cholangioscope is attached to the handle of a conventional duodenoscope and the procedure is completed concurrent with ERCP. Improvements in the optical image quality and in the accessories, such as biopsy forceps, that can be used through this system have significantly enhanced the diagnostic capability of ERCP.
Detection of Cholangiocarcinoma with Cholangioscopy
It has been reported that SOC improves the diagnostic precision of ERCP for indeterminate biliary strictures [24, 25]. A systematic review and meta-analysis, including eight studies involving 335 patients, confirmed that the overall diagnostic performance of SOC visual impression had a sensitivity of 90% (95% CI, 73%–97%), and specificity of 87% (95% CI, 76–94%). However, the sensitivity for histological diagnosis with biopsy forceps was 69% (95% CI, 57–79%) and specificity of 98% (95% CI, 92–99%) [26].
Another systematic review of 10 studies with 456 patients reported sensitivity of 60.1% (95% CI 54.9–65.2%) and specificity of 98.0% (95% CI, 96.0–99.0%) for SOC-guided biopsies [24]. These studies suggest that visual impression might have better diagnostic performance than targeted biopsies, but the concern is that in most centers, surgical/oncologic treatment is difficult to recommend without a corroborating tissue diagnosis.
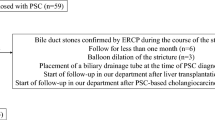
In the case of PSC, the diagnostic performance of SOC-targeted biopsies has been inconstant, with studies indicating sensitivities as low as 33% for the diagnosis of CCA (Table 1) [27, 31, 36]. In a systematic review and meta-analysis of 49 studies, the overall estimated accuracy of SOC for a visual diagnosis was 89% (95% CI 84–93%) while it was 79% (95% CI 74–84%) for a histological diagnosis, with the estimated overall adverse event rate of 7% (95% CI 6–9%) [37]. Nonetheless, there is evidence to suggest that SOC is still the most precise diagnostic procedure for the diagnosis of CCA in PSC [31•]. Furthermore, Arnelo et al. demonstrated the ability of SOC to acquire targeted biopsies from biliary strictures not accessible with conventional ERCP [31]. Even though some centers suggest a step-up approach for the detection of CCA in PSC [32••], we feel that SOC should be considered earlier in this diagnostic algorithm as having a diagnosis in a timely manner is critical for management (Fig. 1).
A more recent study evaluating the performance features of SOC-guided biopsies and transpapillary biopsies with regular sampling methods for the diagnosis of CCA demonstrated that sensitivity for the detection of CCA was improved using SOC-guided and transpapillary biopsies in combination with other ERCP-based procedures when compared to only brush cytology alone. Although SOC was harmless, these procedures do not considerably increase the sensitivity for the diagnosis of malignancy in PSC [34].
Similar results were reported in a single-center retrospective of patients who received SOC for the assessment of indeterminate biliary strictures. Eighty patients were evaluated and 40% had PSC, and more than 80% had prior ERCP. Sensitivity and specificity for visual impression was 64 and 62% and for targeted biopsies was 15 and 65% respectively [38]. In addition, for 32% of patients, SOC results did not change management; in 51%, results confirmed the previous diagnosis; and in 17%, SOC results changed the management plan [38].
Newly, high-resolution per-oral video cholangioscopy allowed to visualize tumor margins in CCA in comparison with traditional fluoroscopy-based ERCP, with 48% increase in dubious lesions biopsied with narrow band imaging compared with white-light imaging; however, an enhancement in dysplasia detection in PSC was not established [39]. An additional advantage of SOC, however, is its ability to distinguish PSC from other stricturing biliary diseases such as IgG4-associatied cholangitis [40].
There are also some limitations with SOC. Despite similar accuracy for cancer diagnosis in PSC and patients with single biliary strictures, the inability to traverse strictures with the cholangioscope and incidence of cholangitis post-SOC seems to be more prevalent in patients with PSC (15 versus 2%; P = 0.051) [41].
We acknowledge limitations and discrepancies in the evidence behind current guidelines and recommend that additional data are required to elucidate the role of SOC in PSC.
Endoscopic Treatment of Dominant Strictures
The development of DS in PSC patients has been related to worse long-term outcomes, mainly related to the fact that a substantial percentage of DS has an underlying CCA [42]. Chapman et al. describe their 25-year experience in 128 patients with PSC and found that there was a 26% risk of developing CCA only in those with a DS, and a shorter survival was observed in this group compared to those without a DS (14 versus 23 years) [43].
In the presence of DS not related to CCA, treatment with endoscopic balloon dilatation is recommended, preferably without plastic stent insertion [44,45,46]. Baluyut et al. demonstrated that the 5-year survival rate of patients with a DS who underwent endoscopic balloon dilatation was superior to the prediction by the Mayo Risk Score (83% versus 65%, P = 0.027) [47]. Gluck et al. presenting their 20-year practice with endoscopic therapy for 84 symptomatic PSC patients also found that survival was higher than expected [48].
Short-term stenting was compared to the balloon dilatation for a DS in a more recent multicentre randomized trial and no differences in outcome measures between the 2 groups, but adverse events, consisting primarily of post-ERCP pancreatitis and suppurative cholangitis, were more common in patients that underwent short-term stenting (42 versus 10%, OR 6.4, 95% CI 1.6–25.4) [44].
Recently, a large retrospective study evaluated 286 patients of whom 133 (47.5%) underwent arranged ERCP and the rest received on-demand ERCP. At 10 years follow-up, higher rate of LT-free survival was observed in patients who underwent scheduled ERCP (51 versus 29.3%; P < 0.001). Results of this study recommend that regular ERCP with balloon dilatation considerably benefits PSC patients with a DS, detected both at early presentation and throughout surveillance, even if patients are asymptomatic [49].
For those patients with a failed ERCP, percutaneous transhepatic biliary access is an alternative treatment option [2].
Detection and Removal of Stones
Biliary stones constitute another indication for endoscopic biliary intervention in PSC patients. In a retrospective study of more than 100 patients with PSC, approximately 50% of patients who received ERCP had biliary stones [48]. Extrahepatic bile duct stones are fairly frequent in the general population, whereas intrahepatic bile duct stones are unusual. In patients with PSC, both occur relatively frequently [50].
One of the earlier experiences of SOC in PSC demonstrated that stones identified by cholangioscopy were not detected by cholangiography in 30% of patients, and SOC-directed lithotripsy might be better than conventional ERCP for reaching comprehensive stone clearance [36]. A more recent study similarly demonstrated that residual biliary stones could be found with SOC in 34% of cases missed by occlusion cholangiography in patients with dilated bile ducts and in those receiving lithotripsy [51]. In a systematic review and meta-analysis that comprised 49 studies, the overall predicted stone clearance rate was 88% (95% CI 85–91%) [37].
Adverse Events Associated with SOC
The use of SOC has been linked to the elevated risk of cholangitis and bacteremia, possibly related to longer procedure time, increased intraluminal pressure from irrigation, and insufflation within the bile duct causing bacterial translocation [52]. In a prospective experience, SOC was associated with a bacteremia and cholangitis rate of 8.8% and 7.0%, respectively [53].
Prior to the cholangioscopy, pre-procedural antibiotics may be used particularly if tissue harvesting with biopsy sampling is required [54]. Antibiotics recommended are ciprofloxacin 500 mg orally given within 60 to 90 min before procedure (or 400 mg IV over 60 min beginning within 120 min before procedure), or amoxicillin-clavulanate 1750 mg orally within 60 min prior to procedure, or ampicillin-sulbactam 3 g IV within 60 min prior to procedure [55].
Cholangioscopy Classification of PSC and Potential Prognostic Significance
PSC is a diverse disease, with an extensive variety of disease phenotypes. A cholangiography-based classification has been demonstrated to correlate with clinical outcomes in PSC [56]. A recent classification, not specific for PSC, proposed a system using a new set of descriptions which, in a single-centered non-randomized study, seemed to advance performance for malignancy detection, with a sensitivity of 96%, specificity of 92%, with a PPV and NPV of 93% and 96%, respectively [57]. Edmonton Classification has been proposed by our group to stratify PSC patients with extrahepatic dominant strictures according to the phenotypic expression differences seen on cholangioscopy (Table 2) [35]. However, the clinical efficacy of these classification systems needs to be identified. Similar to patients with IBD, it is tempting to consider that SOC could benefit from routine screening strategies and early detection of premalignant biliary lesion that might indicate surgical resection or LT [58]; nevertheless, the feasibility of such strategies has yet to be established.
Conclusions
In summary, up to 50% of PSC patients develop DS during the evaluation of their disease. All DS should be investigated as PSC carries a significant risk for CCA. ERCP with brushing cytology is performed in most centers, but diagnostic accuracy is suboptimal despite inclusion of techniques such as FISH or DIA. SOC is a safe and efficient adjunctive tool with ERCP that allows for visual characterization and direct targeted biopsies, with studies demonstrating superior diagnostic performance. In addition, SOC could be useful for potential characterization of different phenotypes and treatment of residual bile duct stones in PSC. Most of the data for SOC in PSC comes from retrospective single-center studies analyzing heterogeneous cohorts without standardized protocols. As we still have an unmet need for appropriate diagnosis of CCA in PSC, additional prospective and multicenter studies are warranted to clarify the role of SOC in PSC.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lazaridis KN, LaRusso NF. Primary sclerosing cholangitis. N Engl J Med. 2016;375:1161–70. https://doi.org/10.1056/NEJMra1506330.
Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis - a comprehensive review. J Hepatol. 2017;67:1298–323. https://doi.org/10.1016/j.jhep.2017.07.022.
Dyson JK, Beuers U, Jones DEJ, Lohse AW, Hudson M. Primary sclerosing cholangitis. Lancet. 2018;39:2547–59. https://doi.org/10.1016/S0140-6736(18)30300-3.
Bambha K, Kim WR, Talwalkar J, Torgerson H, Benson JT, Therneau TM, et al. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology. 2003;125:1364–9. https://doi.org/10.1016/j.gastro.2003.07.011.
Lindkvist B, de Benito Valle M, Gullberg B, Bjornsson E. Incidence and prevalence of primary sclerosing cholangitis in a defined adult population in Sweden. Hepatology. 2010;52:571–7. https://doi.org/10.1002/hep.23678.
Boonstra K, Weersma RK, van Erpecum KJ, Rauws EA, Spanier BW, Poen AC, et al. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology. 2013;58:2045–55. https://doi.org/10.1002/hep.26565.
Weismuller TJ, Trivedi PJ, Bergquist A, Imam M, Lenzen H, Ponsioen CY, et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology. 2017;152:1975–84 e8. https://doi.org/10.1053/j.gastro.2017.02.038.
Kim WR, Poterucha JJ, Wiesner RH, LaRusso NF, Lindor KD, Petz J, et al. The relative role of the Child-Pugh classification and the Mayo natural history model in the assessment of survival in patients with primary sclerosing cholangitis. Hepatology. 1999;29:1643–8. https://doi.org/10.1002/hep.510290607.
Eaton JE, Vesterhus M, McCauley BM, Atkinson EJ, Schlicht EM, Juran BD, et al. Primary sclerosing cholangitis risk estimate tool (PREsTo) predicts outcomes of the disease: a derivation and validation study using machine learning. Hepatology. 2020;71(1):214–24. https://doi.org/10.1002/hep.30085.
Goode EC, Clark AB, Mells GF, Srivastava B, Spiess K, Gelson WTH, et al. Factors associated with outcomes of patients with primary sclerosing cholangitis and development and validation of a risk scoring system. Hepatology. 2019;69:2120–35. https://doi.org/10.1002/hep.30479.
Bergquist A, Ekbom A, Olsson R, Kornfeldt D, Loof L, Danielsson A, et al. Hepatic and extrahepatic malignancies in primary sclerosing cholangitis. J Hepatol. 2002;36:321–7. https://doi.org/10.1016/s0168-8278(01)00288-4.
• Choi JG, Ghoz HM, Peeraphatdit T, Baichoo E, Addissie BD, Harmsen WS, et al. Aspirin use and the risk of cholangiocarcinoma. Hepatology. 2016;64:785–96. https://doi.org/10.1002/hep.28529This is an interesting case-control study showing that aspirin use might decrease the risk of cholangiocarcinoma.
•• Bowlus CL, Lim JK, Lindor KD. AGA clinical practice update on surveillance for hepatobiliary cancers in patients with primary sclerosing cholangitis: expert review. Clin Gastroenterol Hepatol. 2019;17:2416–22. https://doi.org/10.1016/j.cgh.2019.07.011These manuscript provides practical guidelines for screening of hepatobiliary malignancies in primary sclerosing cholangitis.
Korc P, Sherman S. ERCP tissue sampling. Gastrointest Endosc. 2016;84:557–71. https://doi.org/10.1016/j.gie.2016.04.039.
Kipp BR, Stadheim LM, Halling SA, Pochron NL, Harmsen S, Nagorney DM, et al. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. Am J Gastroenterol. 2004;99:1675–81. https://doi.org/10.1111/j.1572-0241.2004.30281.x.
Barr Fritcher EG, Voss JS, Brankley SM, Campion MB, Jenkins SM, Keeney ME, et al. An optimized set of fluorescence in situ hybridization probes for detection of Pancreatobiliary tract cancer in cytology brush samples. Gastroenterology. 2015;149:1813–24 e1. https://doi.org/10.1053/j.gastro.2015.08.046.
Smoczynski M, Jablonska A, Matyskiel A, Lakomy J, Dubowik M, Marek I, et al. Routine brush cytology and fluorescence in situ hybridization for assessment of pancreatobiliary strictures. Gastrointest Endosc. 2012;75:65–73. https://doi.org/10.1016/j.gie.2011.08.040.
Moreno Luna LE, Gores GJ. Advances in the diagnosis of cholangiocarcinoma in patients with primary sclerosing cholangitis. Liver Transpl. 2006;12:S15–9. https://doi.org/10.1002/lt.20938.
Moreno Luna LE, Kipp B, Halling KC, Sebo TJ, Kremers WK, Roberts LR, et al. Advanced cytologic techniques for the detection of malignant pancreatobiliary strictures. Gastroenterology. 2006;131:1064–72. https://doi.org/10.1053/j.gastro.2006.08.021.
Bowlus CL, Olson KA, Gershwin ME. Evaluation of indeterminate biliary strictures. Nat Rev Gastroenterol Hepatol. 2016;13:28–37. https://doi.org/10.1038/nrgastro.2015.182.
Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010;23:692–7. https://doi.org/10.1111/j.1432-2277.2010.01108.x.
Chen YK. Preclinical characterization of the Spyglass peroral cholangiopancreatoscopy system for direct access, visualization, and biopsy. Gastrointest Endosc. 2007;65:303–11. https://doi.org/10.1016/j.gie.2006.07.048.
Pereira P, Peixoto A, Andrade P, Macedo G. Peroral cholangiopancreatoscopy with the SpyGlass(R) system: what do we know 10 years later. J Gastrointestin Liver Dis. 2017;26:165–70. https://doi.org/10.15403/jgld.2014.1121.262.cho.
Navaneethan U, Hasan MK, Lourdusamy V, Njei B, Varadarajulu S, Hawes RH. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: a systematic review. Gastrointest Endosc. 2015;82:608–14.e2. https://doi.org/10.1016/j.gie.2015.04.030.
Nanda A, Brown JM, Berger SH, Lewis MM, Fritcher EGB, Gores GJ, et al. Triple modality testing by endoscopic retrograde cholangiopancreatography for the diagnosis of cholangiocarcinoma. Ther Adv Gastroenter. 2015;8:56–65. https://doi.org/10.1177/1756283x14564674.
Sun X, Zhou ZR, Tian JM, Wang ZQ, Huang QY, Fan KC, et al. Is single-operator peroral cholangioscopy a useful tool for the diagnosis of indeterminate biliary lesion? A systematic review and meta-analysis. Gastrointest Endosc. 2015;82:79–87. https://doi.org/10.1016/j.gie.2014.12.021.
Tischendorf JJW, Kruger M, Trautwein C, Duckstein N, Schneider A, Manns MP, et al. Cholangioscopic characterization of dominant bile duct stenoses in patients with primary sclerosing cholangitis. Endoscopy. 2006;38:665–9. https://doi.org/10.1055/s-2006-925257.
Siiki A, Rinta-Kiikka I, Koivisto T, Vasama K, Sand J, Laukkarinen J. Spyglass single-operator peroral cholangioscopy seems promising in the evaluation of primary sclerosing cholangitis-related biliary strictures. Scand J Gastroenterol. 2014;49:1385–90. https://doi.org/10.3109/00365521.2014.940376.
Liu R, Cox Rn K, Siddiqui A, Feurer M, Baron T, Adler DG. Peroral cholangioscopy facilitates targeted tissue acquisition in patients with suspected cholangiocarcinoma. Minerva Gastroenterol Dietol. 2014;60:127–33.
Rey JW, Hansen T, Dumcke S, Tresch A, Kramer K, Galle PR, et al. Efficacy of SpyGlass(TM)-directed biopsy compared to brush cytology in obtaining adequate tissue for diagnosis in patients with biliary strictures. World J Gastrointest Endosc. 2014;6:137–43. https://doi.org/10.4253/wjge.v6.i4.137.
Arnelo U, von Seth E, Bergquist A. Prospective evaluation of the clinical utility of single-operator peroral cholangioscopy in patients with primary sclerosing cholangitis. Endoscopy. 2015;47:696–702. https://doi.org/10.1055/s-0034-1391845.
• Njei B, TR MC, Varadarajulu S, Navaneethan U. Systematic review with meta-analysis: endoscopic retrograde cholangiopancreatography-based modalities for the diagnosis of cholangiocarcinoma in primary sclerosing cholangitis. Aliment Pharmacol Ther. 2016;44:1139–51. https://doi.org/10.1111/apt.13817This is the largest meta-analysis indicating that single-operator cholangioscopy with targeted biopsies seems to be the most precise ERCP-based modality for cholangiocarcinoma diagnosing compared to the other modalities in primary sclerosing cholangitis.
•• Majeed A, Castedal M, Arnelo U, Soderdahl G, Bergquist A, Said K. Optimizing the detection of biliary dysplasia in primary sclerosing cholangitis before liver transplantation. Scand J Gastroenterol. 2018;53:56–63. https://doi.org/10.1080/00365521.2017.1385840This is the largest study showing that single-operator cholangioscopy for targeted examination at the second ERCP significantly improved sensitivity and specificity.
Kaura K, Sawas T, Bazerbachi F, Storm AC, Martin JA, Gores GJ, et al. Cholangioscopy biopsies improve detection of cholangiocarcinoma when combined with cytology and FISH, but not in patients with PSC. Dig Dis Sci. 2019:1–8. https://doi.org/10.1007/s10620-019-05866-2.
Sandha G, D'Souza P, Halloran B, Montano-Loza AJ. A cholangioscopy-based novel classification system for the phenotypic stratification of dominant bile duct strictures in primary sclerosing cholangitis-the Edmonton Classification. J Can Assoc Gastroenterol. 2018;1:174–80. https://doi.org/10.1093/jcag/gwy020.
Awadallah NS, Chen YK, Piraka C, Antillon MR, Shah RJ. Is there a role for cholangioscopy in patients with primary sclerosing cholangitis? Am J Gastroenterol. 2006;101:284–91. https://doi.org/10.1111/j.1572-0241.2006.00383.x.
Korrapati P, Ciolino J, Wani S, Shah J, Watson R, Muthusamy VR, et al. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E263–75. https://doi.org/10.1055/s-0042-100194.
de Vries AB, van der Heide F, Ter Steege RWF, Koornstra JJ, Buddingh KT, Gouw ASH, et al. Limited diagnostic accuracy and clinical impact of single-operator peroral cholangioscopy for indeterminate biliary strictures. Endoscopy. 2019. https://doi.org/10.1055/a-1061-7067.
Azeem N, Gostout CJ, Knipschield M, Baron TH. Cholangioscopy with narrow-band imaging in patients with primary sclerosing cholangitis undergoing ERCP. Gastrointest Endosc. 2014;79:773–9 e2. https://doi.org/10.1016/j.gie.2013.09.017.
Nakazawa T, Naitoh I, Hayashi K, Miyabe K, Simizu S, Joh T. Diagnosis of IgG4-related sclerosing cholangitis. World J Gastroenterol. 2013;19:7661–70. https://doi.org/10.3748/wjg.v19.i43.7661.
Kalaitzakis E, Sturgess R, Kaltsidis H, Oppong K, Lekharaju V, Bergenzaun P, et al. Diagnostic utility of single-user peroral cholangioscopy in sclerosing cholangitis. Scand J Gastroenterol. 2014;49:1237–44. https://doi.org/10.3109/00365521.2014.936032.
Tischendorf JJW, Hecker H, Kruger M, Manns MP, Meier PN. Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: a single center study. Am J Gastroenterol. 2007;102:107–14. https://doi.org/10.1111/j.1572-0241.2006.00872.x.
Chapman MH, Webster GJ, Bannoo S, Johnson GJ, Wittmann J, Pereira SP. Cholangiocarcinoma and dominant strictures in patients with primary sclerosing cholangitis: a 25-year single-centre experience. Eur J Gastroenterol Hepatol. 2012;24:1051–8. https://doi.org/10.1097/MEG.0b013e3283554bbf.
Ponsioen CY, Arnelo U, Bergquist A, Rauws EA, Paulsen V, Cantu P, et al. No superiority of stents vs balloon dilatation for dominant strictures in patients with primary Sclerosing cholangitis. Gastroenterology. 2018;155:752–9. https://doi.org/10.1053/j.gastro.2018.05.034.
• Aabakken L, Karlsen TH, Albert J, Arvanitakis M, Chazouilleres O, Dumonceau J-M, et al. Role of endoscopy in primary sclerosing cholangitis: European Society of Gastrointestinal Endoscopy (ESGE) and European Association for the Study of the Liver (EASL) clinical guideline. J Hepatol 2017;66:1265-81 doi:101016/jjhep201702013. This review summarizes the current role of endoscopy in patients with primary sclerosing cholangitis.
Chapman MH, Thorburn D, Hirschfield GM, Webster GGJ, Rushbrook SM, Alexander G, et al. British Society of Gastroenterology and UK-PSC guidelines for the diagnosis and management of primary sclerosing cholangitis. Gut. 2019;68:1356–78. https://doi.org/10.1136/gutjnl-2018-317993.
Baluyut AR, Sherman S, Lehman GA, Hoen H, Chalasani N. Impact of endoscopic therapy on the survival of patients with primary sclerosing cholangitis. Gastrointest Endosc. 2001;53:308–12. https://doi.org/10.1067/mge.2001.112739.
Gluck M, Cantone NR, Brandabur JJ, Patterson DJ, Bredfeldt JE, Kozarek RA. A twenty-year experience with endoscopic therapy for symptomatic primary sclerosing cholangitis. J Clin Gastroenterol. 2008;42:1032–9. https://doi.org/10.1097/MCG.0b013e3181646713.
Rupp C, Hippchen T, Bruckner T, Kloters-Plachky P, Schaible A, Koschny R, et al. Effect of scheduled endoscopic dilatation of dominant strictures on outcome in patients with primary sclerosing cholangitis. Gut. 2019;68:2170–8. https://doi.org/10.1136/gutjnl-2018-316801.
Dodd GD 3rd, Niedzwiecki GA, Campbell WL, Baron RL. Bile duct calculi in patients with primary sclerosing cholangitis. Radiology. 1997;203:443–7. https://doi.org/10.1148/radiology.203.2.9114102.
Sejpal DV, Trindade AJ, Lee C, Miller LS, Benias PC, Inamdar S, et al. Digital cholangioscopy can detect residual biliary stones missed by occlusion cholangiogram in ERCP: a prospective tandem study. Endosc Int Open. 2019;7:E608–E14. https://doi.org/10.1055/a-0842-6450.
Sethi A, Chen YK, Austin GL, Brown WR, Brauer BC, Fukami NN, et al. ERCP with cholangiopancreatoscopy may be associated with higher rates of complications than ERCP alone: a single-center experience. Gastrointest Endosc. 2011;73:251–6. https://doi.org/10.1016/j.gie.2010.08.058.
Othman MO, Guerrero R, Elhanafi S, Davis B, Hernandez J, Houle J, et al. A prospective study of the risk of bacteremia in directed cholangioscopic examination of the common bile duct. Gastrointest Endosc. 2016;83:151–7. https://doi.org/10.1016/j.gie.2015.05.018.
Peiseler M, Reiners D, Pinnschmidt HO, Sebode M, Jung F, Hartl J, et al. Risk of endoscopic biliary interventions in primary sclerosing cholangitis is similar between patients with and without cirrhosis. PLoS One. 2018;13:e0202686. https://doi.org/10.1371/journal.pone.0202686.
Khashab MA, Chithadi KV, Acosta RD, Bruining DH, Chandrasekhara V, Eloubeidi MA, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2015;81:81–9. https://doi.org/10.1016/j.gie.2014.08.008.
Ponsioen CY, Reitsma JB, Boberg KM, Aabakken L, Rauws EA, Schrumpf E. Validation of a cholangiographic prognostic model in primary sclerosing cholangitis. Endoscopy. 2010;42:742–7. https://doi.org/10.1055/s-0030-1255527.
Robles-Medranda C, Valero M, Soria-Alcivar M, Puga-Tejada M, Oleas R, Ospina-Arboleda J, et al. Reliability and accuracy of a novel classification system using peroral cholangioscopy for the diagnosis of bile duct lesions. Endoscopy. 2018;50:1059–70. https://doi.org/10.1055/a-0607-2534.
Boyd S, Vannas M, Jokelainen K, Isoniemi H, Makisalo H, Farkkila MA, et al. Suspicious brush cytology is an indication for liver transplantation evaluation in primary sclerosing cholangitis. World J Gastroenterol. 2017;23:6147–54. https://doi.org/10.3748/wjg.v23.i33.6147.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
A Montano-Loza and M Ebadi declares no conflict of interest.
G Sandha is a consultant for Boston Scientific Corporation and has received honoraria for speaking commitments and advisory board meetings.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Autoimmune, Cholestatic, and Biliary Diseases
Rights and permissions
About this article
Cite this article
Montano-Loza, A.J., Ebadi, M. & Sandha, G. The Role of Cholangioscopy in the Management of Primary Sclerosing Cholangitis. Curr Hepatology Rep 19, 78–85 (2020). https://doi.org/10.1007/s11901-020-00514-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-020-00514-0