Abstract
Purpose of Review
Update current knowledge of the use of hepatic venous pressure gradient (HVPG) as a predictor of clinical events and of efficacy of therapy for portal hypertension.
Recent Findings
HVPG is a good predictor of clinical events. Decrease in HVPG during therapy is accompanied by a decreased incidence of complications from portal hypertension and improved survival.
Summary
HVPG measurements are a valuable tool in the management of portal hypertension in cirrhosis. In addition of detecting and grading the severity of portal hypertension, HVPG measurements provide robust prognostic information on the risk of complications, disease progression/regression, and survival. Changes in HVPG in response to therapy predict the effects on clinical outcomes, both during treatment with beta-blockers and when treating HCV-related cirrhosis with specific antivirals. This has led to suggest that HVPG can be used as a surrogate for clinical events when developing new therapies for portal hypertension. Limitations of this approach are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Portal hypertension (PH) is defined as a pathological increase of portal venous pressure. In normal conditions, the pressure gradient between the portal vein and the hepatic veins, which represents the portal perfusion pressure of the liver, ranges between 1 and 5 mmHg. This gradient, known as the portal pressure gradient (PPG), increases whenever there are obstacles to portal blood flow, resulting in portal hypertension. Not all increases of portal pressure are of clinical relevance; cross-sectional and longitudinal studies have shown that until the PPG does not reach values of 10 mmHg or above there is no risk that portal hypertension is associated with clinical manifestations. On the contrary, above this threshold that defines clinically significant portal hypertension (CSPH), the consequences of portal hypertension may develop. These include formation of portal-systemic collaterals and gastroesophageal varices, gastrointestinal bleeding from ruptured varices or from portal hypertensive gastropathy, ascites, hepatic encephalopathy, hepatorenal and hepatopulmonary syndrome, porto-pulmonary hypertension, and disturbances of the metabolism of endo- and xeno-biotics.
According to the anatomic location of the obstacle to portal blood flow, portal hypertension is classified as pre-hepatic, intrahepatic, or post-hepatic. In developed countries, about 90% of cases of portal hypertension have an intra-hepatic origin and are due to advanced chronic liver diseases, mostly cirrhosis of the liver. This review deals with the specific situation of portal hypertension due to cirrhosis of the liver of non-cholestatic origen.
The HVPG
Direct measurements of portal pressure are invasive, difficult, and carry the risk of causing major complications, as these require puncturing or catheterizing the portal vein via a percutaneous trans-hepatic or trans-splenic access, or a surgical approach, by means of a laparotomy or by re-permeabilizing the remnant of a paraumbilical vein. Because of this, the much safer indirect technique of measuring the hepatic venous pressure gradient (HVPG) at hepatic vein catheterization is the preferred method for measuring the PPG in patients with portal hypertension due to advanced chronic liver disease (ACLD).
The HVPG represents the difference between the “wedged” and “free” hepatic vein pressure at hepatic vein catheterization. The wedged hepatic venous pressure (WHVP) is measured when the lumen of the hepatic vein is occluded by means of a balloon catheter and represents the pressure at the hepatic sinusoids. This is so because when a balloon catheter stops blood flow in a hepatic vein, a static column of blood is formed that transmits the pressure existing in the preceding vascular territory, which in normal livers are the hepatic sinusoids, since intersinusoidal communications make that the pressure transmitted by the occluded column of blood does not reach the portal system [1, 2]. In the cirrhotic liver, formation of septa and nodules disrupts these intersinusoidal communications and makes that the static column of blood extends beyond the sinusoids and transmits the pressure at the portal vein. Therefore, the WHVP represents an accurate estimation of portal pressure in cirrhosis of any etiology, with the exception of PBC and other cholestatic diseases, in which periductular injury at the portal tracts may compress portal venules and cause “pre-sinusoidal” intrahepatic portal hypertension that may be present long before development of histologic cirrhosis. HVPG is obtained by subtracting the free hepatic vein pressure from the WHVP. The “free” hepatic vein pressure is measured after releasing the balloon, with the precaution of having the catheter tip only 2–3 cm inside the hepatic vein, and is usually very close to the inferior vena cava (IVC) pressure. However, in the segment of the IVC where the hepatic veins drain is quite short and close to thoracic part of the IVC, it is more reliable and easier to measure accurately the “free” pressure that the IVC pressure. HVPG accurately reflects the PPG in patients with cirrhosis [1, 3]. Pressure measurements should be performed by triplicate. Permanent tracings should be obtained either in paper or in digital recording systems. The results are given with a precision of 0.5 mmHg, which is the best discrimination accuracy of carefully performed measurements in experienced hands.
Hepatic vein catheterization and measurement of HVPG are invasive techniques, but relatively simple and safe. It is usually performed on an outpatient basis, on fasting conditions and under local anesthesia. Slight sedation with midazolam is optional. However, deep sedation using IV opioids or propofol is not recommended as it is unnecessary in most patients and because it may interfere with accuracy of the measurements [4]. Hepatic vein catherization can be done by the percutaneous puncture of an arm vein, of the internal jugular vein, or of the femoral vein. Femoral vein approach is safer as catheterization of the hepatic vein does not need passing through the heart, which reduced markedly the risk of causing arrythmias, but causes more local discomfort. Transjugular access is most popular as it is very rapid and allows performing a transjugular liver biopsy during the same procedure. Real-time ultrasound guidance reduces markedly the risk of local complications during percutaneous access.
Applications of HVPG Measurements
The HVPG is considered the gold standard technique for determining the portal pressure gradient in cirrhosis. Although it was initially introduced as a diagnostic tool for classifying portal hypertension, subsequently, many studies have validated the HVPG as an accurate prognostic marker in patients with ACLD, and as a useful tool for evaluating the efficacy of drug therapy [3, 5,6,7,8]. Moreover, it has also been proposed that it should be used in trials investigating novel therapies, in which reductions in HVPG could represent a surrogate marker of clinical outcomes [9, 10••, 11••].
Evaluation of the Degree of Liver Fibrosis
Liver fibrosis is one of the primary mechanisms of portal hypertension. Several studies have correlated histopathologic features on liver biopsy with the severity of portal hypertension in patients with ACLD of any etiology. The thickness of fibrous septae and nodule size correlates with the degree of HVPG elevation and can be used as predictors of the presence of CSPH (HVPG ≥ 10 mmHg) [12]. In patients with recurrent hepatitis C after liver transplantation, it has been well established that HVPG significantly correlates with the score of fibrosis [13, 14]. In this scenario, the collagen proportionate area, assessed by computer-assisted morphometric image analysis, was significantly associated with an elevated HVPG (≥ 6 mmHg) [15]. An HVPG ≥ 6 mmHg was more accurate than histological findings to identify patients at risk of disease progression and predict clinical decompensation after liver transplantation for hepatitis C [13].
Stages of Cirrhosis: Prognostic Value of HVPG in Patients with Advanced Chronic Liver Disease
The natural history of ACLD is characterized by an initial, prolonged “compensated” stage where the patient is frequently totally asymptomatic. Mortality while in this stage is low, of 1–3%, and has a median duration over 10 years [16]. This is followed by a “decompensated” stage, defined by the appearance of complications due mainly to portal hypertension, such as variceal bleeding, ascites, and hepatic encephalopathy. Some authors also include jaundice and bacterial infections among the complications defining decompensation although most frequently these complications occur in already decompensated patient.
Development of decompensation therefore indicates that the HVPG is of at least ≥ 10 mmHg (and almost invariably ≥ 12 mmHg). Prognosis after the first complication defining decompensation is much worse, with a 1-year mortality that ranges between 20 and 50%, depending on the specific complication presented and if more than one decompensating event occur simultaneously. Ascites is the more frequent decompensating event, followed by variceal bleeding and clinically overt hepatic encephalopathy. The best prognosis is when variceal bleeding is the only manifestation of decompensation; the worse is when there are several decompensating events [10••, 17].
The bad prognosis associated with decompensation makes it important to define predictors of progression to decompensation while in the compensated stage and predictors of survival in decompensated patients.
Compensated Patients: Baseline HVPG as a Predictor of Decompensation
Multiple studies have validated the HVPG as the primary predictor of the development of gastroesophageal varices, decompensation, and hepatocellular carcinoma (HCC) [5,6,7, 18•]. Long-term longitudinal studies in patients with compensated cirrhosis have shown that a HVPG ≥ 10 mmHg (which defines CSPH) is an independent predictor of the risk of developing gastroesophageal varices [5] and of clinical decompensation (development of ascites, hepatic encephalopathy, or variceal bleeding) [6]. The risk of decompensation in patients with CSPH was of 10% per year, while patients with an HVPG < 10 mmHg had a 90% probability of not developing clinical decompensation over a 4-year follow-up [6]. Furthermore, a 10% reduction in HVPG was associated with a decreased risk of developing gastroesophageal varices [5]. On the contrary, it has been shown that for every 1 mmHg increase in HVPG, the risk of decompensation increases by 11% [6]. More recently, HVPG has been confirmed to be a good prognostic indicator in patients with liver cirrhosis due to NASH [19•].
In compensated patients, mortality is also associated with an HVPG > 10 mmHg [20]. More specifically, many studies have demonstrated that mortality increases markedly in patients with a HVPG above 16 mmHg [21, 22, 23•, 24].
Together with HVPG, albumin and body mass index (BMI) were also independent predictors of decompensation [25]. HVPG and albumin were more robust predictors of decompensation than MELD score in a retrospective study in compensated cirrhosis due to hepatitis C virus infection (HCV) [26]. This was further confirmed in a study showing that HVPG measured before starting treatment for HCV (pegylated interferon alpha-2a plus ribavirin) was the strongest predictor of decompensation and liver transplant-free survival [27]. In patients with recurrent HCV infection after liver transplantation, the HVPG 1 year after liver transplant was a better predictor of disease progression and of decompensation than histology and serum markers [13].
Decompensated Patients: HVPG as a Predictor of Death
Several studies have shown that a HVPG above 16 mmHg is the better cutoff to predict mortality [21, 23•]. In patients studied during acute variceal bleeding, an HVPG ≥ 20 mmHg is the strongest independent predictor of failure to control the bleeding, early rebleeding, and mortality [28, 29]. Patients with acute alcoholic hepatitis that have an HVPG over 22 mmHg at the time of transjugular liver biopsy have an increased risk of death [30, 31].
Prognostic Value of Changes in HVPG in during the Treatment of Portal Hypertension
As mentioned above, once HVPG reaches values of at least 10 mmHg portal-systemic collaterals, gastroesophageal varices may start developing [5]. This is accompanied by the development of splanchnic vasodilatation and hyperdynamic circulation [32••]. Splanchnic vasodilatation increases the portal-collateral blood flow, contributes to aggravate the portal hypertension in ACLD, and is the target for treatments for portal hypertension such as non-selective beta-blockers (NSBBs: propranolol, nadolol, timolol, carvedilol), vasopressin, somatostatin, and its derivatives [33•].
Many studies have shown that varices do not bleed until the HVPG has reached a minimal threshold of 12 mmHg [34,35,36,37]. Furthermore, reduction of HVPG to values ≤ 12 mmHg is totally protected from variceal bleeding in a prospective study [38]. Moreover, a reduction of the HVPG equal or greater than 20% of the baseline value is associated with a marked decrease of the risk of first variceal bleeding and of rebleeding [34, 35, 39,40,41,42]. Because of that, patients achieving a reduction of HVPG of at least 20% of baseline values, or ≤ 12 mmHg, have been named “hemodynamic responders.” Several studies and meta-analysis have shown that the clinical benefit of achieving a hemodynamic “response” is not limited to a reduced risk of variceal bleeding/rebleeding but that it extends to a lower incidence of ascites, spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, hepatic encephalopathy, and death during the follow-up [16, 39, 42, 43]. Studies limited to groups of mostly compensated patients receiving NSBBs for the prevention of first bleeding suggest that in them, the criteria for hemodynamic response can be less stringent, a fall of ≥ 10% of baseline or below 12 mmHg being already associated with lower risk of first variceal bleeding or SBP [42, 43]. A simplification of the assessment of the hemodynamic response is to verify the decrease in HVPG 15 min after IV propranolol administration (0.15 mg/kg), a decrease of ≥ 10% of baseline or to values ≤ 12 mmHg being associated to decreased risk of bleeding and death during the follow-up [44, 45].
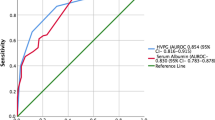
The relevance of HVPG in evaluating the effectiveness of therapy for portal hypertension has been demonstrated in several meta-analyses [46, 47]. In a recent meta-analysis, the proportion of patients achieving a good hemodynamic response was 50.9%. The occurrence of bleeding was 3.8% in responders and 27.8% in non-responders [48]. Similar data was shown in a previous meta-analysis, where the risk for bleeding was 6% for responders and 32% in non-responders [46]. Importantly, the benefit of NSBBs is independent of the presence of ascites and hepatic function [49].
Carvedilol is a NSBB with anti-alpha1-adrenergic activity that has been shown to be more potent than propranolol decreasing portal pressure, thus increasing the number of responder patients [50, 51]. A recent study including 104 patients evaluated the efficacy of carvedilol in patients without hemodynamic response to propranolol in primary prophylaxis; 56% of propranolol non-responders achieved a good hemodynamic response when shifted to carvedilol [52]. Low doses of carvedilol (12.5 mg/day) are very well tolerated [53] and are effective in obtaining a satisfactory hemodynamic response [54]. Because of that, carvedilol is increasingly considered the NSBB of choice in portal hypertension.
HVPG Response as Guidance for Therapy
Patients who achieve an HVPG ≤ 12 mmHg during treatment or a HVPG decrease of ≥ 20% from baseline (“HVPG responders”) have a low residual risk of variceal bleeding during long-term follow-up, while patients who do not achieve this hemodynamic response are at higher risk of bleeding and death. HVPG-guided therapy aims at significantly reducing the number of non-responders patients by adapting treatment to the hemodynamic response [45, 52, 55]. The interval between HVPG measurements should be short to avoid non-responders to continue under suboptimal therapy. It is recommended to perform this assessment within 2 weeks of achieving the final dose of NSBBs, which represents an interval of about 3–5 weeks between baseline and on-treatment HVPG measurements. The HVPG-guided therapy was associated with a reduction in the risk of bleeding, rebleeding, and mortality [32••, 45, 55], as well as an increase in transplant-free survival [32••]. The therapies used to improve the hemodynamic response when HVPG did not decrease enough under propranolol alone were the “à la carte” association of isosorbide-5-mononitrate to propranolol therapy [55]; the association of low dose prazosin, an alpha-adrenergic antagonist to propranolol [32••]; and shifting from propranolol to carvedilol [52]. Ideally, such drug combinations should include drugs acting on the splanchnic vasodilation and increased portal inflow characteristic of advanced cirrhosis, with agents with a capacity to act on hepatic resistance and endothelial dysfunction (such as statins, emricasan, obethicolic acid, anti-angiogenic agents, and other drugs under study) [33•].
Repeated measurements of HVPG could be difficult to perform. Furthermore, it has been reported that the risk of rebleeding between the baseline and on-treatment measurements of HVPG ranges between 7 and 22% [56], so ideally, this interval should be kept as short as possible. In that regard, it is worth noting that two independent studies have shown that the acute HVPG response 15 min after IV propranolol (1.5 mg/kg) predicts clinical outcomes during long-term therapy with NSBBs [44, 45]. The acute response was shown to be a robust independent predictor of bleeding and survival [44] and helps eliminating the risk period between the two measurements of HVPG. These studies showed that in the prophylaxis of first bleeding reaching a HVPG of ≤ 12 mmHg or having a decrease in HVPG of ≥ 10% of baseline defined a good hemodynamic response, while in patients treated after the first episode of variceal bleeding, the decrease in HVPG should be ≥ 20% of baseline or to values ≤ 12 mmHg. This strategy is likely to be cost-effective but requires specific validation.
Prognostic Value of HVPG in Acute Variceal Hemorrhage
Measurement of HVPG during the acute variceal bleeding episode provides important prognostic information. In this setting, a HVPG ≥ 20 mmHg is an independent predictor of failure to control bleeding, of early rebleeding, and of decreased 1-year survival [28, 29, 57]. The last of these studies [29] examined clinical factors that could predict an HVPG ≥ 20 mmHg; the most robust indicator was having very advanced cirrhosis (Child–Pugh class C). Other studies suggested that being in Child class C but exhibiting active bleeding at endoscopy while under vasoactive drug therapy was also a high-risk criteria. Based on these findings, there have been several randomized controlled trials aiming at providing more aggressive therapy to patients with poor prognostic indicators. The first was the study of Monescillo et al., in which patients with a HVPG ≥ 20 mmHg were randomized to receive standard of care treatment vs an immediate TIPS [57]. High-risk patients receiving TIPS had better outcomes in terms of control of bleeding and mortality than those receiving endoscopic therapy, but the study was criticized on the basis of using only endoscopic therapy in the medical arm and for using uncovered stents for TIPS. The second study [58] assessed high-risk of failure at admission for variceal hemorrhage from the finding of Child–Pugh class C (but with a score of < 14 points) or Child class B plus active bleeding despite vasoactive drug infusion. These high-risk patients were randomized to be continued under combined endoscopic band ligation plus drug therapy or to receive an early TIPS during the first 72 h from admission (with the vast majority of patients having the early TIPS during the first 48 h). The study demonstrated much better outcomes for the group receiving early TIPS, both in terms of control of bleeding, development of other complications of portal hypertension, and survival. Two later multicenter surveys confirmed these findings in larger populations [59••, 60].
HVPG and HCC
HVPG is an independent predictor of HCC development. In a subanalysis of a randomized trial that included 213 compensated cirrhotic patients, 12% developed HCC. A baseline HVPG > 10 mmHg was associated with a 6-fold increased incidence of HCC on follow-up [7]. In addition, several studies have demonstrated that patients with HCC that have increased bilirubin values or CSPH who undergo surgical resection have an increased risk of postoperative complications, including irreversible hepatic decompensation after 90 days, which is associated to high mortality [61,62,63]. A meta-analysis including almost 1737 patients compensated cirrhosis with HCC showed that CSPH significantly increased the risk of clinical decompensation after surgery and mortality at 3 and 5 years [18•].
Currently, the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD) guidelines consider CSPH a contraindication for liver resection surgery in patients with cirrhosis due to this higher risk to postoperative decompensation [64••, 65••].
The Use of HVPG in Developing New Therapies: Experience from Controlled Trials
Hepatic venous pressure gradient (HVPG) measurement is the gold standard method for determining the presence of CSPH (HVPG ≥ 10 mmHg). As reported above, few studies have used HVPG as guidance for therapy, probably due to the impracticality of measuring HVPG in every single patient requiring treatment for portal hypertension. However, many studies have used HVPG to determine the efficacy of new treatments for portal hypertension, to provide not only a proof of concept in phase II studies but also in some cases as a tentative surrogate of clinical outcomes to assess rapidly the effectiveness of a new treatment. As already mentioned, the effectivity of beta-blockers decreasing HVPG in patients with portal hypertension can be robustly assessed over a 4–12-week treatment period in relatively small groups of placebo and actively treated patients, including from 30 to 50 patients in each arm. For assessing clinical outcomes (bleeding/decompensation/survival), much higher effective numbers and treatment periods are required (100–200 patients per arm, 2–5-year treatment period, depending on the clinical setting). Therefore, there would be a significant cut of expenses and time required for drug development if this could be done on the basis of degree of HVPG reduction and/or number of HVPG “responders.” Before accepting this, however, it should be kept in mind that for a parameter to be considered a valid surrogate, it should have been proved that the clinical benefit reflected by an amelioration of the surrogate is independent of the mechanism by which the new agent is ameliorating the surrogate. In other words, having proved that HVPG is a good surrogate of the beneficial effects of NSBBs in portal hypertension does not mean that it would necessarily be a good surrogate for the effects of a drug which is acting on another mechanism of the increased portal pressure, for instance, on the disrupted liver architecture of cirrhosis. It is likely to be so, but the degree of improvement required is conjectural. It is even likely that a greater decrease in portal pressure would be required, given the fact that the beneficial effects of propranolol go beyond the fall in portal pressure and include from decreased bacterial translocation [66] and decreased intestinal permeability [67] to a greater reduction in variceal pressure than in HVPG [34].
In that regard, it is worth noting the recent studies assessing the hemodynamic effects of achieving a sustained viral response (SVR) with direct-acting antivirals (DAA) in patients with cirrhosis and portal hypertension due to chronic HVC or HVB virus infection. In a large study in HCV cirrhosis patients investigated before starting DAA and at 6 months after achieving SVR, there was a significant reduction in HVPG. However, this was modest (on average 1.8 mmHg) and over 70% of patients still had CSPH, indicating that they remained at risk of portal hypertension related complications and HCC. Independent predictors of persistent CSPH despite SVR were the presence of esophageal varices and a high basal HVPG. On the other hand, 17% of the patients despite SVR presented some increase in HVPG. Another relevant data from this study was that the liver stiffness measurement (LSM) 6 months after SVR was not able to rule out CSPH. Therefore, it appears that unfortunately these patients continue at risk of developing decompensation early after SVR and that this cannot be sensed by current non-invasive tests [68•]. Another study in patients with advanced cirrhosis, due to hepatitis C achieving SVR, evaluated the HVPG before and at 1 and 2 years of therapy. Among patients having the third HVPG measurement, HVPG reduction was greater than that observed at 1 year. Of note, 89% showed a reduction of > 20% and 30% reached a HVPG ≤ 12 mmHg [69], suggesting that amelioration of HVPG occurs slowly over time after achieving SVR. Interestingly, it has also been shown that decompensation is much less likely after SVR [70]. Actually, previous studies during treatment of HVB cirrhosis already showed that a marked histological improvement, including the disappearance of cirrhosis, was observed only after a mean of over 5 years of therapy [71]. Therefore, there is evidence supporting that reductions in HVPG caused by acting on the etiology of cirrhosis also result in lower risk of clinical events, which supports the use of HVPG as a surrogate in trials of new drugs for cirrhosis and portal hypertension.
Actually, a conference by the American Association for the Study of Liver Disease suggested that HVPG could be used as a surrogate marker of treatment efficacy in patients with advanced liver disease due to nonalcoholic steatohepatitis (NASH) (Sanyal 2015 Hepatology). This started a controversy on whether new drugs for NASH could have an accelerated approval after showing a beneficial effect on HVPG in a randomized, placebo controlled, double-blind clinical trial. The first of these studies investigated simtuzumab, a monoclonal antibody against lysyl oxidase-like 2 (LOXL2), which was used in a phase 2 trial with patients with NASH to induce regression of fibrosis in patients with NASH-cirrhosis and CSPH. LOLX2 is an enzyme that intervenes in the cross-linking of collagen; therefore, it is involved in collagen metabolism. The primary efficacy end point was the difference in the mean change from baseline in HVPG. Sintuzumab was not effective compared with placebo in achieving a significant decrease in HVPG. Additionally, Sintuzumab was also ineffective in reducing the progression of fibrosis [19•]. This study, however, shows that individual HVPG measurements had a very low variability (averaging less than 1 mmHg). A pilot study in patients with CSPH showed that taurine supplementation achieves a reduction of ≥ 20% on basal HVPG in 33% of patients [72]. Galectin-3 intervenes in processes such as apoptosis, angiogenesis, inflammation, adiposity regulation, and collagen synthesis [73]. Experimental studies have shown that Gal-3 knockout mice under atherogenic diets develop less steatosis, less oxidative stress and less hepatic fibrosis [74,75,76]. In a phase 2 study, 162 NASH cirrhosis patients with portal hypertension (HVPG ≥ 6 mmHg) were randomized to receive a galectin-3 inhibitor (GR-MD-02) at 2 mg/kg or 8 mg/kg or placebo during 52 weeks. At the end of treatment, no significant changes were observed in the HVPG of different groups. Differences in the degree of fibrosis or in the NAFLD Activity Score are also not found. One remarkable fact in this study was that patients in the treatment group developed fewer new varices than in the placebo group [77].
Recently, a multicenter open study evaluated the effect of caspase inhibition on portal pressure in compensated patients with portal hypertension (HVPG ≥ 6 mmHg). After a 4-week treatment with emricasan, a pan-caspase inhibitor, HVPG was significantly reduced in patients with compensated cirrhosis and basal HVPG ≥ 12 mmHg. One-third of these patients had a ≥ 20% decrease from baseline, and two-thirds had ≥ 10% decreases from baseline. Patients with mild portal hypertension did not show any HVPG reduction. To which extent the data may have been influenced by the lack of a control group remains conjectural. HVPG measurements were done according to state of the art and externally read by a central reviewer, which is likely to reduce observer bias and eliminates interobserver variability. The possible effect of emricasan on portal pressure was presumably associated with a reduction in intrahepatic resistance [78]. An ongoing multicenter phase II randomized clinical trial comparing three doses of emricasan vs placebo using change in HVPG as efficacy end point was recently closed, and results will be soon available. Even if these studies show a significant reduction in HVPG in the overall population or in a pre-specified subgroup, the degree of HVPG reduction associated with a clinical benefit will require further studies with a long-term follow-up to be clarified.
Specific Difficulties for the Use of HVPG in Large Multicenter Clinical Trials
The interest in using changes in HVPG as surrogate of clinical events or even for explanatory purposes on the effects of new drugs is not without problems. Most of these are originated by the fact that HVPG measurements are not routinely performed in many centers. Although HVPG in expert centers is a highly reliable technique with little variability over time, it is uncertain if the same can be obtained in multicenter studies involving many hospitals without specific expertise on HVPG.
To minimize these problems, multicenter studies have used several precautions including having a devoted brochure and video clips illustrating how to do a correct measurement and giving detailed instructions for a standardized procedure and step by step guidance using a checklist. Moreover, participating centers usually are asked to provide some sample HVPG tracings before started on the study to verify their ability in the measurement as judged by an expert central reader that qualifies every HVPG and may ask for a repeat procedure if required. Also, measurements are usually done by triplicate and include specific tricks for a good quality. It is our personal experience that such precautions allow obtaining in general reliable tracings of acceptable quality, the more important problem being the large center with rotating radiologists that should all be trained. This is much less problematic in European centers, where in most cases, HVPG is measured by hepatologists with specific training and large experience.
The use of HVPG for assessing new treatments or the effect of therapy for portal hypertension usually involves serial measurements. Time intervals vary widely between different studies. Obviously, the greater the time interval, the more likely is that there are changes in the underlying abnormalities leading to portal hypertension. Therefore, variability is expected to increase with longer time intervals between measurements. These have ranged from 15 min (the time interval used for measuring the “acute” hemodynamic response to IV propranolol) [44] to 1 year (the time interval used in the Timolol and the PREDESCI studies) [5, 79]. Of interest, no significant changes in HVPG were observed under placebo in the recent PREDESCI study over a 3-year follow-up period [79].
Another issue is the interobserver variability. This is usually low among experienced investigators (below 1 mmHg in the authors experience) but increases markedly in tracings of suboptimal quality, mainly due to the presence of respiratory artifacts, sedation, obesity, or tense ascites, factors that detract accuracy from measurements that interfere with a stable pressure tracing. Interobserver variability is abolished by using a “central” reader that reads all tracings blindly.
For this reason, the reproducibility of HVPG measurements is very important. Zipprich demonstrated that the measurements using balloon catheters had less variability than those using end-hole catheters. Measurements using balloon catheters have lower variation and show a much better correlation with directly measured portal pressure [80, 81]. In a study conducted to observe the effect of midazolam on HVPG, serial measurements were made at 3-min intervals for 30 min. No significant differences in mean HVPG were observed, reflecting the low intra-observer variability [82]. Several studies have shown no significant changes after placebo administration, including a large study where measurements were separated by 28 days [5, 83] or yearly for 3–4 years [79]. This confirms that when performing the measurements under the adequate standards, the reproducibility of measurements is excellent [1].
Conclusions
Measurement of HVPG is an invasive but safe and reproducible procedure that is usually done in an outpatient basis. HVPG provides reliable information about presence and degree of portal hypertension, extent of fibrosis, stage of the disease, response to therapy for portal hypertension, and risk of mortality. Because of this, it is an invaluable marker of disease severity and prognosis in advanced chronic liver disease.
HVPG can have several uses in the context of clinical trial. These go from patient selection, risk-stratification, use as explanatory marker of treatment benefit, and as a surrogate of the incidence of clinical events. The latter however requires further studies to establish which degree of HVPG reduction is required for achieving an unequivocal clinical benefit using new therapies acting by mechanisms different from that of non-selective beta-blockers.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bosch J, Garcia-Pagan JC, Berzigotti A, Abraldes JG. Measurement of portal pressure and its role in the management of chronic liver disease. Semin Liver Dis. 2006;26(4):348–62.
Groszmann RJ, Wongcharatrawee S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology. 2004;39(2):280–2.
Bosch J, Abraldes JG, Berzigotti A, Garcia-Pagan JC. The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol. 2009;6(10):573–82.
Reverter E, Blasi A, Abraldes JG, Martinez-Palli G, Seijo S, Turon F, et al. Impact of deep sedation on the accuracy of hepatic and portal venous pressure measurements in patients with cirrhosis. Liver Int. 2014;34(1):16–25.
Groszmann RJ, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Planas R, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353(21):2254–61.
Ripoll C, Groszmann R, Garcia-Tsao G, Grace N, Burroughs A, Planas R, et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 2007;133(2):481–8.
Ripoll C, Groszmann RJ, Garcia-Tsao G, Bosch J, Grace N, Burroughs A, et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J Hepatol. 2009;50(5):923–8.
Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362(9):823–32.
Gluud C, Brok J, Gong Y, Koretz RL. Hepatology may have problems with putative surrogate outcome measures. J Hepatol. 2007;46(4):734–42.
•• de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52. Current guidelines on the management of portal hypertension.
•• Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310–35. Guidance document on the current management of portal hypertension.
Nagula S, Jain D, Groszmann RJ, Garcia-Tsao G. Histological-hemodynamic correlation in cirrhosis-a histological classification of the severity of cirrhosis. J Hepatol. 2006;44(1):111–7.
Blasco A, Forns X, Carrion JA, Garcia-Pagan JC, Gilabert R, Rimola A, et al. Hepatic venous pressure gradient identifies patients at risk of severe hepatitis C recurrence after liver transplantation. Hepatology. 2006;43(3):492–9.
Samonakis DN, Cholongitas E, Thalheimer U, Kalambokis G, Quaglia A, Triantos CK, et al. Hepatic venous pressure gradient to assess fibrosis and its progression after liver transplantation for HCV cirrhosis. Liver Transpl. 2007;13(9):1305–11.
Calvaruso V, Burroughs AK, Standish R, Manousou P, Grillo F, Leandro G, et al. Computer-assisted image analysis of liver collagen: relationship to Ishak scoring and hepatic venous pressure gradient. Hepatology. 2009;49(4):1236–44.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–31.
Ripoll C, Bari K, Garcia-Tsao G. Serum albumin can identify patients with compensated cirrhosis with a good prognosis. J Clin Gastroenterol. 2015;49(7):613–9.
• Berzigotti A, Reig M, Abraldes JG, Bosch J, Bruix J. Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: a systematic review and meta-analysis. Hepatology. 2015;61(2):526–36. Evidence for using HVPG in selecting candidates for liver resection.
• Harrison SA, Abdelmalek MF, Caldwell S, Shiffman ML, Diehl AM, Ghalib R, et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis. Gastroenterology. 2018;155(4):1140–53. Use of HVPG as a marker of disease progression in NASH.
Zipprich A, Garcia-Tsao G, Rogowski S, Fleig WE, Seufferlein T, Dollinger MM. Prognostic indicators of survival in patients with compensated and decompensated cirrhosis. Liver Int. 2012;32(9):1407–14.
Merkel C, Bolognesi M, Bellon S, Zuin R, Noventa F, Finucci G, et al. Prognostic usefulness of hepatic vein catheterization in patients with cirrhosis and esophageal varices. Gastroenterology. 1992;102(3):973–9.
Berzigotti A, Rossi V, Tiani C, Pierpaoli L, Zappoli P, Riili A, et al. Prognostic value of a single HVPG measurement and Doppler-ultrasound evaluation in patients with cirrhosis and portal hypertension. J Gastroenterol. 2011;46(5):687–95.
• Silva-Junior G, Baiges A, Turon F, Torres F, Hernandez-Gea V, Bosch J, et al. The prognostic value of hepatic venous pressure gradient in patients with cirrhosis is highly dependent on the accuracy of the technique. Hepatology. 2015;62(5):1584–92. Importance of accurate technique in HVPG measurements.
Stanley AJ, Robinson I, Forrest EH, Jones AL, Hayes PC. Haemodynamic parameters predicting variceal haemorrhage and survival in alcoholic cirrhosis. QJM. 1998;91(1):19–25.
Berzigotti A, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Morillas R, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54(2):555–61.
Rincon D, Lo Iacono O, Tejedor M, Hernando A, Ripoll C, Catalina MV, et al. Prognostic value of hepatic venous pressure gradient in patients with compensated chronic hepatitis C-related cirrhosis. Scand J Gastroenterol. 2013;48(4):487–95.
Lens S, Rincon D, Garcia-Retortillo M, Albillos A, Calleja JL, Banares R, et al. Association between severe portal hypertension and risk of liver decompensation in patients with hepatitis C, regardless of response to antiviral therapy. Clin Gastroenterol Hepatol. 2015;13(10):1846–53 e1.
Moitinho E, Escorsell A, Bandi JC, Salmeron JM, Garcia-Pagan JC, Rodes J, et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology. 1999;117(3):626–31.
Abraldes JG, Villanueva C, Banares R, Aracil C, Catalina MV, Garci APJC, et al. Hepatic venous pressure gradient and prognosis in patients with acute variceal bleeding treated with pharmacologic and endoscopic therapy. J Hepatol. 2008;48(2):229–36.
Rincon D, Lo Iacono O, Ripoll C, Gomez-Camarero J, Salcedo M, Catalina MV, et al. Prognostic value of hepatic venous pressure gradient for in-hospital mortality of patients with severe acute alcoholic hepatitis. Aliment Pharmacol Ther. 2007;25(7):841–8.
Navasa M, Garcia-Pagan JC, Bosch J, Riera JR, Banares R, Mas A, et al. Portal hypertension in acute liver failure. Gut. 1992;33(7):965–8.
•• Villanueva C, Graupera I, Aracil C, Alvarado E, Minana J, Puente A, et al. A randomized trial to assess whether portal pressure guided therapy to prevent variceal rebleeding improves survival in cirrhosis. Hepatology. 2017;65(5):1693–707. Randomized clinical trial showing superiority of HVPG guided over standard of care medical therapy for portal hypertension.
• Bosch J, Groszmann RJ, Shah VH. Evolution in the understanding of the pathophysiological basis of portal hypertension: how changes in paradigm are leading to successful new treatments. J Hepatol. 2015;62(1 Suppl):S121–30. Review of evolving mechanisms of portal hypertension during the progression of cirrhosis.
Escorsell A, Bordas JM, Castaneda B, Llach J, Garcia-Pagan JC, Rodes J, et al. Predictive value of the variceal pressure response to continued pharmacological therapy in patients with cirrhosis and portal hypertension. Hepatology. 2000;31(5):1061–7.
Feu F, Garcia-Pagan JC, Bosch J, Luca A, Teres J, Escorsell A, et al. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. Lancet. 1995;346(8982):1056–9.
Grace ND, Conn HO, Resnick RH, Groszmann RJ, Atterbury CE, Wright SC, et al. Distal splenorenal vs. portal-systemic shunts after hemorrhage from varices: a randomized controlled trial. Hepatology. 1988;8(6):1475–81.
Rigau J, Bosch J, Bordas JM, Navasa M, Mastai R, Kravetz D, et al. Endoscopic measurement of variceal pressure in cirrhosis: correlation with portal pressure and variceal hemorrhage. Gastroenterology. 1989;96(3):873–80.
Groszmann RJ, Bosch J, Grace ND, Conn HO, Garcia-Tsao G, Navasa M, et al. Hemodynamic events in a prospective randomized trial of propranolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology. 1990;99(5):1401–7.
Abraldes JG, Tarantino I, Turnes J, Garcia-Pagan JC, Rodes J, Bosch J. Hemodynamic response to pharmacological treatment of portal hypertension and long-term prognosis of cirrhosis. Hepatology. 2003;37(4):902–8.
Villanueva C, Balanzo J, Novella MT, Soriano G, Sainz S, Torras X, et al. Nadolol plus isosorbide mononitrate compared with sclerotherapy for the prevention of variceal rebleeding. N Engl J Med. 1996;334(25):1624–9.
Villanueva C, Minana J, Ortiz J, Gallego A, Soriano G, Torras X, et al. Endoscopic ligation compared with combined treatment with nadolol and isosorbide mononitrate to prevent recurrent variceal bleeding. N Engl J Med. 2001;345(9):647–55.
Turnes J, Garcia-Pagan JC, Abraldes JG, Hernandez-Guerra M, Dell’Era A, Bosch J. Pharmacological reduction of portal pressure and long-term risk of first variceal bleeding in patients with cirrhosis. Am J Gastroenterol. 2006;101(3):506–12.
Villanueva C, Lopez-Balaguer JM, Aracil C, Kolle L, Gonzalez B, Minana J, et al. Maintenance of hemodynamic response to treatment for portal hypertension and influence on complications of cirrhosis. J Hepatol. 2004;40(5):757–65.
La Mura V, Abraldes JG, Raffa S, Retto O, Berzigotti A, Garcia-Pagan JC, et al. Prognostic value of acute hemodynamic response to i.v. propranolol in patients with cirrhosis and portal hypertension. J Hepatol. 2009;51(2):279–87.
Villanueva C, Aracil C, Colomo A, Hernandez-Gea V, Lopez-Balaguer JM, Alvarez-Urturi C, et al. Acute hemodynamic response to beta-blockers and prediction of long-term outcome in primary prophylaxis of variceal bleeding. Gastroenterology. 2009;137(1):119–28.
Albillos A, Banares R, Gonzalez M, Ripoll C, Gonzalez R, Catalina MV, et al. Value of the hepatic venous pressure gradient to monitor drug therapy for portal hypertension: a meta-analysis. Am J Gastroenterol. 2007;102(5):1116–26.
D’Amico G, Garcia-Pagan JC, Luca A, Bosch J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: a systematic review. Gastroenterology. 2006;131(5):1611–24.
Kerbert AJ, Chiang FW, van der Werf M, Stijnen T, Slingerland H, Verspaget HW, et al. Hemodynamic response to primary prophylactic therapy with nonselective beta-blockers is related to a reduction of first variceal bleeding risk in liver cirrhosis: a meta-analysis. Eur J Gastroenterol Hepatol. 2017;29(4):380–7.
Bellot P, Garcia-Pagan JC, Abraldes JG, Bosch J. Primary prophylaxis of esophageal variceal bleeding in cirrhosis. Gastroenterol Clin Biol. 2008;32(5 Pt 1):532–40.
Banares R, Moitinho E, Piqueras B, Casado M, Garcia-Pagan JC, de Diego A, et al. Carvedilol, a new nonselective beta-blocker with intrinsic anti-Alpha1-adrenergic activity, has a greater portal hypotensive effect than propranolol in patients with cirrhosis. Hepatology. 1999;30(1):79–83.
Banares R, Moitinho E, Matilla A, Garcia-Pagan JC, Lampreave JL, Piera C, et al. Randomized comparison of long-term carvedilol and propranolol administration in the treatment of portal hypertension in cirrhosis. Hepatology. 2002;36(6):1367–73.
Reiberger T, Ulbrich G, Ferlitsch A, Payer BA, Schwabl P, Pinter M, et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut. 2013;62(11):1634–41.
Bosch J. Carvedilol for portal hypertension in patients with cirrhosis. Hepatology. 2010;51(6):2214–8.
Schwarzer R, Kivaranovic D, Paternostro R, Mandorfer M, Reiberger T, Trauner M, et al. Carvedilol for reducing portal pressure in primary prophylaxis of variceal bleeding: a dose-response study. Aliment Pharmacol Ther. 2018;47(8):1162–9.
Bureau C, Peron JM, Alric L, Morales J, Sanchez J, Barange K, et al. "a La carte" treatment of portal hypertension: adapting medical therapy to hemodynamic response for the prevention of bleeding. Hepatology. 2002;36(6):1361–6.
Thalheimer U, Mela M, Patch D, Burroughs AK. Monitoring target reduction in hepatic venous pressure gradient during pharmacological therapy of portal hypertension: a close look at the evidence. Gut. 2004;53(1):143–8.
Monescillo A, Martinez-Lagares F, Ruiz-del-Arbol L, Sierra A, Guevara C, Jimenez E, et al. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology. 2004;40(4):793–801.
Garcia-Pagan JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, et al. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362(25):2370–9.
•• Hernandez-Gea V, Procopet B, Giraldez A, Amitrano L, Villanueva C, Thabut D, et al. Preemptive-TIPS improves outcome in high-risk variceal bleeding: an observational study. Hepatology. 2018. Larger study on early use of TIPS for variceal bleeding in high-risk patients.
Garcia-Pagan JC, Di Pascoli M, Caca K, Laleman W, Bureau C, Appenrodt B, et al. Use of early-TIPS for high-risk variceal bleeding: results of a post-RCT surveillance study. J Hepatol. 2013;58(1):45–50.
Cucchetti A, Cescon M, Golfieri R, Piscaglia F, Renzulli M, Neri F, et al. Hepatic venous pressure gradient in the preoperative assessment of patients with resectable hepatocellular carcinoma. J Hepatol. 2016;64(1):79–86.
Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999;30(6):1434–40.
Bruix J, Castells A, Bosch J, Feu F, Fuster J, Garcia-Pagan JC, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology. 1996;111(4):1018–22.
•• Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723–50. Current guidelines for management of hepatocellular carcinoma.
•• European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. Current guidelines for management of hepatocellular carcinoma.
Perez-Paramo M, Munoz J, Albillos A, Freile I, Portero F, Santos M, et al. Effect of propranolol on the factors promoting bacterial translocation in cirrhotic rats with ascites. Hepatology. 2000;31(1):43–8.
Reiberger T, Ferlitsch A, Payer BA, Mandorfer M, Heinisch BB, Hayden H, et al. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J Hepatol. 2013;58(5):911–21.
• Lens S, Alvarado-Tapias E, Marino Z, Londono MC, LLop E, Martinez J, et al. Effects of all-oral anti-viral therapy on HVPG and systemic hemodynamics in patients with hepatitis C virus-associated cirrhosis. Gastroenterology. 2017;153(5):1273–83 e1. Large study on effects of anti-HCV therapy on HVPG.
Afdhal N, Everson GT, Calleja JL, McCaughan GW, Bosch J, Brainard DM, et al. Effect of viral suppression on hepatic venous pressure gradient in hepatitis C with cirrhosis and portal hypertension. J Viral Hepat. 2017;24(10):823–31.
van der Meer AJ, Veldt BJ, Feld JJ, Wedemeyer H, Dufour JF, Lammert F, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308(24):2584–93.
Chang TT, Lai CL, Kew Yoon S, Lee SS, Coelho HS, Carrilho FJ, et al. Entecavir treatment for up to 5 years in patients with hepatitis B e antigen-positive chronic hepatitis B. Hepatology. 2010;51(2):422–30.
Schwarzer R, Kivaranovic D, Mandorfer M, Paternostro R, Wolrab D, Heinisch B, et al. Randomised clinical study: the effects of oral taurine 6g/day vs placebo on portal hypertension. Aliment Pharmacol Ther. 2018;47(1):86–94.
Buechler C, Haberl EM, Rein-Fischboeck L, Aslanidis C. Adipokines in liver cirrhosis. Int J Mol Sci. 2017;18(7).
Iacobini C, Menini S, Ricci C, Blasetti Fantauzzi C, Scipioni A, Salvi L, et al. Galectin-3 ablation protects mice from diet-induced NASH: a major scavenging role for galectin-3 in liver. J Hepatol. 2011;54(5):975–83.
Nomoto K, Nishida T, Nakanishi Y, Fujimoto M, Takasaki I, Tabuchi Y, et al. Deficiency in galectin-3 promotes hepatic injury in CDAA diet-induced nonalcoholic fatty liver disease. TheScientificWorldJournal. 2012;2012:959824.
Pejnovic N, Jeftic I, Jovicic N, Arsenijevic N, Lukic ML. Galectin-3 and IL-33/ST2 axis roles and interplay in diet-induced steatohepatitis. World J Gastroenterol. 2016;22(44):9706–17.
Chalasani N, Garcia-Tsao G, Goodman Z, Lawitz E, Abdelmalek M, Rinella M, et al. A multicenter, randomized, double-blind, PLB-controlled trial of galectin-3 inhibitor (GR-MD-02) in patients with NASH cirrhosis and portal hypertension. J Hepatol. 2018;68:S100–1.
Garcia-Tsao G, Fuchs M, Shiffman M, Borg BB, Pyrsopoulos N, Shetty K, et al. Emricasan (IDN-6556) lowers portal pressure in patients with compensated cirrhosis and severe portal hypertension. Hepatology. 2019;69(2):717–28.
Villanueva C, Genescà J, Garcia-Pagan J, Calleja J, Aracil C, Bañares R, et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2019;18:1–12.
Zipprich A, Winkler M, Seufferlein T, Dollinger MM. Comparison of balloon vs. straight catheter for the measurement of portal hypertension. Aliment Pharmacol Ther. 2010;32(11–12):1351–6.
Perello A, Escorsell A, Bru C, Gilabert R, Moitinho E, Garcia-Pagan JC, et al. Wedged hepatic venous pressure adequately reflects portal pressure in hepatitis C virus-related cirrhosis. Hepatology. 1999;30(6):1393–7.
Steinlauf AF, Garcia-Tsao G, Zakko MF, Dickey K, Gupta T, Groszmann RJ. Low-dose midazolam sedation: an option for patients undergoing serial hepatic venous pressure measurements. Hepatology. 1999;29(4):1070–3.
Abraldes JG, Albillos A, Banares R, Turnes J, Gonzalez R, Garcia-Pagan JC, et al. Simvastatin lowers portal pressure in patients with cirrhosis and portal hypertension: a randomized controlled trial. Gastroenterology. 2009;136(5):1651–8.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Jaume Bosch reports personal fees from Conatus, personal fees from Gilead, grants and personal fees from Exallenz, personal fees from Actelion, personal fees from BioVie, grants from Brudy, other from BLB, and personal fees from Blade Therapeutics, outside the submitted work. Maria Gabriela Delgado declares no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Portal Hypertension
Rights and permissions
About this article
Cite this article
Delgado, M.G., Bosch, J. HVPG Measurements as a Surrogate of Clinical Events in Cirrhosis: Experience from Clinical Trials. Curr Hepatology Rep 18, 164–173 (2019). https://doi.org/10.1007/s11901-019-00461-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-019-00461-5