Abstract
Advanced Chronic Liver Disease (ACLD) can be classified from Stage 0 to Stage 6. The Hepatic Venous Pressure Gradient (HVPG) remains the gold standard for deriving portal pressure in sinusoidal portal hypertension. Studies have established the threshold HVPG of 10 mmHg as clinically significant portal hypertension (CSPH). CSPH heralds the development of gastroesophageal varices and bleeding and other complications of decompensation such as ascites and hepatic encephalopathy. Interest in the prevention of decompensation has been revived by the PREDESCI trial demonstrating the potential for pharmacological therapy to prevent decompensation. There have also been recent developments in non-invasive methods to assess CSPH and stratify those at greatest risk of decompensation. These methods are attractive alternatives to HVPG, which is invasive and, in some countries, remains a research tool. This review aims to summarize the current data on the assessment of CSPH, and variables predicting decompensation.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Clinically significant portal hypertension
- Hepatic venous pressure gradient
- Nonselective beta-blocker
- Advanced chronic liver disease
- Decompensation
Stages of Cirrhosis and Clinically Significant Portal Hypertension
In ACLD, stages 0–2 (compensated phase) have a median duration of over 10 years, and further progression leads to decompensation (Fig. 35.1) with variceal bleeding, ascites, and hepatic encephalopathy (alone or in combination). Some patients may recompensate to stages 0–2, but a second decompensation invariably leads to the downward spiral to end-stage liver disease, ACLF, or death. Mortality from decompensated cirrhosis is much higher at 40%, 65%, and 80% at 1, 2, and 5 years respectively, compared to 1% in the compensated state [1].
Clinical stages of cirrhosis [1]
Portal hypertension in cirrhosis results from increased intra–hepatic resistance due to fibrosis and contraction of sinusoidal and peri-sinusoidal cells due to interplay between vascular mediators favoring vasoconstriction with reduced intrahepatic eNOS activity. There is also increased portal inflow due to splanchnic vasodilatation driven by nitric oxide (NO) and sGC-PKG signaling, which perpetuates the initial rise in portal pressure [2, 3]. These hemodynamic changes result in the development of the hyperdynamic circulation. HVPG is an estimation of the true portal pressure in sinusoidal portal hypertension and is the Wedge Hepatic Venous Pressure (WHVP) minus Free Hepatic Venous Pressure (FHVP). The method of accurately measuring HVPG is described elsewhere [4].
Normal HVPG is between 1–5 mmHg and is described as CSPH at ≥10 mmHg. The hyperdynamic circulation has not yet fully developed at HVPG <10 mmHg where portal inflow has less of a contribution. Thus, the therapeutic effect of NSBB on portal hypertension is more pronounced at HVPG ≥10 mmHg [5]. Above this threshold varices may develop with progression to ascites or hepatic encephalopathy [6, 7]. Studies consistently show that the more common first decompensating event is ascites [7,8,9].
Thus, the discovery of surrogate markers predicting decompensation is an important clinical goal. These tools can aid in patient selection for therapies such as beta-blockers (or future therapies), or closely monitor those at low risk.
Hepatic Venous Pressure Gradient in Predicting Decompensation
HVPG as a marker of prognosis in cirrhosis and decompensation has been widely studied. Table 35.1 provides summaries of the important studies investigating the role of HVPG in predicting decompensation [6,7,8,9,10,11,12,13,14,15,16]. Significant heterogeneity exists in baseline characteristics with regards to the presence of CSPH, cirrhosis, varices, use of NSBB as prophylaxis against bleeding, etiology, the definition of decompensation and presence of hepatocellular carcinoma. Decompensation can vary considerably from 12.8% to 33.6% for cholestatic diseases and alcohol-related liver diseases respectively [17]. HVPG may underestimate the true portal pressure in cholestatic diseases due to the pre-sinusoidal component. Recent data also suggests patients with NAFLD can decompensate on follow-up even with baseline HVPG slightly <10 mmHg [18] and at a higher frequency for a given HVPG than RNA positive HCV [19], although this requires further validation. There is also variability with regards to antiviral therapy, and one can argue that studies using interferon-based regimens are outdated in the current era of directly acting antiviral therapy. However, a study showed that baseline HVPG influenced decompensation rates rather than interferon-based regimens [12]. One can infer that the results would apply to current antiviral therapies.
Baseline HVPG as a Marker of Risk of Decompensation
A seminal placebo-controlled trial investigating the role of timolol in preventing the development of varices and variceal bleeding in patients without varices and HVPG ≥6 mmHg showed that varices only developed at HVPG ≥10 mmHg [6]. The primary endpoint occurred in 84 out of 213 patients, without any difference between timolol and placebo. A nested cohort study within this RCT showed that HVPG mmHg <10 mmHg was associated with reduced decompensation, in particular ascites [7]. A further post hoc analysis of the timolol study showed that baseline BMI was a predictor of decompensation, although the association was stronger with baseline HVPG and albumin [10].
A retrospective analysis of patients with ACLD (73% compensated) showed that baseline HVPG ≥16 mmHg and bilirubin predicted the first decompensation, with HVPG having the greatest discriminative ability. In this study, the presence of abdominal portosystemic collaterals (APC) was only seen with HVPG ≥10 mmHg, and strongly correlated with HVPG >16 mmHg and suggests that APC on ultrasound scan could be a non-invasive tool to categorize patients with high HVPG [11]. This requires validation in prospective studies.
A single-center retrospective study with a mixture of compensated and decompensated patients showed that baseline HVPG >10 mmHg and MELD >12 predicted decompensation [15]. Furthermore baseline single HVPG had the greatest discriminative ability and patients with HVPG <10 mmHg were unlikely to decompensate, The high decompensation rate of 29% most likely reflects patients with HCC and varices being included.
Another retrospective study identified baseline HVPG and albumin to predict decompensation in compensated patients with HCV infection [14]. Patients with prognostic index <2.5 were very unlikely to decompensate. As in the study by Ripoll et al. [15], the high decompensation rate appears to reflect the inclusion of patients with HCC and varices. Lens and colleagues found that baseline HVPG before HCV treatment but not sustained viral response predicted decompensation and transplant-free survival [12]. These patients had interferon-based antiviral therapies.
A large recent study of 741 consecutive compensated patients with cirrhosis (predominantly NASH, 30.8%) and HVPG ≥6 mmHg, showed that decompensation developed in 29.2% over a mean follow-up of 1.6 ± 0.4 years [20]. Decompensation occurred earlier and more frequently in patients with high HVPG (≥20 mmHg, 35.5% NASH) with higher mortality. Baseline HVPG independently predicted decompensation. Limitations of this study include retrospective uncontrolled design, small numbers of patients in the high HVPG group (n = 18), and short follow-up.
HVPG Response as a Marker of Risk of Decompensation
Studies show the role of HVPG response to drug therapies as a prognostic marker predicting decompensation. In these studies, the protocols involve acute HVPG response and repeat HVPG measurements performed at variable intervals. The latter can make a comparison of studies challenging. There could also be a degree of selection bias since not all patients would have repeat HVPG measurements due to dropout or censoring events such as decompensation, death, or transplantation.
Acute HVPG response to NSBB is consistently reliable in predicting decompensation. A retrospective study found that a 12% reduction in HVPG in response to intravenous propranolol had the greatest discriminative ability for rebleeding and mortality [21]. Acute and chronic (1–3 months) HVPG response to NSBB, defined as reduction ≥10% or to <12 mmHg, was associated with a lower risk of variceal bleeding and ascites in a prospective study of 105 patients [16]. Another prospective series with a similar study design investigated the role of HVPG response to NSBB in a purely compensated cirrhotic population and mirrored these findings [9]. Baseline MELD >9 and chronic hemodynamic nonresponse were associated with ascites development. MELD added additional prognostic data in hemodynamic responders.
In the nested study of the timolol RCT, HVPG reduction of <10% from baseline predicted decompensation [7]. An increase of 1 mmHg in HVPG led to an 11% increased risk of decompensation. Multivariate analysis revealed that a lack of hemodynamic response at 12 months predicted decompensation (HR, 2.6; 95% CI, 1.1–5.6). A retrospective study found that, unlike baseline HVPG, delta HVPG at 1 year did not influence outcomes after multivariate analysis [15]. Furthermore, NSBB therapy did not appear to influence clinical outcomes. Heterogeneity with the inclusion of both compensated and decompensated patients, and those with HCC, along with low sample size and retrospective design are limitations.
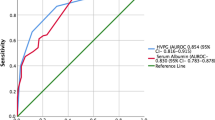
A retrospective study of 100 compensated HCV patients on antiviral therapy over 24 weeks found that repeat HVPG decreased significantly and was related to high baseline viral load. After 24 weeks only those with SVR had HVPG reduction [12]. There was a trend toward higher decompensation in patients failing to achieve HVPG <10 mmHg. The small sample size in this study is a limitation. In a prospective study, 90 HCV patients treated with interferon-free therapies underwent hemodynamic studies. All patients had portal hypertension (HVPG ≥6 mmHg) and underwent follow-up HVPG assessment at 8.79 months [22]. Patients with HVPG <10 mmHg at baseline did not progress to CSPH. Follow-up HVPG was associated with decompensation (per mmHg rise, HR 1.18 (95% CI 1.08–1.28; AUROC 0.819)). By contrast, baseline HVPG was not associated with decompensation during follow-up.
A prospective study of patients treated with either propranolol or carvedilol (in propranolol nonresponders) as primary prevention, found less decompensation in the carvedilol group when compared with VBL (p = 0.035) [13]. Haemodynamic responders on propranolol or carvedilol also suffered less decompensation (ascites (p = 0.031) and variceal bleeding (p = 0.012) than those on VBL. There was a history of previous ascites in 10% of patients. In the large hemodynamic study from India mentioned earlier, 20 patients with HVPG ≥12 mmHg were started on carvedilol, and the hemodynamic response was less in the high HVPG group [20]. Moreover, reductions in portal pressure did not influence the risk of decompensation.
The PREDESCI RCT, compared NSBB with placebo in patients with compensated liver disease (Fig. 35.2) [8]. The rigorous protocol comprised a hemodynamic study at baseline to assess for the presence of CSPH and determine acute hemodynamic response to intravenous propranolol. Responders received propranolol and non-responders were given carvedilol. A placebo arm was required for each NSBB. The HVPG measurements were repeated annually. Decompensation was inversely associated with HVPG reduction >10% from baseline or to <10 mmHg at 1 year. Indeed, the primary outcome was significantly reduced in these hemodynamic responders compared to non-responders (HR = 0.32, 95% CI = 0.13 to 0.75; p = 0.008).
Schema of PREDESCI trial [8]
A recent meta-analysis of over 1100 patients showed that HVPG response (<12 mmHg or >20% from baseline) to NSBB as part of primary or secondary prevention was associated with significantly fewer clinical events and lower deaths [23].
The Role of Other Factors in Predicting Decompensation
Although HVPG remains the gold standard for predicting decompensation it is invasive, with limited availability in many countries. Therefore, non-invasive markers predicting decompensation have an important role (Table 35.2).
Ripoll found that MELD, albumin, and HVPG predicted decompensation [7], and a nomogram based on this study incorporating platelet count, MELD, albumin, and AST has been proposed [24]. Markers of systemic inflammation predicting decompensation have also been studied. Obesity has also been associated with decompensation [10]. The role of nutrition and etiology is covered elsewhere.
Simple serum markers of fibrosis have been assessed in several studies [25,26,27,28,29]. Prospective studies in patients with compensated cirrhosis have failed to show APRI nor FIB-4 to predict decompensation [28, 29]. A recently published retrospective study found FIB-4 and ALBI to predict decompensation [25]. A study on the predictive value of non-invasive markers and HVPG in NASH cirrhosis was published recently [18, 30]. ELF was the serum marker with greater prognostic capacity. Other large retrospective [31] and prospective studies [32] in NAFLD cirrhosis have found noninvasive markers to be highly predictive of decompensation.
Liver stiffness (LS) has been shown to accurately reflect HVPG ≤12 mmHg, but at higher pressures correlation with HVPG is less strict and likely to reflect other factors in the pathogenesis of portal hypertension, in particular increased portal inflow [33]. A large multicentre study found that LSM ≥ 25 kPa correlates with CSPH in cACLD apart from obese NASH patients. In obese NASH, the ANTICIPATE-NASH model was proposed based on a nomogram [34]. A prospective study showed that LSM < 21.1 kPa predicted freedom from decompensation with similar precision to HVPG [35]. Other studies have confirmed these findings in patients with HCV cirrhosis with or without HIV co-infection and alcohol-related liver disease [28, 29, 36, 37]. The LS thresholds for predicting the presence of decompensation varied between 34.5 and 40 kPa. However, in the PREDESCI trial [8], LS at baseline had low precision in predicting decompensation and/or death. Another study confirmed this finding [20]. However, sequential LSM was found to be accurate for diagnosing CSPH [22]. Baseline (threshold LSM 21 kPa) and changes in repeated LSM were found to predict decompensation, HCC, and mortality in a large retrospective cohort of NAFLD patients with F3–F4 fibrosis [38]. Studies have shown that LSM obtained using MRE was strongly associated with the development of decompensation in different aetiologies [39,40,41,42].
Spleen Stiffness (SS) has been suggested to correlate better with portal hypertension at higher portal pressures. In a prospective study [43] of 100 patients with compensated HCV cirrhosis, LS, and SS were more precise than other noninvasive makers (platelet/spleen ratio, LSPS) in predicting CSPH. The “Anticipate” study, revealed that LSM x spleen diameter/platelet count (LSPS) score values >2.65 were associated with an 80% risk of CSPH with AUC of 0.88 [44]. In a study of HCV patients with compensated cirrhosis, SS value of 54 kPa had sensitivity and specificity of 97% and 63% respectively in predicting low risk of decompensation [26]. Using TE and 2D-SWE, there can be greater non-valid or failed reading of SS compared with LS due to small-sized spleens. pSWE such as ARFI can be more reliable since it can compensate for high BMI, ascites, or small spleens. However, the data on variability is somewhat limited.
A prospective study found that IL-6 levels correlated with risk of decompensation (hazard ratio 1.06 (96% CI 1.01–1.10), with CRP and HVPG showing a strong trend, highlighting the importance of markers of systemic inflammation [45].
In a nested study of the PREDESCI trial, Bacterial Infections (BI) were developed in 36 patients that presented with decompensation [46]. BI occurred invariably before decompensation, with the principal sources being community-acquired respiratory and urinary tract and predominantly gram-negative organisms. Decompensation and particularly mortality were associated with BI, with subdistribution hazard ratios of 2.98 (95% CI, 1.02–8.42) and 6.93 (95% CI, 2.64–18.18) respectively. Age, lower albumin, lower BMI, and HCC were noted to be risk factors for BI in compensated cirrhotic patients. NSBB use showed a trend towards reduced risk of developing BI.
Conclusions
The development of CSPH has profound effects on the natural history of ACLD, and much research has been undertaken to understand factors predicting decompensation. Although HVPG, both at baseline and change over time or in response to pharmacotherapy, remains the gold standard, there is an unmet need to identify noninvasive surrogate makers of CSPH and decompensation. Liver and spleen stiffness are promising in this regard, although a lack of large, controlled studies including different etiologies with extended follow-up prevents universal adoption of these tools.
Abbreviations
- ACLD:
-
Advanced chronic liver disease
- HVPG:
-
Hepatic venous pressure gradient
- CSPH:
-
Clinically significant portal hypertension
- ACLF:
-
Acute on chronic liver failure
- NAFLD:
-
Non-alcoholic fatty liver disease
- RCT:
-
Randomised controlled trial
- RNA:
-
Ribonucleic acid
- HCV:
-
Hepatitis C virus
- BMI:
-
Body mass index
- APC:
-
Abdominal porto-systemic collaterals
- MELD:
-
Model for end stage liver disease
- HCC:
-
Hepatocellular carcinoma
- NASH:
-
Non-alcoholic steatohepatitis
- NSBB:
-
Non-selective beta blocker
- SVR:
-
Sustained virological response
- VBL:
-
Variceal band ligation
- As:
-
Ascites
- HE:
-
Hepatic encephalopathy
- PB:
-
Portal hypertensive bleeding
- Ja:
-
Jaundice
- SBP:
-
Spontaneous bacterial peritonitis
- LSM:
-
Liver stiffness measurement
- IQR:
-
Interquartile range
- SS:
-
Splenic stiffness
- LSPS:
-
LSM x spleen diameter/platelet count
- TE:
-
Transient elastography
- SWE:
-
Shear wave elastography
- ARFI:
-
Acoustic radiation force impulse
- BI:
-
Bacterial infections
- SHR:
-
Subdistribution hazard ratios
- tAUC:
-
Time-dependent area under the curve
- ABIDE:
-
Aspartate aminotransferase/alanine, aminotransferase ratio, bilirubin, International normalized ratio, type 2 Diabetes, and oesophageal varices
References
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–31.
Newby DE, Hayes PC. Hyperdynamic circulation in liver cirrhosis: not peripheral vasodilatation but ‘splanchnic steal’. QJM. 2002;95:827–30.
Wiest R, Groszmann RJ. The paradox of nitric oxide in cirrhosis and portal hypertension: too much, not enough. Hepatology. 2002;35:478–91.
Groszmann RJ, Wongcharatrawee S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology. 2004;39:280–2.
Villanueva C, Albillos A, Genesca J, et al. Development of hyperdynamic circulation and response to beta-blockers in compensated cirrhosis with portal hypertension. Hepatology. 2016;63:197–206.
Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254–61.
Ripoll C, Groszmann R, Garcia-Tsao G, et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 2007;133:481–8.
Villanueva C, Albillos A, Genesca J, et al. Beta-blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomized, double-blind, placebo-controlled, multicentre trial. Lancet. 2019;393:1597–608.
Hernandez-Gea V, Aracil C, Colomo A, et al. Development of ascites in compensated cirrhosis with severe portal hypertension treated with beta-blockers. Am J Gastroenterol. 2012;107:418–27.
Berzigotti A, Garcia-Tsao G, Bosch J, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54:555–61.
Berzigotti A, Rossi V, Tiani C, et al. Prognostic value of a single HVPG measurement and Doppler-ultrasound evaluation in patients with cirrhosis and portal hypertension. J Gastroenterol. 2011;46:687–95.
Lens S, Rincon D, Garcia-Retortillo M, et al. Association between severe portal hypertension and risk of liver decompensation in patients with hepatitis C, regardless of response to antiviral therapy. Clin Gastroenterol Hepatol. 2015;13:1846–1853.e1.
Reiberger T, Ulbrich G, Ferlitsch A, et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with hemodynamic non-response to propranolol. Gut. 2013;62:1634–41.
Rincon D, Lo Iacono O, Tejedor M, et al. Prognostic value of hepatic venous pressure gradient in patients with compensated chronic hepatitis C-related cirrhosis. Scand J Gastroenterol. 2013;48:487–95.
Ripoll C, Lastra P, Rincon D, et al. Comparison of MELD, HVPG, and their changes to predict clinically relevant endpoints in cirrhosis. Scand J Gastroenterol. 2012;47:204–11.
Villanueva C, Aracil C, Colomo A, et al. Acute hemodynamic response to beta-blockers and prediction of long-term outcome in primary prophylaxis of variceal bleeding. Gastroenterology. 2009;137:119–28.
D’Amico G, Perricone G. Prediction of decompensation in patients with compensated cirrhosis: does etiology matter? Curr Hepatol Rep. 2019;18:144–56.
Sanyal AJ, Harrison SA, Ratziu V, et al. The natural history of advanced fibrosis due to nonalcoholic steatohepatitis: data from the simtuzumab trials. Hepatology. 2019;70:1913–27.
Bassegoda O, Olivas P, Turco L, et al. Decompensation in advanced non-alcoholic fatty liver disease may occur at lower hepatic venous pressure gradient levels than in patients with viral disease. Clin Gastroenterol Hepatol. 2021; https://doi.org/10.1016/j.cgh.2021.10.023.
Jindal A, Bhardwaj A, Kumar G, et al. Clinical decompensation and outcomes in patients with compensated cirrhosis and a hepatic venous pressure gradient >/=20 mmHg. Am J Gastroenterol. 2020;115:1624–33.
La Mura V, Abraldes JG, Raffa S, et al. Prognostic value of acute hemodynamic response to i.v. propranolol in patients with cirrhosis and portal hypertension. J Hepatol. 2009;51:279–87.
Mandorfer M, Kozbial K, Schwabl P, et al. Changes in hepatic venous pressure gradient predict hepatic decompensation in patients who achieved sustained Virologic response to interferon-free therapy. Hepatology. 2020;71:1023–36.
Turco L, Villanueva C, La Mura V, et al. Lowering portal pressure improves outcomes of patients with cirrhosis, with or without ascites: a meta-analysis. Clin Gastroenterol Hepatol. 2020;18:313–327.e6.
Abraldes JG, Garcia-Tsao G. Simple clinical tools to predict decompensation in patients with compensated cirrhosis: an unmet need. Clin Gastroenterol Hepatol. 2019;17:2179–81.
Guha IN, Harris R, Berhane S, et al. Validation of a model for identification of patients with compensated cirrhosis at high risk of decompensation. Clin Gastroenterol Hepatol. 2019;17:2330–2338.e1.
Colecchia A, Colli A, Casazza G, et al. Spleen stiffness measurement can predict clinical complications in compensated HCV-related cirrhosis: a prospective study. J Hepatol. 2014;60:1158–64.
Sebastiani G, Alshaalan R, Wong P, et al. Prognostic value of non-invasive fibrosis and steatosis tools, hepatic venous pressure gradient (HVPG) and histology in nonalcoholic steatohepatitis. PLoS One. 2015;10:e0128774.
Kitson MT, Roberts SK, Colman JC, et al. Liver stiffness and the prediction of clinically significant portal hypertension and portal hypertensive complications. Scand J Gastroenterol. 2015;50:462–9.
Merchante N, Rivero-Juarez A, Tellez F, et al. Liver stiffness predicts clinical outcome in human immunodeficiency virus/hepatitis C virus-coinfected patients with compensated liver cirrhosis. Hepatology. 2012;56:228–38.
Harrison SA, Abdelmalek MF, Caldwell S, et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis. Gastroenterology. 2018;155:1140–53.
Calzadilla-Bertot L, Vilar-Gomez E, Wong VW, et al. ABIDE: an accurate predictive model of liver decompensation in patients with nonalcoholic fatty liver-related cirrhosis. Hepatology. 2021;73(6):2238–50.
Younes R, Caviglia GP, Govaere O, et al. Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease. J Hepatol. 2021;75(4):786–94.
Vizzutti F, Arena U, Romanelli RG, et al. Liver stiffness measurement predicts severe portal hypertension in patients with HCV-related cirrhosis. Hepatology. 2007;45:1290–7.
Pons M, Augustin S, Scheiner B, et al. Noninvasive diagnosis of portal hypertension in patients with compensated advanced chronic liver disease. Am J Gastroenterol. 2021;116:723–32.
Robic MA, Procopet B, Metivier S, et al. Liver stiffness accurately predicts portal hypertension-related complications in patients with chronic liver disease: a prospective study. J Hepatol. 2011;55:1017–24.
Merchante N, Téllez F, Rivero-Juárez A, et al. Progression of liver stiffness predicts clinical events in HIV/HCV-coinfected patients with compensated cirrhosis. BMC Infect Dis. 2015;15:557.
Perez-Latorre L, Sanchez-Conde M, Rincon D, et al. Prediction of liver complications in patients with hepatitis C virus-related cirrhosis with and without HIV coinfection: comparison of hepatic venous pressure gradient and transient elastography. Clin Infect Dis. 2014;58:713–8.
Petta S, Sebastiani G, Viganò M, et al. Monitoring occurrence of liver-related events and survival by transient elastography in patients with nonalcoholic fatty liver disease and compensated advanced chronic liver disease. Clin Gastroenterol Hepatol. 2021;19:806–815.e5.
Eaton JE, Sen A, Hoodeshenas S, et al. Changes in liver stiffness, measured by magnetic resonance elastography, associated with hepatic decompensation in patients with primary sclerosing cholangitis. Clin Gastroenterol Hepatol. 2020;18:1576–83. e1
Osman KT, Maselli DB, Idilman IS, et al. Liver stiffness measured by either magnetic resonance or transient elastography is associated with liver fibrosis and is an independent predictor of outcomes among patients with primary biliary cholangitis. J Clin Gastroenterol. 2021;55:449–57.
Gidener T, Ahmed OT, Larson JJ, et al. Liver stiffness by magnetic resonance elastography predicts future cirrhosis, decompensation, and death in NAFLD. Clin Gastroenterol Hepatol. 2021;19(9):1915–1924.e6.
Han MAT, Vipani A, Noureddin N, et al. MR elastography-based liver fibrosis correlates with liver events in nonalcoholic fatty liver patients: a multicenter study. Liver Int. 2020;40:2242–51.
Colecchia A, Montrone L, Scaioli E, et al. Measurement of spleen stiffness to evaluate portal hypertension and the presence of esophageal varices in patients with HCV-related cirrhosis. Gastroenterology. 2012;143:646–54.
Abraldes JG, Bureau C, Stefanescu H, et al. Noninvasive tools and risk of clinically significant portal hypertension and varices in compensated cirrhosis: the “Anticipate” study. Hepatology. 2016;64:2173–84.
Costa D, Simbrunner B, Jachs M, et al. Systemic inflammation increases across distinct stages of advanced chronic liver disease and correlates with decompensation and mortality. J Hepatol. 2021;74:819–28.
Villanueva C, Albillos A, Genesca J, et al. Bacterial infections adversely influence the risk of decompensation and survival in compensated cirrhosis. J Hepatol. 2021;75(3):589–99.
Acknowledgement
Jaime Bosch supported in part by Stiftung für Leberkrankheiten, Bern, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this paper
Cite this paper
Tripathi, D., Villanueva, C., Bosch, J. (2022). Evaluation of the Effect of CSPH, Reduction of HVPG, and Other Factors Predicting the First Decompensation in Cirrhosis. In: de Franchis, R. (eds) Portal Hypertension VII. Springer, Cham. https://doi.org/10.1007/978-3-031-08552-9_35
Download citation
DOI: https://doi.org/10.1007/978-3-031-08552-9_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08551-2
Online ISBN: 978-3-031-08552-9
eBook Packages: MedicineMedicine (R0)