Abstract
Purpose of Review
To provide an updated overview of the existing and emerging non-invasive diagnostic methods to assess portal hypertension.
Recent Findings
Data on liver stiffness measurement confirmed that it is a mainstay for assessing the risk of clinically significant portal hypertension in patients with advanced chronic liver disease of any etiology. The Baveno criteria for identifying patients who can safely spare endoscopy have been validated in NASH and cholestatic liver disease. New expanded criteria and other simple non-invasive algorithms including MELD score or spleen stiffness have been proposed and can lead to a higher proportion of endoscopies without significantly increasing the risk of missing large esophageal varices. MR and CT improve the anatomical imaging of gastroesophageal varices and abdominal collaterals and dynamic imaging based on MR and able to quantify hepatic blood flow are in development. Contrast-enhanced ultrasound and methacetin breath test are emerging promising methods to estimate the HVPG non-invasively.
Summary
Several different non-invasive methods are now available and can be used in clinical practice to achieve a successful identification of patients with clinically significant portal hypertension in chronic liver disease. However, an exact estimation of HVPG is not available yet, and changes in portal pressure cannot yet be detected by non-invasive methods.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Portal hypertension (PH) is a common clinical syndrome, hemodynamically defined by an increase in the venous pressure gradient across the liver (calculated from its inflow through the portal vein versus its outflow through the hepatic veins) over 5 mmHg [1••].
Common complications of PH include the onset of gastroesophageal varices that can increase in size and rupture leading to gastrointestinal bleeding, ascites that can further complicate with bacterial infection due to bacterial translocation from the intestine (spontaneous bacterial peritonitis) and with renal failure (hepato-renal syndrome), porto-systemic shunting leading to hepatic encephalopathy, and hypersplenism leading to thrombo- and leukocytopenia [1••].
The major cause of PH in the Western countries is advanced chronic liver disease (ACLD)/liver cirrhosis, which accounts for over 90% of cases [2]. However, other causes (schistosomiasis, extrahepatic portal vein obstruction, porto-sinusoidal disease/idiopathic portal hypertension) are common in other geographical areas of the world and should be correctly identified.
Like any other vascular system, as stated by Ohm’s law, portal pressure depends upon two distinct factors: resistance to blood flow and the amount of flow (pressure = resistance × flow) [3].
The initial factor leading to the increase in portal pressure is invariably an increase in resistance to portal blood flow. This can arise at any level, i.e., at the pre-hepatic (portal vein system), intrahepatic (pre-sinusoidal, sinusoidal, or post-sinusoidal site), or post-hepatic (liver veins, inferior vena cava, right heart) level (Table 1).
In cirrhosis, the increase in intrahepatic resistance occurs at a sinusoidal site, due to the structural damage through fibrogenesis, parenchymal extinction, and regeneration [2]. Once PH has developed, an adaptive increase in portal blood flow and subsequently development of porto-systemic collaterals and onset of hyperdynamic circulatory syndrome lead to further increase in portal pressure [4].
In patients with compensated ACLD, the onset of PH marks an important moment of the natural history of the disease, characterized by a significant risk of clinical complications (decompensation) [1••]. However, patients are asymptomatic in this stage and PH must be looked for with specific diagnostic methods [1••, 5••]. On the other hand, in patients in the decompensated stage of cirrhosis, PH is invariably present and diagnosis is clinical. However, patients with decompensated cirrhosis have a high risk of bearing varices that require therapy, and upper gastrointestinal endoscopy is always needed in this population [1••]. Endoscopy remains the reference method to determine the presence and aspect of esophageal and gastric varices, which relate to their risk of rupturing: size, red color signs, and wale marks [1••].Importantly, it has been proven that drugs achieving a decrease in portal pressure are able to avoid the complications of the syndrome, so changing the natural history of the syndrome [1••].
Reference Standard for Portal Hypertension in ACLD: Hepatic Venous Pressure Measurement
In ACLD, the definitive diagnosis and staging of PH are based on hepatic venous pressure gradient (HVPG) measurement, which is considered the reference standard for the estimation of portal pressure. The HVPG is measured on invasive hepatic vein catheterization as the difference between the occlusion pressure (equal to portal pressure in sinusoidal causes of PH) and the free pressure in a main hepatic vein. An HVPG of up to 5 mmHg is considered normal; subclinical PH is defined by an HVPG of 6–9 mmHg; and an HVPG ≥ 10 mmHg represents the clinically significant PH threshold (CSPH), above which gastroesophageal varices can form and the complications of the syndrome can occur [2]. Consequently, an early identification of portal hypertension, ideally before complications have occurred, should be a key aspect of management of patients with compensated ACLD of any etiology.
Patients with compensated ACLD should be screened for the presence of CSPH, and patients with CSPH constitute the population that should undergo endoscopy to screen for the presence of varices at risk of bleeding [1••].
Severe PH (HVPG ≥ 12 mmHg) and very severe PH (HVPG ≥ 16 mmHg) are associated with an increase of variceal bleeding and mortality, respectively, and these thresholds represent additional important endpoints to be identified [1••].
While worsening of HVPG is associated with worsening of prognosis, improvement of portal hypertension is associated with improved prognosis. Specifically, a reduction in HVPG to < 12 mmHg, or by at least of 10–20% of the baseline values, is necessary to obtain clinical efficacy of drugs or non-pharmacological approaches to portal hypertension [1••, 6, 7].
In patients presenting with signs of PH of unknown origin, tests should be aimed at identifying the most likely cause (Table 1), and it must be underlined that HVPG measurement has no value in patients with pre-sinusoidal and pre-hepatic portal hypertension. Yet, the detection of a normal or near-normal HVPG in patients with overt clinical signs of PH can help in the differential diagnosis of complex cases, being the final diagnosis based on histology.
As explained above, HVPG measurement and endoscopy are the reference methods to evaluate PH in CLD. However, they are invasive, expensive, require a specific expertise, and may rarely lead to complications. Non-invasive diagnostic methods that can be used reliably to determine the presence and estimate the severity of PH have been a major research topic in hepatology for at least 30 years. The development of simple, non-invasive methods enabling accurate and rapid diagnosis of patients with a low risk of CSPH and varices requiring treatment (who could avoid invasive tests), and patients with CSPH (at high risk of complications and varices, requiring further testing), has become closer to clinical practice in the last year, fostering further the advancement of personalized medicine in this field. Figure 1 schematically represents the rationale of non-invasive diagnostic methods commonly used for portal hypertension.
Existing Non-invasive Methods for the Assessment of Portal Hypertension
Laboratory Tests
Simple, readily available laboratory parameters related to liver synthetic function, hypersplenism, and remodeling of the extracellular matrix have been studied in the context of the diagnosis of portal hypertension and EV. A decrease in platelet count is the most commonly reported sign of portal hypertension in compensated ACLD, and platelet count alone or in combination with other unrelated tests (e.g., spleen size, liver stiffness, portal vein velocity on Doppler, and Lok index [8]) should be used in clinical practice to identify patients who can safely avoid endoscopy due to a very low risk of varices requiring treatment [5••]. However, normal platelet count can be occasionally observed in patients with CSPH, and the correlation between platelet count and HVPG does not allow accurately extrapolating the severity of PH.
As for the other available serum markers or parameters, while a Child-Pugh score over 6 points might suffice to suggest the presence of CSPH, none of the available tests are accurate enough to rule-in or rule-out varices needing treatment.
Ultrasound and Ultrasound-Doppler
Several anatomical changes occurring in patients with ACLD and portal hypertension can be studied by ultrasound imaging [9, 10]. In patients with typical signs of cirrhosis (nodular liver surface, heterogeneous echo pattern of the liver), the portal vein can show an increased diameter; dilatation over 13 mm is associated with an increased risk of large varices, and this has been used in combination with platelet count in several studies [11]. The presence of porto-systemic collateral circulation (patent paraumbilical vein, spontaneous spleno-renal collaterals, dilated left gastric vein, and short gastric vein, etc.) can be considered a 100% specific sign of CSPH, even if the sensitivity of the test is low. Reversal of blood flow (hepatofugal flow) in the portal vein is similarly a highly specific sign of portal hypertension, usually indicating the presence of large extrahepatic porto-systemic collaterals “stealing” portal blood flow [10]. Doppler ultrasound signs of PH include reduced portal vein blood velocity and increased intrahepatic and intrasplenic arterial resistance index; when used in combination with simpler parameter, specificity for the diagnosis of CSPH is > 80%, but sensitivity does not exceed 40–70%, in compensated patients [10]. None of the abovementioned parameters are sufficiently exact to allow a good estimation of the exact value of the HVPG, nor their change parallels change in HVPG on pharmacological therapy. In the authors’ experience, portal vein velocity decreases significantly in patients undergoing therapy with NSBB, and the lack of decrease in this parameter should strongly suggest a lack of compliance.
Doppler ultrasound is the method of choice to follow up patients who underwent TIPS placement [12]. Portal vein blood velocity, direction of the flow in the intrahepatic branches of the portal vein, and blood velocity within the TIPS stent should be monitored to detect TIPS dysfunction and indicate invasive TIPS revision before the onset of clinical events.
Liver and Spleen Stiffness Measured by Ultrasound Elastography and their Combination with Other Parameters
Al tissues have intrinsic mechanical/elastic properties that can be measured by distorting the tissue and evaluating its response. The term “ultrasound elastography” groups the techniques using ultrasound to detect the velocity of the microdisplacements (shear waves) induced in the tissue [13•]. Since liver fibrosis is the major determinant of the increased hepatic resistance, and consequently of portal pressure in patients with ACLD, liver stiffness measured by elastography has been studied as a possible surrogate of portal hypertension [14•].
Most of the experience in this field has been obtained using vibration-controlled transient elastography (TE, FibroScan®). After transmitting a vibration to the liver, the measurement of the shear wave displacement is obtained by an ultrasound beam on the tip of the probe and is reported in kilo Pascals (kPa).
Liver stiffness measurement (LSM) shows a close correlation with HVPG in compensated patients [15]. The degree of correlation is optimal up to 12 mmHg, while it significantly decreases in patients with higher HVPG. This is likely due to the fact that increase in blood flow following the onset of PH cannot be sensed by LSM, which mostly mirrors intrahepatic resistance. Nonetheless, LSM enables an accurate discrimination between patients with and without CSPH (AUROC > 0.90), particularly if combined to platelet count and even more if spleen size is considered [16, 17]. The consensus conference on PH held in Baveno, Italy, in 2015 agreed that the values of LSM > 20 kPa are strongly suggestive of CSPH, particularly in patients with viral etiology of liver disease [5••]. Consequently, patients with LSM < 20 kPa and normal platelet count (> 150 G/L) can safely skip endoscopy, since their risk of having varices needing treatment is below 5%. Several recent studies validated these “Baveno VI criteria” in different etiologies, including NASH and cholestatic liver disease, and in different geographical areas [18•, 19•, 20]. Furthermore, recent data suggest that the Baveno VI criteria are quite conservative, allowing to skip not more than 20–25% of endoscopies, but they can be safely expanded by allowing a LSM up to 25 kPa and a platelet count above 110 G/L, increasing the spared endoscopies to 40% with a moderate increase in the proportion of missed varices [21]. Other proposed strategies to increase the proportion of spared endoscopies include the use of MELD score or spleen stiffness in combination with platelet count and/or liver stiffness [22].
Importantly, LSM indicating the presence of CSPH predicts the onset of clinical decompensation with an accuracy similar to that of HVPG [23, 24].
It should be underlined that in patients with cirrhosis and CSPH who underwent successful treatment of HCV, LSM markedly decreases after treatment and sustained virological response; despite this, CSPH persists after treatment in up to 70% after 1 year [25••]. Thus, LSM results should be taken with caution in these patients, and currently, no firm conclusion regarding fibrosis stage and regression of portal hypertension based on post-treatment LSM should be taken.
Data regarding the correlation between LSM changes and HVPG changes are scarce and seem to indicate that LSM is not adequate to follow up portal hypertension. However, recent data show that LSM decreases significantly after TIPS in patients with cirrhosis not developing post-TIPS liver failure, but the data require validation [26].
Newer ultrasound elastography methods are available on modern ultrasound devices, are based on acoustic radiation force impulse (ARFI), and focus on high-intensity short-duration acoustic pulses to generate the tissue displacement, either at one point (point shear wave elastography, pSWE) or in larger areas (two-dimensional shear wave elastography, 2D-SWE) [13•]. The main advantage is due to the possibility of selecting the liver stiffness measurement point in real time.
Despite the quality criteria for the correct interpretation of results not yet completely defined, the available evidence on the two most commonly available systems in the market suggest that the diagnostic performance for the assessment of portal hypertension is similar to that of TE with AUROCs of 0.82–0.90 [14•].
Spleen stiffness measurement (SSM) has been proposed as a more precise method to assess portal pressure. Since long, it is known that the spleen undergoes parenchymal remodeling in patients with PH, often showing as splenomegaly. This is due to passive congestion and increased arterial inflow and enhanced angiogenesis and fibrogenesis. Using TE, SSM showed an accuracy similar or superior to that of LSM to diagnose CSPH, varices needing treatment, and to predict clinical events [14•]. In the authors’ experience, SSM is particularly useful in patients having LSM in the “gray” zone, between 15 and 20 kPa, where the discrimination between those with and without PH is most difficult. In these patients, the finding of SSM > 54 kPa is in our experience a useful hint of CSPH. In addition, in patients with non-cirrhotic portal hypertension who by definition have normal LSM, SSM well correlated with the presence of gastroesophageal varices [27]. Finally, recent data show that SSM might reflect the improvement of portal pressure after TIPS placement (confirmed in our experience) [26].
The limitations of LSM and SSM by TE, pSWE and 2D-SWE have been reviewed elsewhere; it is important to underline that LSM should be considered reliable only in the absence of factors inducing an increase in liver stiffness independent of fibrosis (venous congestion, acute hepatic inflammation, meal ingestion, obstructive cholestasis) [13•]. In addition, as for TE, no specific probe is commercially available for SSM, and this limits the possibility of measuring SSM to patients with splenomegaly.
Computerized Tomography– and Magnetic Resonance Imaging–Based Parameters
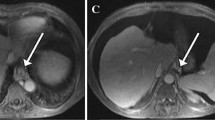
Contrast-enhanced CT and MRI of the abdomen provide high-quality images of the portal venous system and of porto-systemic collaterals and are potentially useful in the identification of patients with CSPH. In a recent systematic review and meta-analysis of the existing observational data, CT had an AUROC of 0.898 for diagnosing varices of any size and of 0.949 for high-risk varices [28]. Multi-detector CT had the highest performance. Despite this data not validated in prospective and well-conducted studies, in the opinion of the authors’ of this review, it is logical that any porto-systemic collateral visualized by any imaging method should suffice to confirm the presence of CSPH, and to suspect the presence of gastroesophageal varices, which are more common in patients with porto-systemic collaterals of any kind [29, 30]. Therefore, in patients with compensated ACLD who require CT or MR due to concomitant morbidity, a careful examination of the portal venous phases to identify or exclude the presence of porto-systemic collateral should be performed. Future data will address whether portal pressure estimation by using computational fluid dynamic modeling, which has been postulated, can be reliably obtained in human subjects [31].
Different magnetic resonance imaging and elastography (MRE) techniques have been tested in patients with ACLD and suspected PH. Encouraging but limited results regarding the correlation between HVPG and liver and spleen stiffness on MRE, as well as dynamic contrast-enhanced perfusion parameters (e.g., liver upslope), and quantitative magnetic resonance imaging [32, 33, 34•] exist. However, no head-to-head comparison to simpler methods (e.g., ultrasound elastography) is available. In addition, the limited sample size and design of the published studies do not allow concluding about the utility of these methods in real-life scenarios, and further studies are needed.
New Promising Methods Not Yet Fully Validated
Contrast-Enhanced Ultrasound
Ultrasound contrast agents (UCAs) consist in microbubbles of inert gas stabilized into a lipid/phospholipid shell. Due to their acoustic properties, microbubbles enhance the ultrasound signal and once injected in a peripheral vein they behave as intravascular agents, allowing the visualization of micro- and macrovessels in real-time. Currently, three UCAs are available for the study of the liver according to the different geographic regions: SonoVue® (sulfur hexafluoride; Bracco, Switzerland), which is authorized in Europe; Definity® (octafluoropropane; Lantheus Medical Imaging, Billerica, MA, USA), and Sonazoid® (perfluorobutane; GE Healthcare, UK Ltd), which is mostly used in Asia, and is the only one showing a parenchymal phase.
The most common indication for the use of contrast-enhanced ultrasound (CEUS) in the liver is characterization of focal lesions [35]. In addition, CEUS is already used routinely to improve the results of ultrasound and Doppler ultrasound in specific complications of portal hypertension. This includes the confirmation of portal vein thrombosis in patients with difficult Doppler assessment, the differential diagnosis of bland thrombosis from malignant portal vein invasion, and further assessment of suspected TIPS dysfunction.
In the last 10 years, CEUS is being increasingly studied as a potential method to assess portal hypertension. As previously mentioned, increase in porto-collateral blood flow and hyperdynamic systemic circulation follows the onset of CSPH and is not well detected by elastography. CEUS allows measuring the arrival time of contrast in different vessels of the liver, and as such can provide data on the presence of hyperdynamic circulation and portal hypertension. Hepatic veins arrival time (HVAT) of SonoVue showed a linear significant correlation with HVPG in one study including patients with cirrhosis (n = 71, R2 = 0.56, p < 0.001) [36]. Using this method, CSPH could be detected with high discriminative ability (AUROC 0.97) and the suggested that a cut-off of 14 s had a sensitivity > 90% with a specificity > 80% for this diagnosis. The results were validated in an independent group of 35 patients and were similar.
Dynamic CEUS using the disruption-reperfusion technique was used to estimate regional hepatic perfusion (RHP) [37]. This showed a weak albeit significant correlation with liver function and HVPG, providing a proof of concept about the potential of this technique to estimate parenchyma perfusion. In the authors’ opinion, a volumetric assessment in real time (4D DCE-US) would likely improve the accuracy of measurements and its correlation with portal pressure.
Based on the concept that the liver vascular network anatomy is progressively disrupted in cirrhosis, and that this explains the onset of portal hypertension, an objective measurement of the degree of derangement of the liver vascular network using DCE-US could closely mirror the HVPG. Graph analysis of the liver DCE-US proved feasible and led to modeling the clustering coefficients of “vascular connectomes” in a preliminary study [38]. Patients with cirrhosis had a lower clustering coefficient indicating disruption of normal anatomy, and this parameter inversely correlated with HVPG, with an excellent correlation coefficient (R = 0.977; MRSE = 1.57). A large European cooperative study (the CLEVER study) has been carried on to validate the results and creating automatic software for the analysis of DCE-US images in this field. Its preliminary results have been presented at the International Liver Congress in 2018. The DCE-US-based software showed a suboptimal applicability, but in patients with reliable measurements, the predicted HVPG and the measured HVPG showed a very good correlation (R = 0.834, p < 0.0001).
The amplitude of ultrasound waves of the subharmonic signal emitted by the microbubbles led to the development of another CEUS-based method. It has been shown that if the microbubbles are contained in a liquid (such as blood), their subharmonic signal amplitude decreases linearly when pressure of the surrounding fluid increases. Therefore, by measuring the subharmonic signals amplitude of microbubbles, the pressure of liquid surrounding them in different points of a vascular system can be estimated and by processing them through an adequate mathematical modeling [39]. This approach, named SHAPE (SubHarmonic Aided Pressure Estimation) was used by Eisenbrey et al. in patients with cirrhosis (n = 45) [40]. The subharmonic signal gradient was calculated as the difference between the portal vein and the hepatic vein subharmonic signals gradient and compared with the HVPG. The estimated pressure gradient showed an excellent correlation with HVPG (R2 = 0.82) and an over 90% accurate cut-off for CSPH could be identified. These results are currently being validated in a large multicentric study conducted in the USA.
In the authors’ opinion, CLEVER and SHAPE methods are very promising and could bring DCE-US/CEUS close to clinical practice in the assessment of portal hypertension.
13C–Methacetin Breath Test
13C is a non-radioactive, stable isotope, which can be incorporated into substrates; once metabolized by the liver microsomes, it will be released as 13CO2 and as such it can be detected in breath using a spectrophotometer device. Breath tests using methacetin (MBT) marked with 13C, administered either orally or i.v., have been developed, since marked methacetin would be exclusively metabolized by the liver and would lead to the following equation:
The MBT measures an important metabolic function which reflects the degree of overall liver impairment [41]. Therefore, since portal pressure typically correlates with poorer liver function, the 13C–methacetin breath test (MBT) has been tested for the prediction of CSPH. A model based on MBT had an AUROC of 0.881 to identify CSPH in patients with NASH. In the authors’ opinion, MBT represents an interesting novel tool that could complement other tests for portal pressure assessment (e.g., ultrasound, liver stiffness, and spleen stiffness) in patients with compensated advanced chronic liver disease. In particular, the use of MBT to predict non-invasively the HVPG response to NSBB would be of great interest for the hepatology community, since this remains a major unmet need in the field.
Conclusion
As discussed in this review, several different non-invasive methods are now available and can be used in clinical practice to achieve a successful identification of patients with clinically significant portal hypertension in chronic liver disease. However, several challenges remain a field open for research. In particular, an exact estimation of HVPG is not available yet, and changes in portal pressure cannot yet be detected by non-invasive methods. In patients with extrahepatic portal vein obstruction, the only promising method available is spleen stiffness measurement, but prospective validation against clinically relevant outcomes is needed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310–35 Practical evidence-based guidance on the modern management of portal hypertension.
Berzigotti A, Seijo S, Reverter E, Bosch J. Assessing portal hypertension in liver diseases. Expert Rev Gastroenterol Hepatol. 2013;7(2):141–55.
Bosch J. Vascular deterioration in cirrhosis: the big picture. J Clin Gastroenterol. 2007;41(Suppl 3):S247–53.
Berzigotti A, Bosch J. Pharmacologic management of portal hypertension. Clin Liver Dis. 2014;18(2):303–17.
•• de Franchis R, Baveno VI. Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52 Summary of the most recent international consensus conference on portal hypertension.
D'Amico G, Garcia-Pagan JC, Luca A, Bosch J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: a systematic review. Gastroenterology. 2006;131(5):1611–24.
Procopet B, Berzigotti A. Diagnosis of cirrhosis and portal hypertension: imaging, non-invasive markers of fibrosis and liver biopsy. Gastroenterol Rep. 2017;5(2):79–89.
Thiele M, Madsen BS, Procopet B, Hansen JF, Moller LM, Detlefsen S, et al. Reliability criteria for liver stiffness measurements with real-time 2D shear wave elastography in different clinical scenarios of chronic liver disease. Ultraschall Med 2017;38(6):648–654.
Berzigotti A, Piscaglia F. Ultrasound in portal hypertension--part 1. Ultraschall Med. 2011;32(6):548–68 quiz 69-71.
Berzigotti A, Piscaglia F, Education E, Professional Standards C. Ultrasound in portal hypertension--part 2--and EFSUMB recommendations for the performance and reporting of ultrasound examinations in portal hypertension. Ultraschall Med. 2012;33(1):8–32 quiz 0-1.
Schepis F, Camma C, Niceforo D, Magnano A, Pallio S, Cinquegrani M, et al. Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection? Hepatology. 2001;33(2):333–8.
Abraldes JG, Gilabert R, Turnes J, Nicolau C, Berzigotti A, Aponte J, et al. Utility of color Doppler ultrasonography predicting tips dysfunction. Am J Gastroenterol. 2005;100(12):2696–701.
• Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, et al. EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, Update 2017 (Long Version). Ultraschall Med. 2017;38(4):e48 Updated guidelines on the use of elastography in liver disease.
• Berzigotti A. Non-invasive evaluation of portal hypertension using ultrasound elastography. J Hepatol. 2017;67(2):399–411 Updated summary on the use of elastography for portal hypertension.
Vizzutti F, Arena U, Romanelli RG, Rega L, Foschi M, Colagrande S, et al. Liver stiffness measurement predicts severe portal hypertension in patients with HCV-related cirrhosis. Hepatology. 2007;45(5):1290–7.
Shi KQ, Fan YC, Pan ZZ, Lin XF, Liu WY, Chen YP, et al. Transient elastography: a meta-analysis of diagnostic accuracy in evaluation of portal hypertension in chronic liver disease. Liver Int. 2013;33(1):62–71.
Berzigotti A, Seijo S, Arena U, Abraldes JG, Vizzutti F, Garcia-Pagan JC, et al. Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Gastroenterology. 2013;144(1):102–11 e1.
• Petta S, Sebastiani G, Bugianesi E, Vigano M, Wong VW, Berzigotti A, et al. Noninvasive prediction of esophageal varices by stiffness and platelet in nonalcoholic fatty liver disease cirrhosis. Journal of hepatology. J Hepatol. 2018;69(4):878–85 First validation of the Baveno non-invasive criteria for avoiding endoscopy in patients with NASH.
• Moctezuma-Velázquez C, Saffioti F, Tasayco-Huamán S, Casu S, Mason A, Roccarina D.V, et al. Non-invasive prediction of high-risk varices in patients with primary biliary cholangitis and primary sclerosing cholangitis. Am J Gastroenterol 2018. https://doi.org/10.1038/s41395-018-0265-7 First validation of the Baveno non-invasive criteria for avoiding endoscopy in patients with cholestatic liver disease.
Bae J, Sinn DH, Kang W, Gwak GY, Choi MS, Paik YH, et al. Validation of the Baveno VI and the expanded Baveno VI criteria to identify patients who could avoid screening endoscopy. Liver Int. 2018;38(8):1442–8.
Augustin S, Pons M, Maurice JB, Bureau C, Stefanescu H, Ney M, et al. Expanding the Baveno VI criteria for the screening of varices in patients with compensated advanced chronic liver disease. Hepatology. 2017;66(6):1980–8.
Colecchia A, Ravaioli F, Marasco G, Colli A, Dajti E, Di Biase AR, et al. A combined model based on spleen stiffness measurement and Baveno VI criteria to rule out high-risk varices in advanced chronic liver disease. J Hepatol. 2018;69(2):308–17.
Robic MA, Procopet B, Metivier S, Peron JM, Selves J, Vinel JP, et al. Liver stiffness accurately predicts portal hypertension related complications in patients with chronic liver disease: a prospective study. J Hepatol. 2011;55(5):1017–24.
Margini C, Murgia G, Stirnimann G, De Gottardi A, Semmo N, Casu S, et al. Prognostic significance of controlled attenuation parameter in patients with compensated advanced chronic liver disease. Hepatol Commun. 2018;2(8):929–40.
•• Lens S, Alvarado-Tapias E, Marino Z, Londono MC, LL E, Martinez J, et al. Effects of all-Oral anti-viral therapy on HVPG and systemic hemodynamics in patients with hepatitis C virus-associated cirrhosis. Gastroenterology. 2017;153(5):1273–83 e1 Detailed description of portal pressure changes after modern antiviral therapy of HCV.
Jansen C, Moller P, Meyer C, Kolbe CC, Bogs C, Pohlmann A, et al. Increase in liver stiffness after transjugular intrahepatic portosystemic shunt is associated with inflammation and predicts mortality. Hepatology. 2018;67(4):1472–84.
Sharma P, Mishra SR, Kumar M, Sharma BC, Sarin SK. Liver and spleen stiffness in patients with extrahepatic portal vein obstruction. Radiology. 2012;263(3):893–9.
Deng H, Qi X, Guo X. Computed tomography for the diagnosis of varices in liver cirrhosis: a systematic review and meta-analysis of observational studies. Postgrad Med. 2017;129(3):318–28.
Simon-Talero M, Roccarina D, Martinez J, Lampichler K, Baiges A, Low G, et al. Association between portosystemic shunts and increased complications and mortality in patients with cirrhosis. Gastroenterology. 2018;154(6):1694–705 e4.
Berzigotti A, Rossi V, Tiani C, Pierpaoli L, Zappoli P, Riili A, et al. Prognostic value of a single HVPG measurement and Doppler-ultrasound evaluation in patients with cirrhosis and portal hypertension. J Gastroenterol. 2011;46(5):687–95.
Rohan E, Lukes V, Jonasova A. Modeling of the contrast-enhanced perfusion test in liver based on the multi-compartment flow in porous media. J Math Biol. 2018;77(2):421–54.
Kihira S, Kagen AC, Vasudevan P, Jajamovich GH, Schiano TD, Andrle AF, et al. Non-invasive prediction of portal pressures using CT and MRI in chronic liver disease. Abdom Radiol. 2016;41(1):42–9.
Wagner M, Hectors S, Bane O, Gordic S, Kennedy P, Besa C, et al. Noninvasive prediction of portal pressure with MR elastography and DCE-MRI of the liver and spleen: preliminary results. J Magn Reson Imaging: JMRI. 2018;48(4):1091–1103.
• Palaniyappan N, Cox E, Bradley C, Scott R, Austin A, O'Neill R, et al. Non-invasive assessment of portal hypertension using quantitative magnetic resonance imaging. J Hepatol. 2016;65(6):1131–9 Proof of concept study showing the potential of quantitative MRI to assess portal pressure.
Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34(1):11–29.
Kim MY, Suk KT, Baik SK, Kim HA, Kim YJ, Cha SH, et al. Hepatic vein arrival time as assessed by contrast-enhanced ultrasonography is useful for the assessment of portal hypertension in compensated cirrhosis. Hepatology. 2012;56(3):1053–62.
Berzigotti A, Nicolau C, Bellot P, Abraldes JG, Gilabert R, Garcia-Pagan JC, et al. Evaluation of regional hepatic perfusion (RHP) by contrast-enhanced ultrasound in patients with cirrhosis. J Hepatol. 2011;55(2):307–14.
Amat-Roldan I, Berzigotti A, Gilabert R, Bosch J. Assessment of hepatic vascular network connectivity with automated graph analysis of dynamic contrast-enhanced US to evaluate portal hypertension in patients with cirrhosis: a pilot study. Radiology. 2015;277(1):268–76.
Halldorsdottir VG, Dave JK, Leodore LM, Eisenbrey JR, Park S, Hall AL, et al. Subharmonic contrast microbubble signals for noninvasive pressure estimation under static and dynamic flow conditions. Ultrason Imaging. 2011;33(3):153–64.
Eisenbrey JR, Dave JK, Halldorsdottir VG, Merton DA, Miller C, Gonzalez JM, et al. Chronic liver disease: noninvasive subharmonic aided pressure estimation of hepatic venous pressure gradient. Radiology. 2013;268(2):581–8.
Stravitz RT, Reuben A, Mizrahi M, Lalazar G, Brown K, Gordon SC, et al. Use of the methacetin breath test to classify the risk of cirrhotic complications and mortality in patients evaluated/listed for liver transplantation. J Hepatol. 2015;63(6):1345–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ahmed M.Elmahdy and Annalisa Berzigotti each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Management of Cirrhotic Patient
Rights and permissions
About this article
Cite this article
Elmahdy, A.M., Berzigotti, A. Non-invasive Measurement of Portal Pressure. Curr Hepatology Rep 18, 20–27 (2019). https://doi.org/10.1007/s11901-019-00446-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-019-00446-4