Abstract
Purpose of the Review
Left ventricular non-compaction (LVNC) is characterised by prominent left ventricular trabeculae and deep inter-trabecular recesses. Although considered a distinct cardiomyopathy, prominent trabeculations may also be found in other cardiomyopathies, in athletes or during pregnancy. Clinical presentation includes heart failure symptoms, systemic embolic events, arrhythmias and sudden cardiac death. Currently, LVNC diagnosis relies on imaging criteria, and clinicians face several challenges in the assessment of patients with prominent trabeculations. In this review, we summarise the available information on the role of the ECG in the diagnosis and management of LVNC.
Recent Findings
ECG abnormalities have been reported in 75–94% of adults and children with LVNC. The lack of specificity of these ECG abnormalities does not allow (in isolation) to diagnose the condition. However, when considered in a set of diagnostic criteria including family history, clinical information, and imaging features, the ECG may differentiate between physiological and pathological findings or may provide clues raising the possibility of specific underlying conditions. Finally, some ECG features in LVNC constitute ominous signs that require a stricter patient surveillance or specific therapeutic measures.
Summary
The ECG remains a cornerstone in the diagnosis and management of patients with cardiomyopathies, including LVNC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Left ventricular non-compaction (LVNC) is a cardiomyopathy characterised by prominent left ventricular trabeculae and deep inter-trabecular recesses. While the European Society of Cardiology includes LVNC in the unclassified cardiomyopathies group, the American Heart Association defines LVNC as a genetic cardiomyopathy [1, 2]. The diagnosis of LVNC relies on a double-layered myocardial architecture demonstrating a non-compacted myocardium with deep trabeculations and a thin compacted epicardial layer. Imaging techniques, such as echocardiography and cardiovascular magnetic resonance (CMR) are the main diagnostic tools in this setting. The commonly used imaging diagnostic criteria are mainly based on the ratio between the non-compacted and the compacted layer of the ventricular myocardium [3]. However, there are currently no gold standard echocardiographic or CMR criteria for the diagnosis of LVNC [4]. The diagnosis of LVNC remains challenging, reflecting the lack of stringent criteria for the definition of this condition. Prominent trabeculations (the characterising feature of the disease) may be physiological in athletes or during certain stages of pregnancy or may be commonly found in other cardiomyopathies (e.g. dilated, hypertrophic, arrhythmogenic), congenital heart diseases or as part of inherited genetic multiorgan diseases such as Barth syndrome [4,5,6,7,8]. Practical consequences linked to this diagnostic variability emerge in the high prevalence of “spongy myocardium” phenotypes observed in echocardiographic laboratories or CMR units, often resulting in an overinterpretation of clinical findings that may be physiological [9]. While data from the European Cardiomyopathy Pilot Registry report LVNC prevalence of 3.2%, this prevalence is even higher (9.2%) in children according to the National Australian Childhood Cardiomyopathy Study [10, 11]. The overall prevalence of LVNC seems to be much higher when considering a specific subset of patients and certain ethnicities [3, 9, 12]. The spectrum of clinical presentation is wide, depending for example on whether LVNC occurs in isolation or in the context of a complex genetic syndrome. Overall, the clinical key features (classic triad) include heart failure symptoms (as the result of ventricular systolic/diastolic dysfunction), systemic embolic events and ventricular arrhythmias [4]. Life-threatening arrhythmias were reported in more than 20% of the patients and sudden cardiac death (SCD) is a matter of concern [4]. In this context, the electrocardiogram (ECG) may be a relevant tool in the assessment of patients with possible or ascertained LVNC. Its use may be particularly relevant in differentiating between physiological and pathological changes, but also in prognostic stratification and clinical management (Fig. 1). In this review, we will discuss the role of the ECG in the clinical approach to patients with LVNC. The ECG might be a useful tool, especially in situations where the increasing amount of information (often with findings of uncertain significance) derived from other more advanced diagnostic techniques does not provide practical support for clinical choices.
Electrocardiographic abnormalities in patients with different LVNC structural phenotypes on cardiac magnetic resonance imaging. (a) ECG fulfills voltage criteria for left ventricular hypertrophy; deep T-wave inversion in leads V4–V6 with associated ST segment depression; minor T-wave inversion in leads I, II, avL and aVF; biphasic T-wave noted in lead 3 with a proceeding convex ST segment. (b) Left axis deviation with minor T-wave inversion in lateral leads (leads I, aVL, V4–V6). (c) Minor T-wave inversion in V1–V3. (d) Fragmentation of QRS morphology in leads III, V3 and V4. (e) Minor T-wave inversion in leads II, III, aVF and V4–V6. There is also an isolated ventricular extra-systole. (f) Normal ECG with no repolarization changes. (g) Deep R/S complexes in leads V2–V3
Methods
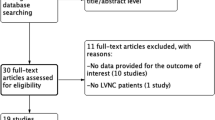
The following research question was addressed: What is the role of the ECG in the diagnosis and management of LVNC? A search through the web-based engine PubMed was conducted to identify all studies relevant to the topic. Due to the lack of studies specifically focussing on the ECG and the complexity of the disease in terms of diagnostic criteria, we considered all literature on LVNC that reported on the ECG including research papers, reviews, case series and reports. Table 1 summarises sample characteristics and key findings in manuscripts of particular importance that were considered in this review.
Systematic Approach in ECG Interpretation
ECG abnormalities are frequently observed in patients with LVNC, ranging from 75 to 94% in adults and children [13,14,15,16,17,18,19,20]. When interpreting the ECG, the recognition of specific “red flags” should be carefully integrated into the broader clinical and familial context (Table 2).
P Wave
Although the left ventricle (LV) is the chamber predominantly affected by LVNC, the atria may also be involved. This would be a consequence of LV involvement with diastolic dysfunction and subsequent left atrial (LA) dilatation [21]. These changes may be reflected in the ECG with broad or peaked P waves [13, 17, 22]. Sinus node dysfunction and sinus bradycardia can be the initial manifestations in some patients with LVNC [17, 23].
PR Interval
Conduction abnormalities such as first-degree and advanced atrio-ventricular (AV) block are found in a variable percentage (3–25%) of patients with LVNC [17, 19, 24]. In a study by Steffel et al., conduction abnormalities were associated with a reduced LV ejection fraction (LVEF), LV and LA dilatation and congestive heart failure (HF) [22]. Conduction abnormalities have also been observed in children with LVNC when compared to age-matched healthy individuals, with a prolonged PR interval observed in LVNC (136 ± 28 ms vs 105 ± 16 ms, p < 0.001) [17].
The QRS Complex
Structural abnormalities of the LV (and sometimes of both ventricles) and the possible involvement of the conduction tissue are both reflected on the QRS complex. ECG voltage criteria of left or bi-ventricular hypertrophy are reported in > 40% of patients, and extremely high QRS voltages have been described in children with LVNC [17,18,19,20, 22, 24, 25]. Steffel et al. showed a higher prevalence of systemic embolic events among patients with ECG signs of left ventricular hypertrophy [22]. In a recent bi-centric retrospective study involving 305 patients and investigating the relationships between QRS duration and left ventricular (LV) mass in subtypes of abnormal LV wall thickness for differentiation of hypertrophic cardiomyopathy (HCM) from other forms of LV hypertrophy, QRS duration increased in the subgroup (n = 28) of patients with LVNC (rho 0.40, p = 0.007 on bivariate regression between QRS duration and LV mass), while a reverse relationship was present in patients with HCM [26]. Bundle branch blocks (especially left bundle branch block — LBBB) are a common finding in adult patients with LVNC (over 40% of cases), while they are rare in children [13,14,15,16,17, 19]. Intraventricular conduction delay (particularly LBBB) is associated with reduced systolic function, heart failure and left ventricular dilation [15, 17]. The presence of fragmented QRS (fQRS) though non-specific has also been described in LVNC. A study by Ning et al. suggested that the presence of fragmented QRS was associated with a significantly lower survival rate [27].
ST Segment/T Wave Abnormalities
Repolarization abnormalities are reported in over 70% of all cases. The most common findings are ST-segment depression and negative or flat T waves, especially in the inferior and lateral leads [15, 17, 22]. A positive T wave in aVR lead is also commonly described (up to 40% of cases) [28•]. In a study by Caliskan et al., an early repolarization pattern was a common finding in LVNC, especially in subjects presenting with malignant ventricular arrhythmias and inferior or inferolateral pattern and horizontal/descending type seems to be associated with higher risk of poor outcomes [29]. Interestingly, a Brugada ECG pattern has been reported in 3.2% of Japanese patients with LVNC, with a significantly higher prevalence compared to the general population [30].
QT Interval
Several studies have shown that patients with LVNC may exhibit a prolonged QTc interval. Stöllberger et al. found a QTc interval > 440 ms in 38% of patients with LVNC [19]. Similarly, Steffel et al. documented a high prevalence (up to 52%) of prolonged QTc (QTc ≥ 450 ms for men and ≥ 470 ms for women) in these patients [22]. Brescia et al. found in a series of 242 patients that 22 (9%) had a prolonged QT interval (461–652 ms). The significance of prolonged QTc interval in this context is unclear [20].
VEBs
Ventricular ectopic beats (VEBs) are commonly found in patients with LVNC [31]. A study by Van Malderen et al. on 101 patients with ECG-investigated LVNC showed that VEBs were present in 54% of cases [31]. Most (95%) VEBs originated from the outflow tracts, the fascicles and the mitral and/or tricuspid annulus. Therefore, it is possible that VEBs are not causally related to the structural abnormalities typical of LVNC per se. However, a link between ventricular arrhythmias and the presence of micro-reentry circuits in the trabeculated myocardium, epicardial coronary hypoperfusion, abnormal ion channel activity and microvascular dysfunction have been hypothesized [20, 31].
Ventricular Pre-excitation
Pre-excitation can be observed in patients with LVNC, especially in children [15]. Wolff-Parkinson-White (WPW) syndrome has been found in 0–3% of adult patients and 8–17% of paediatric patients [13, 15, 16, 18, 20, 32]. In a retrospective study, WPW was found to be an independent risk factor for the development of significant cardiac dysfunction in LVNC [33].
Supraventricular Arrhythmias
Supraventricular arrhythmias, including focal atrial tachycardia, atrial fibrillation (AF) and other paroxysmal supraventricular tachyarrhythmias are commonly observed in LVNC, with variable reported prevalences (18–20,24). The most common supraventricular arrhythmia in adults with LVNC is AF, with a prevalence varying from 0.4 to 39% [14, 16, 19, 20, 34, 35]. Although AF pathogenesis in LVNC is often linked to secondary structural remodelling of both atria, a primary atrial myopathy is another proposed mechanism [36]. The most commonly reported supraventricular arrhythmia in children with LVNC is atrioventricular reentrant tachycardia and focal atrial tachycardia with a prevalence ranging from 6 to 13% [13, 15, 20, 36].
The ECG in Isolated LVNC
Familial occurrence in LVNC ranges from 12 to 50% of cases [37]. Although autosomal dominant or X-linked patterns are most common, autosomal recessive and mitochondrial inheritance, as well as chromosome defects have also been reported. Many of the pathogenic variants found in LVNC are shared with other cardiomyopathies, mainly dilated cardiomyopathy (DCM) and HCM [21]. Pathogenic variants are localised in genes encoding sarcomeric, cytoskeletal or ion channel proteins and those involved in cellular energy metabolism [21, 38]. The ECG patterns in some of the most common LVNC-associated genotypes are reported in Table 3 [38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54].
Left Ventricular Non-compaction in Association With Other Conditions
LVNC may be associated with other cardiac and non-cardiac conditions, including cardiomyopathies, congenital heart diseases and inherited systemic diseases.
Other Cardiomyopathies
LVNC may present as a distinct cardiomyopathy or in association with DCM, HCM and ACM [55, 56]. Clinical studies have investigated the role of imaging techniques in differential diagnosis or in the identification of overlapping phenotypes. In this context the ECG might be useful in the diagnostic process, as it is usually the expression of the predominant phenotypic features [57, 58•].
Congenital Heart Diseases
LVNC may be associated with congenital heart diseases (CHD) [21]. In a large series of 202 adult patients with LVNC, Stähli et al. reported an association with CHD in 12% of cases, including left ventricular outflow tract abnormalities and Ebstein anomaly (EA). In this study, the prevalence of LVNC in patients with EA was 15% [59]. In another retrospective analysis of 84 patients with EA, 4 (5%) had LVNC [60]. In a paediatric cohort of 61 patients with EA, 10 (16%) showed features of LVNC; interestingly, there were no significant differences in the ECG findings; incidence of RBBB, ventricular pre-excitation or supraventricular tachycardias were similar in patients with or without EA [61]. EA and LVNC may share the same genetic background; in a cohort of 141 unrelated probands with EA, pathogenic variants in myosin heavy chain 7 (MYH7) gene (all except for 1 3-bp were missense variants) were found in 8 patients (6 of which had LVNC) [39]. LVNC has been described also in association with tetralogy of Fallot [59]. In a Japanese series of 53 patients with LVNC and CHD, 29 [55%] had ventricular septal defects, 17 [32%] atrial septal defects, 10 patent ductus arteriosus (PDA) and 7 [13%] had EA and double outlet right ventricle); fragmented QRS was observed in 16 patients (40%), followed by RBBB (25%), T-wave abnormality (20%), Q waves (17%), ST-segment depression (12%) and prolonged QT interval (12%) [62].
Neuromuscular Disorders
The combination of an NMD and LVNC may be found in the context of genetic conditions due to pathogenic variants in dystrophin, dystrobrevin, lamin, ZASP (Z-band alternatively spliced PDZ-motif protein) or in the context of metabolic diseases such as infantile glycogenosis type II (Pompe’s disease), myoadenylate-deaminase deficiency, or other conditions such as Barth syndrome, Friedreich ataxia or Charcot-Marie-Tooth disease [63]. The ECG abnormalities usually reflect the mixed phenotype.
In a CMR study of patients with Duchenne muscular dystrophy (DMD), LVNC criteria were met by 27/96 patients (28% prevalence) [64]. In another cohort of 86 adult patients with LVNC, 53 (62%) had associated NMDs. A specific NMD was diagnosed in 21 (metabolic myopathy in 14, Leber’s hereditary optic neuropathy in 3, myotonic dystrophy in 2, Becker muscular dystrophy in 1 and DMD in 1, respectively). The presence of ECG abnormalities did not differ between patients with or without NMDs. In this study, high QRS voltages, ST/T wave abnormality and LBBB were the most frequently observed ECG abnormalities [65, 66].
Metabolic Conditions
LVNC has been described in association with monogenic syndromes, including metabolic conditions (e.g. storage diseases such as Danon disease) [55]. The hypothesised mechanism responsible for the development of increased trabeculations in storage disorders might be represented by abnormal intramyocardial storage; whether an immunologic reaction to abnormal proteins or storage material triggers the development of increased trabeculations remains speculative [67]. Danon disease is a rare, X-linked dominant disorder characterised by left ventricular hypertrophy, cardiac conduction abnormalities, skeletal muscle weakness and mild intellectual disability, and is caused by variants in the LAMP2 gene [68]. An association between Danon disease and LVNC has been reported [55]. ECG signs of pre-excitation are common and present in up to 70% of affected male patients [68].
Barth Syndrome
Barth syndrome (BTHS) is a rare X-linked genetic disease characterised by cardiomyopathy (most commonly LVNC), skeletal myopathy, neutropenia and organic aciduria [69, 70]. The main gene involved in BTHS is tafazzin (TAZ) located at Xq28 which encodes an acyltransferase that catalyses the remodelling of cardiolipin in mitocondrial membranes [69]. Several pathogenic variants in the tafazzin gene have been described. Spencer et al. reported prolonged or borderline prolonged QTc in a high proportion of BTHS patients (43%), although this feature did not appear to correlate with episodes of documented ventricular arrhythmias [71].
Differential Diagnosis With Cardiac Adaptation to Exercise
Highly trained athletes may show some degree of LV trabeculations. In a large study of over 1000 asymptomatic athletes, 8.1% fulfilled conventional echocardiographic criteria for LVNC [5]. Increased LV trabeculations were more common in athletes of African/Afro-Caribbean origin. As the majority of athletes with excessive trabeculation did not exhibit any other cardiomyopathic features, it has been postulated that this may be an exercise-induced remodelling phenomenon [72]. Increased cardiac preload is the most probable mechanism for increased trabeculation in the majority of athletes [8]. Differential diagnosis is extremely relevant, but at the same time challenging. The ECG may help in this setting, keeping in mind that the athlete’s heart ECG is also often abnormal [7]. Significant differences in the pattern of T-wave inversion may help in discriminating between physiological cardiac remodelling and LVNC (Fig. 2). Patients with LVNC often show T-wave inversion in the inferolateral leads, whereas athletes either show a normal ECG or T-wave inversion in V1–V3, a pattern that has been recognised as physiological especially in black athletes and if accompanied by J point elevation [73].
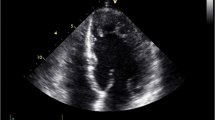
Twelve-lead electrocardiogram in two cases of augmented left ventricular trabeculation (echocardiographic apical 4-chamber view). Thirty-year-old male with familial LVNC. Black arrows indicate non-specific repolarization abnormalities in limb leads, Goldberger’s leads and lateral precordial leads (a). Twenty-two-year-old cyclist with increased left ventricular trabeculation. ECG is normal with high, but physiological T-waves (red arrows) (b)
ECG in the Management and Risk Stratification of Patients With LVNC
ECG abnormalities carry a prognostic role in patients with LVNC. Although a normal ECG is uncommon in LVNC, patients with a normal ECG have a lower degree of structural and functional echocardiographic abnormalities and appear to have a better prognosis [16, 17, 19, 22, 74]. On the contrary, some ECG findings suggest a malignant phenotype and might influence the surveillance of patients at higher risk of adverse events [16, 20, 36]. For example, atrial fibrillation (both permanent and paroxysmal) has been associated with a more severe clinical picture of heart failure and higher mortality in several studies [16, 19, 36, 66, 75, 76]. The association between LVNC and a pre-excitation pattern consistent with WPW syndrome is associated with a greater risk of development of a dilated phenotype and systolic dysfunction [33].
Intraventricular conduction delay (mainly LBBB) in LVNC, as well as in other cardiomyopathies, is associated with reduced LV systolic function, heart failure and LV dilation [19, 74]; further studies are required to better define the prognostic role of this ECG abnormality. As in other cardiac conditions characterised by severe LV systolic dysfunction, the presence of LBBB may be an indication for the use of cardiac resynchronization therapy (CRT) [77]. Although some ECG abnormalities (e.g. positive TaVR) represent ominous signs significantly and independently associated with lethal arrhythmic events including sudden death, their presence does not represent per se an indication for an implantable cardioverter-defibrillator (ICD) [28•]. The decision on whether or not to implant an ICD for primary prevention of sudden cardiac death should be balanced, taking into account both family and patients’ clinical history, symptoms and instrumental features (ECG, ambulatory ECG monitoring, echocardiography, CMR). High QRS voltages have been associated with higher mortality and systemic embolism (probably due to profound alterations of myocardial structure that can predispose to the development of intraventricular thrombi) [22, 66]. Stöllberger et al. studied 105 patients with LVNC over a mean follow-up of 3.6 years, and they compared the ECG features of surviving and deceased patients; multivariate analysis identified atrial fibrillation, low voltages, increase in QRS width and high QRS voltages as predictors of poor outcome [66]. Repolarization abnormalities seem to be linked to increased mortality in some studies [20, 74]. In a cohort of LVNC patients with an average follow-up of 57 months (0–153.4 months), repolarization abnormalities (ST-segment depression or elevation > 0.1 mV in limb leads and > 0.2 mV in precordial leads or T-wave inversion) in the inferior leads were independently associated with poor outcome, with an increased risk for cardiovascular death or heart transplantation [74]. The presence of a prolonged QT interval has been variably linked with systolic dysfunction, myocardial fibrosis and a higher risk of cardiovascular death [22, 74, 78]. In a subgroup analysis by Steffel et al., the LV ejection fraction in patients with prolonged QT was lower than in patients with QT in the normal range (EF 32.2 ± 15.8% vs 48.5 ± 18, p < 0.0001) [26]. Similarly, Zhou et al. found that a prolonged QT was associated with lower LV ejection fraction and higher risk of adverse events [78]. Ventricular arrhythmias are commonly described in patients with LVNC (up to 47%) and are an independent risk factor for mortality [13, 14, 20]. Periodic clinical monitoring with ECG and ambulatory ECG monitoring aimed at detecting ventricular arrhythmias are recommended [20, 25, 36].
Clinical Implications
Several uncertainties about nomenclature and definition of LVNC continue to exist and while the focus and dilemmas concern mainly the imaging assessment of this condition, the ECG provides useful hints that, when appropriately interpreted in the clinical context, might or might not reinforce the diagnostic hypothesis of LVNC. Unfortunately, the lack of specificity of the ECG abnormalities in patients with LVNC described so far, does not allow (if considered in isolation) diagnosis of the condition. Unlike other cardiomyopathies (mainly DCM and HCM), in which some ECG abnormalities may constitute real red flags able to guide clinicians towards a specific aetiology, this is currently not the case in LVNC. The main reason, apart from the lack of pathognomonic ECG signs, is that when approaching patients with prominent trabeculations, clinicians are facing diagnostic queries at two different levels: (1) is the observed cardiac phenotype pathological or not?; (2) what is the specific aetiology? Although we should recognise that grey zones and wide areas of overlap between normal and pathologic phenotypes exist also in the context of other cardiomyopathies (e.g. differential diagnosis between HCM and athlete’s heart), the knowledge gaps in the setting of LVNC seem wider. So, does the ECG modify our diagnostic workup in patients with excessive trabeculations, and possibly our management of the underlying condition? Of course, the ECG in isolation is not able to solve the diagnostic conundrum of LVNC; however, when considered in a set of diagnostic criteria including family history, clinical information and imaging features (as already done for ACM), the ECG may differentiate between physiological and pathological findings or may provide clues raising the possibility of specific underlying genetic conditions (Fig. 3). Moreover, some ECG features in patients with LVNC constitute ominous signs that require a stricter patient surveillance or the need of specific therapeutic measures (e.g. ICD implantation).
Gaps in Evidence and Future Suggestions
LVNC diagnostic criteria are traditionally focused on cardiac imaging (echocardiography and CMR). Our knowledge on ECG abnormalities in LVNC mainly derives from single-centre studies, case reports or small case series. The many uncertainties surrounding the definition of LVNC make this entity difficult to grasp, and future studies should include ECG data systematically, in order to identify possible additional roles of the ECG in the diagnosis, risk stratification and clinical management of the disease. The first step should consist of the identification of the ECG abnormalities with higher sensitivity and specificity observed in patients with isolated LVNC cardiomyopathy (clearly differentiating the paediatric population from adults). The second step should be the incorporation of these ECG abnormalities into the diagnostic criteria of the disease. A scoring system (points-based or with major and minor criteria) should be advisable to exit from a diagnostic quagmire.
Conclusions
The ECG remains a cornerstone in the diagnosis and management of patients with cardiomyopathies, including LVNC. Although recent advances in cardiac imaging resulted in enormous progress in the diagnosis and management of LVNC, an approach that is entirely based on phenotypic visualization may lead to erroneous interpretations. An integrated approach including clinical, ECG, imaging data and possibly genetic information in selected cases probably constitutes the best diagnostic approach to this intriguing condition.
Availability of Data and Material
Not applicable for this type of manuscript.
Code Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J. 2008;29(2):270–6.
Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; quality of care and outcomes research and function. Circulation. 2006;113(14):1807–16.
Kohli SK, Pantazis AA, Shah JS, Adeyemi B, Jackson G, McKenna WJ, et al. Diagnosis of left-ventricular non-compaction in patients with left-ventricular systolic dysfunction: time for a reappraisal of diagnostic criteria? Eur Heart J. 2008;29(1):89–95.
Oechslin E, Jenni R. Left ventricular non-compaction revisited: a distinct phenotype with genetic heterogeneity? Eur Heart J. 2011;32(12):1446–56.
Gati S, Chandra N, Bennett RL, Reed M, Kervio G, Panoulas VF, et al. Increased left ventricular trabeculation in highly trained athletes: do we need more stringent criteria for the diagnosis of left ventricular non-compaction in athletes? Heart. 2013;99(6):401–8.
Moon JC, McKenna WJ. Myocardial crypts: a prephenotypic marker of hypertrophic cardiomyopathy? Circ Cardiovasc Imaging. 2012;5(4):431–2.
Zorzi A, Vio R, Bettella N, Corrado D. Criteria for interpretation of the athlete’s ECG: a critical appraisal. Pacing Clin Electrophysiol. 2020;43(8):882–90.
Gati S, Papadakis M, Papamichael ND, Zaidi A, Sheikh N, Reed M, et al. Reversible de novo left ventricular trabeculations in pregnant women: implications for the diagnosis of left ventricular noncompaction in low-risk populations. Circulation. 2014;130(6):475–83.
Captur G, Flett AS, Jacoby DL, Moon JC. Left ventricular non-noncompaction: the mitral valve prolapse of the 21st century? Int J Cardiol. 2013;164(1):3–6.
Elliott P, Charron P, Blanes JRG, Tavazzi L, Tendera M, Konté M, et al. European cardiomyopathy pilot registry: EURObservational research programme of the European society of cardiology. Eur Heart J. 2016;37(2):164–73.
Nugent AW, Daubeney PEF, Chondros P, Carlin JB, Cheung M, Wilkinson LC, et al. The epidemiology of childhood cardiomyopathy in Australia. N Engl J Med. 2003;348(17):1639–46.
Captur G, Muthurangu V, Cook C, Flett AS, Wilson R, Barison A, et al. Quantification of left ventricular trabeculae using fractal analysis. J Cardiovasc Magn Reson. 2013;15(1):1–10.
Chin TK, Perloff JK, Williams RG, Jue K, Mohrmann R. Isolated noncompaction of left ventricular myocardium. A study of eight cases Circulation. 1990;82(2):507–13.
Ritter M, Oechslin E, Sütsch G, Attenhofer C, Schneider J, Jenni R. Isolated noncompaction of the myocardium in adults. Mayo Clin Proc. 1997;72(1):26–31.
Ichida F, Hamamichi Y, Miyawaki T, Ono Y, Kamiya T, Akagi T, et al. Clinical features of isolated noncompaction of the ventricular myocardium. J Am Coll Cardiol. 1999;34(1):233–40.
Oechslin EN, Attenhofer Jost CH, Rojas JR, Kaufmann PA, Jenni R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36(2):493–500.
Ergul Y, Nisli K, Varkal MA, Oner N, Dursun M, Dindar A, et al. Electrocardiographic findings at initial diagnosis in children with isolated left ventricular noncompaction. Ann Noninvasive Electrocardiol. 2011;16(2):184–91.
Pignatelli RH, McMahon CJ, Dreyer WJ, Denfield SW, Price J, Belmont JW, et al. Clinical characterization of left ventricular noncompaction in children: a relatively common form of cardiomyopathy. Circulation. 2003;108(21):2672–8.
Stöllberger C, Gerger D, Wegner C, Finsterer J. Quantitative electrocardiographic measures, neuromuscular disorders, and survival in left ventricular hypertrabeculation/noncompaction. Ann Noninvasive Electrocardiol. 2013;18(3):251–5.
Brescia ST, Rossano JW, Pignatelli R, Jefferies JL, Price JF, Decker JA, et al. Mortality and sudden death in pediatric left ventricular noncompaction in a tertiary referral center. Circulation. 2013;127(22):2202–8.
Towbin JA, Jefferies JL. Cardiomyopathies due to left ventricular noncompaction, mitochondrial and storage diseases, and inborn errors of metabolism. Circ Res. 2017;121(7):838–54.
Steffel J, Kobza R, Oechslin E, Jenni R, Duru F. Electrocardiographic characteristics at initial diagnosis in patients with isolated left ventricular noncompaction. Am J Cardiol [Internet]. 2009;104(7):984–9. https://doi.org/10.1016/j.amjcard.2009.05.042.
Gungor B, Alper AT, Celebi A, Bolca O. Sinus node dysfunction as the first manifestation of left ventricular noncompaction with multiple cardiac abnormalities. Indian Pacing Electrophysiol J. 2013;13(4):157–61.
Tsai SF, Ebenroth ES, Hurwitz RA, Cordes TM, Schamberger MS, Batra AS. Is left ventricular noncompaction in children truly an isolated lesion? Pediatr Cardiol. 2009;30(5):597–602.
Towbin JA, Lorts A, Jefferies JL. Left ventricular non-compaction cardiomyopathy. Lancet. 2015;386(9995):813–25.
Domain G, Chouquet C, Réant P, Bongard V, Vedis T, Rollin A, et al. Relationships between left ventricular mass and QRS duration in diverse types of left ventricular hypertrophy. Eur Heart J Cardiovasc Imaging. 2022;23(4):560–8.
Ning XH, Tang M, Chen KP, Hua W, Chen RH, Sha J, et al. The prognostic significance of fragmented QRS in patients with left ventricular noncompaction cardiomyopathy. Can J Cardiol [Internet]. 2012;28(4):508–14. https://doi.org/10.1016/j.cjca.2012.01.011.
Ekizler FA, Cay S, Ulvan N, Tekin Tak B, Cetin EHO, Kafes H, et al. Importance of lead aVR on predicting adverse cardiac events in patients with noncompaction cardiomyopathy. Ann Noninvasive Electrocardiol. 2020;25(3):212–23. In this study positive TaVR was superior to any other ECG findings in the establishment of patients with LVNC most at risk for adverse cardiac events.
Caliskan K, Ujvari B, Bauernfeind T, Theuns DAMJ, Van Domburg RT, Akca F, et al. The prevalence of early repolarization in patients with noncompaction cardiomyopathy presenting with malignant ventricular arrhythmias. J Cardiovasc Electrophysiol. 2012;23(9):938–44.
Shoji M, Yamashita T, Uejima T, Asada K, Semba H, Otsuka T, et al. Electrocardiography characteristics of isolated non-compaction of ventricular myocardium in Japanese adult patients. Circ J. 2010;74(7):1431–5.
Van Malderen S, Wijchers S, Akca F, Caliskan K, Szili-Torok T. Mismatch between the origin of premature ventricular complexes and the noncompacted myocardium in patients with noncompaction cardiomyopathy patients: involvement of the conduction system? Ann Noninvasive Electrocardiol. 2017;22(2):1–7.
Stöllberger C, Blazek G, Winkler-Dworak M, Finsterer J. Sex differences in left ventricular noncompaction in patients with and without neuromuscular disorders. Rev Española Cardiol (English Ed). 2008;61(2):130–6.
Howard TS, Valdes SO, Hope KD, et al. Association of Wolff-Parkinson-White with left ventricular noncompaction cardiomyopathy in children. J Card Fail. 2019;25(12):1004–8. https://doi.org/10.1016/j.cardfail.2019.09.014.
Sedaghat-Hamedani F, Haas J, Zhu F, Geier C, Kayvanpour E, Liss M, et al. Clinical genetics and outcome of left ventricular non-compaction cardiomyopathy. Eur Heart J. 2017;38(46):3449–60.
Salazar-Mendiguchía J, González-Costello J, Oliveras T, Gual F, Lupón J, Manito N. Long-term follow-up of symptomatic adult patients with noncompaction cardiomyopathy. Rev Española Cardiol (English Ed). 2019;72(2):169–71.
Miyake CY, Kim JJ. Arrhythmias in left ventricular noncompaction. Card Electrophysiol Clin [Internet]. 2015;7(2):319–30. https://doi.org/10.1016/j.ccep.2015.03.007.
Negri F, De Luca A, Morea G, Ferro MD, Faganello G, Vitrella G, et al. Facciamo il punto: Miocardio non compatto. G Ital Cardiol. 2018;19(6):371–8.
Li S, Zhang C, Liu N, Bai H, Hou C, Wang J, Song L, Pu J. Genotype-positive status is associated with poor prognoses in patients with left ventricular noncompaction cardiomyopathy. J Am Heart Assoc. 2018;7(20):e009910.
Postma AV, Van Engelen K, Van De Meerakker J, Rahman T, Probst S, Baars MJH, et al. Mutations in the sarcomere gene MYH7 in Ebstein anomaly. Circ Cardiovasc Genet. 2011;4(1):43–50.
Baban A, Cicenia M, Magliozzi M, Gnazzo M, Cantarutti N, Silvetti MS, et al. Cardiovascular Involvement in pediatric laminopathies. Report of six patients and literature revision. Front Pediatr. 2020;8(July):1–9.
Campbell MJ, Czosek RJ, Hinton RB, Miller EM. Exon 3 deletion of ryanodine receptor causes left ventricular noncompaction, worsening catecholaminergic polymorphic ventricular tachycardia, and sudden cardiac arrest. Am J Med Genet Part A. 2015;167(9):2197–200.
Nozaki Y, Kato Y, Uike K, Yamamura K, Kikuchi M, Yasuda M, et al. Co-phenotype of left ventricular non-compaction cardiomyopathy and atypical catecholaminergic polymorphic ventricular tachycardia in association with R169q, a ryanodine receptor type 2 missense mutation. Circ J. 2020;84(2):226–34.
Ohno S, Omura M, Kawamura M, Kimura H, Itoh H, Makiyama T, et al. Exon 3 deletion of RYR2 encoding cardiac ryanodine receptor is associated with left ventricular non-compaction. Europace. 2014;16(11):1646–54.
Roston TM, Guo W, Krahn AD, Wang R, Van Petegem F, Sanatani S, et al. A novel RYR2 loss-of-function mutation (I4855M) is associated with left ventricular non-compaction and atypical catecholaminergic polymorphic ventricular tachycardia. J Electrocardiol [Internet]. 2017;50(2):227–33. https://doi.org/10.1016/j.jelectrocard.2016.09.006.
Milano A, Vermeer AMC, Lodder EM, Barc J, Verkerk AO, Postma AV, et al. HCN4 mutations in multiple families with bradycardia and left ventricular noncompaction cardiomyopathy. J Am Coll Cardiol. 2014;64(8):745–56.
Schweizer PA, Schröter J, Greiner S, Haas J, Yampolsky P, Mereles D, et al. The symptom complex of familial sinus node dysfunction and myocardial noncompaction is associated with mutations in the HCN4 channel. J Am Coll Cardiol. 2014;64(8):757–67.
Klaassen S, Probst S, Oechslin E, Gerull B, Krings G, Schuler P, et al. Mutations in sarcomere protein genes in left ventricular noncompaction. Circulation. 2008;117(22):2893–901.
Hoedemaekers YM, Caliskan K, Michels M, Frohn-Mulder I, Van Der Smagt JJ, Phefferkorn JE, et al. The importance of genetic counseling, DNA diagnostics, and cardiologic family screening in left ventricular noncompaction cardiomyopathy. Circ Cardiovasc Genet. 2010;3(3):232–9.
Frustaci A, De Luca A, Guida V, Biagini T, Mazza T, Gaudio C, Letizia C, Russo MA, Galea N, Chimenti C. Novel α-actin gene mutation p.(Ala21Val) causing familial hypertrophic cardiomyopathy, myocardial noncompaction, and transmural crypts. Clinical-Pathologic Correlation. J Am Heart Assoc. 2018;7(4):e008068.
Rigaud C, Lebre AS, Touraine R, Beaupain B, Ottolenghi C, Chabli A, et al. Natural history of Barth syndrome: a national cohort study of 22 patients. Orphanet J Rare Dis. 2013;8(1):9–18.
Sasaki T, Ikeda K, Nakajima T, Kawabata-Iwakawa R, Iizuka T, Dharmawan T, et al. Multiple arrhythmic and cardiomyopathic phenotypes associated with an SCN5A A735E mutation. J Electrocardiol [Internet]. 2021;65:122–7. https://doi.org/10.1016/j.jelectrocard.2021.01.019.
Shan L, Makita N, Xing Y, Watanabe S, Futatani T, Ye F, et al. SCN5A variants in Japanese patients with left ventricular noncompaction and arrhythmia. Mol Genet Metab. 2008;93(4):468–74.
Hermida-Prieto M, Monserrat L, Castro-Beiras A, Laredo R, Soler R, Peteiro J, et al. Familial dilated cardiomyopathy and isolated left ventricular noncompaction associated with lamin A/C gene mutations. Am J Cardiol. 2004;94(1):50–4.
Liu Z, Shan H, Huang J, Li N, Hou C, Pu J. A novel lamin A/C gene missense mutation (445 V > E) in immunoglobulin-like fold associated with left ventricular non-compaction. EP Eur [Internet]. 2016;18(4):617–22. https://doi.org/10.1093/europace/euv044.
Arbustini E, Favalli V, Narula N, Serio A, Grasso M. Left ventricular noncompaction: a distinct genetic cardiomyopathy? J Am Coll Cardiol. 2016;68(9):949–66.
Oechslin E, Jenni R. Left ventricular noncompaction: from physiologic remodeling to noncompaction cardiomyopathy ∗. J Am Coll Cardiol. 2018;71(7):723–6.
Gati S, Rajani R, Carr-White GS, Chambers JB. Adult left ventricular noncompaction: reappraisal of current diagnostic imaging modalities. JACC Cardiovasc Imaging. 2014;7(12):1266–75.
Finocchiaro G, Merlo M, Sheikh N, De Angelis G, Papadakis M, Olivotto I, Rapezzi C, Carr-White G, Sharma S, Mestroni L, Sinagra G. The electrocardiogram in the diagnosis and management of patients with dilated cardiomyopathy. Eur J Heart Fail. 2020;22(7):1097–107. This paper emphasizes the importance of the ECG and the role of systematic approach in its interpretation in patients with cardiomyopathies.
Stähli BE, Gebhard C, Biaggi P, Klaassen S, Valsangiacomo Buechel E, Attenhofer Jost CH, et al. Left ventricular non-compaction: prevalence in congenital heart disease. Int J Cardiol. 2013;167(6):2477–81.
Kumor M, Lipczyńska M, Biernacka EK, Klisiewicz A, Wójcik A, Konka M, et al. Cardiac arrest and ventricular arrhythmia in adults with Ebstein anomaly and left ventricular non-compaction. J Cardiol. 2018;71(5):484–7.
Pignatelli RH, Texter KM, Denfield SW, Grenier MA, Altman CA, Ayres NA, et al. LV noncompaction in ebstein’s anomaly in infants and outcomes. JACC Cardiovasc Imaging. 2014;7(2):207–9.
Hirono K, Hata Y, Miyao N, Okabe M, Takarada S, Nakaoka H, et al. Left ventricular noncompaction and congenital heart disease increases the risk of congestive heart failure. J Clin Med. 2020;9(3):785.
Finsterer J, Stöllberger C, Blazek G. Neuromuscular implications in left ventricular hypertrabeculation/noncompaction. Int J Cardiol. 2006;110(3):288–300.
Statile CJ, Taylor MD, Mazur W, Cripe LH, King E, Pratt J, et al. Left ventricular noncompaction in Duchenne muscular dystrophy. J Cardiovasc Magn Reson. 2013;15(1):1.
Stöllberger C, Winkler-Dworak M, Blazek G, Finsterer J. Association of electrocardiographic abnormalities with cardiac findings and neuromuscular disorders in left ventricular hypertrabeculation/non-compaction. Cardiology. 2007;107(4):374–9.
Stöllberger C, Gerger D, Jirak P, Wegner C, Finsterer J. Evolution of electrocardiographic abnormalities in association with neuromuscular disorders and survival in left ventricular hypertrabeculation/noncompaction. Ann Noninvasive Electrocardiol. 2014;19(6):567–73.
Stöllberger C, Finsterer J. How to manage left ventricular hypertrabeculation/noncompaction in Fabry’s disease? Cardiology. 2011;120(2):95–6.
Martin S, Ingles J, Hunyor I, Bagnall RD, Puranik R, Semsarian C. LAMP2 shines a light on cardiomyopathy in an athlete. HeartRhythm Case Rep. 2017;3(3):172–6. https://doi.org/10.1016/j.hrcr.2016.11.005.
Clarke SLN, Bowron A, Gonzalez IL, Groves SJ, Newbury-Ecob R, Clayton N, et al. Barth syndrome. Orphanet J Rare Dis. 2013;8(1):1–17.
Ferreira C, Pierre G, Thompson R, Vernon H, Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A (editors). Barth syndrome. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993. 2014 Oct 9 [updated 2020 Jul 9].
Spencer CT, Bryant RM, Day J, Gonzalez IL, Colan SD, Thompson WR, Berthy J, Redfearn SP, Byrne BJ. Cardiac and clinical phenotype in Barth syndrome. Pediatrics. 2006;118(2):e337–46.
Gati S, Sharma S, Pennell D. The role of cardiovascular magnetic resonance imaging in the assessment of highly trained athletes. JACC Cardiovasc Imaging. 2018;11(2 Pt 1):247–59.
Gati S, Rajani R, Carr-White GS, Chambers JB. Adult left ventricular noncompaction: reappraisal of current diagnostic imaging modalities. JACC Cardiovasc Imaging. 2014;7(12):1266–75.
Steffel J, Hürlimann D, Namdar M, Despotovic D, Kobza R, Wolber T, et al. Long-term follow-up of patients with isolated left ventricular noncompaction: role of electrocardiography in predicting poor outcome. Circ J. 2011;75(7):1728–34.
Stöllberger C, Blazek G, Winkler-Dworak M, Finsterer J. Atrial fibrillation in left ventricular noncompaction with and without neuromuscular disorders is associated with a poor prognosis. Int J Cardiol [Internet]. 2009;133(1):41–5. https://doi.org/10.1016/j.ijcard.2007.11.099.
Weiford BC, Subbarao VD, Mulhern KM. Noncompaction of the ventricular myocardium. Circulation. 2004;109(24):2965–71.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Vol. 37. Eur Heart J. 2016;2016:2129–2200m.
Zhou H, Lin X, Fang L, Zhu W, Zhao X, Ding H, et al. Prolonged QTc indicates the clinical severity and poor prognosis in patients with isolated left ventricular non-compaction. Int J Cardiovasc Imaging. 2017;33(12):2013–20.
Murphy RT, Thaman R, Blanes JG, Ward D, Sevdalis E, Papra E, et al. Natural history and familial characteristics of isolated left ventricular non-compaction. Eur Heart J. 2005;26(2):187–92 (80).
Cetin MS, Ozcan Cetin EH, Canpolat U, Cay S, Topaloglu S, Temizhan A, et al. Usefulness of fragmented QRS complex to predict arrhythmic events and cardiovascular mortality in patients with noncompaction cardiomyopathy. Am J Cardiol [Internet]. 2016;117(9):1516–23. https://doi.org/10.1016/j.amjcard.2016.02.022 (81).
Author information
Authors and Affiliations
Contributions
Main contributions: GDS, AP, SG, GF (conceptualization); AP, GDS, GF (literature search and data analysis); GDS, AP, GP, GS, MP, AP, SS (manuscript drafting); SG and GF (manuscript critical revision as senior authors). All the authors were actively involved in all the stages of the project.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable (not required for this type of article).
Consent to Participate/Consent for Publication
Not applicable for this type of manuscript.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors have no conflicts of interest to declare. Dr Finocchiaro is supported by the charity Cardiac Risk in the Young (CRY).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Editors would like to thank Prof. Christiane Angermann for handling the review of this manuscript.
This article is part of the Topical Collection on Imaging in Heart Failure.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanna, G.D., Piga, A., Parodi, G. et al. The Electrocardiogram in the Diagnosis and Management of Patients With Left Ventricular Non-Compaction. Curr Heart Fail Rep 19, 476–490 (2022). https://doi.org/10.1007/s11897-022-00580-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-022-00580-z