Abstract
Purpose of Review
Cancer treatment–related cardiotoxicity (CTRC) represents a significant cause of morbidity and mortality worldwide. The purpose of our review is to summarize the epidemiology, natural history, and pathophysiology of cardiotoxicity-related to cancer treatment. We also summarize appropriate screening, surveillance, and management of CTRC. While cardiotoxicity is characteristically associated with anthracyclines, HER2-B antagonists, and radiation therapy (XRT), there is growing recognition of toxicity with immune checkpoint inhibitors (ICI), tyrosine kinase inhibitors, and proteasome inhibitors.
Recent Findings
Patients at risk for cardiotoxicity should be screened based on available guidelines, generally with serial echocardiograms. The role of medical heart failure (HF) therapies is controversial in patients with asymptomatic left ventricular dysfunction but may be considered in some instances. Once symptomatic HF has developed, treatment should be in accordance with ACC/AHA guidelines.
Summary
The goal in caring for patients receiving cancer treatment is to optimize cardiac function and prevent interruptions in potentially lifesaving cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer treatment–related cardiomyopathy (CTRC) is an underrecognized disorder associated with substantial morbidity and mortality. Cancer currently represents the second leading cause of death worldwide [1]. With an aging population and advances in cancer treatment, a greater number of patients are both diagnosed with and surviving cancer [2]. Improved outcomes in cancer treatment have led to the increasing incidence of longer-term cardiovascular toxicities following cancer treatment, specifically CTRC [3]. Previously, only a relatively small number of cancer therapies were known to cause cardiomyopathy. However, with introduction of new targeted and immune-based cancer therapies, many of these agents are being linked to cardiomyopathy. As the development of cardiomyopathy may impact patient survival and lead to disruptions in cancer treatment, it is essential that the practicing cardiologist recognize the importance of CTRC and its management. The core goal for the cardiologist caring for patients receiving cardiotoxic cancer therapies is to optimize cardiac function, minimize treatment interruptions, and allow the patient to receive appropriate cancer treatment whenever possible.
The scope of our review focuses on the diagnosis and management of CTRCs. We will describe the epidemiology and natural history of CTRC. We will discuss the most common agents implicated in this disorder including anthracyclines, HER-2/ERB antagonists, proteasome inhibitors, tyrosine kinase inhibitors, immune checkpoint inhibitors (ICI), and radiation (XRT). We will also outline guidelines and recommendations on the screening, surveillance, and diagnosis of patients with and at risk for CTRC. We will finally discuss evidence-based treatment strategies for CTRC including the management of cancer treatment regimens and appropriate heart failure (HF) therapies.
Implicated Agents
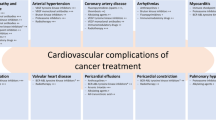
The list of cancer drugs associated with cardiomyopathy is exhaustive; thus, we will strategically focus on the following drug classes which have the most evidence for cardiotoxicity. Table 1 highlights the cancer treatments most commonly associated with CTRC and their corresponding incidences:
Anthracyclines
Anthracyclines are widely used in the treatment of both hematologic and oncologic malignancies, and their cardiotoxicity is well described. Anthracycline cardiotoxicity was first reported in the 1970s, about a decade after their use began [4]. Multiple mechanisms have been proposed over the years to explain anthracycline cardiotoxicity. The most widely accepted theory is that anthracyclines inhibit topoisomerase II-β in the cardiomyocytes leading to oxidative stress, mitochondrial dysfunction, and cell death (Fig. 1) [5•]. Anthracyclines also inhibit the ability of topoisomerase II-β to repair double stranded DNA breaks [6].
Pathophysiology of anthracycline induced cardiotoxicity. Cardiotoxicity is generally thought to occur due to inhibition of topoisomerase II-β. Inhibition of this enzyme leads to impaired ability to repair double stranded breaks, mitochondrial dysfunction, and the generation of reactive oxygen species (ROS) (adapted from J Am Coll Cardiol. 2014 Sep 2;64(9):938–45)
The reported incidence of cardiomyopathy from anthracyclines is around 3–26%; compared with other anthracyclines, epirubicin appears to confer the lowest risk of HF [5]. Toxicity may occur acutely (immediately after infusion), subacutely (< 1 year), or chronically (> 1 year). Subacute (2–9%) and chronic (1–9%) toxicities are most common with acute toxicity being a rare entity [7,8,9]. Interestingly, many chronic presentations may actually be missed cases of subacute toxicity; in a study by Cardinale et al., 98% of anthracycline toxicity is within the first year with close surveillance [9].
The risk of cardiotoxicity with anthracyclines is related to the lifetime dosage received [9]. In one large meta-analysis, the risk of HF increased exponentially after receipt of ≥ 400 mg/m [2] of doxorubicin with 5% risk at 400 mg/m [2], 16% at 500 mg/m2, 26% at 550 mg/m2, and 48% at 700 mg/m2 [10]. Based on this and other trials, the American Society of Clinical Oncology (ASCO) defines patients receiving ≥ 250 mg/m2 of doxorubicin and ≥ 600 mg/m2 of epirubicin as high risk [11•]. Additionally, advanced age, female gender, coronary artery disease (CAD), diabetes, hypertension, baseline left ventricular (LV) dysfunction, or concomitant radiation or trastuzumab use further increase the risk of HF [10,11,12,13]. Certain polymorphisms in the topoisomerase 2β and iron metabolism genes are also associated with increased cardiotoxicity with anthracyclines [14].
Once developed, anthracycline-associated cardiomyopathy carries a poor prognosis with as low as 50% survival at 5 years [15]. Cardiotoxicity from anthracyclines was previously thought to be permanent. However, there is some evidence that LV function may improve with early diagnosis and prompt initiation of appropriate medical therapy for HF [9].
HER-2/ERB Antagonists
Monoclonal antibodies targeting the HER-2/ERB receptor are frequently used in patients suffering from breast cancer. Overexpression of the HER-2/ERB receptor on the surface of breast cancer cells helps to promote abnormal cell proliferation through the PI3K/AKT/mTOR/kRAS pathway [7]. When added to anthracycline based regimens, the use of trastuzumab is associated with a significant survival benefit [16]. Therefore, these agents have become an integral part of therapy for patients with HER-2/ERB positive breast cancer. HER-2/ERB is also expressed by myocytes and is thought to play a role in protecting the myocyte against cellular stress. Non-selective inhibition of this receptor on cardiomyocytes is thought to be the mechanism of cardiotoxicity with these agents [17, 18••].
Rates of cardiotoxicity are reported around 2–28%, comparable to that of anthracyclines [5]. However, unlike with anthracyclines, asymptomatic LV dysfunction is the most common presentation (7–19%) with HER-2/ERB antagonists and severe HF is much less common (1–4%) [18,19,••–20]. Concomitant use of anthracyclines is associated with as much as a sevenfold increase in the risk of cardiomyopathy [21, 22]. Similar to anthracyclines, advanced age, impaired baseline LV function, and cardiovascular comorbidities also appear to increase HF risk [20, 23].
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors (ICI) exert their effect by inhibition of either CTLA-4 or PDL-1, which are ligands responsible for bolstering regulatory T cell function and inhibiting the host T cell immune response. By blocking these receptors, ICI enhance the host antitumor immune response. ICI use has drastically improved mortality in subtypes of advanced stage non-small cell lung cancer, melanoma, renal cell carcinoma, and others. Unfortunately, upregulation of the immune response may lead to collateral damage in the form of autoimmune adverse effects. Enhanced host immune response against cardiomyocytes is thought to be the mechanism of cardiotoxicity and has been demonstrated in mouse models [24]. Myopericarditis, atrial and ventricular tachyarrhythmias, and heart failure are all recognized complications of ICI [25]. Myocardial biopsy of patients with ICI myocarditis may show an inflammatory T cell infiltrate similar to that seen in acute allograft rejection [26].
As the use of these medications is fairly recent, the true incidence of cardiotoxicity is not well characterized. In one multicenter study, the incidence of myocarditis was 1.1% [27]. The median onset of myocarditis was at 34 days with 81% presenting within 3 months of therapy initiation [28]. The risk of myocarditis appeared to be highest with combination ICI. Troponin was elevated in majority of the patients presenting with ICI-associated myocarditis (94%). Interestingly, LV ejection fraction (LVEF) may be normal in up to 21–51% of cases [25]. Outcomes with ICI-associated myocarditis are extremely poor with mortality as high as 17–27% [28, 29]. In the study by Mahmood et al., 46% (16/35) of patients with ICI-associated myocarditis developed cardiogenic shock, complete heart block, cardiac arrest, or death [28]. Combination therapy was also associated with worse survival [29]. Normal LV function also does not appear to be protective, and 38% of major adverse events occurred in patients with normal LVEF [28].
Radiation
Radiation-induced cardiotoxicity has been described for over 50 years [28]. As cardiac tumors are exceedingly rare, cardiotoxicity is usually due to collateral damage from irradiation of nearby structures such as the lung, lymphoid, or breast tissue. The mechanism of injury is multifactorial due to inflammatory vascular damage leading to accelerated atherosclerosis and myocardial fibrosis and consequently systolic/diastolic dysfunction (Fig. 2) [30].
Pathophysiology of radiation-induced cardiotoxicity. Radiation is thought to result in micro and macrovascular damage which results in impaired myocardial perfusion, myocardial fibrosis, and progressive systolic/diastolic dysfunction. Radiation may also lead to epicardial coronary disease, resulting in further impairment of myocardial performance (adapted from J Am Coll Cardiol. 2019 Aug 20;74(7):905–927)
Radiation-induced cardiac injury can manifest as constrictive pericarditis, coronary artery disease (CAD), valvular disease, or heart failure [30]. In patients receiving chest wall radiation for Hodgkin’s lymphoma, rates of heart failure were around 13% and as high as 33% with concomitant anthracycline use [29]. The risk of cardiotoxicity was even higher in patients receiving radiation therapy (XRT) in the 1970s–1980s due to the use of high dose mantle radiation for lymphoma [30]. Diastolic HF is far more commonly associated with XRT than systolic. Given the known association between XRT and CAD, the development of systolic dysfunction should raise concern for concomitant ischemia [31]. Cardiotoxicity is most common within 1–5 years following exposure, although cases have been reported immediately or up to 15 years after treatment [32, 33]. Given the time to toxicity, it is difficult to determine the true incidence of cardiotoxicity with modern radiation regimens, although it would be expected to be lower with newer strategies aimed at reducing cardiac exposure. The overall risk depends on cardiac structure involved in the radiation field and the dose received30, [32]. Additional risk factors for cardiotoxicity include younger age at the time of XRT, the presence of pre-existing heart disease, and concomitant use of anthracycline chemotherapy [34, 35]
Other Implicated Agents
Multiple additional chemotherapy drugs are associated with cardiotoxicity. The alkylating agent cyclophosphamide has been associated with as high as 7–28% risk of HF [5, 36]. The prognosis with cyclophosphamide-associated CTRC is poor with mortality around 20%. Cardiac dysfunction tends to manifest earlier in the treatment course with older patients being at higher risk [37]. Proteasome inhibitors such as bortezomib and carfilzomib are commonly used to treat multiple myeloma. Rates of cardiac adverse events and heart failure in patients treated with carfilzomib were 22% and 7%, respectively [38]. Tyrosine kinase inhibitors and monoclonal antibodies directed against vascular endothelial growth factor (VEGF) such as sorafenib, sunitinib, and bevacizumab have grown in popularity in the treatment of various cancers. While hypertension and arterial emboli appear most common, systolic heart failure is noted in 7–8% of patients [39, 40]. Rates of HF with sunitinib appear higher in patients with pre-existing hypertension or CAD [41]. Cardiac function generally improved with cessation of the offending agent and institution of guideline-directed therapy.
Risk Factors for Cancer Treatment–Related Cardiomyopathy
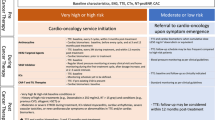
Certain patient characteristics portend a particularly high risk of developing cardiotoxicity. In their guidelines, the American Society of Clinical Oncologists (ASCO) defined the following patient populations as being at increased risk of developing cardiomyopathy (Fig. 3) [11•]:
Risk scores have been developed to help predict risk of cardiotoxicity in patients receiving anthracyclines and trastuzumab [42, 43].
Classifications of Heart Failure Due to Cancer Treatment
Diagnosis of Cancer Treatment–Related Cardiomyopathy
Multiple imaging modalities aid in the detection of cardiomyopathy due to cancer treatment. Given its widespread availability and low cost, echocardiography is the most common modality for diagnosing and monitoring for CTRC. Serial echocardiograms can be performed prior to and during therapy to evaluate for systolic dysfunction. The American Society of Echocardiography (ASE) authors define CTRC as a decline in EF of > 10% to ≤ 53% which is confirmed on subsequent imaging [46]. While our authors agree with this definition, this is expert opinion due to the lack of studies validating this cutoff.
The addition of 3-D volumetric analysis, diastolic function, and myocardial strain imaging compliment EF in the echocardiographic evaluation of CTRC [ 47]. Changes in longitudinal strain precede EF decline and appear to predict the subsequent development of systolic dysfunction in patients receiving anthracyclines [48, 49]. Strain also appears to be more sensitive for detecting myocardial dysfunction than LVEF in patients with prior XRT [13]. Based on several trials, the ASE define subclinical LV dysfunction as baseline strain ≥ lower limit of normal (LLN) in the setting of normal LVEF [47]. A relative decrease in longitudinal strain of ≥ 15% from baseline is highly predictive of subsequent cardiotoxicity [47]. Further research is necessary to determine whether early detection of strain abnormalities impact clinical outcomes in patients receiving cancer treatment. The Strain Surveillance of Chemotherapy for Improving Cardiovascular Outcomes (SUCCOUR) trial is currently underway to help answer this important question [50].
Additionally, cardiac magnetic resonance imaging (CMR) is an increasingly used modality in the assessment of CTRC. In addition to being the gold standard for assessment of ventricular volumes and systolic function, it also has the added ability of tissue characterization. In this setting, CMR can still be useful to rule out other potential etiologies of cardiomyopathy such as ischemia, hypertrophic cardiomyopathy, or infiltrative cardiomyopathies [47]. CMR is particularly useful in the diagnosis of ICI-associated myocarditis. CMR findings of ICI-associated myocarditis include mid-myocardial or epicardial fibrosis via late gadolinium enhancement (LGE), global or focal hypokinesis, and elevation in T2 relaxation time indicative of myocardial inflammation/edema (Fig. 5) [51].
Cardiac MRI in a 61 year old male with Immune Checkpoint Inhibitor myocarditis due to nivolumab. The patient was recieving ICI for Hodgkin’s Lymphoma. There is inferior and septal myocardial edema (solid arrow) on T2 mapping (A) and patchy replacement fibrosis (dashed arrow) on late gadolinium enhancement images (B) in a non – coronary distribution suggesting an inflammatory cardiomyopathy.
Biomarkers also are a novel method of screening for subclinical cardiotoxicity in patients receiving cancer treatment. Elevation in troponin in response to anthracyclines is common and predictive of subsequent LV dysfunction [52]. Multiple other studies have validated the association between troponin elevation and future LVEF decline in patients receiving both anthracyclines and trastuzumab [47, 53, 54]. B-type natriuretic peptide (BNP) and NT-proBNP may also be of prognostic utility, although the data is less robust [55, 56]. Biomarkers are generally cheap and accessible, suggesting a promising role in screening for subclinical LV dysfunction.
Screening and Surveillance for CTRC
The basis of screening for CTRC is the notion that by screening high-risk patients, cardiotoxicity may be identified at earlier stages where interventions may be most beneficial. Our authors generally agree with the approach to screening and surveillance proposed by the authors of the ASE consensus document [47]. Baseline assessment of LV function—ideally with strain—should be strongly considered in anyone initiating cardiotoxic cancer treatment, particularly those at high risk [11, 47]. CMR should be considered if the echocardiogram images are suboptimal or if the diagnosis is in question [47]. Those with overt LV dysfunction or subclinical dysfunction (as defined by abnormal strain or biomarkers) at baseline should generally be referred to cardiology prior to initiation of cardiotoxic therapy (Fig. 6a). Therapy may still be initiated if the benefits outweigh the risk but done with close monitoring.
In patients receiving low doses of anthracyclines (≤ 240 mg/m [2]), it is reasonable to repeat LV assessment at the conclusion of chemotherapy and 6–12 months later (Fig. 6b). More frequent screening is indicated in patients receiving higher doses of anthracycline. In patients taking trastuzumab, screening should be considered every 3 months while on therapy and at the completion of treatment. These surveillance intervals are consistent with the current FDA recommendations [57].
There is no clear consensus on screening and surveillance for HF in patients receiving XRT. The ASE guidelines recommend obtaining a screening echocardiogram 10 years after XRT in all patients and every 5 years after XRT in high-risk patients (Fig. 7) [36]. They further recommend considering surveillance stress testing beginning at 5–10 years in high-risk patients, although there is no evidence that such screening reduces adverse events. These recommendations are expert opinion and sound evidence is lacking on proper surveillance intervals. There should be a low threshold for echocardiogram and ischemic evaluation in any symptomatic patient with a history of prior chest XRT. Pericardial constriction due to XRT should also be considered in any patient presenting with HF symptoms.
There are no formal guidelines for monitoring ICI, but based on a consensus document by ASCO, it is reasonable to obtain baseline troponin and EKG prior to therapy, particularly in those on multiple ICI [58]. In symptomatic patients, additional testing is necessary to establish the diagnosis. As discussed above, normal LV function does not rule out ICI-associated myocarditis, and CMR or myocardial biopsy should be considered in anyone on ICI presenting with HF symptoms, atrial/ventricular arrhythmias, or heart block.
There are similarly no formal guidelines for screening or surveillance with other chemotherapeutic agents such as tyrosine kinase inhibitors, checkpoint inhibitors, or proteasome inhibitors, although a baseline assessment of LV function is reasonable prior to initiating these agents.
Patients with > 10% drop in EF to < 53% or > 15% relative decrease in longitudinal strain from baseline should generally be referred to a cardiologist. While some studies have less strict cutoffs, our authors agree with the ASE cutoff of ≥ 10% decline in EF given the ± 5% interobserver variability seen with echocardiography [48]. Additionally, anyone with signs and symptoms suggestive of heart failure should have repeat imaging and cardiology evaluation. Overall, these recommendations are expert opinion and further studies are needed to validate appropriate screening/surveillance intervals.
Approach to Cancer Therapies in Patients with Cardiotoxicity
Neither ASCO nor the European Society for Medical Oncology (ESMO) provides concrete recommendations on when cardiotoxic cancer therapies should be held in those with LV dysfunction [11•, 59]. This decision should be a multidisciplinary and involve both the treating oncologist and cardiologist. In general, all efforts should be made to continue potential lifesaving cancer treatments whenever possible. The role of the cardiologist is to optimize cardiac function to allow for further chemotherapy, particularly when alternative treatment regimens are not available.
Anthracyclines
The ESMO recommend holding anthracyclines in patients with LVEF if EF ≤ 40% or ≥ 10% decrease from baseline to ≤ 50% [60]. With anthracyclines, toxicity is cumulative and dose-dependent; therefore, patients who develop symptomatic HF from anthracycline cardiotoxicity should generally not be re-challenged unless the benefits outweigh the risks.
In patients at high risk for cardiotoxicity who need to receive anthracyclines, several strategies have been shown to reduce the risk of CRTC. Compared with bolus dosing, continuous infusion of anthracycline is associated with reduced cardiotoxicity [60]. Anthracycline mediated cardiotoxicity is related to peak drug levels whereas anti-tumor effects are generally related to area under the curve (AUC), which perhaps explains this finding [14]. The use of the liposomal form of doxorubicin may also reduce the risk of cardiotoxicity due to altered tissue distribution [11•, 14]. Additionally, epirubicin appears to be less cardiotoxic than other anthracyclines and may be considered in high-risk patients [5•]. One promising agent in the prevention of anthracycline toxicity has been dexrazoxane. This medication is an iron chelator which also inhibits topoisomerase II, but its mechanism of cardioprotection is poorly understood [5•]. Multiple studies have demonstrated a reduction in HF incidence with dexrazoxane [61, 62]. Unfortunately, few small studies revealed an increased risk of subsequent hematologic malignancies with dexrazoxane [62, 63]. Though subsequent meta-analysis refuted these findings, the FDA has only approved the use of dexrazoxane in adult patients with metastatic breast cancer who have received ≥ 300 mg/m [2] of lifetime doxorubicin and may need additional anthracycline-based chemotherapy [5•].
HER-2/ERB Antagonists
In patients receiving HER-2/ERB antagonists, the FDA recommends holding therapy in patients who develop ≥ 16% drop in EF from baseline or ≥ 10 to ≤ 50% [58]. Unlike with anthracyclines, cardiotoxicity due to trastuzumab is often reversible, and it appears safe to re-challenge patients following EF recovery [23, 64]. Therefore, HER-2/ERB antagonists may be safely resumed once EF normalizes. Moreover, several studies have even demonstrated the safety of continuing trastuzumab in patients with asymptomatic LV dysfunction (stage B) [65]. In the 30 patient, prospective SAFE-HEaRt study, 90% of patients with asymptomatic LV dysfunction were able to complete their HER-2/ERB therapy with the use of beta blockers and angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) [66]. Of the HER-2/ERB antagonists, lapatinib, pertuzumab, and T-DM1 appear to be less cardiotoxic compared to trastuzumab, and these agents may be appropriate in certain high-risk patients [67, 68].
Immune Checkpoint Inhibitors
As ICI-associated myocarditis is an autoimmune phenomenon, it is best treated with immunosuppression. The available evidence to date supports the use of steroids. In previous retrospective studies, the use of steroids was associated with improved systolic function and reduced major adverse cardiovascular events [25, 27]. The ASCO consensus authors recommend initial doses of prednisone 1–2 mg/kg/day for severe cases of myocarditis [58]. Patients who develop myocarditis should generally not be re-challenged with ICI given the substantial morbidity and mortality associated with ICI myocarditis, although further investigation is needed.
Radiation
There is no specific management for radiation induced cardiac dysfunction. Treatment is focused on the specific cardiotoxicity developed such as valvular heart disease, pericardial constriction, coronary disease, or restrictive cardiomyopathy. Therefore, it is imperative to reduce radiation exposure to the heart whenever possible. Newer techniques such as cardiac shielding, breath holding, and proton therapy have helped to reduce collateral cardiac exposure [28, 69]. Modification of other cardiovascular risk factors is also recommended given their association with worse outcomes [28].
Stage A Heart Failure Management
Clinicians should take all possible steps to minimize cardiotoxicity for patients receiving potentially cardiotoxic cancer therapies. In addition to appropriate screening and surveillance detailed above, additional steps may help to prevent the development of CTRC.
All patients at risk for cardiotoxicity should clearly be screened for potential cardiovascular risk factors such as hypertension, diabetes, tobacco use, and hyperlipidemia [11•, 59]. As mentioned above, these risk factors increase the risk of CTRC. Risk factors should be optimized before and during cancer treatment with a low threshold for cardiology consultation. Hypertension should be treated in accordance with the ACC/AHA guidelines for stage A HF with a blood pressure target of < 130/80 [44]. Statins have been associated with attenuated EF decline in patients receiving anthracyclines and should be considered in anyone with an indication for one [70].
The role of neurohormonal antagonists in patients receiving anthracyclines is controversial due to conflicting findings from multiple small trials. Carvedilol may attenuate the decline in systolic function in patients receiving anthracyclines [71,72,73]. However, other studies did not show benefit with beta-blockers [74, 75]. In the recently published CECCY trial, prophylactic use of carvedilol did not protect against LV systolic dysfunction in patients receiving anthracycline-based chemotherapy [76]. Similarly, there is some evidence to support the use of ACEI and ARBs in patients receiving anthracycline-based cancer therapy. The Prevention of Cardiac Dysfunction During Adjuvant Breast Cancer Therapy (PRADA) trial, involving 130 patients, showed that candesartan reduced LVEF decline in patients receiving anthracycline-based cancer therapy [77]. As with beta blockers, the evidence is somewhat conflicting [75]. In the OVERCOME trial, the use of enalapril and carvedilol was associated with a significant attenuation in EF decline in patients receiving anthracyclines, perhaps highlighting a potential benefit of combination therapy [78]. Interestingly, patients treated with both enalapril and carvedilol also had significantly lower rates of the combined endpoint of death or heart failure. To date, this is the only trial that demonstrated an effect of neurohormonal blockade on major HF events in stage A heart failure.
Similarly, the use of neurohormonal blockade is controversial in stage A HF patients receiving trastuzumab [79]. In the MANTICORE (Multidisciplinary Approach to Novel Therapies in Cardiology Oncology Research) trial, the combination of perindopril and bisoprolol was associated with attenuated decline in LV function [80]. Perhaps more importantly, the use of these medications was associated with less interruption in trastuzumab therapy. Similar to anthracyclines, there is little data demonstrating a reduction in major HF endpoints with the use of ACEI/ARBs or beta blockers in stage A HF.
At this time, there is insufficient evidence to recommend the widespread use of beta blockers or ACEI/ARBs in all stage A HF patients receiving cardiotoxic cancer treatment. Decisions regarding these medications should be individualized by the treating physician. We agree with the ESMO consensus statement which states that beta blockers and ACE/ARB should be considered in patients at high risk for cardiotoxicity; however, what defines high risk and which stage A HF patients most benefit is poorly understood [59]. Our authors recommend the use of ACEI/ARBs and beta blockers in patients with subclinical LV dysfunction as defined by abnormal strain or positive biomarkers in response to cardiotoxic cancer treatment (Fig. 8). This is supported by a study by Cardinale et al. in which the use of enalapril resulted in less cardiotoxicity in patients with elevated troponin after high dose chemotherapy [81]. As above, the SUCCOUR trial is also currently underway to evaluate the prognostic benefit of strain imaging in this population [50].
Stage B Heart Failure Management
In patients who develop overt LV dysfunction (ACC/AHA stage B), multidisciplinary care is required to determine the optimal management of HF and cancer treatment.
The medical management of patients with stage B heart failure secondary to cancer treatment should be in accordance with the 2017 ACC/AHA Heart failure guidelines [44]. ACEI/ARBs, and beta blockers are recommended in anyone with LVEF ≤ 50% (class I, LOE-A). In a study by Cardinale et al., earlier intervention with neurohormonal blockade in patients who developed anthracycline-mediated LV dysfunction resulted in improved LV recovery and lower cardiovascular event rates [82]. The benefit of early initiation of HF therapies has been supported in other small trials as well [9].
All cardiomyopathy in patients receiving cancer treatment should not be assumed to be related to CTRC. The diagnosis of cancer treatment–related cardiomyopathy is a diagnosis of exclusion, and a comprehensive search for alternative etiologies—particularly ischemia—should also be undertaken.
Stage C Heart Failure Management
Just as in stage B patients, those who develop symptomatic HF due to cancer treatment should be managed in accordance with the ACC/AHA HF guidelines [44]. All patients with LVEF ≤ 50% should receive beta blockers and ACEI/ARBs (class I, LOE-A). In addition, patients with symptomatic HF (NYHA classes II–IV) with LVEF ≤ 35% should receive mineralocorticoid antagonists such as eplerenone or spironolactone (class I, LOE-A). Based on data from the landmark PARADIGM trial, the angiotensin neprolysin inhibitor (ARNI) sacubitril-valsartan is also recommended for all patients with LVEF ≤ 35% with NYHA class II–III symptoms [83].
Device-based interventions in patients with CTRC should also be in accordance with the ACC/AHA guidelines. Implantable cardioverter-defibrillator (ICD) should be considered in patients with LVEF ≤ 35% with NYHA class II–III symptoms (class I-LOE A) [44]. Patients being considered for ICD should have a prognosis ≥ 1 year, as the benefit of ICD is generally only seen beyond this point. Clarification of hematologic/oncologic prognosis is necessary prior to implantation. Cardiac resynchronization therapy (CRT) should also be considered in patients with LVEF ≤ 35% and QRS > 150 ms with left bundle branch block morphology on electrocardiogram (class I-LOE A). There is evidence that benefits with CRT are similar in anthracycline-mediated cardiomyopathy when compared with non-ischemic cardiomyopathy (NICM) [84].
Stage D Heart Failure
In patients with stage D heart failure, survival is poor without advanced heart failure therapies such as heart transplantation or left ventricular assist device (LVAD). Post-transplant survival of patients with CTRC appears to be comparable to cardiomyopathy from other causes. In a large retrospective registry study of 232 CTRC and 8890 NICM patients, there was no difference in survival at 1, 3, or 5 years amongst groups [85]. Unsurprisingly, rates of post-transplant malignancies were higher in the CTRC group. This highlights the need for careful patient selection in CRTC given the increased risk of post-transplant malignancy due to immunosuppression.
Outcomes with LVAD in CTRC patients are comparable to patients with other forms of cardiomyopathy [86]. Rates of RV dysfunction and need for right ventricular assist device (RVAD) after LVAD do appear to be higher in patients with CTRC [86]. This is unsurprising as patients with CTRC tend to have biventricular dysfunction [87].
Conclusion
Overall, cardiomyopathy is a significant cause of morbidity and mortality in patients receiving cancer treatment. While best described in patients receiving anthracyclines, trastuzumab, and radiation therapy, CTRC is being increasingly recognized in patients being treated with other cancer therapies including immune checkpoint inhibitors, tyrosine kinase inhibitors, and proteasome inhibitors. With an increasing number of cancer survivors, it is imperative for cardiologists to be able to diagnose and manage patients with CTRC. While high-quality evidence is lacking, expert consensus recommends initial imaging and close surveillance in patients receiving anthracyclines and HER-2/ERB antagonists, particularly in those at high risk. While echocardiogram remains the screening modality of choice, the role of biomarkers as well as advanced imaging modalities such as CMR is rapidly evolving. In patients with stage A HF, neurohormonal blockade such as ACEI, ARBs, or beta blockers may be considered, although the body of evidence supporting this is currently weak. Once symptomatic heart failure has developed, treatment should be in accordance with the ACC/AHA HF guidelines. Patients with advanced heart failure due to cancer treatment appear to have good clinical outcomes with advanced HF therapies. Therefore, LVAD and heart transplantation may be considered in appropriate candidates. The primary goal of the treating cardiologist is to optimize cardiac function and continue life-saving cancer treatment whenever possible. Decisions regarding the withholding or modification of cancer treatment are complex and should involve multidisciplinary discussions between the treating cardiologist and hematologist/oncologist.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Reboux G. Cancer. https://www.who.int/news-room/fact-sheets/detail/cancer. September 12, 2018. Accessed November 11, 2019.
American Society of Clinical Oncology. The state of cancer care in America, 2015: a report by the American Society of Clinical Oncology. Journal of Oncology Practice. 2015;11(2):79–113.
Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Research BCR. 2011;13(3):R64.
Lefrak EA, Pitha J, Rosenheim S, Gottlieb JA. A clinicopathologic analysis of adriamycin cardiotoxicity. Cancer. 1973;32(2):302–14.
• Chang H-M, Moudgil R, Scarabelli T, Okwuosa TM, Yeh ETH. Cardiovascular complications of cancer therapy: best practices in diagnosis, prevention, and management: part 1. Journal of the American College of Cardiology. 2017;70(20):2536–51. This paper discusses about the best practice guidelines for management of cancer-therapy mediated cardiomyopathy.
Zhang S, Liu X, Bawa-Khalfe T, Lu L-S, Lyu YL, Liu LF, et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nature Medicine. 2012;18(11):1639–42.
Ky B. In: Zypes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, editors. Cardio-oncology. Braunwald’s heart disease: a textbook of cardiovascular medicine. Philadelphia: Elsevier; 2015.
Wouters KA, Kremer LCM, Miller TL, Herman EH, Lipshultz SE. Protecting against anthracycline-induced myocardial damage: a review of the most promising strategies. British Journal of Haematology. 2005;131(5):561–78.
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131(22):1981–8.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79.
• Armenian SH, Lacchetti C, Lenihan D. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline summary. Journal of Oncology Practice. 2017;13(4):270–5. This paper is a consensus document which discusses the role of close monitoring and surveillance in cancer survivors.
Qin A, Thompson CL, Silverman P. Predictors of late-onset heart failure in breast cancer patients treated with doxorubicin. Journal of Cancer Survivorship: Research and Practice. 2015;9(2):252–9.
Armstrong GT, Joshi VM, Ness KK, Marwick TH, Zhang N, Srivastava DK, et al. Comprehensive echocardiographic detection of treatment-related cardiac dysfunction in adult survivors of childhood cancer: results from the St. Jude Lifetime Cohort Study. Journal of the American College of Cardiology. 2015;65(23):2511–22.
Vejpongsa P, Yeh ETH. Prevention of anthracycline-induced cardiotoxicity: challenges and opportunities. Journal of the American College of Cardiology. 2014;64(9):938–45.
Armenian, Saro, and Smita Bhatia. Predicting and preventing anthracycline-related cardiotoxicity. American Society of Clinical Oncology Educational Book. American Society of Clinical Oncology. Annual Meeting 38 (2018): 3–12.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. The New England Journal of Medicine. March 15, 2001;344(11):783–92.
Keulenaer D, Gilles W, Doggen K, Lemmens K. The vulnerability of the heart as a pluricellular paracrine organ: lessons from unexpected triggers of heart failure in targeted ErbB2 anticancer therapy. Circulation Research. 2010;106(1):35–46.
•• Bloom MW, Hamo CE, Cardinale D, Ky B, Nohria A, Baer L, et al. Cancer therapy-related cardiac dysfunction and heart failure: part 1: definitions, pathophysiology, risk factors, and imaging. Circulation. Heart Failure. 2016;9(1):e002661. This paper provides comprehensive review of cancer therapy-related cardiomyopathy enumerating the etiology, risk factors, and screening modalities.
Procter M, Suter TM, de Azambuja E, Dafni U, van Dooren V, Muehlbauer S, et al. Longer-term assessment of trastuzumab-related cardiac adverse events in the herceptin adjuvant (HERA) trial. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2010;28(21):3422–8.
Advani PP, Ballman KV, Dockter TJ, Colon-Otero G, Perez EA. Long-term cardiac safety analysis of NCCTG N9831 (alliance) adjuvant trastuzumab trial. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. February 20, 2016;34(6):581–7.
Bowles EJ, Aiello RW, Feigelson HS, Onitilo AA, Freedman AN, Delate T, et al. Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. Journal of the National Cancer Institute. 2012;104(17):1293–305.
Chen J, Long JB, Hurria A, Owusu C, Steingart RM, Gross CP. Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. Journal of the American College of Cardiology. 2012;60(24):2504–12.
Perez EA, Rodeheffer R. Clinical cardiac tolerability of trastuzumab. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2004;22(2):322–9.
Nishimura H, Okazaki T, Tanaka Y, Nakatani K, Hara M, Matsumori A, et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science (New York, N.Y.). 2001;291(5502):319–22.
Escudier M, Cautela J, Malissen N, Ancedy Y, Orabona M, Pinto J, et al. Clinical features, management, and outcomes of immune checkpoint inhibitor-related cardiotoxicity. Circulation. 2017;136(21):2085–7.
Johnson DB, Balko JM, Compton ML, Chalkias S, Gorham J, Xu Y, et al. Fulminant myocarditis with combination immune checkpoint blockade. The New England Journal of Medicine. 2016;375(18):1749–55.
Mahmood SS, Fradley MG, Cohen JV, Nohria A, Reynolds KL, Heinzerling LM, et al. Myocarditis in patients treated with immune checkpoint inhibitors. Journal of the American College of Cardiology. 2018;71(16):1755–64.
Desai MY, Windecker S, Lancellotti P, Bax JJ, Griffin BP, Cahlon O, et al. Prevention, diagnosis, and management of radiation-associated cardiac disease: JACC Scientific Expert Panel. Journal of the American College of Cardiology. 2019;74(7):905–27.
van Nimwegen FA, Schaapveld M, Janus CPM, Krol ADG, Petersen EJ, Raemaekers JMM, et al. Cardiovascular disease after Hodgkin lymphoma treatment: 40-year disease risk. JAMA Internal Medicine. 2015;175(6):1007–17.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. The New England Journal of Medicine. March 14, 2013;368(11):987–98.
Saiki H, Petersen IA, Scott CG, Bailey KR, Dunlay SM, Finley RR, et al. Risk of heart failure with preserved ejection fraction in older women after contemporary radiotherapy for breast cancer. Circulation. April 11, 2017;135(15):1388–96.
van Nimwegen FA, Ntentas G, Darby SC, Schaapveld M, Hauptmann M, Lugtenburg PJ, et al. Risk of heart failure in survivors of Hodgkin lymphoma: effects of cardiac exposure to radiation and anthracyclines. Blood. 2017;129(16):2257–65.
Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. The Lancet. Oncology. August 2005;6(8):557–65.
Patrizio L, Nkomo VT, Badano LP, Bergler-Klein J, Bergler J, Bogaert J, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Journal of the American Society of Echocardiography: Official Publication of the American Society of Echocardiography. 2013;26(9):1013–32.
Dess RT, Sun Y, Matuszak MM, Sun G, Soni PD, Bazzi L, et al. Cardiac events after radiation therapy: combined analysis of prospective multicenter trials for locally advanced non-small-cell lung cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2017;35(13):1395–402.
Goldberg MA, Antin JH, Guinan EC, Rappeport JM. Cyclophosphamide cardiotoxicity: an analysis of dosing as a risk factor. Blood. 1986;68(5):1114–8.
Zver S, Zadnik V, Bunc M, Rogel P, Cernelc P, Kozelj M. Cardiac toxicity of high-dose cyclophosphamide in patients with multiple myeloma undergoing autologous hematopoietic stem cell transplantation. International Journal of Hematology. 2007;85(5):408–14.
Siegel D, Martin T, Nooka A, Harvey RD, Vij R, Niesvizky R, et al. Integrated safety profile of single-agent carfilzomib: experience from 526 patients enrolled in 4 phase II clinical studies. Haematologica. 2013;98(11):61–1753.
Abdel-Qadir H, Ethier J-L, Lee DS, Thavendiranathan P, Amir E. Cardiovascular toxicity of angiogenesis inhibitors in treatment of malignancy: a systematic review and meta-analysis. Cancer Treatment Reviews. 2017;53:120–7.
Chu TF, Rupnick MA, Kerkela R, Dallabrida SM, Zurakowski D, Nguyen L, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet (London, England). 2007;370(9604):2011–9.
Di Lorenzo G, Autorino R, Bruni G, Cartenì G, Ricevuto E, Tudini M, et al. Cardiovascular toxicity following sunitinib therapy in metastatic renal cell carcinoma: a multicenter analysis. Annals of Oncology: Official Journal of the European Society for Medical Oncology. September 2009;20(9):1535–42.
Ezaz G, Long JB, Gross CP, Chen J. Risk Prediction Model for Heart Failure and Cardiomyopathy after Adjuvant Trastuzumab Therapy for Breast Cancer. Journal of the American Heart Association. 2014;3(1):e000472.
Dranitsaris G, Rayson D, Vincent M, Chang J, Gelmon K, Sandor D, et al. The development of a predictive model to estimate cardiotoxic risk for patients with metastatic breast cancer receiving anthracyclines. Breast Cancer Research and Treatment. 2008;107(3):443–50.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America. Journal of Cardiac Failure. et al., 2017;23(8):628–51.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Journal of the American College of Cardiology. 2013;62(16):e147-239.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European Heart Journal Cardiovascular Imaging. 2014;15(10):1063–93.
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. Journal of the American College of Cardiology. 2013;61(1):77–84.
Thavendiranathan P, Poulin F, Lim K-D, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. Journal of the American College of Cardiology. 2014;63(25 Pt A):2751–68.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Tan TC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circulation. Cardiovascular Imaging. 2012;5(5):596–603.
Negishi T. Paaladinesh Thavendiranathan, Kazuaki Negishi, Thomas H. Marwick, and SUCCOUR investigators. Rationale and design of the strain surveillance of chemotherapy for improving cardiovascular outcomes: the SUCCOUR Trial. JACC. Cardiovascular Imaging. 2018;11(8):1098–105.
Zhang L, Awadalla M, Mahmood SS, Groarke JD, Nohria A, Liu S, et al. Late gadolinium enhancement in patients with myocarditis from immune checkpoint inhibitors. Journal of the American College of Cardiology. 2019;73(9 Supplement 1):675.
Cardinale D, Sandri MT, Martinoni A, Tricca A, Civelli M, Lamantia G, et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy. Journal of the American College of Cardiology. 2000;36(2):517–22.
Cardinale D, Sandri MT, Colombo A, Colombo N, Boeri M, Lamantia G, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109(22):2749–54.
Cardinale D, Colombo A, Torrisi R, Sandri MT, Civelli M, Salvatici M, et al. Trastuzumab-induced cardiotoxicity: clinical and prognostic implications of troponin I evaluation. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2010;28(25):3910–6.
Romano S, Fratini S, Ricevuto E, Procaccini V, Stifano G, Mancini M, et al. Serial measurements of NT-ProBNP are predictive of not-high-dose anthracycline cardiotoxicity in breast cancer patients. British Journal of Cancer. 2011;105(11):1663–8.
Sandri MT, Salvatici M, Cardinale D, Zorzino L, Passerini R, Lentati P, et al. N-terminal pro-B-type natriuretic peptide after high-dose chemotherapy: a marker predictive of cardiac dysfunction? Clinical Chemistry. 2005;51(8):1405–10.
FDA Drug Label for HERCEPTIN- trastuzumab. Available at: http:// dailymed.nlm.nih.gov.ezproxy.hsclib.sunysb.edu/dailymed/drugInfo. cfm?setid = 492dbdb2-077e-4064-bff3-372d6af0a7a2%3E.
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2018;36(17):1714–68.
Curigliano G, Cardinale D, Suter T, Plataniotis G, de Azambuja E, Sandri MT, et al. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO clinical practice guidelines. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2012;23(Suppl 7):vii155–66.
Valdivieso M, Burgess MA, Ewer MS, Mackay B, Wallace S, Benjamin RS, et al. Increased therapeutic index of weekly doxorubicin in the therapy of non-small cell lung cancer: a prospective, randomized study. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 1984;2(3):207–14.
Swain SM, Whaley FS, Gerber MC, Weisberg S, York M, Spicer D, et al. Cardioprotection with dexrazoxane for doxorubicin-containing therapy in advanced breast cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 1997;15(4):1318–32.
Marty M, Espié M, Llombart A, Monnier A, Rapoport BL, Stahalova V, et al. Multicenter randomized phase III study of the cardioprotective effect of dexrazoxane (cardioxane) in advanced/metastatic breast cancer patients treated with anthracycline-based chemotherapy. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2006;17(4):614–22.
Tebbi CK, London WB, Friedman D, Villaluna D, De Alarcon PA, Constine LS, et al. Dexrazoxane-associated risk for acute myeloid leukemia/myelodysplastic syndrome and other secondary malignancies in pediatric Hodgkin’s disease. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2007;25(5):493–500.
Ewer MS, Vooletich MT, Durand J-B, Woods ML, Davis JR, Valero V, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2005;23(31):7820–6.
Yu AF, Yadav NU, Eaton AA, Lung BY, Thaler HT, Liu JE, et al. Continuous trastuzumab therapy in breast cancer patients with asymptomatic left ventricular dysfunction. The Oncologist. 2015;20(10):1105–10.
Lynce F, Barac A, Geng X, Dang C, Yu AF, Smith KL, et al. Prospective evaluation of the cardiac safety of HER2-targeted therapies in patients with HER2-positive breast cancer and compromised heart function: the SAFE-HEaRt study. Breast Cancer Research and Treatment. 2019;175(3):595–603.
Azim H, Azim HA, Escudier B. Trastuzumab versus lapatinib: the cardiac side of the story. Cancer Treatment Reviews. 2009;35(7):633–8.
Lenihan D, Suter T, Brammer M, Neate C, Ross G, Baselga J. Pooled analysis of cardiac safety in patients with cancer treated with pertuzumab. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2012;23(3):791–800.
Drost L, Yee C, Lam H, Zhang L, Wronski M, McCann C, et al. A systematic review of heart dose in breast radiotherapy. Clinical Breast Cancer. 2018;18(5):e819–24.
Acar Z, Kale A, Turgut M, Demircan S, Durna K, Demir S. Murat Meriç, and Mustafa Tarık Ağaç. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. Journal of the American College of Cardiology. 2011;58(9):988–9.
Kalay N, Basar E, Ozdogru I, Er O, Cetinkaya Y, Dogan A. Tugrul Inanc, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. Journal of the American College of Cardiology. 2006;48(11):2258–62.
Jhorawat R, Kumari S, Varma SC, Rohit MK, Narula N, Suri V, et al. Preventive role of carvedilol in adriamycin-induced cardiomyopathy. The Indian Journal of Medical Research. 2016;144(5):725–9.
Nabati M, Janbabai G, Baghyari S, Esmaili K, Yazdani J. Cardioprotective Effects of Carvedilol in Inhibiting Doxorubicin-Induced Cardiotoxicity. Journal of Cardiovascular Pharmacology. 2017;69(5):279–85.
Salehi R, Zamani B, Esfehani A, Ghafari S, Abasnezhad M, Goldust M. Protective effect of carvedilol in cardiomyopathy caused by anthracyclines in patients suffering from breast cancer and lymphoma. The American Heart Hospital Journal. 2011;9(2):95–8.
Georgakopoulos P, Roussou P, Matsakas E, Karavidas A, Anagnostopoulos N, Marinakis T, et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. American Journal of Hematology. 2010;85(11):894–6.
Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR, das Dores Cruz F, Brandão SMG, Rigaud VOC, et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. Journal of the American College of Cardiology. 2018;71(20):2281–90.
Gulati G, Heck SL, Ree AH, Hoffmann P, Schulz-Menger J, Fagerland MW, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. European Heart Journal. 2016;37(21):1671–80.
Bosch X, Rovira M, Sitges M, Domènech A, Ortiz-Pérez JT, de Caralt TM, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME Trial (PreventiOn of Left Ventricular Dysfunction with Enalapril and CaRvedilol in Patients Submitted to Intensive ChemOtherapy for the Treatment of Malignant HEmopathies). Journal of the American College of Cardiology. 2013;61(23):2355–62.
Boekhout AH, Gietema JA, Kerklaan BM, van Werkhoven ED, Altena R, Honkoop A, et al. Angiotensin II-receptor inhibition with candesartan to prevent trastuzumab-related cardiotoxic effects in patients with early breast cancer: a randomized clinical trial. JAMA Oncology. 2016;2(8):1030–7.
Pituskin E, Mackey JR, Koshman S, Jassal D, Pitz M, Haykowsky MJ, et al. Multidisciplinary approach to novel therapies in cardio-oncology research (MANTICORE 101-Breast): a randomized trial for the prevention of trastuzumab-associated cardiotoxicity. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2017;35(8):870–7.
Cardinale D, Colombo A, Sandri MT, Lamantia G, Colombo N, Civelli M, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114(23):2474–81.
Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacomi G, et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. Journal of the American College of Cardiology. 2010;55(3):213–20.
McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. The New England Journal of Medicine. 2014;371(11):993–1004.
Rickard J, Kumbhani DJ, Baranowski B, Martin DO, Tang WH, Wilkoff BL. Usefulness of cardiac resynchronization therapy in patients with adriamycin-induced cardiomyopathy. The American Journal of Cardiology. 2010;105(4):522–6.
Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. The Journal of Heart and Lung Transplantation: The Official Publication of the International Society for Heart Transplantation. 2012;31(8):805–10.
Oliveira, Guilherme H., Matthias Dupont, David Naftel, Susan L. Myers, Ya Yuan, W. H. Wilson Tang, Gonzalo Gonzalez-Stawinski, James B. Young, David O. Taylor, and Randall C. Starling. Increased need for right ventricular support in patients with chemotherapy-induced cardiomyopathy undergoing mechanical circulatory support: outcomes from the INTERMACS Registry (Interagency Registry for Mechanically Assisted Circulatory Support). Journal of the American College of Cardiology 63, no. 3 (2014): 240–48.
Tanindi A, Demirci U, Tacoy G, Buyukberber S, Alsancak Y, Coskun U, et al. Assessment of right ventricular functions during cancer chemotherapy. European Journal of Echocardiography: The Journal of the Working Group on Echocardiography of the European Society of Cardiology. 2011;12(11):834–40.
Funding
Dr. Addison was supported in part by an NIH K12‐CA133250 grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nonpharmacologic Therapy: Surgery, Ventricular Assist Devices, Biventricular Pacing, and Exercise
Rights and permissions
About this article
Cite this article
Slivnick, J., Vallakati, A., Addison, D. et al. Personalized Approach to Cancer Treatment–Related Cardiomyopathy. Curr Heart Fail Rep 17, 43–55 (2020). https://doi.org/10.1007/s11897-020-00453-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-020-00453-3