Abstract
Purpose of Review
The goal of this review is to present and summarize studies on endoscopic findings in eosinophilic esophagitis (EoE), at diagnosis and in response to treatment, utilizing rigorous peer-reviewed literature in children wherever possible and to introduce a recently proposed standardized endoscopic evaluation system.
Recent Findings
Gold standard of diagnosis and assessment of response to therapy in EoE requires multiple endoscopies with biopsies for histology, which allows for observation of the esophageal mucosa. Typical endoscopic findings in patients with EoE include edema, exudate, furrowing, concentric rings, and strictures. Endoscopic findings have been broadly characterized into inflammatory features (edema, exudate, furrowing) and fibro-stenotic features (rings, stricture), in order to better reflect their underlying pathophysiology. Recent studies suggest strong correlations between endoscopic findings, through composite scoring systems, and histology, and therefore may be helpful as part of disease surveillance. The EoE Endoscopic Reference Score (EREFS) classification system was proposed in 2013 as an outcome metric for standardization in reporting endoscopic signs of EoE. Subsequent studies support utility of composite scoring, which utility has similarly been seen in pediatric treatment trials.
Summary
Endoscopy in children provides insight into the natural history of EoE, with progressively more fibro-stenotic features occurring over time, giving an additional perspective into esophageal remodeling and response to treatment. Recognition of typical endoscopic findings at diagnosis and upon repeat endoscopy has allowed a clinician to monitor visual changes in esophageal mucosal health. Further studies to assess the role of composite scoring in disease management are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eosinophilic esophagitis (EoE) is a chronic immune/antigen-mediated disease characterized by symptoms of esophageal dysfunction and eosinophil-predominant esophageal inflammation. Consensus guidelines for diagnosis of EoE in children require 6–8 weeks of high dose proton pump inhibitor (PPI) followed by esophagogastroduodenoscopy (EGD) with esophageal biopsies demonstrating at least 15 eosinophils per high power field (eos/hpf) [1]. Neither visual findings on endoscopy nor esophageal eosinophilia are unique findings specific to EoE, as they can be found in other diseases of the esophagus including GERD, proton-pump inhibitor-responsive eosinophilia (PPI-REE), infection, connective tissue diseases, and achalasia [2]. Over the past several years significant progress has been made in the identification of endoscopic findings and understanding their underlying meaning and utility. Visual evaluation of the esophagus is an important emerging tool that in conjunction with histology aids in diagnosis and routine disease surveillance of EoE. The goal of this review is to present and summarize studies on endoscopic findings in EoE relating to diagnosis and responses to treatment, utilizing rigorous peer-reviewed literature in children wherever possible, and to introduce recent novel innovations.
Endoscopic Findings at Diagnosis
At diagnosis, most patients with EoE have an abnormal appearing esophagus during endoscopy [2,3,4]. Typical endoscopic findings in patients with EoE include edema (decreased vasculature, pallor), exudate (superficial white specks coating the mucosa), furrowing (linear lines, longitudinal to the esophageal axis), concentric rings (“trachealization”), and strictures [1, 5,6,7,8]. Examples of visual findings in EoE are shown in Fig. 1. Between 10 and 33% of children diagnosed with EoE have been reported as having visually normal esophageal mucosa [3, 4••, 9]. Each endoscopic finding may occur in isolation or combination. Exudate, first reported as white specks in the esophagus in children [8], represent aggregation of eosinophils on the surface of the esophageal mucosa. In two of the earliest reports of EoE, exudates were identified as a hallmark finding [10,11,12]. Furrowing, which can be patchy or diffuse, consists of vertical lines caused by thickening of the mucosa and submucosa [12]. In 2003, Kaplan et al. noted “soft and subtle rings” in the esophagus in seven of eight EoE patients, and rigidity in three of the eight, describing these rings as a “feline esophagus,” because of its similarity to the normal endoscopic findings in a cat’s esophagus, which has the appearance of trachea with multiple rings [13]. Strictures may occur at any segment along the esophageal length, but they are most commonly found in adults and are rarely seen in children [1, 4••].
Inflammatory Vs Fibro-Stenotic Features
The last decade has witnessed the emerging characterization of endoscopic findings into inflammatory and fibro-stenotic features, thought to reflect their underlying pathophysiology. Whereas edema, exudate, and furrows are thought to reflect an inflammatory process, rings and strictures reflect fibrosis and esophageal remodeling. A device measuring the cross-sectional area of the esophagus while measuring intra-luminal pressure during controlled volume distension found more severe rings were associated with a lower distensibility plateau, whereas severity of exudates and furrows were not [14]. Indeed, a second study found no significant difference in distensibility between patients with endoscopically visible rings and those with strictures [15], supporting rings as a gradual process of fibrosis to be monitored, with prompt concern for progression or development of stricture. A Swiss EoE registry demonstrated that duration of symptoms before diagnosis was the most significant factor that predicted stricture formation, in a time-dependent manner, supporting untreated inflammation as a strong determinant of fibrosis [16]. Dellon et al. in 2014 found the likelihood of fibro-stenotic disease increased markedly with age: the odds doubled with every 10-year increase in age [17]. Mean symptom length before diagnosis was shorter for inflammatory features of EoE compared to other endoscopic findings. Notably, while age has been shown to correlate positively with esophageal distensibility in control patients, EoE patients have reduced distensibility even when controlling for age [18]. Active inflammation (≥ 15 eos/hpf), histologic lamina propria fibrosis, and various features of a fibrotic phenotype (stricture, food impaction, circumferential rings on endoscopy) were associated with decreased distensibility [18]. Thus children are likely to have inflammatory endoscopic findings at diagnosis though normal findings are also possible. Children are less likely than adults to have evidence of fibro-stenosis, which suggests long-standing disease.
Prevalence of Endoscopic Findings
The underlying etiology of each endoscopic finding is unclear, but significant insight has been gained from studies examining prevalence and variation with age. Clinical and endoscopic features of children and adults with EoE differ quite significantly, and this may be due in part to the inherently inflammatory nature of pediatric EoE and their respective endoscopic findings versus the progressive fibrosis that occurs with increasing age [1, 4••, 18, 19]. A meta-analysis of 100 studies, of both adults and children, in 2012 by Kim et al., reported prevalence of visual findings including edema (41%), exudate (27%), furrowing (48%), and rings (44%). At least one endoscopic abnormality was observed in 93% of patients [4••]. This study also noted that there were significant differences in the visual findings between children and adults, with edema (58 vs 18%) and exudate (36 vs 19%) more common in children whereas rings (11 vs 57%) and strictures (8 vs 25%) were more common in adults. In a large retrospective pediatric study comprised of 381 patients, Liacouras et al. reported abnormal findings in 68%, finding 41% with furrowing, 12% with rings, and 15% with exudate. There were no strictures reported in this cohort. A recent prospective pediatric elimination diet study of 78 patients demonstrated 70% with edema, 73% with furrows, 54% with exudate, 12% with rings, and 1% with strictures prior to treatment [20••]. A summary of studies performed over the past decade showing the prevalence of visual findings is provided in Table 1. Such a pronounced variation and clear impact of age on endoscopic findings relates to the natural course of inflammation but more importantly suggests that multiple phenotypes of EoE exist, and a need for ongoing research. The differences in endoscopic manifestations with age may also explain why while children tend to present with heartburn, vomiting, abdominal pain, feeding intolerance, or failure to thrive, while adults primarily present with dysphagia.
Sensitivity, Specificity of Endoscopic Findings
There are no publications identifying a correlation between endoscopic abnormalities and symptoms, since there is clear dissociation between symptoms and histology in EoE [21, 22]. However, interesting insight has been gained from correlations of endoscopic findings, histology, and ultimate diagnosis. Studies of endoscopic findings from children and adults suggest the sensitivity for the diagnosis of EoE range from 50 to 90% [4••, 23]. In the meta-analysis by Kim et al., an overall sensitivity, specificity, pooled positive predictive value (PPV), and pooled negative predictive value (NPV) was assessed for each endoscopic finding. For rings, the overall sensitivity was 48%, specificity of 91%, PPV of 64%, and NPV of 84%. Strictures had a sensitivity of 15%, specificity of 95%, PPV of 51%, and NPV of 76%, while furrows had a sensitivity of 40%, specificity of 95%, PPV of 73%, and NPV of 83%, and edema showed a sensitivity of 43%, specificity of 90%, PPV of 65%, and NPV of 79% [4••]. While the sensitivity of specific findings is low, the sensitivity of at least one endoscopic finding was 87% in the meta-analysis [4••]. In an adult study, 96% of EoE patients had at least one endoscopic finding at initial endoscopy [24••]. Thus, while no individual finding is pathognomonic, the presence of multiple inflammatory and fibro-stenotic endoscopic abnormalities is very suggestive of EoE.
Endoscopic Findings in Children Post Therapy
Routine endoscopy for therapy surveillance has provided information about changes in the gross appearance of esophageal mucosa with therapy. Several publications have assessed the change in endoscopic abnormalities with treatment. In 2007, Aceves et al. utilized and “EoE endoscopy score” in a trial of 20 patients assessing swallowed budesonide as a therapy for EoE in children. With this score, points were allocated based on endoscopic findings; one point was allocated for each specific type of finding if one or two esophageal sites were involved, and two points for pan-esophageal involvement with that finding [25]. Pre-treatment, the mean EoE endoscopy score of 3.6 (ranging from 1 to 6) decreased to 0.8 (ranging from 0 to 5) post-treatment. Most importantly, 18 (90%) of the patients, including the histologic partial-responder and one non-responder, had improved endoscopy scores with steroid therapy. This may be explained in that non-responders in their cohort had a 50–75% reduction in eosinophil count [25].
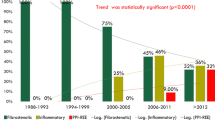
More recently in 2017, Kagalwalla et al. published a prospective four-food elimination diet (FFED) study of 78 patients in which endoscopic changes as well as histologic response to therapy were assessed. Endoscopic features were scored absent (0) or present (+1) and total scoring was derived by summation. Mean endoscopic baseline scores decreased from 2.1 to 1.3 overall in FFED histologic responders. Exudates resolved in 96% of respondents, edema in 66%, furrows in 62%, whereas rings persisted in all subjects from baseline. Therapeutic changes in endoscopic findings from this four-food elimination study are shown in Fig. 2.
Examples of endoscopic findings in patients undergoing elimination diet (a–d) or swallowed steroid (f–h) therapy, pre- and post-treatment. Post-treatment endoscopies are on the right. Patients A, B, and E–G were histologic responders to treatment (post-treatment endoscopy with less than 15 eos/hpf), while C, D, H were histologic non-responders. a Significant improvement in edema and exudate with diet elimination. b Near resolution of edema and furrowing post-treatment. c Improvement of edema and exudate post-treatment with persistence of furrowing. d No significant improvement after diet elimination. e Near complete resolution of findings after steroid therapy with persistence of mild edema. f Normal appearing esophagus after steroid therapy. g Complete resolution of edema and mild exudate following treatment. h Persistence of edema, exudate, and furrowing post-treatment
A pediatric study comparing efficacy of flovent vs budesonide noted a significant improvement or complete resolution of furrows and whitish exudates after treatment with the topical steroids, and a more significant and robust resolution of inflammatory endoscopic findings in the budesonide group compared to the flovent group, especially in the resolution of furrows. Overall, the post-treatment group had a significant reduction in furrowing and exudate, but no significant change in rings [26].
Overall, treatment targeted at histologic eosinophilia improves the inflammatory endoscopic abnormalities in EoE, supporting a role for eosinophilia in these endoscopic abnormalities. Notable from these studies is a small subset of patients with persistent inflammatory endoscopic abnormalities despite resolution of eosinophilia. There may be several explanations for this discrepancy: (1) delayed mucosal healing, (2) persistent inflammation of another cell type, (3) sampling error. While there is limited data regarding the first two possibilities, sampling error could be secondary to insufficient biopsy number or from inflammation deeper in the tissue beyond the mucosa. In most patients, inflammatory endoscopic findings respond to therapy, however fibro-stenotic rings and strictures are more refractory. One of the limitations of the current literature regarding endoscopic changes in children with EoE is the lack of standardized scoring capable of functioning as an outcome metric.
A Scoring Metric Utilizing Endoscopic Findings
In 2013, Hirano et al. proposed the EoE Endoscopic Reference Score (EREFS) classification system as a way for standardization and reporting the endoscopic signs of EoE in adults [27]. This was of particular importance given previous studies concluding that gastroenterologists identified rings and furrows with fair to good reliability, but did not reliably identify exudate or normal images [28], and was meant to counter the poor sensitivity of any individual finding for diagnosis. The EREFS, formally the Endoscopic REFerence Score, notably encompasses each finding in the acronym, and is evaluated as a grading system for exudate, rings, edema, furrowing, and stricture. An atlas of images is a key component of the publication, provided to standardize and improve reporting of endoscopic findings [27]. Exudates are recorded as absent (grade 0) to severe (involving 10% or more of the esophageal mucosa—grade 2), rings as absent (grade 0) to severe (in which distinct rings did not allow a standard adult upper endoscope to pass—grade 3). Edema is recorded as absent (grade 0) to complete loss of vascular markings (grade 2). Finally, furrows are recorded as absent (grade 0) to severe (in which there is visible depth or mucosal indentation—grade 2) [27]. The grading was modified to enhance generalizability via simplifying edema and furrows to absent vs present (0 vs 1). This system has considerably enhanced the degree of agreement between gastroenterologists when assessing features of eosinophilic esophagitis and has allowed for further rigorous studies of endoscopic findings [27, 29].
EREFS Score in EoE: Adults and Children, New Directions
Dellon et al. prospectively assessed the utility of individual component findings and composite aspects of the scoring in EoE diagnosis and treatment response: inflammatory (Edema, Exudate, Furrowing) versus fibro-stenotic (Rings, Strictures) scores [24••]. While the individual component scores did not discriminate histologic severity, likely due to the variable frequency of each individual finding and many different patterns of findings, composite scores accurately identified patients with EoE versus controls. This study found a composite inflammatory score computed by the sum of edema, exudate, and furrowing (range of 0 to 5) had an AUC of 0.936 for diagnosis, whereas a model that contained all five components of the EREFS system as categorical variables had an AUC of 0.946. A model using the total EREFS score had an AUC of 0.934. All scores demonstrated the significant utility of composite scoring to predict EoE status. The EREFS inflammatory score, measuring only edema, furrows, and exudate, had the greatest correlation with changes in mucosal eosinophilia. In addition, patients with EoE who responded to treatment had significantly lower overall scores than histologic non-responders, signifying utility of the scores in surveillance as well. The use of outcome metrics such as EREFS in children has potential to provide a meaningful method to record endoscopic findings in EoE and the changes found with treatment in a validated, scientific manner. However, more studies are needed to evaluate a role in diagnosis and disease surveillance. Ongoing studies, such as the Consortium of Eosinophilic Gastrointestinal Researchers (CEGIR), will assess in a multi-center prospective manner the EREFS’s relationship to histology and molecular pathways.
Application of the EREFS metrics to treatment response has further demonstrated utility and provided promising results. An adult study examined 67 EoE cases and found that total EREFS scores decreased from an average of 3.88 to 2.01 after treatment, with an inflammatory score (the sum of edema, exudate, and furrowing) decreasing from 2.41 to 1.22. This change was most dramatic in the patients who responded histologically to treatment (< 15 eos/hpf), as responders had post-treatment total and inflammatory EREFS scores of 0.45 and 0.63, compared to non-responders (3.24 and 2.00) [24••]. A similar study evaluating response to budesonide demonstrated a baseline mean EREFS score of 7.7 in the budesonide group and 6.9 in the placebo group, while after treatment the scores were reduced to 3.9 and 7.3, respectively [30]. The dramatic difference in endoscopic scores between those with histologic response to therapy and those with non-response signifies a significant correlation of abnormal findings on endoscopy with continued disease activity. Although individual findings have been often described in children and changes noted during therapy, the standardized EREFS classification had not been applied, and its utility for both diagnosis and response to treatment is only now being addressed. Our group recently published a prospective study in children undergoing diagnostic and post-treatment endoscopy using real-time EREFS scoring (31). Composite EREFS inflammatory scores and receiver operating characteristic were determined for incident EoE cases vs controls along with active vs inactive disease post-treatment. A longitudinal cohort with pre- and post-treatment endoscopies was examined to identify how the scores change with therapy. Quite similar to adult findings, an inflammatory score accurately distinguished newly diagnosed EoE patients from controls as well as active disease from inactive disease in a post-treatment cohort [31]. Furrowing was the strongest predictor of eosinophilia, followed by edema and exudate. A significant reduction was found in the EREFS Inflammatory Score in histologic treatment responders (92%) compared to non-responders (53%). As these studies support a strong correlation between EREFS scores and histologic inflammation, the presence of persistent endoscopic abnormalities in patients with histologic remission may reflect insufficient therapy.
Conclusion
Endoscopic findings in eosinophilic esophagitis provide a macroscopic view of the mucosa that is quite unique to this disease process, because of the need for repeat endoscopies to assess the histologic response to therapy. This is particularly true for EoE, given the lack of reliable biomarkers and the poor reliability of symptom improvement with histologic response. Endoscopy of pediatric EoE has provided insight into the natural course of EoE, with progressively more fibro-stenotic features occurring over time with age, illuminating an interesting perspective into esophageal remodeling and treatment success. Repeat endoscopy allows monitoring changes in visual findings in response to treatment. The studies discussed above, as well as evolving literature, demonstrate the importance of endoscopic findings and their reliable correlation with underlying eosinophilia in EoE, and describe a scoring metric that is an effective predictor for response to therapy.
References
Papers of particular interest, published recently, have been highlighted as: ••Of major importance
Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128(1):3–20 e26; quiz 21-22. https://doi.org/10.1016/j.jaci.2011.02.040.
Cianferoni A, Spergel J. Eosinophilic esophagitis: a comprehensive review. Clin Rev Allergy Immunol. 2016;50(2):159–74. https://doi.org/10.1007/s12016-015-8501-z.
Liacouras CA, Spergel JM, Ruchelli E, Verma R, Mascarenhas M, Semeao E, et al. Eosinophilic esophagitis: a 10-year experience in 381 children. Clin Gastroenterol Hepatol. 2005;3(12):1198–206. https://doi.org/10.1016/S1542-3565(05)00885-2.
•• Kim HP, Vance RB, Shaheen NJ, Dellon ES. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:988–996 e985. This meta-analysis is a thorough examination of the published literature regarding the utility of endoscopic findings in adults and children with EoE.
Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133(4):1342–63. https://doi.org/10.1053/j.gastro.2007.08.017.
Straumann A, Rossi L, Simon HU, Heer P, Spichtin HP, Beglinger C. Fragility of the esophageal mucosa: a pathognomonic endoscopic sign of primary eosinophilic esophagitis? Gastrointest Endosc. 2003;57(3):407–12. https://doi.org/10.1067/mge.2003.123.
Gupta SK, Fitzgerald JF, Chong SK, Croffie JM, Collins MH. Vertical lines in distal esophageal mucosa (VLEM): a true endoscopic manifestation of esophagitis in children? Gastrointest Endosc. 1997;45(6):485–9. https://doi.org/10.1016/S0016-5107(97)70178-0.
Lim JR, Gupta SK, Croffie JM, Pfefferkorn MD, Molleston JP, Corkins MR, et al. White specks in the esophageal mucosa: an endoscopic manifestation of non-reflux eosinophilic esophagitis in children. Gastrointest Endosc. 2004;59(7):835–8. https://doi.org/10.1016/S0016-5107(04)00364-5.
Dellon ES. Diagnostics of eosinophilic esophagitis: clinical, endoscopic, and histologic pitfalls. Dig Dis. 2014;32(1-2):48–53. https://doi.org/10.1159/000357009.
Landres RT, Kuster GG, Strum WB. Eosinophilic esophagitis in a patient with vigorous achalasia. Gastroenterology. 1978;74(6):1298–301.
Picus D, Frank PH. Eosinophilic esophagitis. AJR Am J Roentgenol. 1981;136(5):1001–3. https://doi.org/10.2214/ajr.136.5.1001.
Fox VL, Nurko S, Furuta GT. Eosinophilic esophagitis: it’s not just kid’s stuff. Gastrointest Endosc. 2002;56(2):260–70. https://doi.org/10.1016/S0016-5107(02)70188-0.
Kaplan M, Mutlu EA, Jakate S, Bruninga K, Losurdo J, Losurdo J, et al. Endoscopy in eosinophilic esophagitis: “feline” esophagus and perforation risk. Clin Gastroenterol Hepatol. 2003;1(6):433–7. https://doi.org/10.1016/S1542-3565(03)00222-2.
Chen JW, Pandolfino JE, Lin Z, Ciolino JD, Gonsalves N, Kahrilas PJ, et al. Severity of endoscopically identified esophageal rings correlates with reduced esophageal distensibility in eosinophilic esophagitis. Endoscopy. 2016;48(9):794–801. https://doi.org/10.1055/s-0042-107340.
Kwiatek MA, Hirano I, Kahrilas PJ, Rothe J, Luger D, Pandolfino JE. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140(1):82–90. https://doi.org/10.1053/j.gastro.2010.09.037.
Schoepfer AM, Safroneeva E, Bussmann C, Kuchen T, Portmann S, Simon HU, et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology. 2013;145:1230–6. e1231–1232
Dellon ES, Kim HP, Sperry SL, Rybnicek DA, Woosley JT, Shaheen NJ. A phenotypic analysis shows that eosinophilic esophagitis is a progressive fibrostenotic disease. Gastrointest Endosc. 2014;79(4):577–585 e574. https://doi.org/10.1016/j.gie.2013.10.027.
Menard-Katcher C, Benitez AJ, Pan Z, Ahmed FN, Wilkins BJ, Capocelli KE, et al. Influence of age and eosinophilic esophagitis on esophageal distensibility in a pediatric cohort. Am J Gastroenterol. 2017;112(9):1466–73. https://doi.org/10.1038/ajg.2017.131.
Dellon ES. Diagnosis and management of eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2012;10(10):1066–78. https://doi.org/10.1016/j.cgh.2012.06.003.
•• Kagalwalla AF, Wechsler JB, Amsden K, Schwartz S, Makhija M, Olive A, Davis CM, et al. Efficacy of a 4-food elimination diet for children with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2017;15:1698–1707 e7. This prospective pediatric study describes the changes in endoscopic findings with diet elimination therapy.
Pentiuk S, Putnam PE, Collins MH, Rothenberg ME. Dissociation between symptoms and histological severity in pediatric eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2009;48(2):152–60. https://doi.org/10.1097/MPG.0b013e31817f0197.
Safroneeva E, Straumann A, Coslovsky M, Zwahlen M, Kuehni CE, Panczak R, et al. Symptoms have modest accuracy in detecting endoscopic and histologic remission in adults with eosinophilic esophagitis. Gastroenterology. 2016;150(3):581–590 e584. https://doi.org/10.1053/j.gastro.2015.11.004.
Prasad GA, Talley NJ, Romero Y, Arora AS, Kryzer LA, Smyrk TC, et al. Prevalence and predictive factors of eosinophilic esophagitis in patients presenting with dysphagia: a prospective study. Am J Gastroenterol. 2007;102(12):2627–32. https://doi.org/10.1111/j.1572-0241.2007.01512.x.
•• Dellon ES, Cotton CC, Gebhart JH, Higgins LL, Beitia R, Woosley JT, et al. Accuracy of the eosinophilic esophagitis endoscopic reference score in diagnosis and determining response to treatment. Clin Gastroenterol Hepatol. 2016;14:31–9. This prospective study in adults assess the utility of the EREFS scoring system in adults.
Aceves SS, Bastian JF, Newbury RO, Dohil R. Oral viscous budesonide: a potential new therapy for eosinophilic esophagitis in children. Am J Gastroenterol. 2007;102(10):2271–2279; quiz 2280. https://doi.org/10.1111/j.1572-0241.2007.01379.x.
Fable JM, Fernandez M, Goodine S, Lerer T, Sayej WN. Retrospective comparison of fluticasone propionate and oral viscous budesonide in children with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2018;66:26–32
Hirano I, Moy N, Heckman MG, Thomas CS, Gonsalves N, Achem SR. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: validation of a novel classification and grading system. Gut. 2013;62(4):489–95. https://doi.org/10.1136/gutjnl-2011-301817.
Dellon ES, Aderoju A, Woosley JT, Sandler RS, Shaheen NJ. Variability in diagnostic criteria for eosinophilic esophagitis: a systematic review. Am J Gastroenterol. 2007;102(10):2300–13. https://doi.org/10.1111/j.1572-0241.2007.01396.x.
van Rhijn BD, Warners MJ, Curvers WL, van Lent AU, Bekkali NL, Takkenberg RB, et al. Evaluating the endoscopic reference score for eosinophilic esophagitis: moderate to substantial intra- and interobserver reliability. Endoscopy. 2014;46(12):1049–55. https://doi.org/10.1055/s-0034-1377781.
Dellon ES, Katzka DA, Collins MH, Hamdani M, Gupta SK, Hirano I, et al. Budesonide oral suspension improves symptomatic, endoscopic, and histologic parameters compared with placebo in patients with eosinophilic esophagitis. Gastroenterology. 2017;152(4):776–786 e775. https://doi.org/10.1053/j.gastro.2016.11.021.
Wechsler JB, Bolton S, Amsden K, et al. Eosinophilic Esophagitis reference score accurately identifies disease activity and treatment effects in children. Clin gastroenterol hepatol 2017. https://doi.org/10.1016/j.cgh.2017.12.019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Scott Bolton, Kagalwalla Amir, and Joshua Wechsler declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Gastroenterology
Rights and permissions
About this article
Cite this article
Bolton, S.M., Kagalwalla, A.F. & Wechsler, J.B. Eosinophilic Esophagitis in Children: Endoscopic Findings at Diagnosis and Post-intervention. Curr Gastroenterol Rep 20, 4 (2018). https://doi.org/10.1007/s11894-018-0607-z
Published:
DOI: https://doi.org/10.1007/s11894-018-0607-z