Abstract
Purpose of Review
This review aims to provide a summary of the evaluation and treatment of older adults (≥ 65 years) with type 2 diabetes and/or hyperglycemia in the hospital.
Recent Findings
Caring for these older adults requires special considerations. Diabetes is a risk factor for hospitalization and hyperglycemia in the hospital is associated with increased complications and mortality. Treatment plans for hospitalized older adults with diabetes should include a comprehensive geriatric assessment. This team-based approach aims to develop an individualized care plan, with consideration of the patients’ personal goals, comorbidities, functional status, life expectancy, and hypoglycemia risk. Studies from hospitalized middle age and older adults with hyperglycemia can help guide diabetes treatment goals and management in older adults.
Summary
Further studies, examining both glucose targets and care management assessments and treatment plan specifically targeting older adults in the hospital setting, are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 35.6 million Americans will have diabetes (DM) by 2045 [1], while currently nearly 50% of the US population 65 years or older meet criteria for pre-diabetes and up to 33% with DM [2, 3]. Older adults in developed countries are defined as age 65 years and older per the World Health Organization and this age cutoff will be used for this article [3]. Older adults are developing type 2 diabetes (T2DM) at a rate nearly 3× higher than younger adults [4]. Projections indicate that by 2035, older adults will outnumber children for the first time in US history [4, 5].
Among older adults, DM is an independent risk factor for hospitalization and hyperglycemia is associated with increased risk of complications and hospital mortality in critically ill patients [6]. Although older adults may have lower rates of A1c over 9%, compared with patients under 65 years, their hospital discharge rates related to DM are 1.5× higher in those 65–74 years and 2.4× higher in those over 75 years [5, 7]. Furthermore, in older hospitalized adults, new hyperglycemia is associated with increased mortality compared with age-matched controls with a history of DM [8].
The cost of DM care is approximately $300 billion annually; up to 59% of this expenditure is the care of older adults with DM and DM complications [5, 9]. The average estimated cost for DM care in older adults is $11,825 per year, approximately 2× the expenditure for patients under 65 years [10]. Furthermore, older hospitalized adults with T2DM are more likely to be discharged to a transitional care or nursing facility, adding significantly to medical costs [11]. It is critical that providers have an understanding of inpatient DM care in older adults, given the burden of hyperglycemia, DM, and complications in this population.
This population poses several unique considerations, as there is increased risk of DM-related complications and associated morbidity and mortality, geriatric syndromes (GS), and pharmacotherapy-related adverse events [12]. This review aims to provide a summary of initial evaluation and considerations for management of older adults with T2DM and/or hyperglycemia in the hospital.
Pathophysiology in Older Adults
T2DM is an age-related disease, caused by a combination of factors, including genetic, lifestyle, and aging influences, and leading causes of hyperglycemia in this population can be linked to impairment of beta-cell function, decline in insulin secretion, as well as peripheral insulin resistance [13]. Hyperglycemia in acute illness is associated with increased circulating counter-regulatory hormones and pro-inflammatory cytokines, interfering with glucose metabolism, increased gluconeogenesis, and decreased glucose uptake in peripheral tissues [14].
Older adults are at risk for DM complications and the complication burden increases with age and duration of T2DM [15]. Age is a strong predictor of DM-related congestive heart failure, ischemic heart disease, and stroke [9]. The prevalence of diabetic kidney disease exceeds 50% in patients over 65 years and is associated with impaired lower extremity function, disability, and dementia [9]. While cognitive decline is not typically viewed as a DM complication, T2DM increases the risk for vascular dementia and Alzheimer’s disease [9]. These complications lead to decreased functional autonomy and impaired cognition and may contribute to poor self-care and DM management. Goals for DM care in older adults should focus on not just preventing complications per se, but on extending disability-free life expectancy and improving quality of life (QOL) [9, 16]. These goals should be taken into account in the hospital and in transition to outpatient or long-term facilities.
Clinical Presentation in Older Adults
Older adults with DM may not experience typical hyperglycemia symptoms, including polyuria and polydipsia. The renal threshold for glycosuria increases with age and older adults often have decreased thirst sensation. Older adults with DM, therefore, present with non-specific symptoms including fatigue or weight loss [17]. New or progressive DM may manifest as dehydration, confusion, urinary incontinence, slow lower extremity wound healing, and functional disability, and these may be overlooked as presenting symptoms of hyperglycemia [18].
Older adults with longer duration of T2DM are at particular risk for polypharmacy [9]. The National Electronic Injury Surveillance System-Cooperative Adverse Drug Event Surveillance Project evaluated emergency visits and hospitalizations related to adverse drug events in older adults and found that patients ≥ 65 are 2× more likely to present to the emergency department for adverse drug events and 7× more likely to be hospitalized after an emergency visit. Half the hospitalizations for adverse drug events occur in patients ≥ 80 years old [19]. Two of the four most common medications leading to emergency visits are insulin (13.9%) and oral hypoglycemic agents (10.7%) [19]. A significant number of these adverse events are related to hypoglycemia and estimates from Medicare beneficiaries with DM (mean age differed per study year, range between 76.0 and 77.2 years with average standard deviation 7.5 years) demonstrate that hospital admissions for hypoglycemia exceed those for hyperglycemia [19, 20].
Assessment of Older Adults with Diabetes: Outpatient and Inpatient Settings
Diabetes in older adults is accompanied by multiple coexisting medical conditions, as well as an increased prevalence of geriatric syndromes (GS) [21]. Geriatric syndromes refer to a constellation of conditions including functional disabilities, falls, malnutrition, cognitive impairment, depression, delirium, and dementia, which affect DM self-care, health outcomes, and QOL [22]. Care for older adults with DM requires screening for coexisting GS with a comprehensive geriatric assessment (CGA) [22]. The CGA is an evaluation comprised of screening tools and tests, performed by a multidisciplinary team, to address several domains, including medical, psychological, cognitive, social, and functional capacity (Fig. 1). The CGA is not a single billable domain; however, the individual components are required by the centers for Medicare and Medicaid services (CMS) for older adults annually [23]. The goal is to identify abnormalities, develop targeted therapy for reversible causes, and formulate an individualized strategy for older adults, with a focus on QOL and functional status [21]. These assessments are distinct from a standard medical evaluation and guidelines for older adults with DM recommend screening for GS in both the outpatient and inpatient settings [21, 22, 24••, 25, 26]. Routine CGA in older adults has been associated with improved outcomes, including lower mortality rates, lower rates of institutionalization, and slower decline of QOL [27, 28].
The Endocrine Society Guidelines for DM in older adults recommend an overall assessment of health and personal values prior to determining individualized treatment goals and strategies [24••]. Periodic cognitive screening is recommended with baseline testing at DM diagnosis and subsequent screening every 2 to 3 years or if cognitive complaints arise [24••]. Patients with cognitive impairment should receive simplified or de-intensification regimens and all patients over 65 should be treated with regimens aimed at minimizing hypoglycemia [29]. Algorithms for streamlined regimens and simplification strategies exist and have been shown to decrease hypoglycemia duration in older adults without sacrificing glycemic management [30].
Use of the CGA has been well established for the outpatient setting; however, there may be limitations in its routine use in the hospital. Hospitalized older adults with DM are at risk of developing GS as well as progression of underlying conditions [31•]. It is ideal for the inpatient team to consider pre-existing GS and further evaluate in the hospital when appropriate, including considerations of multiple medical conditions, cognition, polypharmacy, and goals of care, where screening tools and assessments are used based on the individual need. Of significance, a full CGA is not necessary for every older hospitalized adult, rather utilizing a patient-centered approach that targets evaluation only in the domains essential to understanding the components relevant to each individual clinical case. The primary team identifies the relevant components of the CGA and evaluations are performed with the help of a multidisciplinary team, where domains may be evaluated by several services, depending on the clinical scenario [32]. This team may include (but is not limited to) consultation services (endocrinology, geriatrics, psychiatry, neurology, and palliative care), diabetes education, physical therapy, occupational therapy, registered dietitians, pharmacy, nursing, and social work (Fig. 2). Upon discharge, an individualized care plan is developed, where several components of the CGA help with this transition, including assessment of functional capacity, and social and financial support.
A prospective study of older adults (age ≥ 70, mean 85.4 years) with T2DM highlights the prevalence of GS in hospitalized patients [33]. Components of the CGA employed in this study found dementia in 27.8%, delirium in 21.1%, depression in 38.9%, and dependency in activities of daily living (ADL) in 91.1%. Cognitive testing was normal in 12.2% of patients and of those with abnormal testing, up to 43.8% had no prior diagnosis of dementia [33]. This study demonstrates the prevalence of functional dependency and unrecognized cognitive impairment in older adults with T2DM, highlighting the importance of evaluating GS in the hospital.
The CGA in older adults is helpful for inpatient clinicians and teams to guide targeted therapy plans in the hospital and at discharge [31•]. A meta-analysis of the effectiveness of inpatient geriatric evaluation and management units (GEMU) found favorable outcomes. A GEMU is a hospital ward focused on care of older adults, where the CGA is utilized to develop an individualized care plan, including a focus on rehabilitation, discharge planning, and early post-hospital follow-up. Hospital environments varied among the 7 studies, including university, community, and veteran affairs medical centers and were conducted in the USA (4 studies) and abroad (3 studies total conducted in Austria, Norway, and Germany). This study found the GEMU approach effective in two distinct areas: less functional decline at discharge (relative risk [RR] = 0.87, 95% CI 0.77–0.99, P = 0.04) and a lower rate of institutionalization 1 year post discharge (RR = 0.78, CI = 0.66–0.92, P = 0.003) [31•]. This analysis evaluated data of 4759 older adults admitted to a GEMU from 7 studies, and highlights similarities, including focus on care coordination with a multidisciplinary team and use of the CGA. However, these interventions were not associated with decreased length of stay or readmission rates and had no effect on mortality [31•].
A complete CGA may lack a practical and efficient method of use in hospital settings. A study of a targeted inpatient geriatric assessment was developed via expert consensus for older hospitalized adults and was tested and validated in this population (mean age 79.5 ± 8.4 years) at a geriatric day hospital in Brazil [34]. This study demonstrated that this one-page assessment of 10 domains (social support, recent hospital admissions, falls, number of medications, ADL, cognitive performance, self-rated health, depressive symptoms, nutritional status, and gait speed) could be utilized in this setting [34]. Further studies evaluating the predictive value of this instrument are needed; however, this tool represents a guide better suited for evaluation of GS in the hospital. In addition, there are diagnostic tools utilized in hospitalized patients that could be adapted for use in older adults with DM [35, 36]. For example, the mini-cog performance assessment has been used in heart failure patients and was shown to help identify high-risk patients [37]. The development of an abbreviated DM distress scale could also be ideal for use in the inpatient setting [38]. Overall, the CGA is a diagnostic and therapeutic approach to developing a treatment plan in older adults and plays a significant role in the inpatient and outpatient settings.
Glycemic Management in Hospitalized Older Adults
Background and Approach to Glycemic Management
Insulin therapy is recommended in hospitalized patients for hyperglycemia starting at a threshold of blood glucose (BG) > 180 mg/dL. The target glucose range of 140–180 mg/dL is recommended for the majority of non-critically and critically ill hospitalized patients [39, 40]. The Endocrine Society Guidelines for older adults recommend a glycemic target of 100–140 mg/dL fasting and 140–180 mg/dL postprandial in the hospital [24••]. However, in older adults, anecdotally, we recommend these guidelines apply to non-critical care patients who are eating. More stringent goals (BG 110–140 mg/dL) may be appropriate in select circumstances, including cardiac surgery patients and in acute ischemic cardiac or neurologic events, with close monitoring for hypoglycemia [17, 39]. More relaxed targets may be appropriate in patients with severe comorbidities, history of hypoglycemia, or limited life expectancy [24••]. Individualized care planning is recommended for hospitalized older adults and incorporates an evaluation of hypoglycemia risk in the context of overall health, functional and cognitive status, and life expectancy [24••, 39]. Further, recommendations indicate that all hospitalized patients with DM or a BG > 140 mg/dL are screened with HbA1c measurement (if not performed in the preceding 3-month period) [24••, 40]. However, more studies are needed to understand the relationship between glucose management, age, and morbidity in the hospital, so that potential modified targets could be correlated with age and glucose across the spectrum.
Glycemic Management in Hospitalized Patients: What Have We Learned for Older Adults?
Critically Ill Patients
Intravenous insulin infusions are the cornerstone of hyperglycemia management in critically ill patients, and its use for hospitalized older adults is ideal. Because of the short half-life of IV insulin, which offers flexibility and rapid dose titration, infusion protocols have been developed in the intensive care unit (ICU). Interestingly, methodologically rigorous studies on glycemic management and their findings from the ICU may be more applicable to older adults then those from the floor, as the mean participant age is higher in the critical care literature. However, it is important to note that several of the ICU studies include patients with “new” hyperglycemia without a history of T2DM.
A sentinel study of glycemic management in the surgical ICU evaluated intensive (goal BG 80–110 mg/dL; mean age 63.4 ± 13.6 years) versus conventional insulin treatment regimens (goal BG 180–200 mg/dL; mean age 62.2 ± 13.9 years), and of significance, results showed a reduction in mortality in the intensive arm (P < 0.04, absolute risk reduction [ARR] 3.7%) [41]. A subsequent study by the same research group evaluated patients in the medical ICU, with intensive versus conventional glycemic management (mean age in the intensive and mean age in the conventional arm were 63 ± 16 years and 64 ± 16 years respectively) and found intensive therapy reduced BG levels, but did not significantly reduce mortality [42]. Further studies of BG targets in critical illness includes the Normoglycaemia in Intensive Care Evaluation and Survival Using Glucose Algorithm Regulation (NICE-SUGAR) study, evaluating conventional versus intensive glucose control. The conventional arm had fewer deaths (27.5% versus 24.9%) and demonstrated decreased incidence of severe hypoglycemia [43]. Additionally, the role of insulin has been studied in severe sepsis in the Efficacy of Volume Substitution and Insulin Therapy in Severe Sepsis (VISEP) trial, where use of intensive insulin therapy was related to higher rates of severe hypoglycemia and adverse events compared with conventional insulin therapy [44].
Interestingly, these large randomized controlled trials in the ICU reported recruiting participants who were mainly older adults; mean age in NICE-SUGAR was 60.4 ± 17.2 years in the intensive and 59.5 ± 17.1 years in the conventional arm and mean age in VISEP was 64.6 ± 13.7 years for all subjects [43, 44]. Results from all the above studies are mixed and are likely attributable to a myriad of factors including differences in control group glycemic targets, differences in implementation methods, and differences in hypoglycemia rates. The impact of age is not fully clear from the data presented from these studies to date.
Targeting intermediate glucose levels is the current practice standard in critical illness. Consensus guidelines from critical care, thoracic surgeons, the American Association of Clinical Endocrinologists and American Diabetes Association recommend that in critically ill patients, a glucose level > 180 mg/dL triggers initiation of an IV infusion of insulin, with goal BG level between 140 and 180 mg/dL for most patients [43, 45, 46].
Non-critically Ill Patients
Subcutaneous insulin is the preferred agent for hyperglycemia management in non-critically ill hospitalized patients. Several insulin strategies exist, including basal insulin (BI) alone or in combination with prandial insulin (PI) [17]. Unlike the randomized controlled trials in the ICU setting, studies in the non-critically ill included a younger population; therefore, extrapolating the findings to older adults poses more of a challenge [41,42,43,44, 47, 48].
The RABBIT 2 trial evaluated the safety and efficacy of sliding-scale regular insulin (SSI) to a basal bolus insulin (BBI) regimen in patients with T2DM on a hospital medicine service [47]. Patients were treated with a regular SSI protocol four times daily (for BG > 140 mg/dL, mean age 56 ± 11 years) or BBI (glargine plus glulisine before meals, mean age 56 ± 13 years). Goal BG was achieved in 66% of patients in the BBI arm and 38% in the SSI group, with no difference in hypoglycemia rates [47]. A similar study, the RABBIT 2 surgery trial, was conducted in hospitalized surgical patients [48]. Mean age of participants was 58 ± 12 years and goal BG was reached in 55% of patients in the BBI group, compared with 31% in the SSI group (P < 0.001). Hypoglycemia was reported in 21.3% of patients in the BBI arm compared with 4.7% in the SSI group (P < 0.001); data was not reported by age [48].
These studies were conducted in middle-aged patients; however, the Basal Plus Trial provides guidance for hospitalized older adults with T2DM (61 [16%] of 375 participants ≥ 70 years) [49]. This study randomized patients to BBI (mean age 58.7 ± 11 years) versus basal regimen plus SSI for meals (mean age 58.6 ± 13 years) versus regular SSI alone (mean age 58.7 ± 12 years). Improvement was similar in the BBI and basal plus regimens, with no difference in hypoglycemia rates; both BBI and basal plus regimens were superior to regular SSI. For participants age ≥ 70 years, adjustments in insulin were made; weight-based insulin dosing was reduced from 0.25 to 0.15 units/kg/day in patients ≥ 70 years. The authors suggest the basal plus regimen for patients with reduced or inconsistent caloric intake (basal insulin 0.1–0.15 units/kg/day plus correction SSI) [49]. For older adults with adequate nutrition, a BBI regimen has been suggested (0.2–0.3 units/kg/day divided equally between BI and PI dosing) [17, 49, 50].
A retrospective observational study evaluated the efficacy of a BBI protocol in hospitalized adults aged ≥ 65 years (mean age 82 ± 7 years, BG target 90–200 mg/dL) [51•]. In frail adults (using the geriatric cumulative illness rating scale), total daily dose (TDD) insulin requirement was adjusted for hypoglycemia risk with a starting dose of 0.2–0.3 units/kg/day (versus 0.3–0.7 units/kg/day in the non-frail population). SSI regimens subtracted one unit of insulin from the scale if the pre-meal BG level was low (70–90 mg/dL). Furthermore, educational courses were provided to providers using this protocol. During the study period, mean BG improved (P < 0.005), mild hypoglycemia occurred in 9.1% patients (95% CI, 3–15.2%), and there were no severe hypoglycemia events. This study presents a guide for BBI protocols aimed at hypoglycemia reduction in frail older adults [51•].
Hypoglycemia in Hospitalized Older Adults
Guidelines for DM management in older adults anchor on individualized treatment plans and minimizing hypoglycemia [21, 22, 24••]. In a study of DM complication rates in older adults (cohort of 72,310 persons ≥ 60 years), hypoglycemia increases with age and duration of DM (in patients with DM duration ≥ 10 years, acute hypoglycemia occurred 9.62 per 1000 person-years in ages 60–69, 15.88 per 1000 person-years in ages 70–79, and 19.6 per 1000 person-years in persons over 80 years, P < 0.01) [16]. Several factors contribute to hypoglycemia in older adults, including comorbidities, cognitive impairment, frailty, polypharmacy, and variable nutritional status [52]. In the hospital, additional risks include acute illness, renal insufficiency, sepsis, low albumin, and impaired functional status [16, 53].
A study of older hospitalized adults (mean age 80.5 years, 42% with underlying DM) found hypoglycemia was associated with a 2× increase in in-hospital mortality (P < 0.001), as well as increased death at 3 and 6 months post discharge [52]. However, the increased mortality risk may not be related to hypoglycemia itself, rather a marker of severe illness [52, 54]. Hypoglycemia risk prediction models have been developed and validated for use in older hospitalized patients (mean age 76.08 ± 11.17) and may help guide DM management to avoid hypoglycemia in patients at risk [55].
Identifying hypoglycemia risk is imperative, but mitigation efforts are difficult to achieve; computerized insulin order sets and titration algorithms have been shown to decrease inpatient hypoglycemia and widespread use of these methods help decrease hypoglycemia rates in patients on insulin therapy [56, 57]. Further, Baldwin et al. recommend incorporating renal function into the traditional weight-based insulin dosing method to avoid hypoglycemia; initial insulin therapy for hospitalized patients with impaired renal function (estimated glomerular filtration rate [GFR] < 45 mL/min) is a TDD of 0.25 units/kg/day (compared with 0.5–0.6 units/kg/day for healthy adults), divided in half for basal insulin and the remainder divided equally for prandial insulin [58]. These recommendations should be considered, as mild elevation in creatinine in older adults may reflect a substantial decrease in GFR, and therefore these recommendations offer a helpful guide in mitigating hypoglycemia in hospitalized older adults [58].
Multidisciplinary Teams and Diabetes Education in Older Adults
Studies evaluating the role of a multidisciplinary team focusing on inpatient glycemic management, DM education, and discharge planning showed improved glycemic management at 1 year post discharge, with significant improvement in glycemic management in patients newly started on insulin (average HbA1c reduction 2.4%, P = 0.04) [59]. Formal inpatient DM education is also independently associated with lower frequency of all-cause hospital readmission within 30 days (11 versus 16%, P = 0.0001) [60].
Psychological insulin resistance is common and studies indicate that insulin-naïve older adults experience fear of self-monitoring of BG and insulin injections [61]. A study evaluated barriers to diabetes self-care in older adults (mean age 75 ± 5 years) in the outpatient setting over a 12-month period [62]. A multidisciplinary team developed individualized care plans with coping strategies, implemented by a DM educator between clinic visits. After the intervention period, HbA1c decreased by 0.45% in the intervention group compared with 0.31% in the control arm, with further improvement in HbA1c at 1 year for the intervention group only (additional 0.21% reduction, P < 0.03). The intervention group showed benefits in self-care, gait/balance, and endurance [62]. This study demonstrates positive outcomes and, if proven beneficial on a larger scale, may provide a framework for DM care in older adults.
Discharge Planning
Discharge planning should be individualized, using the admission HbA1c to help tailor DM treatment upon discharge [63]. Umpierrez et al. recommend the following framework for discharge DM therapy in older adults: admission HbA1c range < 7.5–8%, re-start home regimen (oral agents with insulin if necessary), HbA1c 8.0–10.0%, consider oral agents plus basal insulin (50% of hospital insulin dose), and for HbA1c > 10%, patients should be discharged on a BBI regimen or on a combination of pre-admission oral agents with approximately 80% of hospital BI dose [17]; this is modified from the treatment algorithm previously tested [63]. This is a useful framework; however, additional studies of discharge therapy in older adults are required to validate this recommendation.
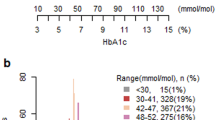
Another guide is consideration of health status of older adults with DM using a validated framework categorizing patients into increasing levels of mortality risk, for example, the Endocrine Society Guidelines suggest the following: a relatively healthy group, intermediate health group, and poor health group (based on chronic conditions, cognitive/visual impairment, and functional status) [64]. Using this framework, the Endocrinology Society Guidelines on older adults recommend the outpatient goal HbA1c levels for the healthy group, intermediate health group, and poor health group are between 7.0–7.5%, 7.5–8.0%, and 8.0–8.5% respectively [24••].
Comprehensive discharge plans for older adults often include a home health referral. Patients under Medicare coverage are eligible for home health if the patient is homebound and requires intermittent skilled nursing care, physical or occupational therapy, or speech-language pathology services [65]. The referral must indicate DM as a home-care concern in order for glucose monitoring and DM care to be included. Home health services are not applicable if a patient requires full-time or extended periods of skilled nursing care [65, 66].
Conclusion
Diabetes in older adults is a growing public health concern, with an unprecedented number of older adults with DM in the USA and worldwide. The management of older adults with DM requires treatment plans with consideration of the patients’ personal goals, life expectancy, comorbidities, functional status, and risk of hypoglycemia. More studies are needed to help integrate aspects of the CGA in the inpatient setting.
Guidelines for management of inpatient and outpatient care have been developed; however, it is important to recognize there are limited studies specific to either T2DM and/or hyperglycemia in older adults. Therefore, recommendations and treatment guidelines are in part extrapolated from studies in middle-aged patients. Currently, insulin therapy is the cornerstone of inpatient hyperglycemia management both in critical illness and non-critically ill hospitalized patients, with a specific aim of avoiding hypoglycemia. Future research should aim to account for the complexity of care for older adults, with a specific goal of assessing the effectiveness and safety of therapies in older adults with DM and evaluating differing glycemic targets by age and the relationship to subsequent comorbidities and safety outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021–9. https://doi.org/10.1001/jama.2015.10029.
Proposed working definition of an older person in Africa for the MDS Project In: Healt statistics and information systems. World Health Survey. World Health Organization 2002. https://www.who.int/healthinfo/survey/ageingdefnolder/en/ - .XLEMyTWR1fU.email. Accessed April 12th, 2019 2019.
Older People Projected to Outnumber Children for First Time in U.S. History. 2017 National Population Projections. United States Census Bureau U.S. Department of Commerce 2018. https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html. Accessed 03/18/2019 2019.
National Diabetes Statistics Report. Centers for Disease Control and Prevention. Atlanta: US Department of Health and Human Services; 2017. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 3/5/2019 2019
Falciglia M, Freyberg RW, Almenoff PL, D’Alessio DA, Render ML. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med. 2009;37(12):3001–9. https://doi.org/10.1097/CCM.0b013e3181b083f7.
Healthy People 2020. Clinical Preventive Services. . In: Poor glycemic control (D-5.1) 200 Independence Avenue, S.W., Washington, DC 20201. https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services/data - D-5.1. Accessed June 4th, 2019 2019.
Sleiman I, Morandi A, Sabatini T, Ranhoff A, Ricci A, Rozzini R, et al. Hyperglycemia as a predictor of in-hospital mortality in elderly patients without diabetes mellitus admitted to a sub-intensive care unit. J Am Geriatr Soc. 2008;56(6):1106–10. https://doi.org/10.1111/j.1532-5415.2008.01729.x.
Halter JB, Musi N, McFarland Horne F, Crandall JP, Goldberg A, Harkless L, et al. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578–89. https://doi.org/10.2337/db14-0020.
Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–46. https://doi.org/10.2337/dc12-2625.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978–82. https://doi.org/10.1210/jcem.87.3.8341.
Sinclair AJ, Abdelhafiz AH, Forbes A, Munshi M. Evidence-based diabetes care for older people with type 2 diabetes: a critical review. Diabet Med. 2018;36:399–413. https://doi.org/10.1111/dme.13859.
Lee PG, Halter JB. The pathophysiology of hyperglycemia in older adults: clinical considerations. Diabetes Care. 2017;40(4):444–52. https://doi.org/10.2337/dc16-1732.
McDonnell ME, Umpierrez GE. Insulin therapy for the management of hyperglycemia in hospitalized patients. Endocrinol Metab Clin N Am. 2012;41(1):175–201. https://doi.org/10.1016/j.ecl.2012.01.001.
Sinclair A, Dunning T, Rodriguez-Manas L. Diabetes in older people: new insights and remaining challenges. Lancet Diabetes Endocrinol. 2015;3(4):275–85. https://doi.org/10.1016/s2213-8587(14)70176-7.
Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014;174(2):251–8. https://doi.org/10.1001/jamainternmed.2013.12956.
Umpierrez GE, Pasquel FJ. Management of inpatient hyperglycemia and diabetes in older adults. Diabetes Care. 2017;40(4):509–17. https://doi.org/10.2337/dc16-0989.
Soe K, Sacerdote A, Karam J, Bahtiyar G. Management of type 2 diabetes mellitus in the elderly. Maturitas. 2011;70(2):151–9. https://doi.org/10.1016/j.maturitas.2011.07.006.
Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–12. https://doi.org/10.1056/NEJMsa1103053.
Lipska KJ, Ross JS, Wang Y, Inzucchi SE, Minges K, Karter AJ, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116–24. https://doi.org/10.1001/jamainternmed.2014.1824.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60(12):2342–56. https://doi.org/10.1111/jgs.12035.
Sinclair AJ, Abdelhafiz A, Dunning T, Izquierdo M, Rodriguez Manas L, Bourdel-Marchasson I, et al. An international position statement on the management of frailty in diabetes mellitus: summary of recommendations 2017. J Frailty Aging. 2018;7(1):10–20. https://doi.org/10.14283/jfa.2017.39.
Medicare Learning Network Booklet. Annual wellness visit. . In: Services USCfMaM, editor. Website. . 7500 Security Boulevard, Baltimore, MD 21244: American Medical Association 2018. p. 1–16.
•• Le Roith D, Biessels GJ, Braithwaite SS, Casanueva FF, Draznin B, Halter JB, et al. Treatment of diabetes in older adults: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1520–74. https://doi.org/10.1210/jc.2019-00198 The Endocrine Society 2019 clinical practice guidelines include the prevalence, pathophysiology, assessment, and management considerations in older adults with DM. These guidelines outline the approach to inpatient and outpatient therapy with special considerations for the aging adult population with DM.
12. Older adults: standards of medical care in diabetes-2019. Diabetes Care 2019;42(Suppl 1):S139-s47. https://doi.org/10.2337/dc19-S012.
Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics Society guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc. 2013;61(11):2020–6. https://doi.org/10.1111/jgs.12514.
Pilotto A, Cella A, Pilotto A, Daragjati J, Veronese N, Musacchio C, et al. Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J Am Med Dir Assoc. 2017;18(2):192.e1–e11. https://doi.org/10.1016/j.jamda.2016.11.004.
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:Cd006211. https://doi.org/10.1002/14651858.CD006211.pub3.
Munshi MN. Cognitive dysfunction in older adults with diabetes: what a clinician needs to know. Diabetes Care. 2017;40(4):461–7. https://doi.org/10.2337/dc16-1229.
Munshi MN, Slyne C, Segal AR, Saul N, Lyons C, Weinger K. Simplification of insulin regimen in older adults and risk of hypoglycemia. JAMA Intern Med. 2016;176(7):1023–5. https://doi.org/10.1001/jamainternmed.2016.2288.
• Van Craen K, Braes T, Wellens N, Denhaerynck K, Flamaing J, Moons P, et al. The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta-analysis. J Am Geriatr Soc. 2010;58(1):83–92. https://doi.org/10.1111/j.1532-5415.2009.02621.x In this meta-analysis of studies performed in a hospital ward focused on the care of older adults (GEMU), components of the CGA were employed with a team-based approach to develop an individualized care plan, including a focus on rehabilitation, discharge planning, and early post-hospital follow-up. This study found the GEMU approach effective in two distinct areas: less functional decline at discharge (relative risk [RR] = 0.87, P = 0.04) and a lower rate of institutionalization 1 year post discharge (RR = 0.78, P = 0.003).
Halter J, Ouslander JG, Studenski S, High KP, Asthana S, Supiano MA, et al. Hazzard’s geriatric medicine and gerontology, seventh edition chapter 16: Acute hospital care. New York, NY: McGraw-Hill; 2017.
Jover N, Traissac T, Pinganaud G, Moras JB, Rainfray M, Bourdel-Marchasson I. Varying insulin use in older hospitalized patients with diabetes. J Nutr Health Aging. 2009;13(5):456–9.
Aliberti MJR, Apolinario D, Suemoto CK, Melo JA, Fortes-Filho SQ, Saraiva MD, et al. Targeted geriatric assessment for fast-paced healthcare settings: development, validity, and reliability. J Am Geriatr Soc. 2018;66(4):748–54. https://doi.org/10.1111/jgs.15303.
Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451–4.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–31.
Patel A, Parikh R, Howell EH, Hsich E, Landers SH, Gorodeski EZ. Mini-cog performance: novel marker of post discharge risk among patients hospitalized for heart failure. Circ Heart Fail. 2015;8(1):8–16. https://doi.org/10.1161/circheartfailure.114.001438.
Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med. 2008;6(3):246–52. https://doi.org/10.1370/afm.842.
14. Diabetes care in the hospital: standards of medical care in diabetes-2018. Diabetes care. 2018;41(Suppl 1):S144-s51. https://doi.org/10.2337/dc18-S014.
15. Diabetes care in the hospital: standards of medical care in diabetes-2019. Diabetes care. 2019;42(Suppl 1):S173-s81. https://doi.org/10.2337/dc19-S015.
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–67. https://doi.org/10.1056/NEJMoa011300.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–61. https://doi.org/10.1056/NEJMoa052521.
Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–97. https://doi.org/10.1056/NEJMoa0810625.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–39. https://doi.org/10.1056/NEJMoa070716.
Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite SS, Deutschman C, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40(12):3251–76. https://doi.org/10.1097/CCM.0b013e3182653269.
Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract. 2009;15(4):353–69. https://doi.org/10.4158/ep09102.Ra.
Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial). Diabetes Care. 2007;30(9):2181–6. https://doi.org/10.2337/dc07-0295.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care. 2011;34(2):256–61. https://doi.org/10.2337/dc10-1407.
Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169–74. https://doi.org/10.2337/dc12-1988.
Lansang MC, Umpierrez GE. Inpatient hyperglycemia management: a practical review for primary medical and surgical teams. Cleve Clin J Med. 2016;83(5 Suppl 1):S34–43. https://doi.org/10.3949/ccjm.83.s1.06.
• Franchin A, Maran A, Bruttomesso D, Corradin ML, Rossi F, Zanatta F, et al. The GesTIO protocol experience: safety of a standardized order set for subcutaneous insulin regimen in elderly hospitalized patients. Aging Clin Exp Res. 2017;29(6):1087–93. https://doi.org/10.1007/s40520-017-0728-5 This retrospective, observational study of older hospitalized adults with T2DM evaluated the safety, efficacy, and benefit of a standard order protocol for SQ insulin therapy in the hospital. In frail adults (mean age 82 ± 7), total daily (TDD) insulin requirement was adjusted (decreased) to avoid hypoglycemia; 9.1% experienced mild hypoglycemia, no severe hypoglycemia was reported, and mean blood glucose improved (P < 0.005).
Kagansky N, Levy S, Rimon E, Cojocaru L, Fridman A, Ozer Z, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003;163(15):1825–9. https://doi.org/10.1001/archinte.163.15.1825.
Lee AK, Lee CJ, Huang ES, Sharrett AR, Coresh J, Selvin E. Risk factors for severe hypoglycemia in Black and White adults with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care. 2017;40(12):1661–7. https://doi.org/10.2337/dc17-0819.
Boucai L, Southern WN, Zonszein J. Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med. 2011;124(11):1028–35. https://doi.org/10.1016/j.amjmed.2011.07.011.
Ena J, Gaviria AZ, Romero-Sanchez M, Carretero-Gomez J, Carrasco-Sanchez FJ, Segura-Heras JV, et al. Derivation and validation model for hospital hypoglycemia. Eur J Intern Med. 2018;47:43–8. https://doi.org/10.1016/j.ejim.2017.08.024.
Sinha Gregory N, Seley JJ, Gerber LM, Tang C, Brillon D. Decreased rates of hypoglycemia following implementation of a comprehensive computerized insulin order set and titration algorithm in the inpatient setting. Hosp Pract (1995). 2016;44(5):260–5. https://doi.org/10.1080/21548331.2016.1250603.
Sinha Gregory N, Seley JJ, Ukena J, Shah S, Fred MR, Dargar SK, et al. Decreased rates of inpatient hypoglycemia following implementation of an automated tool in the electronic medical record for identifying root causes. J Diabetes Sci Technol. 2018;12(1):63–8. https://doi.org/10.1177/1932296817744808.
Baldwin D, Apel J. Management of hyperglycemia in hospitalized patients with renal insufficiency or steroid-induced diabetes. Curr Diab Rep. 2013;13(1):114–20. https://doi.org/10.1007/s11892-012-0339-7.
Wexler DJ, Beauharnais CC, Regan S, Nathan DM, Cagliero E, Larkin ME. Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. Diabetes Res Clin Pract. 2012;98(2):249–56. https://doi.org/10.1016/j.diabres.2012.09.016.
Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36(10):2960–7. https://doi.org/10.2337/dc13-0108.
Bahrmann A, Abel A, Zeyfang A, Petrak F, Kubiak T, Hummel J, et al. Psychological insulin resistance in geriatric patients with diabetes mellitus. Patient Educ Couns. 2014;94(3):417–22. https://doi.org/10.1016/j.pec.2013.11.010.
Munshi MN, Segal AR, Suhl E, Ryan C, Sternthal A, Giusti J, et al. Assessment of barriers to improve diabetes management in older adults: a randomized controlled study. Diabetes Care. 2013;36(3):543–9. https://doi.org/10.2337/dc12-1303.
Umpierrez GE, Reyes D, Smiley D, Hermayer K, Khan A, Olson DE, et al. Hospital discharge algorithm based on admission HbA1c for the management of patients with type 2 diabetes. Diabetes Care. 2014;37(11):2934–9. https://doi.org/10.2337/dc14-0479.
Blaum C, Cigolle CT, Boyd C, Wolff JL, Tian Z, Langa KM, et al. Clinical complexity in middle-aged and older adults with diabetes: the Health and Retirement Study. Med Care. 2010;48(4):327–34.
Medicare and home health care In: Services USDoHaH, editor. 7500 Security Blvd., Baltimore, MD 21244–1850: Centers for Medicare and Medicais Services 2017. p. 1–32.
Linekin PL. Home health care and diabetes assessment, care, and education. Diabetes Spectr. 2003;16(4):217–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kristen DeCarlo declares no conflict of interest. Amisha Wallia receives grants from Novo Nordisk and serves as research investigator for studies for United Health Group and Eli Lilly.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hospital Management of Diabetes
Rights and permissions
About this article
Cite this article
DeCarlo, K., Wallia, A. Inpatient Management of T2DM and Hyperglycemia in Older Adults. Curr Diab Rep 19, 104 (2019). https://doi.org/10.1007/s11892-019-1209-3
Published:
DOI: https://doi.org/10.1007/s11892-019-1209-3