Abstract
Purpose of Review
Children and adolescents with acute hyperglycemia and diabetes mellitus frequently have acute, potentially life-threatening presentations which require high-acuity care in an inpatient and often intensive care setting. This review discusses the evaluation and care of hyperglycemia and diabetes mellitus in hospitalized children in both critical and non-critical care settings, highlighting important differences in their care relative to adults.
Recent Findings
Diabetic ketoacidosis remains highly prevalent at diagnosis among children with type 1 diabetes, and hyperglycemic hyperosmolar state is increasingly prevalent among children with type 2 diabetes. Recent clinical trials have investigated the potential benefits of various types of intravenous fluids and their rates of administration as well as the risks and benefits of intensive glucose control in critically ill children. The Endocrine Society has developed guidelines focused on managing hyperglycemic hyperosmolar state, outlining important aspects of care shown to decrease morbidity and mortality. In the non-critical illness setting, intensive therapy on newly diagnosed diabetes is increasingly recommended at the outset.
Summary
With the increasing incidence of diabetes mellitus in children and adolescents, recent studies addressing acute diabetes emergencies help inform best practices for care of hospitalized children with hyperglycemia and diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes in the pediatric population continues to increase in the USA and worldwide [1,2,3]. Type 1 diabetes results from autoimmune destruction of the insulin-producing beta cells with progressive insulinopenia and hyperglycemia, while type 2 diabetes is most commonly caused by a combination of genetic predisposition, obesity, and progression from insulin resistance to beta cell failure and relative insulinopenia. Additional forms of diabetes, including MODY (maturity-onset diabetes of youth), mitochondrial diabetes, neonatal diabetes, and medication-induced diabetes, are less common but important diagnostic considerations for children presenting with specific signs and symptoms in the proper clinical context [4].
There are important diagnostic and treatment considerations which are unique to the pediatric population. In this review, we will focus on the evaluation and management of children hospitalized for the acute care of hyperglycemia, diabetic emergencies, and newly diagnosed diabetes mellitus, highlighting relevant key differences between pediatric and adult care.
Diabetes and Hyperglycemia in the Critical Care Setting
Diabetic Ketoacidosis
Definition
Diabetic ketoacidosis (DKA) is one of the most common complications of type 1 diabetes. It is defined as hyperglycemia (blood glucose > 200 mg/dL) with a serum pH < 7.3 and/or serum bicarbonate level < 15 mmol/L [5]. The blood glucose level is nearly universally elevated at presentation in children with new-onset diabetes, while those with pre-existing diabetes may be euglycemic or even hypoglycemic if insulin was administered by the child or family prior to hospital arrival.
Incidence
In the USA, approximately 30% of children with new-onset type 1 diabetes will present in DKA, a statistic which has remained largely unchanged over the last decade [6]. Globally, the incidence of DKA at initial diagnosis of diabetes varies from 15 to 80%, with higher incidence rates reported in areas with less available medical resources and lower overall incidence of diabetes [7, 8].
Risk Factors
Among children, risk factors for DKA at initial diagnosis include very young age and non-private or no insurance coverage [9, 10]. Children under age 4 years may have a delayed diagnosis due to their limited ability to express various symptoms, difficulty of caregivers in detecting polyuria in children not yet toilet trained, and the assumption that behavior changes such as excessive drinking, irritability, and poor appetite may simply be part of age-appropriate developmental changes.
In children with an established diagnosis of diabetes, particularly adolescents, missed doses of insulin are the major risk factor for developing recurring episodes of DKA. Contrary to earlier studies suggesting insulin pump use increases the risk of DKA, more recent evidence argues that this risk may actually be lower in children using insulin pump therapy compared with those utilizing subcutaneous injections [11]. It is critical that children and their families be aware of this risk with insulin omission, while simultaneously addressing any contributory mental health or psychosocial factors.
Specific Considerations for Children with DKA
There are several important considerations in management of DKA in children. In younger pre-verbal children, it is difficult to obtain specific symptoms such as headaches, limiting the ability to detect complications. Children also have higher basal metabolic rates and a large surface area relative to total body mass compared with adults. Consequently, greater precision is needed in supplementing fluids and electrolytes. Finally, younger children may not have fully developed cerebral and other autoregulatory mechanisms, leading to greater risk of cerebral edema [12].
Initial Assessment and Intervention
DKA should be managed in an inpatient unit with an experienced pediatrician and nursing staff. The unit should have clear written guidelines for DKA management, as well as access to a laboratory capable of frequent and rapid biochemical evaluation. Management in an intensive care unit is recommended for children with signs of severe DKA such as altered consciousness and circulatory compromise. Initial evaluation should include assessment of airway, breathing, circulatory status, and level of consciousness per Pediatric Advanced Life Support (PALS) guidelines. Ongoing monitoring of children with DKA should include hourly monitoring of vital signs, fluid intake/output, capillary blood glucose, and neurological status. Electrolytes, urea, hematocrit, blood glucose, and blood gases should be measured every 2–4 h [13, 14].
Intravenous Fluid Management
Current guidelines for DKA management recommend initial resuscitation with isotonic fluid boluses of 10–20 mL/kg. There are no recommendations favoring any specific intravenous fluid solution or rate of fluid administration for subsequent hydration. A randomized clinical trial by Kupperman and colleagues compared the use of 0.45% to 0.9% normal saline in children treated for DKA and found no significant difference in the rate of mental status decline or rate of clinically apparent brain injury among patients treated with the various fluid regimens. There was also no significant difference in neurocognitive function after recovery from DKA [15•]. Other studies have similarly found no difference in neurological impairment between children on isotonic versus more hypotonic fluids [16]. It has been suggested that administering isotonic fluids at 2–2.5 times above maintenance requirements may result in decreased rates of morbidity and mortality from cerebral edema [17]. However, isotonic fluid administration has also been reported to be associated with the development of hyperchloremic acidosis, which may result in longer duration of hospitalization [18], although this association has not been corroborated by other studies [19]. At the present time, the recommendation is therefore to continue subsequent hydration with isotonic solutions, or at least a solution with tonicity ≥ 0.45% normal saline, with the fluid rate calculated to rehydrate evenly over 24–48 h.
Insulin Administration
While intravenous fluids improve hyperglycemia by improving the glomerular filtration rate, insulin administration is required for normalization of blood glucose levels and resolution of ketoacidosis. Current guidelines recommend the use of regular insulin infused intravenously at a rate of 0.1 U/kg/h [13, 14]. There is data to suggest that low-dose insulin infusion (0.05 units/kg/h) may be equally effective in achieving normoglycemia and resolution of ketoacidosis [20, 21]. Insulin bolus has not been shown to be necessary in improving blood glucose levels or ketoacidosis [22, 23]. Subcutaneous insulin regimens have been shown to be effective in managing DKA, although this method may result in longer time to resolution of acidosis [24, 25].
Cerebral Edema
Cerebral edema is the main cause of morbidity and mortality, accounting for 60–90% of all deaths in children with DKA. The incidence of clinically apparent cerebral edema in the USA is 0.5–0.9%, with a mortality rate of 21–24%. Cerebral edema may also be clinically asymptomatic and only evident radiographically [14, 26]. Signs and symptoms of cerebral edema include headache, gradual decline in level of consciousness, hypertension, and bradycardia. Cerebral edema is often initially clinically noted 4–12 h after treatment of DKA is initiated but may occur at any time during an episode of DKA [13, 14].
The pathophysiology of cerebral edema is not completely understood. Rapid fluid administration causing abrupt changes in serum osmolality has been a proposed mechanism [13]. More recent data suggests that vasogenic edema, rather than osmotic cell swelling, may play a role [26]. Risk factors associated with development of cerebral edema include more severe hypocapnia, higher serum urea nitrogen at presentation of DKA, smaller increases in serum sodium concentration during therapy, and treatment with bicarbonate [27]. Although a more recent study did not find an association between the rate of fluid administration and increased risk of cerebral edema [28•], this point remains an important debate among clinicians caring for these children.
Cerebral edema should be treated as soon as it is suspected. The rate of fluid administration should be reduced by one-third. Mannitol should be administered at a dose of 0.25–1 g/kg over 20 min. Hypertonic (3%) saline is an alternative to mannitol and can be given at a dose of 5–10 mL/kg over 30 min [13]. Use of hypertonic saline has increased in recent years, although some reports suggest an increase in mortality when compared with mannitol alone [29]. Intubation may be necessary for patients with impending respiratory failure, although intubation with hyperventilation has been shown to be associated with poor outcome [30].
Hyperglycemic Hyperosmolar State
Definition
Hyperglycemic hyperosmolar state (HHS) is defined as blood glucose > 600 mg/dL with serum osmolality > 330 mOsm/kg and the absence of significant ketosis and acidosis (serum bicarbonate > 15 mEq/L and/or urine ketone concentration < 15 mg/dL [14].
Incidence
HHS was historically recognized as an entity largely confined to adults with diabetes, although it is becoming more prevalent in pediatric patients. Between 1997 and 2009, the population rate for HHS hospitalizations in children increased by 52.4% [31].
Risk Factors
The main risk factor for HHS is obesity and type 2 diabetes. Children treated with atypical antipsychotics have also been reported to be at increased risk of developing HHS [32].
Specific Considerations for Children with HHS
Unlike adults, pediatric patients may present with no identifiable precipitating factor [33]. Children with HHS also have a greater degree of dehydration than those in DKA, although the signs and symptoms of dehydration may be less clinically evident [34••]. Some children may present with a mixed picture of DKA and HSS, making management more challenging [35]. The potential complications of HHS are also distinct from those in DKA and include increased risk of thromboembolism, rhabdomyolysis, and a malignant hyperthermia-like syndrome [34••].
Initial Assessment and Intervention
The gradual nature of the worsening polyuria and polydipsia in HSS can be subtle, resulting in more severe dehydration and electrolyte imbalances due to delayed presentation [14]. HHS in children is most commonly reported in the adolescent population. Due to the severe degree of dehydration and profound hyperglycemia, adolescents often present with altered mental status and irritability, and may initially be suspected of being under the influence of illicit drugs or alcohol. The initial degree of glucose elevation may be extreme and difficult to accurately measure in capillary venous samples, delaying the diagnosis further even once they are in the acute care setting.
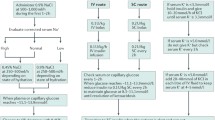
Intravenous Fluid Management
Given the severe degree of dehydration in patients with HHS, aggressive fluid replacement, rather than insulin administration, is the cornerstone of therapy. Patients with HHS who receive early and more aggressive fluid resuscitation have been shown to have better rates of survival [36]. Multiple fluid boluses should be administered, with fluid deficit of 12–15% of body weight assumed for subsequent fluid replacement calculations. Clinicians should be aware that these adolescents may require as much as 10–15 L of IV fluids in the first 24 h to prevent renal failure and intravascular fluid depletion, particularly as the hyperglycemia begins to improve. Isotonic fluids are recommended initially despite the possibility of raising serum sodium concentration, as they are more effective in maintaining intravascular volume. Subsequently, 0.45–0.75% normal saline solution should be given to replace fluid deficit over the subsequent 48–72 h. Urinary fluid losses should be replaced with 0.45% normal saline [14, 34••].
Insulin Administration
Unlike in DKA, early insulin administration is not necessary in HHS as there is minimal ketosis. Premature administration of insulin may result in circulatory compromise by decreasing serum glucose levels, which contribute to maintaining intravascular volume. Insulin therapy should be considered once serum glucose levels are decreasing by less than 50 mg/dL/h with intravenous fluids alone and after aggressive fluid hydration has been provided. If acidosis and ketosis are present, insulin administration can be started earlier. Current guidelines recommend starting insulin infusion at a dose of 0.025 to 0.05 units/kg/h, with the goal of decreasing serum glucose concentrations by no more than 50 to 75 mg/dL/h [14, 34••].
Correction of Electrolyte Imbalances
Children with HHS can have more significant depletion of total body potassium, phosphate, and magnesium than that seen in DKA. Potassium replacement should be started at a rate of 40 mEq/L as soon as potassium levels are normal in patients with adequate renal function. Increased rates may be needed after insulin therapy is initiated. Phosphorous replacement should be administered with a 50:50 mixture of potassium phosphate and either potassium chloride or potassium acetate [14]. Magnesium replacement should be considered in patients with hypocalcemia and hypomagnesemia at a recommended dose of 25–50 mg/kg/dose for 3 to 4 doses every 4 to 6 h (maximum dose of 2 g/h) [34••].
Evaluation for Additional Comorbidities
HHS in children predisposes to a high risk of dural venous sinus thrombosis, so a low threshold should be used for obtaining neuroimaging in a child with excessive irritability or somnolence. The high risk of thrombosis should preclude placement of central venous catheters unless absolutely clinically necessary. There is no data to support the use of prophylactic low-dose heparin in children with HHS [14]. Serum measurement of CPK levels and urinalysis is recommended given the increased risk of rhabdomyolysis [34••]. A malignant hyperthermia-like syndrome has also been reported. Children with fever and increasing creatine kinase levels should accordingly be treated promptly with dantrolene [37]. Hypovolemic shock and acute renal failure in HHS must be treated aggressively to mitigate the high risk of multi-system organ failure and death [34••].
Table 1 summarizes the main diagnostic test results and initial therapeutic consideration in pediatric DKA and HHS.
Hyperglycemia During Critical Illness
Stress hyperglycemia is a well-described entity in both inpatient and outpatient settings, and critical illness can predispose to hyperglycemia even among children without a diagnosis of diabetes mellitus [38]. Hyperglycemia in acutely ill children in pediatric intensive care, particularly at increasingly higher glucose levels, has been associated with increased length of stay and increased mortality [39,40,41]. In light of this association, a number of trials have been conducted to assess the potential benefits of tight glycemic management in critically ill children and have found conflicting results. Vlasselaers and colleagues conducted a prospective, randomized controlled study of 700 critically ill infants and children, the majority of whom underwent cardiac surgery for congenital heart disease, to assess the effect of intensive glucose management on clinical outcomes [42]. The intensive glucose management groups achieved mean glucose levels of 94 mg/dL in infants under age 1 year and 113 mg/dL in children over age 1 year, while the conventionally treated glucose management groups achieved mean glucose levels of 128 mg/dL in infants and 158 mg/dL in children. The authors of the study reported significantly lower rates of mortality, decreased length of stay, and greater attenuation of inflammatory responses in the intensively treated arm compared with the conventionally treated arm.
Additional prospective studies of intensive glycemic management in pediatric critical illness, summarized in Table 2, have failed to show similar benefits while universally noting significantly higher rates of severe hypoglycemia in the intensive glucose control groups [43,44,45]. Based on the available data, including a recent meta-analysis by Chen et al. [46], current clinical practice should advocate for modest rather than intensive glycemic management in critically ill children.
Diabetes and Hyperglycemia in the Non-critical Care Setting
New-Onset Diabetes
Diagnosis
Most children with new-onset type 1 diabetes will present with the classical symptoms of polyuria, polydipsia, and weight loss, frequently in a state of DKA. Children with new-onset type 2 diabetes, unlike adults, often rapidly deteriorate from a state of obesity and insulin resistance to frank symptomatic hyperglycemia. Given the rapid rise in obesity among children and adolescents in the USA, the presence of obesity and acanthosis nigricans are inadequate to differentiate between a diagnosis of type 1 and type 2 diabetes. In fact, 5–10% of children and adolescents diagnosed with either type 1 or type 2 diabetes based on phenotypic characteristics may be misclassified and potentially improperly treated [47, 48]. Therefore, all children newly diagnosed with diabetes mellitus should have testing for serum autoantibody markers of type 1 diabetes.
Management of the Hospitalized Child with Newly Diagnosed Type 1 Diabetes
Perhaps the biggest limitation in inpatient diabetes management among children with diabetes is the lack of adequate guidelines to direct care, particularly if the child is not in DKA at initial presentation. The American Diabetes Association (ADA) Position statement on Diabetes in Children and Adolescents [49] notes that “children are not just little adults”, and yet most guidelines and recommendations are based on a combination of adult guidelines and expert opinion.
There are potential challenges to managing new-onset diabetes in children in the inpatient setting. Our institution carries insulin pens on formulary and allows patients to use their own non-formulary insulin pens; however, not all institutions do so. Consequently, patients may undergo diabetes education with devices other than the specific ones they will ultimately utilize after discharge. Additionally, insulin delivery in a hospital setting may be cumbersome and require multiple personnel to be involved (i.e., two-nurse medication check, physician entry of insulin order, pharmacy confirmation, and delivery of insulin pen), delaying the time to insulin administration at mealtimes. Importantly, a hospital admission increases the cost of care relative to in-office management. Despite these limitations, at our institution, we routinely hospitalize all children with newly diagnosed insulin-dependent diabetes due to our observation that the inpatient environment provides continuous observation by the clinical staff, increased opportunity for education throughout the day, and access to medical, nursing, nutrition, and social work services simultaneously.
The primary goal of inpatient management of new-onset diabetes in children is providing education for the patient (if developmentally appropriate), parents, and other caregivers. Diabetes education should be provided by trained professionals such as a diabetes educator, although frequently education is delivered by less experienced bedside nurses [49, 68]. In addition to diabetes self-management education, medical nutrition therapy and psychological support should be provided at diagnosis [50]. The ADA recommends that DSMES (diabetes self-management education and support) curriculum including the American Association of Diabetes Educators AADE7 Self Care Behaviors (healthy eating, physical activity, medication, preventing/detecting/treating acute and chronic complications, monitoring blood glucose levels, problem solving, and healthy coping with psychosocial issues and concerns) be delivered to patients and/or care partners. While these guidelines are not pediatric specific, as no set curriculum has been established for pediatrics, they have translated into a basis for diabetes education in all populations [51]. All education should be individualized, developmentally appropriate, and culturally sensitive. Prior to discharge, the patient (if appropriate) and caregivers must demonstrate ability to check blood glucose levels, count carbohydrates, and administer insulin [49]. Importantly, a plan must be created for school re-entry with diabetes.
In light of the long-term benefits of intensive insulin therapy demonstrated by the DCCT (Diabetes Control and Complications Trial) [52••], there has been a significant rise in the use of more intensive multi-dose insulin (MDI) regimens compared with older regimens using once or twice daily insulin therapy. A multi-center trial from Germany and Austria found that the rate of children treated with MDI therapy increased from 61% in 1995 to 78.1% in 2003 [53]. In the USA, it is now considered standard of care to start all children on MDI regimens as a variety of long-acting basal insulins and rapid-acting insulin analogs are FDA approved above 1 year of age. It is recommended to utilize long-acting basal and rapid-acting insulin analogs versus NPH, regular human, and pre-mixed insulins in order to best mimic physiologic insulin release and minimize hypoglycemia [54].
To determine insulin dosing for MDI, it is recommended to start with a weight-based dose ranging from 0.5 to 1 unit/kg/day. Increased insulin requirements are frequently needed for pubertal children, illness, and immediately following an episode of ketoacidosis. The average starting insulin dose for the pre-pubertal child is 0.5 units/kg/day with 50% of the daily dose allotted for basal insulin and 50% insulin for meals. To determine the insulin doses given for mealtime coverage (carbohydrate ratio) and correction of hyperglycemia (correction factor), the total daily insulin dose is divided into fixed numeric values of 500 and 1800, respectively [54]. In contrast to historically modest targets, contemporary recommendations advocate for tight glucose targets in children with type 1 diabetes (T1DM) based on studies demonstrating the ability to accomplish this goal without excessive and severe hypoglycemia (largely due to improved technology including use of continuous glucose monitors and insulin pumps). Blood glucose targets for children with T1DM should be set at 90–130 mg/dL prior to meals and 90–150 mg/dL prior to bedtime, with an overall Hba1c goal of < 7.5% and in some cases < 7% [50].
Management of the Hospitalized Child with Newly Diagnosed Type 2 Diabetes
The ADA recommends that metformin therapy be initiated for all newly diagnosed children with type 2 diabetes (T2DM), with the addition of insulin therapy in those with significant hyperglycemia and if the hemoglobin a1c is greater than 8.5% [50]. Children with T2DM treated with metformin monotherapy have been shown to have a high rate of early treatment failure [55•]. Unlike in adults with T2DM, there are no additional oral agents FDA approved for pediatric use. We therefore advocate for a more aggressive approach involving early insulin therapy in this population. Glucagon-like peptide 1 (GLP-1) agonists, only very recently approved for pediatric use in type 2 diabetes, now provide an additional pharmacologic option in this population.
In our institution, all children with newly diagnosed T2DM requiring initiation of insulin therapy are admitted for education and assessment of insulin requirements. Insulin therapy for children with T2DM can involve both basal and bolus insulin therapy, with both often required during the initial hospital stay. Children with T2DM are often obese and pubertal; both conditions render them more insulin resistant. Therefore, they may require up to 2 units/kg/day of insulin, and this calculation should be done initially based on 90% of ideal body weight.
The newly diagnosed child with T2DM similarly requires comprehensive diabetes education with a large emphasis on nutrition, weight management, and physical activity. Children with T2DM should be screened for complications and comorbidities at diagnosis including hypertension, retinopathy, nephropathy, neuropathy, non-alcoholic fatty liver disease (NAFLD), polycystic ovarian syndrome (PCOS), and dyslipidemia [50]. Since most hospitalized adolescents with newly diagnosed T2DM will require insulin therapy, self-monitoring of blood glucose (SMBG) recommendations are similar to children with T1DM.
Special Considerations for Insulin Dosing in Children
The International Society for Pediatric and Adolescent Diabetes (ISPAD) 2018 Clinical Practice Consensus Guidelines recommend that insulin be delivered pre-meal whenever possible. In the pediatric population, there are circumstances in which it is appropriate to dose post-meal or split prandial doses to 50% pre-meal and 50% post-meal. For example, infants and toddlers are not reliable in completing a meal and are unable to verbalize hypoglycemia symptoms. Additionally, particularly after initial diagnosis and during the adjustment period, children may become defiant and upset and refuse to eat after receiving an injection of insulin at mealtime, predisposing them to risk of hypoglycemia if insulin has been dosed pre-prandially without adequate carbohydrate consumption. Interestingly, a study by Phelan et al. found that with education regarding barriers, structured meal times, and limiting snacking, even young children were able to receive insulin pre-meals. In this study, even with large inaccuracies in the mealtime dose, hypoglycemia typically did not occur immediately [56]. In our institution, we teach pre-meal dosing for all children whenever possible but recognize that in those under age 5 years, post meal dosing may be needed. In the latter case, we typically recommend that the mealtime dose be given no more than 20 min following initiation of the meal.
Care of Children with Diabetes Requiring Surgery
The ISPAD recommends refining diabetes management prior to surgery to improve surgical outcomes and decrease the risk for post-operative infection. The ISPAD recommends blood glucose levels be maintained between 90 and 200 mg/dL intraoperatively and 140–200 mg/dL in the post-surgical setting [57]. It is recommended that children be the first case performed, if possible, to minimize the length the child is NPO. Regardless of the duration of the procedure, an IV should be placed in order to treat hypoglycemia intra- or post-operatively. If the patient’s blood glucose level is > 250 mg/dL, urine or blood ketones should be measured. During the procedure, blood glucose levels should be checked every 30 min. For children who utilize a continuous glucose monitoring system (CGMS), there have been no RCTs performed to determine the safety of the system during surgical procedures [57]. In our institution, children have, on occasion, worn CGMSs for minor/short procedures (e.g., endoscopy, colonoscopy). Nonetheless, hourly fingerstick blood glucose monitoring remains the standard of care during surgery, with adjustment of dextrose or insulin delivery based on fingerstick blood glucose values given the lack of consensus on use of sensor data during surgery.
It is imperative that insulin therapy not be discontinued due to risk of ketosis. Basal insulin should be given as scheduled the night prior, although a dose adjustment might be needed. For children who wear insulin pumps, if the medical team is comfortable managing the insulin pump, it can be worn for procedures that are less than 2 h in length [57]. Similar to adults, children on metformin should have their renal function assessed at admission and hydration status monitored given the increased risk of lactic acidosis [58]. Metformin administration should be held just prior to surgical procedures and contrast-requiring imaging studies and not restarted until 48 h post-procedure and when normal renal function has been confirmed [57].
Use of Insulin Pumps and Continuous Glucose Monitoring Systems in Inpatient Settings
In the pediatric population, there are no formal recommendations for the use of CGMS in the hospital setting [59]. In our institution, hospitalized children continue to wear their CGMS device, although insulin dosing is still based on fingerstick glucose measurements using the hospital point of care blood glucose meter.
For patients with pre-existing diabetes wearing an insulin pump, the ADA and AACE (American Association of Clinical Endocrinologists) recommend continuing insulin pumps if the patient/care partner is physically and mentally capable of managing the insulin pump and if there is a hospital policy in place regarding safe insulin pump use [60]. All insulin pumps should be removed prior to MRI, CT, or X-ray [61,62,63]. In the event that the imaging study duration is greater than 2 h, a subcutaneous insulin bolus may be given for an elevated glucose level.
Management of Medication-Induced Hyperglycemia in Hospitalized Children
The most common cause of medication-induced hyperglycemia in hospitalized children is synthetic steroid therapy for rheumatologic conditions, malignancies, or post solid organ transplantation [64]. Once or twice daily administration of the synthetic steroids prednisone or prednisolone has been shown to result in a pattern of hyperglycemia predominantly manifesting in the early afternoon and late evening and not overnight [65, 66]. While there are no randomized prospective trials in pediatrics comparing prandial, basal, or combined basal-bolus insulin therapy for steroid-induced hyperglycemia, the lack of overnight hyperglycemia in this population suggests that prandial insulin dosing may be more physiologic and predispose to less risk of overnight hypoglycemia. In adult studies, there appears to be no significant difference between various basal insulin regimens, when used, in terms of glucose management or risk of hypoglycemia [67]. Future studies are needed to elucidate the potential risks and benefits of insulin therapy in this population of children.
Conclusion
Children and adolescents with diabetes mellitus and hyperglycemia will frequently require in-hospital management, both at initial diagnosis of diabetes and for subsequent care. Understanding the various aspects of diabetes and hyperglycemia which are unique to the pediatric population is critical in undertaking the most appropriate approach to diagnosis and management. As in all areas of pediatric care, additional randomized clinical trials are needed to better address the aspects of care which to date have largely been informed from trials in adults.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
CDC: www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;376:1419–29. https://doi.org/10.1056/NEJMoa1610187.
Dabelea D. The accelerating epidemic of childhood diabetes. Lancet. 2009;373(9680):1999–2000. https://doi.org/10.1016/S0140-6736(09)60874-6.
American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019;42(Suppl. 1):S13–28. https://doi.org/10.2337/dc19-s002.
Raghupathy R. Diabetic ketoacidosis in children and adolescents. Indian J Endocrinol Metab. 2015;19(Suppl1):S55–7. https://doi.org/10.4103/2230-8210.155403.
Dabelea D, Rewers A, Stafford JM, Standiford DA, Lawrence JM, Saydah S, et al. SEARCH for Diabetes in Youth Study Group. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics. 2014;133(4):e938–45. https://doi.org/10.1542/peds.2013-2795.
Rewers A, Klingensmith G, Davis C, Petitti DB, Pihoker C, Rodriguez B, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics. 2008;121(5):e1258–66. https://doi.org/10.1542/peds.2007-1105.
Grobe J, Hornstein H, Manuwald U, Kugler J, Glauche I, Rothe U. Incidence of diabetic ketoacidosis of new-onset type 1 diabetes in children and adolescents in different countries correlates with human development index (HDI): an updated systematic review, meta-analysis, and meta-regression. Horm Metab Res. 2018;50(3):209–22. https://doi.org/10.1055/s-0044-102090.
Mallare JT, Cordice CC, Ryan BA, Carey DE, Kreitzer PM, Frank GR. Identifying risk factors for the development of diabetic ketoacidosis in new onset type 1 diabetes mellitus. Clin Pediatr (Phila). 2003;42(7):591–7. https://doi.org/10.1177/000992280304200704.
Bui H, To T, Stein R, Fung K, Daneman D. Is diabetic ketoacidosis at disease onset a result of missed diagnosis? J Pediatr. 2010 Mar;156(3):472–7. https://doi.org/10.1016/j.peds.2009.10.001.
Karges B, Schwandt A, Heidtmann B, Kordonouri O, Binder E, Schierloh U, et al. Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA. 2017;318(14):1358–66. https://doi.org/10.1001/jama.2017.13994.
Wolfsdorf JI. Diabetic ketoacidosis in infants, children, and adolescents. Diabetes Care. 2006;29(5):1150–9.
Dunger DB, Sperling MA, Acerini CL, Bohn DJ, Daneman D, Danne TP, et al. European Society for Paediatric Endocrinology/Lawson Wilkins Pediatric Endocrine Society consensus statement of diabetic ketoacidosis in children and adolescents. Pediatrics. 2004;113(2):e133–8.
Wolfsdorf JI, Allgrove J, Craig ME, Edge J, Glasser N, Jain V, et al. ISPAD clinical practice consensus guidelines 2014: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15(Suppl. 20):154–79. https://doi.org/10.1111/pedi.12165.
• Kuppermann N, Ghetti S, Schunk J, Stoner MJ, Rewers A, McManemy JK, et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N Engl J Med. 2018;378(24):2275–87. https://doi.org/10.1056/NEJMoa1716816. This study prospectively studied the still-controversial idea of whether rapid fluid administration leads to potentially adverse outcomes in pediatric DKA< and found no such association.
Hsia DS, Tarai SG, Alimi A, Cross-Bu JA, Haymond MW. Fluid management in pediatric patients and rates of suspected clinical cerebral edema. Pediatr Diabetes. 2015;16(5):338–44. https://doi.org/10.1111/pedi.12268.
White PC, Dickson BA. Low morbidity and mortality in children with diabetic ketoacidosis treated with isotonic fluids. J Pediatr. 2013;163(3):761–6. https://doi.org/10.1016/j/jpeds.2013.02.005.
Basnet S, Venepalli PK, Andoh J, Verhulst S, Koirala J. Effect of normal saline and half normal saline on serum electrolytes during recovery phase of diabetic ketoacidosis. J Intensive Care Med. 2014;29(1):38–42. https://doi.org/10.1177/0885066612467149.
Toledo JD, Modesto V, Peinador M, Alvarez P, Lopez-Prats JL, Sanchis R, et al. Sodium concentration in rehydration fluids for children with ketoacidotic diabetes: effect on serum sodium concentration. J Pediatr. 2009;154:895–900. https://doi.org/10.1016/j.jpeds.2008.12.042.
Puttha R, Cooke D, Subbarayan A, Odeka E, Ariyawansa I, Bone M, et al. Low dose (0.05 units/kg/h) is comparable with standard dose (0.1 units/kg/h) intravenous insulin infusion for the initial treatment of diabetic ketoacidosis in children with type 1 diabetes—an observational study. Pediatr Diabetes. 2010;11(1):12–7. https://doi.org/10.1111/j.1399-5488.2009.00536.x.
Nallasamy K, Jayashree M, Singhi S, Bansal A. Low-dose vs standard-dose insulin in pediatric diabetic ketoacidosis. JAMA Pediatr. 2014;168(11):999–1005. https://doi.org/10.1001/jamapediatrics.2014.1211.
Fort P, Walters SM, Lifshitz F. Low-dose insulin infusion in the treatment of diabetic ketoacisosi: bolus versus no bolus. J Pediatr. 1980;96(1):36–40.
Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422–7. https://doi.org/10.1016/j.jemermed.2007.11.033.
Cohen M, Leibovitz N, Shilo S, Zuckerman-Levin N, Shavit I, Shehadeh N. Subcutaneous regular insulin for the treatment of diabetic ketoacidosis in children. Pediatr Diabetes. 2017;18:290–6. https://doi.org/10.1111/pedi.12380.
Della Manna T, Steinmetz L, Campos PR, Farhat SC, SChvartsman C, Kuperman H, et al. Subcutaneous use of a fast-acting insulin analog: an alternative treatment for pediatric patients with diabetic ketoacidosis. Diabetes Care. 2005;28:1856–61.
Glaser NS, Wootton-Gorges SL, Marcin JP, Buonocore MH, Dicarto J, Neely EK, et al. Mechanism of cerebral edema in children with diabetic ketoacidosis. J Pediatr. 2004;145:164–71.
Glaser N, Barnett P, McCaslin I, Nelson D, Trainor J, Louie J, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. N Engl J Med. 2001;344(4):264–9.
• Glaser NS, Wootton-Gorges SL, Buonocore MH, Tancredi DJ, Marcin JP, Caltagirone R, et al. Subclinical cerebral edema in children with diabetic ketoacidosis randomized to 2 different rehydration protocols. Pediatrics. 2013;131:e73–80. https://doi.org/10.1542/peds.2012-1049. As a follow-up to the 2001 NEJM publication, this study re-evaluated the risk of rapid rehydration and cerebral edema and did not find an increased risk.
DeCourcey DD, Steil GM, Wypij D, Agus MS. Increasing use of hypertonic saline over mannitol in the treatment of symptomatic cerebral edema in pediatric diabetic ketoacidosis: an 11-year-old retrospective analysis of mortality. Pediatr Crit Care Med. 2013;14(7):694–700. https://doi.org/10.1097/PCC.0b013e3182957cab.
Marcin JP, Glaser N, Bernett P, McCaslin I, Nelson D, Trainor J, et al. Factors associated with adverse outcomes in children with diabetic ketoacidosis-related cerebral edema. J Pediatr. 2002;141(6):793–7.
Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Diabetes Care. 2014;37(11):3124–31. https://doi.org/10.2337/dc14-0984.
Correll CU. Monitoring and management of antipsychotic-related metabolic and endocrine adverse events in pediatric patients. Int Rev Psychiatry. 2008;20(2):195–201. https://doi.org/10.1080/09540260801889179.
Fournier SH, Weinzimer SA, Levitt Katz LE. Hyperglycemic hyperosmolar non-ketotic syndrome in children with type 2 diabetes. Pediatr Diabetes. 2005;6:129–35.
•• Zeitler P, Hagg A, Rosenbloom A, Glaser N: Drigs and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Hyperglycemic hyperosmolar syndrome in children: pathophysiological considerations and suggested guidelines for treatment. J Pediatr 2011; 158(1): 9–14.e1–2. Doi: https://doi.org/10.1016/j.peds.2010.09.048. Following the increasing incidence of HHS in pediatrics, these guidelines established critical parameters of care.
Rosenbloom AL. Hyperglycemic hyperosmolar state: an emerging pediatric problem. J Pediatr. 2010;156(2):180–4. https://doi.org/10.1016/j/peds.2009.11.057.
Canarie MF, Bogue CW, Banasiak KJ, Weinzimer SA, Tamborlane WV. Decompensated hyperglycemic hyperosmolarity without significant ketoacidosis in the adolescent and young adult population. J Pediatr Endocrinol Metab. 2007;20:1115–24.
Kilbane BJ, Mehta S, Backeljauw PF, Shanley TP, Crimmins NA. Approach to management of malignant hyperthermia-like syndrome in pediatric diabetes mellitus. Pediatr Crit Care Med. 2006;7(2):169–73.
Faustino EV, Apkon M. Persistent hyperglycemia in critically ill children. J Pediatr. 2005;146(1):30–4.
Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics. 2006;118(1):173–9.
Srinivasan V, Spinella PC, Drott HR, Roth CL, Helfaer MA, Nadkarni V. Association of timing, duration, and intensity of hyperglycemia with intensive care unit mortality in critically ill children. Pediatr Crit Care Med. 2004;5(4):329–36.
Yung M, Wilkins B, Norton L, Slater A, Paediatric Study Group, Australian and New Zealand Intensive Care Society. Glucose control, organ failure, and mortality in pediatric intensive care. Pediatr Crit Care Med. 2008;9(2):147–52. https://doi.org/10.1097/PCC.0b013e3181668c22.
Vlasselaers D, Milants I, Desmet L, Wouters PJ, Vanhorebeek I, van den Heuvel I, et al. Intensive insulin therapy for patients in paediatric intensive care: a prospective, randomised controlled study. Lancet. 2009;373(9663):547–56. https://doi.org/10.1016/S0140-6736(09)60044-1.
Agus MS, Steil GM, Wypij D, Costello JM, Laussen PC, Langer M, et al. Tight glycemic control versus standard care after pediatric cardiac surgery. N Engl J Med. 2012;367(13):1208–19.
Macrae D, Grieve R, Allen E, Sadique Z, Morris K, Pappachan J, et al. A randomized trial of hyperglycemic control in pediatric intensive care. N Engl J Med. 2014;370(2):107–18. https://doi.org/10.1056/NEJMoa1302.
Agus MS, Wypij D, Hirshberg EL, Srinivasan V, Faustino EV, Luckett PM, et al. HALF-PINT Study Investigators and the PALISI Network. Tight glycemic control in critically ill children. N Engl J Med. 2017;376(8):729–41. https://doi.org/10.1056/NEJMoa1612348.
Chen L, Li T, Fang F, Zhang Y, Faramand A. Tight glycemic control in critically ill pediatric patients: a systematic review and meta-analysis. Crit Care. 2018;22(1):57. https://doi.org/10.1186/s/13054-018-1976-2.
Umpaichitra V, Banerji MA, Castells S. Autoantibodies in children with type 2 diabetes mellitus. J Pediatr Endocrinol Metab. 2002;15(Suppl 1):525–30.
Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–86. https://doi.org/10.1001/jama.2014.3201.
Chiang JL, Maahs DM, Garvey KC, Hood KK, Laffel LM, Weinzimer SA, et al. Type 1 diabetes in children and adolescents: a position statement by the American Diabetes Association. Diabetes Care. 2018;41(9):2026–44. https://doi.org/10.2337/dci18-0023.
American Diabetes Association. 13. Children and adolescents: Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019;42(Suppl. 1):S148–64. https://doi.org/10.2337/dc19-s013.
Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National Standards for Diabetes Self-Management Education and Support. Diabetes Care. 2017;40(10):1409–19. https://doi.org/10.2337/dci17-0025.
•• The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. This historical and landmark study established, for the first time, the link between decreased microvascular complications and tight glycemic control.
Rosenbauer J, Dost A, Karges B, Hungele A, Stahl A, Bachle C, et al. Improved metabolic control in children and adolescents with type 1 diabetes: a trend analysis using prospective multicenter data from Germany and Austria. Diabetes Care. 2012;35:80–6. https://doi.org/10.2337/dc11-0993.
Danne T, Phillip M, Buckingham BA, Jarosz-Chobot P, Saboo B, Urakami T, et al. Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes. 2018;2018(19):115–35. https://doi.org/10.1111/pedi.12718.
• TODAY Study Group, Zeitler P, Hirst K, Pyle L, Linder B, Copeland K, et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012;366(24):2247–56. https://doi.org/10.1056/NEJMoa1109333. This report from the TODAY trial identified the high risk of treatment failure with metformin alone in children with type 2 diabetes and led to more aggressive recommendations in care early after diagnosis.
Phelan H, King B, Anderson D, Crock P, Lopez P, Smart C. Young children with type 1 diabetes can achieve glycemic targets without hypoglycemia: results of a novel intensive diabetes management program. Pediatr Diabetes. 2018;19(4):769–75. https://doi.org/10.1111/pedi.12644.
Jefferies C, Rhodes E, Rachmiel M, Agwu JC, Kapellen T, Abdulla MA, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Management of children and adolescents with diabetes requiring surgery. Pediatr Diabetes. 2018;19(Suppl 27):227–36. https://doi.org/10.1111/pedi.12733.
Bristol Meyers Squibb. Retrieved from https://packageinserts.bms.com/pi/pi_gluco
American Diabetes Association. 15. Diabetes care in the hospital: Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019;42(Suppl. 1):S173–81. https://doi.org/10.2337/dc19-S015.
Umpierrez GE, Klonoff DC. Diabetes technology update: use of insulin pumps and continuous glucose monitoring in the hospital. Diabetes Care. 2018;41:1579–89. https://doi.org/10.2337/dci18-0002.
Retrieved from https://www.medtronicdiabetes.com/important-safety-information. October 2016.
Retrieved from https://www.myomnipod.com/safety. Insulet Corporation 2018.
Retrieved from https://www.tandemdiabetes.com/important-safety-information. Tandem Diabetes Care 2019.
Fattorusso V, Nugnes R, Casertano A, Valerio G, Mozzillo E, Franzese A. Non-diabetic hyperglycemia in the pediatric age: why, how, and when to treat? Curr Diab Rep. 2018;18(12):140. https://doi.org/10.1007/s11892-018-1115-0.
Burt MG, Roberts GW, Aguilar-Loza NR, Frith PS, Stranks SN. Continuous monitoring of circadian glycemic patterns in patients receiving prednisolone for COPD. J Clin Endocrinol Metab. 2011;96:1789–96. https://doi.org/10.1210/jc.2010-2729.
Yuen KC, McDaniel PA, Riddle MC. Twenty-four-hour profiles of plasma glucose, insulin, C-peptide and free fatty acid in subjects with varying degrees of glucose tolerance following short-term, medium-dose prednisone (20 mg/day) treatment: evidence for differing effects on insulin secretion and action. Clin Endocrinol. 2012;77:224–32. https://doi.org/10.1111/j.1365-2265.2011.04242.x.
Radhakutty A, Burt MG. Management of endocrine disease: critical review of the evidence underlying management of glucocorticoid-induced hyperglycaemia. Eur J Endocrinol. 2018;179(4):R207–18. https://doi.org/10.1530/EJE-18-0315.
Nettles AT. Patient education in the hospital. Diabetes Spectrum. 2005;18(1):44–8. https://doi.org/10.2337/diaspect.18.1.44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hospital Management of Diabetes
Rights and permissions
About this article
Cite this article
Kharode, I., Coppedge, E. & Antal, Z. Care of Children and Adolescents with Diabetes Mellitus and Hyperglycemia in the Inpatient Setting. Curr Diab Rep 19, 85 (2019). https://doi.org/10.1007/s11892-019-1205-7
Published:
DOI: https://doi.org/10.1007/s11892-019-1205-7