Abstract
Although once considered a benign consequence to the stress of severe illness or injury, a significant body of evidence compiled over the past decade shows that hyperglycemia in critically ill patients is associated with poor outcomes. In both adults and pediatric studies, there is a strong association with hyperglycemia with higher morbidity and mortality, and in some prospective studies, controlling hyperglycemia improves outcomes. These data have resulted in a number of national and international consensus statements and guidelines recommending active glycemic control – though primarily directed at the critically ill or injured adult. Due to the lack of pediatric-specific data, it has been unclear how pediatric intensivists should incorporate glycemic control into their practice. During the past decade data from both retrospective and prospective studies have also shown significant associations between hypoglycemia and dysglycemia (i.e., glycemic variability) and poor outcomes. From the current data, it appears that both hyper- and hypoglycemia occurs in patients who have higher illness severities and require more organ support measures. A number of pediatric-specific protocols have been developed and published which suggest that approaches to identify and manage hyperglycemia in critically ill children can be effectively and safely implemented, and interestingly in many cases hypoglycemic rates are less than that which occurs spontaneously. Although most pediatric practitioners support active glycemic control in certain subsets of patients, it is unclear how widespread standardized, consistent glycemic management has been incorporated into practice. Prospective trials have yielded disparate outcome findings regarding glycemic control in the pediatric ICU. Data from ongoing and completed studies will hopefully yield more definitive data on whether pediatric practitioners should regularly practice glycemic control, and what patient populations might benefit from this practice. This chapter reviews the existing data on hyperglycemia, hypoglycemia and dysglycemia, and will hopefully assist how pediatric practitioners synthesize these data into practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hyperglycemia
- Hypoglycemia
- Dysglycemia
- Glycemic variability
- Protocol
- Insulin
- Glucose
- Clinical trial
- Pediatric critical care
Introduction
A little more than a decade ago active management of glucose in any critical care patient, adult or pediatric, was infrequent and non-standardized. Although likely regularly assessed on most critically ill patients, the impact of blood glucose (BG) level on course or outcome was unclear. Usually considered as part of a protective counter-regulatory fight- or-flight response to acute stress, evidence had been mounting that prolonged exposure to hyperglycemia may be damaging to cells and organs during critical illness and negatively impact recovery. In 2001, a seminal randomized controlled trial from the adult surgical critical care unit in Leuven, Belgium was published demonstrating that in their patient population, maintaining glucose values in a range of “tight glycemic control” (i.e. ~80–110 mg/dL) with infused insulin resulted in improved outcomes compared to patients in whom BGs were controlled in a more “conventional” target range (180–210 mg/dL) [1]. What was most impressive about this report was the range of outcomes that were improved by careful, proactive BG control: shorter lengths of stay, fewer red cell transfusions and bloodstream infections, less renal injury and, importantly, an impressive reduction (i.e. ~40 %) in mortality. The primary adverse effect was an increase in hypoglycemia (from 0.7 to 5.2 %) with unclear clinical impact. In relatively short order, other data from adult ICUs supported the concept of proactive glycemic control using insulin infusions [2–5], which resulted in a number of official recommendations to implement standard approaches in BG management in critically ill patients. Although not specifically stated, recommendations were to practitioners of adult critical care, and it was unclear how these recommendations should be incorporated into pediatric critical care. These included recommendations from the Institute of Healthcare Improvement (IHI) and a combined consensus statement from the American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE) to maintain BG in ICU patients under 110 mg/dL [6]. In 2004, the Society of Critical Care Medicine (SCCM) addressed glycemic control in their Surviving Sepsis Campaign, stating “In patients with severe sepsis, maintain BG <150 mg/dL [using an] insulin infusion and glucose…” [7]. In less than 5 years from the original Leuven report, most adult ICUs had evolved from being indifferent to most patients’ BG, to taking a proactive approach in managing BG in a relatively low and tight threshold.
During this time, a number of studies seemed to refute the benefits of tight glycemic control [8–12]. In addition to supporting the concept that there may not be outcome benefits of maintaining BG in the “tight” range (i.e. 80–110 mg/dL), some of these suggested there may be harm, implicating the higher incidences of iatrogenic hypoglycemia and poorer outcomes with tight glycemic control. In fact, two large randomized controlled trials (RCTs) in adult ICUs, the VISIP [9] and Glucotrol [12] studies, which were comparing outcomes in patients with BG targeted to 80–110 mg/dL to more conservative ranges (180–200 and 140–180 mg/dL respectively) were prematurely stopped due to high rates of protocol violations and high rates of hypoglycemia. Neither of these suggested outcome improvements with tight glycemic control. In 2009, a large multi-national RCT consisting of over 6,000 patients from 42 adult medical or surgical ICUs, the NICE-SUGAR trial, compared outcomes in patients in whom glucoses were controlled 81–108 mg/dL versus under 180 mg/dL [10]. Although the difference of the average BG between groups was only ~30 mg/dL, there was a slight, but statistically higher mortality rate in the group undergoing tight glycemic control (27.5 v. 24.9 %, respectively). The tight glycemic control group had higher hypoglycemic rates (6.8 v 0.5 %, respectively), which appears to have influenced the difference in mortality.
Relatively soon after the publication of these last studies, revisions were made to the aforementioned consensus statements. Currently, IHI, ADA/AACE, and the SCCM Surviving Sepsis Campaign suggest active measure to control BG when it rises above 180 mg/dL [13, 14]. Of note, these groups have not suggested against glycemic control, but used recent studies to revise the target goals away from “tight” glycemic control (i.e. ~80–110 mg/dL). In the fall of 2012, the SCCM published the recommendations from a task force and suggested that a “glycemic control end point such that a BG ≥150 mg/dL triggers interventions to maintain BG below that level and absolutely <180 mg/dL” [15]. The rationale being that “there is a slight reduction in mortality with this treatment end point for general [adult] intensive care unit patients and reductions in morbidity for perioperative patients, postoperative cardiac surgery patients, post-traumatic injury patients, and neurologic injury patients”. This was the first consensus group that included pediatric intensivists on the panel, reviewed data from pediatric studies, and specifically addressed how pediatric intensivists should incorporate general recommendations (which were mostly based on the adult critical care literature) into their practice. Although it was concluded that “the literature is inadequate to support recommendations regarding glycemic control in pediatric patients”, it was recognized that there was associative data on hyperglycemia and poor outcomes in a number of pediatric critical care subpopulations. In addition, there is contrasting data from RCTs regarding direct benefits of glycemic control in critically ill children. In a relatively short time period there has been a substantial philosophical and practical shift adopted by many adult subspecialty critical care practices. Data in pediatric critical care has been slower to come, and due to the paucity of data (which may be conflicting) it has been a challenge for pediatric intensivists to develop a data-based approach to glycemic control.
Incidence and Associations of Hyperglycemiain Pediatric Critical Care
Soon after studies in glycemic control in adult ICUs were published, a number of studies were presented evaluating the incidence of hyperglycemia in pediatric critical care. Rates of hyperglycemia range from as low as 14 % to near 100 % of patients in pediatric ICUs [16–24]. This vast variability is likely due to several factors such as the definition of hyperglycemia and the population studied. There is yet to be a “consensus” on how critical illness hyperglycemia is defined in adult or pediatric critical care. Thresholds to define hyperglycemia in pediatric studies include values from 100 through 200 mg/dL. When given, rationale for these cutoffs included definitions of hyperglycemia and glucose intolerance used to define diabetes and glucose intolerance by the American Diabetes Association (i.e. a non-fasting BG cutoff of 140 mg/dL) and BG levels which surpasses the “renal threshold” and result in glucosuria (i.e. ~200 mg/dL) [25]. Most descriptive studies have been retrospective, and rely on routine, non-standardized glucose testing. In presenting the incidence of hyperglycemia, the denominator given most often is any patient who received a BG evaluation. “Hyperglycemic patients” (i.e. the numerator) are most frequently defined as any patient who had at least one BG greater than their threshold. The lower BG threshold used to define hyperglycemia, the higher the incidence will be, and most likely the more times a patient’s BG was checked, the likelihood of a high BG increases. With these caveats, studies by Faustino and Apkon, Wintergurst et al., and Hirshberg et al. all found that one half to almost two-thirds of all patients in a pediatric medical/surgical intensive care (50, 61, and 56 % respectively) had at least one BG reading of >150 mg/dL [19, 20, 23]. Depending on the BG threshold to define hyperglycemia, rates in general PICUs range from about 10–80 % of patients (Fig. 8.1a). To date, there has been no prospective study in which BGs are systematically checked in all PICU patients to define the true incidence of hyperglycemia in pediatric ICUs.
Relationship of hyperglycemia incidence and BG threshold in pediatric critical care. The incidence of hyperglycemia and defining BG was obtained from published studies and plotted. Studies were divided into three categories: (a) General pediatric medical/surgical PICU evaluating all admissions, (b) Patients with shock or specific organ failure (i.e. requiring mechanical ventilation or vasopressors), (c) Patients in cardiac ICUs and/or post-operative from cardiac surgery (Data sources: (a) [19–21, 23, 26]; (b) [16, 17, 22, 24, 26, 27]; (c) [27–30])
In studies where patients that are more critically ill (i.e. higher illness severity or more organ failure) are evaluated, the incidence of hyperglycemia increases (Fig. 8.1b). Studies have shown that nearly 50–75 % of patients on mechanical ventilation (MV) and 90 % on MV and/or vasopressors [22, 24, 26, 31], 72 % of patients with septic shock [24] and 90 % of patients with meningococcal sepsis had BGs >126–150 mg/dL [18]. When looking in cardiac ICUs, rates of hyperglycemia vary between 57 and 98 %, again depending on BG threshold and patient condition (Fig. 8.1c) [28–30, 32–34]. In other specific high risk PICU subpopulations rates are also high, for example 88 % in traumatic brain injury and 57 % in burn patients [35–38].
Taken together, these studies support an intuitive hypothesis that if patients are “more” critically ill, their likelihood of having a more robust stress response is greater, and thus it is reasonable that their BG would become (more) elevated. From studies of a practice group that initiated a standard protocol to screen for hyperglycemia in what were deemed “high risk” patients (defined as those who were receiving mechanical ventilation, vasopressors, or other vital organ support measures) and required to consecutive BG readings of >140 mg/dL to define hyperglycemia, ~50 % of patients who are mechanically ventilated and not receiving vasopressors and ~90 % of patients who are receiving both vasopressor support and are mechanically ventilated develop hyperglycemia [26, 31]. In further evaluation of patients not deemed “high risk” (i.e. no organ failure/support), hyperglycemia was rare (<6 %) [26]. This suggests that in pediatric patients, there is a strong positive relationship with organ failure and hyperglycemia. Taking this into account, the variability of incidence of hyperglycemia in pediatric ICUs is likely strongly influenced by the unit’s case mix of acuity and illness severity [31].
In addition to reporting incidences, many retrospective and descriptive studies have documented an association between hyperglycemia and poor outcome. A common theme has been a strong positive association of hyperglycemia and morbidity and mortality. In general, it has been found (similar to adult literature) that there is a positive association between hyperglycemia and ventilator days, ICU length of stay, use of high frequency ventilation, infections, inotrope use and renal insufficiency/failure [16–24, 28, 30, 31, 37, 38]. In general medical/surgical PICU populations, mortality rates are up to five to six times higher in those with hyperglycemia. In septic shock patients with respiratory failure, mortality is 2–3× higher in groups with hyperglycemia than without. In a study by Cochan et al., a BG of >300 mg/dL in children with TBI is predictive of non-survival [36]. Taken together, hyperglycemia exists in a substantial amount of patients in pediatrics ICUs. There are strong correlations of higher instances of hyperglycemia and illness severity, organ failure and poor outcomes, including mortality. It has been such studies which have prompted prospective studies of glycemic control in pediatric critical care, and initiating standard approaches to glycemic control by some pediatric intensivists.
Hypoglycemia in the PICU
The practice of glycemic control in critically ill patients has highlighted physicians’ concern for hypoglycemia. Surveys of pediatric intensivists showed that hypoglycemia was considered more dangerous than hyperglycemia [39, 40]. In fact, the fear of hypoglycemia was identified as a barrier to glycemic control in critically ill children [40]. Hypoglycemia is physiologically defined as the concentration of glucose in the blood or plasma at which the individual demonstrates a unique response to the adequate delivery of the glucose to a target organ, particularly the brain [41]. Counter-regulatory hormones such as glucagon, epinephrine, growth hormone and cortisol are usually activated in response to hypoglycemia once blood glucose concentration decreases to 60–80 mg/dL [42]. Hypoglycemic symptoms do not occur until blood glucose concentration is approximately 50 mg/dL and cognition does not appear depressed unless blood glucose concentration is approximately 40 mg/dL. Hypoglycemia has variable effects on the developing brain in preclinical models. Compared with adult rats, the brains of newborn rats are more resistant to neuronal injury from insulin-induced hypoglycemia [43]. The cause of hypoglycemia may also be important. During prolonged fast, the body produces ketones that the brain can use as alternative source of energy in the absence of glucose. Insulin inhibits ketogenesis and deprives the brain of both glucose and ketones, potentially resulting in worse outcomes with insulin-induced hypoglycemia [44]. The duration and frequency of the hypoglycemic episodes also affects the impact of hypoglycemia on the brain [10, 45]. Because of the difficulty in using a blood marker, i.e. blood glucose concentration, to diagnose symptomatic neuroglycopenia, pediatric intensivists use different blood glucose thresholds to define hypoglycemia. Values ranging from 40 to 80 mg/dL are typically used in clinical practice [39, 45, 46]. Observational and interventional studies usually report hypoglycemia as <60 mg/dL and severe hypoglycemia as <40 mg/dL [10, 27, 47]. Current convention is the BG value of <40 mg/dL is defined as “severe” hypoglycemia and <60, but greater or equal to 40 mg/dL is “moderate” hypoglycemia.
Hypoglycemia is not uncommon in critically ill children. In children with spontaneous or non-insulin induced hypoglycemia, 7.5–11.7 % of them have at least one blood glucose concentration <60 mg/dL [20, 45, 48]. The prevalence of severe spontaneous hypoglycemia with blood glucose concentration <40 mg/dL is 2.2–3.2 % [45, 48] of all patients in the pediatric intensive care unit but can be as high as 25 % in selected patients undergoing glycemic control with insulin [27].
Even in the absence of inborn errors of metabolism and insulin-secreting tumors that predispose children to hypoglycemia, critically ill children are at risk of hypoglycemia. Hypoglycemia is likely a reflection of the body’s overall inability to regulate blood glucose concentration [45, 49]. This may explain why children <1 year old, [20, 48] with higher severity of illness [48] and requiring more therapeutic interventions, [45, 48] who tend to be hyperglycemic, are also likely to have episodes of hypoglycemia. Vriesendorp et al. proposed that critically ill patients have relatively insufficient gluconeogenesis analogous to relative adrenal insufficiency [50]. The gluconeogenic pathways are overstressed because of the underlying illness such that they are unable to produce additional glucose to maintain euglycemia when faced with added stress. Additional stress may include side effects of certain drugs, such as octreotide and beta-blockers, or human error [45, 51]. Abrupt discontinuation of high glucose containing parenteral nutrition or renal replacement therapy solutions without glucose supplementation may lead to hypoglycemia. Impaired gluconeogenesis may also result from unrecognized renal or hepatic insufficiency.
The outcomes of hypoglycemia in critically ill children depend on the cause, severity and the frequency of the events. Spontaneous hypoglycemia is associated with increased mortality, [45] prolonged hospital stay [20, 23] and increased risk of nosocomial infections [20]. Compared with children with no hypoglycemia, the odds of mortality ranges from 2.7 in those with blood glucose concentration <60 mg/dL to 4.5 in those with blood glucose concentration <40 mg/dL [45]. Children with recurrent hypoglycemia have worse outcomes than those without or with a single episode of hypoglycemia. Depending on the glucose threshold, the odds of mortality in children with recurrent hypoglycemia are 4.8–6.3 compared with 1.2–3.7 odds in those with a single episode of hypoglycemia [45].
Insulin-induced hypoglycemia seems to have better outcomes compared with spontaneous hypoglycemia. In the randomized controlled trial on glycemic control by Vlasselaers et al., 25 % of children in the insulin-treated group developed severe hypoglycemia compared with 1 % in the control group [27]. The odds of mortality are not increased in the presence of severe hypoglycemia, and in fact this group in whom BG were more tightly controlled had less mortality. Insulin-induced hypoglycemia is also not associated with changes in neurocognitive development when children were tested 4 years after the hypoglycemic event [52]. Similar findings are noted in adults. In the NICE-SUGAR trial, the hazard ratio of mortality is significantly lower in patients with insulin-induced hypoglycemia (1.7 vs. 3.8 in adults with spontaneous hypoglycemia) [10]. In adults with acute myocardial infarction, hypoglycemia is a predictor of mortality in patients not treated with insulin but not in those treated with insulin (odds ratio of mortality: 2.3 vs. 0.9) [53].
The difference in outcomes between spontaneous and insulin-induced hypoglycemia suggests that hypoglycemia is merely a marker of the underlying disease [10, 45, 49]. The better outcomes in critically ill patients with insulin-induced hypoglycemia, compared with animal studies, may reflect the shorter duration that these patients are hypoglycemic. While critically ill children may have unrecognized hypoglycemic symptoms, they are unlikely to be hypoglycemic for prolonged periods of time because their blood glucose concentrations are monitored closely [45].
Glycemic Variability
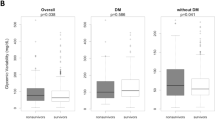
Recent evidence suggests that extreme fluctuations in blood glucose concentrations in critically ill patients are harmful, independent of the actual blood glucose concentrations or the presence of hypoglycemia. It has been postulated that the contrasting results between the Leuven and the NICE-SUGAR trials may be partly explained by differences in glycemic variability [54]. The association between glycemic variability and mortality was initially reported by Egi et al. [55] and Wintergerst et al. in 2006 [23]. Egi et al. reported that in critically ill adults whose blood glucose concentration was strictly controlled with insulin infusion, both the mean and standard deviation of blood glucose concentrations are independently associated with mortality [55]. Subsequent studies have confirmed this association in adults [56]. Wintergerst et al. reported that glycemic variability is also associated with mortality and increased hospital stay in critically ill children [23]. Using a glucose variability index calculated as a time-weighted change in blood glucose concentration, glucose variability had the strongest association with mortality compared with maximal and minimal blood glucose concentrations. Other studies support this association in children. Hirshberg et al. reported that critically ill children with both hyperglycemia and hypoglycemia have higher odds of mortality and nosocomial infection, and longer hospital stays compared with children with isolated hyperglycemia or hypoglycemia [20]. Using the standard deviation of the blood glucose concentrations of each critically ill child, Rake et al. reported that glycemic variability is positively correlated with mortality rates [57].
Similar to hypoglycemia, the increased mortality associated with significant glycemic variability may represent the body’s inability to maintain blood glucose allostasis i.e., physiologic adaptation to change [57]. Glycemic variability during the acute phase of illness is likely adaptive that allows the body to respond to stress. However, glycemic variability during the chronic phase of illness may be maladaptive and represent secondary damage to the systems controlling blood glucose concentration. Rake et al. demonstrated that among survivors, glycemic variability decreases during the late phase of critical illness [57]. In contrast, blood glucose concentration was persistently variable among non-survivors. Alternatively, fluctuations in blood glucose may result in increased oxidative stress and endothelial dysfunction leading to worse patient outcomes [54].
Glycemic Control Protocols in the PICU
The efficacy of glycemic control in critically ill children is unclear. The study by Vlasselaers et al. demonstrated a significant mortality benefit in controlling blood glucose concentrations to age-adjusted normal values [27]. In contrast, the study by Agus et al. did not detect any significant benefit with glycemic control in post-operative cardiac patients [47]. The results of trials in adults are also conflicting. The initial trial by van den Berghe et al. [1] demonstrated mortality benefit with glycemic control while the NICE-SUGAR trial [10] demonstrated increased mortality in the intervention group. Despite the differences in the results of pediatric and adult trials, glycemic control continues to be practiced in critically ill children [46].
Safe implementation of glycemic control requires the use of protocols. An optimal protocol should include an explicit algorithm that determines insulin dosing and minimizes interpretation by the bedside clinician, frequent monitoring of blood glucose concentration, provision for dextrose supplementation or for stopping insulin if glucose source interrupted, and standardize approach to the management of hypoglycemia [15]. Ideally, a protocol should incorporate patient characteristics and caloric intake to individualize insulin dosing recommendations. Because dosing algorithms are usually complex, computerized protocols are preferred. Computerized protocols have been shown to be more effective in achieving target blood glucose concentrations, [58, 59] associated with less hypoglycemic events, [58, 59] better protocol compliance [60] and higher nurse satisfaction [61] compared with paper-based protocols.
A number of protocols have been developed for controlling blood glucose concentrations in critically ill children (Table 8.1). In most of the protocols, the recommended insulin infusion rate is adjusted based on the rate of change in the blood glucose concentration and the current insulin infusion rate [60]. Computerized protocols tend to have more complex insulin dosing algorithms that are difficult to replicate on paper [47, 62]. Because of uncertainty in the optimal blood glucose target for children, different ranges are used. The performance and the risk of hypoglycemia differ per protocol.
Of the existing protocols there are two main types: those that recommend an incremental response to change in blood glucose within different ranges, and those that change the algorithm’s sensitivity to glucose changes. Whichever type of mathematical approach an algorithm employs, the recommendations can be implemented either by written rules for making the incremental adjustments or by equations which continuously calculate incremental adjustments. A benefit of the mathematical algorithm approach is that weight-specific, glucose-concentration specific recommendations can be made for glucose rescue from hypoglycemia.
A critical determinant of the success of any protocol is the quality and frequency of the data that are input into it. Blood glucose concentrations are ideally measured from an arterial source, since there is some arterio-venous decrement due to glucose extraction at the tissue level. Central venous blood may also be a reliable and stable source for measuring glucose. Capillary blood should be reserved for short-term use only due to potential for poor peripheral perfusion in critically ill children. When drawing blood from an intravascular catheter, one should take extreme care to waste adequate amounts of blood, 1–2 mL, prior to collecting the sample that is to be tested. This may be achieved at little cost to the patient by using a closed blood drawing system, several of which are on the market.
Blood glucose should be monitored at a standard interval of 1–2 h during an intravenous insulin infusion. This can be spaced to some extent if insulin dose and carbohydrate supply are not changed in that period. Adult protocols that are based upon every 4 h blood glucose checks may have severe hypoglycemia rates of 10 % or more. There remains much debate as to what devices are acceptable for use to measure blood glucose. The most accurate devices are in the hospital central laboratory, which measure serum concentrations. Blood gas machines are also particularly reliable; some ICUs have the benchtop machines in the ICU, others use a point-of-care blood gas device. FDA-approved hospital glucose meters have become increasingly reliable in recent years. After taking into account the risk of performing glucose control in the ICU without a glucose measurement device at the bedside, we believe the newest generation (after 2011) are acceptable for use in the PICU.
Continuous glucose monitoring devices have also made significant technological progress in the last 5 years, however, not enough to warrant using them to directly guide insulin dosing. Among FDA approved devices, the most commonly available one is the subcutaneous sensor which is designed for use in ambulatory diabetics. While not FDA approved for this indication, these sensors have been successful in the context of clinical trials to significantly reduce the incidence of hypoglycemia when on an insulin infusion. The most appropriate use is as a hypoglycemia alarm device. Through conducting clinical trials in this field, we have learned that there are identifiable risk factors for hypoglycemia (Table 8.2) which the continuous monitor has helped to address.
Randomized Controlled Trial in Glycemic Control in Pediatric Critical Care
The first pediatric randomized controlled trial of 700 critically ill pediatric patients was completed in a single center in Leuven, Belgium, which established that insulin infusion titrated to a goal of 50–80 mg/dL in infants and 70–100 mg/dL in children, compared with insulin infusion only to prevent BG greater than 215 mg/dL, improved short-term outcomes. The absolute risk of mortality was reduced by 54 % (conventional 5.7 % vs. intervention 2.6 %, p = 0.038), and insulin therapy also reduced the ICU length of stay and C-reactive protein (the primary outcome variable). The study was notable for its first proof of principle that lower ranges of glycemic control produce clinical benefit in children. It was also remarkable for its low target BG ranges in the intervention groups, which were described as “age-adjusted normoglycaemia” (50–80 mg/dL in <1 year old, 70–100 mg/dL in >1 year old). Although several outcomes in this trial were favorable, there were extremely high rates of severe hypoglycemia (<40 mg/dL): 44 % in those <1 year old and 25 % overall. In light of this, the protocol is unlikely to be replicated outside Leuven, and the findings of clinical benefit cannot be widely applied. Of note, the 4-year follow-up study assessed neurocognitive outcomes in participants in the trial and did not identify any differences in cognitive performance between those enrolled in the tight control versus conventional therapy arm.
The second published randomized clinical trial in the field, called SPECS (Safe Euglycemia in Cardiac Surgery) was conducted in two centers in a relatively homogeneous population of 980 post-operative cardiac surgical patients less than 3 years of age. Subjects were randomized to 80–110 mg/dL versus standard care, which was essentially no insulin. Although subjects in the TGC arm of the trial reached target range more quickly than the standard care arm, stayed in range longer, and had a lower time-weighted blood glucose average, outcomes were identical between the two groups. It is notable that the differences in the glucose profiles across the two groups became indistinguishable after 48 h, raising the question of whether the exposure to glucose control was too brief to affect a difference in outcomes. When analyzing the entire cohort, no differences in outcomes were noted. Post hoc analyses are reported to be underway which may identify subgroups that did derive benefit, but these have not yet been published.
Three other major trials are underway at the time of writing this chapter, which may help us understand more about controlling blood glucose in critically ill children. Control of Hyperglycaemia In Paediatric Intensive Care (CHiP; ISRCTN61735247) is a 1,384-patient study of cardiac, medical and surgical ICU patients, randomizing to either 72–126 or 180–215 mg/dL with primary outcome of ventilator-free days at 30 days. Pediatric ICUs at Indiana and Emory-Children’s Center Glycemic Control: The PedIETrol Trial (NCT01116752) is a 1,004-patient trial of 80–140 versus 190–220 mg/dL including cardiac, medical and surgical ICU patients, where the primary outcome is recovery of organ function specified as PELOD score at 6 days. Heart And Lung Failure – Pediatric INsulin Titration trial (HALF-PINT; NCT01565941) is a 30-center multi-center trial of 80–110 vs 150–180 mg/dL with the primary outcome of ICU-free days, or 28-day hospital mortality-adjusted ICU length of stay. As the results are published of these three major trials and possibly others we will be able to generate more definitive recommendations about glycemic control in specific situations.
Conclusion
The past decade has shown rapid change in how hyperglycemia is regarded and managed in all disciplines of critical care. In adult critical care there is a strong body of evidence that, at least in some patients, benefit can come from strict management of hyperglycemia using insulin. Although there are strong associations of poor outcome and hyperglycemia and hypoglycemia in pediatric critical illness, is not yet clear which patient populations, if any, will benefit from routine glycemic control. Data to base best practice will only come through the implementation of carefully planned prospective studies.
References
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–67.
Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125(5):1007–21.
Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc. 2004;79(8):992–1000.
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–61.
Scalea TM, Bochicchio GV, Bochicchio KM, Johnson SB, Joshi M, Pyle A. Tight glycemic control in critically injured trauma patients. Ann Surg. 2007;246(4):605–10; discussion 610–2.
Garber AJ, Moghissi ES, Bransome Jr ED, et al. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10 Suppl 2:4–9.
Dellinger RP, Carlet JM, Masur H, et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–73.
Arabi YM, Dabbagh OC, Tamim HM, et al. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med. 2008;36(12):3190–7.
Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–39.
Finfer S, Chittock DR, Su SY, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–97.
Gandhi GY, Nuttall GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery: a randomized trial. Ann Intern Med. 2007;146(4):233–43.
Preiser JC, Devos P, Ruiz-Santana S, et al. A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35(10):1738–48.
Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–31.
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
Jacobi J, Bircher N, Krinsley J, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40(12):3251–76.
Branco RG, Garcia PC, Piva JP, Casartelli CH, Seibel V, Tasker RC. Glucose level and risk of mortality in pediatric septic shock. Pediatr Crit Care Med. 2005;6(4):470–2.
Branco RG, Tasker RC. Glycemic level in mechanically ventilated children with bronchiolitis. Pediatr Crit Care Med. 2007;8(6):546–50.
Day KM, Haub N, Betts H, Inwald DP. Hyperglycemia is associated with morbidity in critically ill children with meningococcal sepsis. Pediatr Crit Care Med. 2008;9(6):636–40.
Faustino EV, Apkon M. Persistent hyperglycemia in critically ill children. J Pediatr. 2005;146(1):30–4.
Hirshberg E, Larsen G, Van Duker H. Alterations in glucose homeostasis in the pediatric intensive care unit: hyperglycemia and glucose variability are associated with increased mortality and morbidity. Pediatr Crit Care Med. 2008;9(4):361–6.
Klein GW, Hojsak JM, Schmeidler J, Rapaport R. Hyperglycemia and outcome in the pediatric intensive care unit. J Pediatr. 2008;153(3):379–84.
Srinivasan V, Spinella PC, Drott HR, Roth CL, Helfaer MA, Nadkarni V. Association of timing, duration, and intensity of hyperglycemia with intensive care unit mortality in critically ill children. Pediatr Crit Care Med. 2004;5(4):329–36.
Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics. 2006;118(1):173–9.
Yung M, Wilkins B, Norton L, Slater A. Glucose control, organ failure, and mortality in pediatric intensive care. Pediatr Crit Care Med. 2008;9(2):147–52.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27 Suppl 1:S5–10.
Preissig CM, Hansen I, Roerig PL, Rigby MR. A protocolized approach to identify and manage hyperglycemia in a pediatric critical care unit. Pediatr Crit Care Med. 2008;9(6):581–8.
Vlasselaers D, Milants I, Desmet L, et al. Intensive insulin therapy for patients in pediatric intensive care: a prospective, randomised controlled study. Lancet. 2009;373(9663):547–56.
Falcao G, Ulate K, Kouzekanani K, Bielefeld MR, Morales JM, Rotta AT. Impact of postoperative hyperglycemia following surgical repair of congenital cardiac defects. Pediatr Cardiol. 2008;29(3):628–36.
Preissig CM, Rigby MR, Maher KO. Glycemic control for postoperative pediatric cardiac patients. Pediatr Cardiol. 2009;30(8):1098–104.
Yates AR, Dyke 2nd PC, Taeed R, et al. Hyperglycemia is a marker for poor outcome in the postoperative pediatric cardiac patient. Pediatr Crit Care Med. 2006;7(4):351–5.
Preissig CM, Rigby MR. Pediatric critical illness hyperglycemia: risk factors associated with development and severity of hyperglycemia in critically ill children. J Pediatr. 2009;155(5):734–9.
Ghafoori AF, Twite MD, Friesen RH. Postoperative hyperglycemia is associated with mediastinitis following pediatric cardiac surgery. Paediatr Anaesth. 2008;18(12):1202–7.
Hebson CL, Chanani NK, Rigby MR, et al. Safe and effective use of a glycemic control protocol for neonates in a cardiac ICU. Pediatr Crit Care Med. 2013;14(3):284–9.
Ulate KP, Lima Falcao GC, Bielefeld MR, Morales JM, Rotta AT. Strict glycemic targets need not be so strict: a more permissive glycemic range for critically ill children. Pediatrics. 2008;122(4):e898–904.
Chiaretti A, De Benedictis R, Langer A, et al. Prognostic implications of hyperglycemia in pediatric head injury. Childs Nerv Syst. 1998;14(9):455–9.
Cochran A, Scaife ER, Hansen KW, Downey EC. Hyperglycemia and outcomes from pediatric traumatic brain injury. J Trauma. 2003;55(6):1035–8.
Gore DC, Chinkes D, Heggers J, Herndon DN, Wolf SE, Desai M. Association of hyperglycemia with increased mortality after severe burn injury. J Trauma. 2001;51(3):540–4.
Pham TN, Warren AJ, Phan HH, Molitor F, Greenhalgh DG, Palmieri TL. Impact of tight glycemic control in severely burned children. J Trauma. 2005;59(5):1148–54.
Hirshberg E, Lacroix J, Sward K, Willson D, Morris AH. Blood glucose control in critically ill adults and children: a survey on stated practice. Chest. 2008;133(6):1328–35.
Preissig CM, Rigby MR. A disparity between physician attitudes and practice regarding hyperglycemia in pediatric intensive care units in the United States: a survey on actual practice habits. Crit Care. 2010;14(1):R11.
Cornblath M, Hawdon JM, Williams AF, et al. Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics. 2000;105(5):1141–5.
Sprague JE, Arbelaez AM. Glucose counterregulatory responses to hypoglycemia. Pediatr Endocrinol Rev. 2011;9(1):463–73; quiz 474–65.
Ennis K, Tran PV, Seaquist ER, Rao R. Postnatal age influences hypoglycemia-induced neuronal injury in the rat brain. Brain Res. 2008;1224:119–26.
Yager JY, Heitjan DF, Towfighi J, Vannucci RC. Effect of insulin-induced and fasting hypoglycemia on perinatal hypoxic-ischemic brain damage. Pediatr Res. 1992;31(2):138–42.
Faustino EV, Bogue CW. Relationship between hypoglycemia and mortality in critically ill children. Pediatr Crit Care Med. 2010;11(6):690–8.
Hirshberg EL, Sward KA, Faustino EV, et al. Clinical equipoise regarding glycemic control: a survey of pediatric intensivist perceptions. Pediatr Crit Care Med. 2013;14(2):123–9.
Agus MS, Steil GM, Wypij D, et al. Tight glycemic control versus standard care after pediatric cardiac surgery. N Engl J Med. 2012;367(13):1208–19.
Ognibene KL, Vawdrey DK, Biagas KV. The association of age, illness severity, and glycemic status in a pediatric intensive care unit. Pediatr Crit Care Med. 2011;12(6):e386–90.
Kyle UG, Coss Bu JA, Kennedy CE, Jefferson LS. Organ dysfunction is associated with hyperglycemia in critically ill children. Intensive Care Med. 2010;36(2):312–20.
Vriesendorp TM, DeVries JH, Hoekstra JB. Hypoglycemia and strict glycemic control in critically ill patients. Curr Opin Crit Care. 2008;14(4):397–402.
Vriesendorp TM, van Santen S, DeVries JH, et al. Predisposing factors for hypoglycemia in the intensive care unit. Crit Care Med. 2006;34(1):96–101.
Mesotten D, Gielen M, Sterken C, et al. Neurocognitive development of children 4 years after critical illness and treatment with tight glucose control: a randomized controlled trial. JAMA. 2012;308(16):1641–50.
Kosiborod M, Inzucchi SE, Goyal A, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301(15):1556–64.
Egi M, Bellomo R. Reducing glycemic variability in intensive care unit patients: a new therapeutic target? J Diabetes Sci Technol. 2009;3(6):1302–8.
Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105(2):244–52.
Egi M, Bellomo R, Reade MC. Is reducing variability of blood glucose the real but hidden target of intensive insulin therapy? Crit Care. 2009;13(2):302.
Rake AJ, Srinivasan V, Nadkarni V, Kaptan R, Newth CJ. Glucose variability and survival in critically ill children: allostasis or harm? Pediatr Crit Care Med. 2010;11(6):707–12.
Bouw JW, Campbell N, Hull MA, Juneja R, Guzman O, Overholser BR. A retrospective cohort study of a nurse-driven computerized insulin infusion program versus a paper-based protocol in critically ill patients. Diabetes Technol Ther. 2012;14(2):125–30.
Cavalcanti AB, Silva E, Pereira AJ, et al. A randomized controlled trial comparing a computer-assisted insulin infusion protocol with a strict and a conventional protocol for glucose control in critically ill patients. J Crit Care. 2009;24(3):371–8.
Faraon-Pogaceanu C, Banasiak KJ, Hirshberg EL, Faustino EV. Comparison of the effectiveness and safety of two insulin infusion protocols in the management of hyperglycemia in critically ill children. Pediatr Crit Care Med. 2010;11(6):741–9.
Dumont C, Bourguignon C. Effect of a computerized insulin dose calculator on the process of glycemic control. Am J Crit Care. 2012;21(2):106–14.
Thompson BT, Orme JF, Zheng H, et al. Multicenter validation of a computer-based clinical decision support tool for glucose control in adult and pediatric intensive care units. J Diabetes Sci Technol. 2008;2(3):357–68.
Verhoeven JJ, Brand JB, van de Polder MM, Joosten KF. Management of hyperglycemia in the pediatric intensive care unit; implementation of a glucose control protocol. Pediatr Crit Care Med. 2009;10(6):648–52.
Branco RG, Xavier L, Garcia PC, et al. Prospective operationalization and feasibility of a glycemic control protocol in critically ill children. Pediatr Crit Care Med. 2011;12(3):265–70.
Chima RS, Schoettker PJ, Varadarajan KR, et al. Reduction in hypoglycemic events in critically ill patients on continuous insulin following implementation of a treatment guideline. Qual Manag Health Care. 2012;21(1):20–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Agus, M.S.D., Faustino, E.V.S., Rigby, M.R. (2014). Hyperglycemia, Dysglycemia and Glycemic Control in Pediatric Critical Care. In: Wheeler, D., Wong, H., Shanley, T. (eds) Pediatric Critical Care Medicine. Springer, London. https://doi.org/10.1007/978-1-4471-6416-6_8
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6416-6_8
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6415-9
Online ISBN: 978-1-4471-6416-6
eBook Packages: MedicineMedicine (R0)