Abstract
Purpose of Review
The aim of this review is to summarize the current data available on the metabolic effects of fecal microbiota transplantation (FMT) including obesity and glucose metabolism in humans.
Recent Findings
Gut microbiota dysbiosis is a frequent characteristic observed in obesity and related metabolic diseases. Pieces of evidence mostly generated in mouse models suggest that rescuing this dysbiosis associates with improved metabolism. In humans, dietary or bariatric surgery interventions are often accompanied by complete or partial restoration of this dysbiosis together with weight reduction and metabolic amelioration. FMT is an interesting option to modify gut microbiota and has been associated with improved clinical outcomes, albeit only used in routine care for Clostridium difficile infection. However, there are only limited data on using FMT in the metabolic context.
Summary
FMT from lean donors significantly improves insulin sensitivity in obese subjects with metabolic syndrome. However, there is a wide range of clinical responses. Interestingly in subjects with high microbial gene richness at baseline and when FMT donors that are metabolically compromised are used, no metabolic improvement is seen. Moreover, more studies evaluating the effect of FMT in patients with overt type 2 diabetes are warranted. Furthermore, interventions (in the receiver prior to FMT) aiming to enhance FMT response also need evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The intestinal microbiome is increasingly recognized to play major roles in human physiology and health. Indeed, among its numerous functions, it modulates and shapes host immunity, is able to digest some otherwise indigestible dietary-derived nutrients [1] leading to the production of important metabolites for the host [2], including short-chain fatty acids (SCFA), and is involved in biliary acid dehydroxylation and synthesis of several vitamins [1]. Flourishing literature shows that many chronic diseases are associated with gut microbiota dysbiosis which include drastic changes in microbiota composition, function, and bacterial-derived metabolite production. This is particularly described for obesity and type 2 diabetes (T2D) [3,4,5,6].
Among reported features, in both mice [7] and humans [8], obesity is characterized by a decrease in bacterial diversity and low microbial gene richness (MGR: gene count number) in some subjects [5, 6]. In overweight to severe obesity, low MGR is associated with increased body mass index (BMI) as well as metabolic derangements including low-grade inflammation and insulin resistance [5, 6]. The proportion of low MGR concerns 23 to 40% of individuals with overweight or moderate obesity [5, 6] and increases up to 75% in severe obesity [9••]. Furthermore, a low MGR-associated gut microbiota profile shows a switch towards increased bacterial strains with pro-inflammatory properties as well as a decrease in those with anti-inflammatory roles [5, 6]. Likewise, both mice and human studies demonstrated that T2D is also characterized by a modification of gut microbiota composition and function, when compared with healthy controls [10] or with individuals with impaired glucose tolerance [3, 11]. Nevertheless, the role of altered gut microbiota as causality or consequence in metabolic diseases remains a source of discussion [12].
Several types of interventions are able to induce both beneficial metabolic outcomes and partial or complete correction of gut microbiota dysbiosis. For example, a moderately restrictive, fiber-enriched diet proposed to overweight or moderately obese individuals induced a significant increase of MGR especially in patients with baseline low MGR, and associations were found between changes in some bacterial groups and weight loss–improved metabolism [6]. Likewise, bariatric surgery reserved for the most severe forms of obesity leads to significant increases in MGR and modifies some bacterial species concomitantly with improvement in metabolic alteration and major weight loss [9••]. Although based on associations, these studies suggest that the modulation of gut microbiota per se could at least be partly involved in metabolic improvements. The role of gut microbiota modulation after bariatric surgery in the improvement of T2D has recently been reviewed in [13]. Ingestion of dietary prebiotics has also demonstrated potential to induce weight loss and improvement of insulin resistance and overall metabolic health in rodent models [14]. Nevertheless, when translating these interventions to humans, while prebiotics were indeed able to modify the composition of gut microbiota, their effects on metabolic health and weight were either very modest with merely a slight decrease in post-prandial glycemia and no effect on weight loss [15] or completely absent [16]. Similar observations can be made regarding the use of probiotics [17]. Overall these studies suggest that interventions modifying gut microbiota could be considered for therapeutic innovation in the field of T2D and obesity, especially when taking baseline microbiota composition and diversity into account. This concept is further reinforced by fecal transplantation experiments in rodents, highlighting the contribution of gut microbiota in weight reduction at least in mice.
For example, transferring feces from mice [18] or humans [19] who have undergone a bariatric procedure, into germ-free recipients, induces per se a weight reduction in the receivers. While the importance of weight loss is much lower than that induced by bariatric surgery, these studies highlight the important role of gut microbiota in weight reduction at least in mice, through fecal microbiota transplantation (FMT). However whereas FMT is now a recommended procedure in the treatment of Clostridium difficile (CD) infection, as described below, it remains to be demonstrated whether FMT could also be considered in the standard care of common disorders including metabolic diseases or obesity.
In this review, we will first review how FMT is being more broadly used due to its clinical successes and its technological innovation. We will then focus on whether using gut microbiota modulation via FMT has demonstrated any beneficial therapeutic effects on obesity and/or T2D. Finally, we will discuss potential factors impacting and modulating FMT success.
Fecal Microbiota Transplantation in Humans
A Success Story in Clostridium difficile Infection
The main routine care indication for FMT lays in the treatment of CD infection, reserved for cases resistant to antibiotherapy [20,21,22,23]. This disease originates from the major gut microbiota dysbiosis induced by the use of several lines of antibiotic regimens. FMT enhances gut microbiota diversity resulting in an improved clinical response or even the cure of this disease in 80 to 90% of the cases [24] with 60% of complete remission 1 month after FMT [25]. One of the first randomized clinical trials performed by our group was stopped prematurely since it showed, before the end of the trial, that FMT was effective and safe compared with antibiotics [26••], and these results have now been confirmed in several other randomized control trials [22, 27••, 28, 29] as well as in a recent meta-analysis [30]. Also, FMT has now been included in guidelines that recommend FMT in the context of recurrent CD infection to be used as the standard of care [31,32,33]. Most importantly, a consensus expert panel defined key recommendations for FMT use in CD infections [34] as well as the guidelines around technical, regulatory, administrative, and laboratory requirements for optimal FMT usage [35]. FMT is now being tested in clinical trials in other diseases such as inflammatory bowel diseases (IBD) [36, 37] and Crohn’s disease [38], which are also associated with a marked dysbiosis.
Novelty in the Administration Route of FMT
FMT was, and is still in most research studies, performed either using a nasojejunal tube, colonoscopy, or enema, sometimes requiring several administrations to be efficient in some diseases [37]. Most studies have observed good treatment tolerance both in the short and longer term and very rarely adverse events are seen, which mostly seem to be originating from the initial disease severity rather than FMT itself [39, 40]. Importantly, careful selection of the FMT donors [34] ensures part of this treatment safety [37, 39, 41]. Nevertheless, the risks originate mainly from the administration route. While no adverse event was detected using enemas, studies using nasogastric tube administration have reported few cases of intestinal bleeding and peritonitis [41]. In a large meta-analysis including over 1000 patients, colonoscopy administration was also associated with adverse events leading to hospitalization in 0.97% of patients receiving FMT. One death directly due to FMT was reported and the patient died from aspiration during sedation, while undergoing FMT through colonoscopy administration for a chronic CD infection [39]. Another death was reported due to pneumonia potentially caused by regurgitation during FMT using a nasoduodenal tube [42]. Nevertheless the most frequent adverse events are not serious and include intestinal symptoms such as bloating, flatulence, belching and abdominal cramps, abdominal discomfort, irregularity of bowel movements, and vomiting [43, 44]. Thus the FMT procedure appears safe overall; a national FMT registry has been initiated to study potential long-term side effects [45].
Based on the efficacy and (short-term) safety of FMT in CD infection, technologic developments have been made to enhance and facilitate FMT in routine clinical care and decrease adverse events linked to administration route by developing oral capsulized frozen FMT [46] and using frozen FMT stooling treated with glycerol as a cryoprotective procedure [47]. Concerning the efficacy of encapsulated FMT, a recent randomized control trial demonstrated that oral administration was as efficient as classic administration routes to obtain beneficial health outcomes mainly in CD infection [48]. Most importantly, no adverse event was observed post-FMT using this oral capsulized technique. Similar results have recently been reproduced in a study with 15 patients that were treated by 30 frozen capsules taken within 2 days (around 20 g of feces). This treatment enabled 86.6% remission rate after one FMT and 100% remission rate after the second administration, with excellent tolerance to this new administration route [49]. The only adverse events observed were linked to the severity of the initial disease [49]. Overall encapsulated FMT or “poop pills” as they are termed seem to be a relevant and safe alternative to more invasive FMT administration route and will probably increase the feasibility and acceptability of this treatment.
Fecal Microbiota Transplantation in Metabolic Diseases and Obesity
Improved Metabolic Health in Humans?
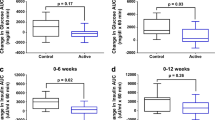
FMT used as a treatment option in obesity and other metabolic diseases has recently emerged. The reasons why gut microbiota modulation could beneficially affect glucose control have been extensively discussed herein [50] and include its actions on SCFA production, altered bile acids composition, and adipose tissue inflammation [51]. Our first pilot FMT study in metabolic syndrome included nine overweight/moderately obese individuals submitted to donor FMT originating from lean healthy controls that displayed a significant improvement in peripheral insulin sensitivity assessed by the gold standard, which is a stable isotope–based euglycemic-hyperinsulinemic clamp [52]. This beneficial effect was confirmed in a threefold larger follow-up study which also observed a minor yet significant reduction in glycated hemoglobin (HbA1c) at 6 weeks. Importantly, this study also showed that a reduced baseline microbial gene richness before lean donor FMT was associated with a better outcome [53••]. Despite the use of gastroduodenoscopy and nasoduodenal tube for donor FMT administration, no adverse events were reported. Interestingly however, response to donor FMT showed major inter-individual variability among receivers in both studies, with some patients displaying major improvements while others remained stable [52, 53••]. Lean donor FMT induced differential microbiota modifications in good and poor responders [53••]. For example, after FMT, good responders displayed an increase in Akkermansia muciniphila which has been previously associated with metabolic health improvement in mice [54, 55] but also in humans [56]. Another critical question is the long-term effect in FMT. The metabolic syndrome intervention showed that at 18 weeks, there was no remaining effect on insulin sensitivity and gut microbiota composition switched back to the baseline composition [53••]. This underscores the temporary nature of this FMT intervention. Nevertheless, these pioneering studies in treating naive prediabetes (metabolic syndrome) male subjects demonstrate that FMT could be of therapeutic use to improve insulin resistance and decrease HbA1c (Fig. 1) yet with a transient effect suggesting that multiple cures of FMT would probably be necessary.
Effects of fecal microbiota transplantation (FMT) in obese patients with metabolic alterations. Obesity, which represents a low-grade inflammatory disease with increased intestinal inflammation, and type 2 diabetes (T2D) are associated with gut microbiota dysbiosis. The literature has shown that fecal microbiota transplantation from lean donors enables the engraftment of bacterial strains from the donor and thus induces improvement in insulin resistance, for a short period of time. In the future, oral capsulized FMT will have to be tested in patients with T2D to evaluate whether it also improves intestinal inflammation, gut microbiota dysbiosis, and glycemic control
Moreover, as T2D is a chronic disease where patients need to take multiple glucose-lowering drugs several times every day, whether FMT has any effect in patients with severe insulin resistance and eventually decreased insulin secretion remains to be studied. Nevertheless, as our study data have shown, subjects with the metabolic syndrome and the most severe insulin resistance do not show any beneficial effect from lean donor FMT on insulin sensitivity. In line with our previously mentioned studies in obesity [52, 53••], it is possible that gut microbiome plays a role in the early stages of insulin resistance and T2D whereas it is less critical in glycemic control of patient with advanced stages of T2D. Nevertheless, since FMT administrated by oral capsule appears safe, it provides an actionable tool to explore the relevance and differential effect of FMT in patients at different stages of glucose dysregulation, paving the way to personalized approaches.
FMT and Weight Modulation
The rationale to use FMT to induce weight loss originates from two sources. Firstly, the gut microbiome from obese individuals was found to increase energy storage as compared with lean individuals with the same caloric intake [57], even if these results have been questioned since. Secondly, since FMT from obese mice or humans into germ-free recipients is able to partly transfer weight gain [58,59,60], it is tempting to speculate that by contrast, using FMT from lean donors into overweight obese individuals could impact the receivers’ weight, thus providing a potential innovative approach in the control of weight. This unproven concept is currently debated. Indeed, a recent study observed that FMT from mice fed a normal chow diet into mice subjected to a high-fat diet induced significantly greater weight gain than that obtained by diet only [61]. Turning to humans, some pieces of evidence accumulate suggesting that FMT could induce weight gain in specific cases. Indeed, FMT from a normal weight individual (BMI = 25) to a patient suffering from anorexia nervosa led the receiver to increase (thus normalize) and stabilize her weight for 36 weeks post-FMT [62]. Furthermore, a brief report observed that a patient suffering from CD infection gained weight and further became obese after receiving FMT from her overweight daughter [63], although she followed strict diet and physical activity. Noteworthy, weight gain in these cited examples could merely reflect that FMT in malnourished patients enables the restoration of a healthy situation with a eubiotic gut microbiota and induces energy storage in patients with previously chronic condition of undernutrition, which thus might be more efficacious than in overweight subjects.
Nevertheless, the effects of FMT from lean donors have also been tested in overweight/obese patients in terms of weight modulation, and no effect on weight was seen [52, 53••]. Thus, to date there is no significant proof that FMT, even when originating from lean donors, is sufficient to induce weight loss. Most importantly, these first sets of data obtained in humans merely stimulate the need to carefully choose the donors both to avoid the transmission of communicable diseases but also to prevent weight gain. In this regard and in line with a study that showed that FMT from both mice [18] or humans [19] that underwent a bariatric procedure into germ-free recipients resulted in weight loss, de Groot et al. recently studied the effects of post-bariatric donor FMT compared with allogenic metabolic syndrome donor FMT in obese insulin-resistant males [64]. Despite the fact that post-bariatric donor FMT affects intestinal transit time in obese humans, in line with a previous animal study [13], we did not observe any effect of post-bariatric surgery donor FMT on either insulin sensitivity or weight modification. Yet and surprisingly, allogenic metabolic syndrome donor FMT worsened insulin sensitivity in all FMT-treated subjects [64]. More insight is now needed to link the correct FMT donor to the recipient in order to gain maximum therapeutic efficacy.
Factors Potentially Modulating FMT Response
Microbiota Engraftment Upon Donor FMT
First, studies have demonstrated that donor FMT induced gut microbiota composition modifications in the receiver as short as 1 week after intervention, switching the receiver’s microbiota composition towards that of the healthy donor [65]. Second, MGR increases post-FMT [52] and can even be restored [66] suggesting that FMT may act via normalizing microbiota dysbiosis, although this observation has not always been reproduced [53••]. Third, with time, gut microbiota composition continues to change after FMT. Using single nucleotide variation analyses, it was observed that whereas it still resembles that of the donor 1 month post-FMT, the dominant bacterial strains in the receiver were not always similar to those of the donor [66]. This result was further confirmed 3 months post-FMT [67]. Importantly, FMT studies have sometimes used antibiotic prior to FMT, potentially inducing confounding effects on the engraftment of the donor’s microbiota into the receiver. Interestingly, a recent study longitudinally analyzed the microbiota engraftment in different receivers without prior antibiotic use and showed a major inter-individual variability in FMT engraftment [68]. FMT as compared with placebo induced a significant modification of the receiver’s microbiota that lasted at least 3 months; however, with time, the receiver’s composition lost similarity with their donors. Furthermore, donor’s specific species only moderately increased post-FMT in all receivers yet were specific to donor-receiver pairs and higher than those observed after placebo FMT [68]. Finally, FMT induced a durable coexistence of bacterial strains present in the receivers and those transferred from the donor as well as a major strain replacement in the receiver yet variable from one receiver to the other [68] which could partially explain FMT variable responses [52, 53••]. Overall, these results suggest that FMT induces the colonization of a new microbiota that can interact with that of the receiver and differs from that of the donor despite an observed beneficial clinical effect of FMT. Furthermore, it suggests that in the future, interventions aiming at improving FMT engraftment according to the receiver or the donor’s microbiota should be undertaken in order to improve and maximize the clinical effect by increased donor bacterial engraftment (i.e., via dietary or antibiotic treatment before donor FMT).
Donor’s Microbiota Composition and Donor FMT Success
Studies evaluating the donor’s characteristics that enable an optimal response are currently ongoing. The notion of super-donor has emerged in the inflammatory bowel diseases (IBD) field. Indeed, seven out of nine patients who entered remission of their ulcerative colitis received their FMT from a single donor [69]. Likewise, an FMT study in patients with IBD using pooled feces from multiple donors finally evidenced that patients who entered remission had benefited from FMT containing the feces of one single donor thus suggested to be a super-donor [70]. Importantly, all subjects who received the FMT were on TNFα blockers, which might have also affected FMT outcome. Whether the notion of a super-donor is also valid in the metabolic field still warrants further investigations. The donor’s microbiota high diversity has been associated with good response in IBD remission [71]. Nevertheless, whether a donor is considered a good donor for every disease type remains an open question. It might well be that to induce a good response in a specific disease, the donor’s microbiota needs to be enriched in specific strains that are lowered or even absent in that specific disease. Further investigations are thus warranted.
Effects of Concomitant Drug Use and Donor FMT Effect
Concomitant presence of drugs and more specifically glucose-lowering drugs taken by the receiver is critical to be examined when using FMT to treat T2D. Metformin, the first line of antidiabetic treatment, induces a change in the composition of gut microbiota with an increase in both beneficial bacterial strains (Akkermansia muciniphila) and known pro-inflammatory strains like E. coli [72, 73]. Forslund et al. observed a shift in microbiota composition in patients with T2D with or without metformin with an increase in E. coli and a decrease in butyrate-producing bacteria, while not impacting MGR [74]. Importantly, Bäckhed’s group identified a strong metformin-related microbiota signature that in itself reproduced some of the beneficial effects of the molecule after FMT experiments in germ-free mice [75]. These data suggest that evaluating the effect of FMT from healthy donors into patients with T2D might be tricky since patients with T2D receive one or associations of glucose-lowering drugs which impact differently the gut microbiota composition as this might interfere with the colonization or engraftment of the donor’s gut microbiota after donor FMT.
Effects of Concomitant Dietary Intervention and Donor FMT Effect
The gut microbiota profile is severely impacted by both short- [76] and longer-term food intake habits, with the latter specifically linked to enterotypes [77], microbial composition, and gene richness [78]. Nevertheless, the acute modification of dietary intake also induces at least partial changes in gut microbiota composition [76, 79]. Dietary intake from receivers might most probably impact the clinical effects of FMT as discussed by Groen and Nieuwdorp [80] and demonstrated in rodent FMT experiments. Indeed, FMT from obese or lean twins into germ-free mice induced differential metabolic and body weight improvement according to the diet administrated to mouse receivers [59]. However, to date there is no standard recommendation regarding the optimal diet that would maximize the FMT therapeutic effects and bacterial strain engraftment. Moreover the donor’s diet might also impact the clinical success of FMT. A recent study using FMT from vegan lean donors enabled a switch in gut microbiota composition in the receiver towards the vegan profile of the donor [81] but with some individual variability in receivers. Importantly, this switch was not accompanied by functional modification as seen with the measured production of trimethylamine. Potentially, the absence of functional effects might originate from inter-individual variability in microbiota composition within the receivers but also by the diet consumed by the receiver, which remained similar before and after FMT [81]. It is tempting to investigate in the future whether modifying the diet after FMT could enhance FMT response yet.
Conclusion and Perspectives
The current literature suggests that FMT could improve metabolic state and in particular insulin sensitivity, yet the impact of FMT on weight loss in obese subjects needs further study. Moreover, to make relevant progress in metabolic disorders, several steps must be completed such as (i) investigating the impact of FMT in patients with various degrees of insulin resistance towards overt T2D, since the evidence to date has been gathered in male subjects with the metabolic syndrome, (ii) evaluating gender effects, (iii) determining the optimal mode of donor selection based on clinical information, (iv) identifying those able to induce a good response, and (v) elucidating which patient profile might benefit the most from FMT. Nevertheless, while donor FMT has undergone technological innovation to simplify and improve its feasibility, it remains a complex and costly procedure, due to the donor selection process which includes a broad infectious analysis as well as complex preparation and administration technics. Furthermore, while FMT has demonstrated its cost-effectiveness in different severe diseases including CD infection [82] and IBD [83], it remains to be proven whether this approach can be extended to T2D and particularly the most severe patients for whom glucose control remains above target, despite intensive medical therapy. A survey on a small study group of obese individuals recently demonstrated that a large number of them would be willing to undergo FMT if the donor was carefully selected [84], thus suggesting that this treatment could be proposed in standard of care for indications other than CD infection. If FMT successfully improves or treats T2D, this could lead to better understanding of pathophysiology and also pave the way towards other microbiota-related therapeutic developments. Indeed, the development of third-generation probiotics based on newly identified beneficial bacterial strains associated with improved metabolism in humans is also an emerging field that calls for future intensive research.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fouhy F, Ross RP, Fitzgerald GF, Stanton C, Cotter PD. Composition of the early intestinal microbiota: knowledge, knowledge gaps and the use of high-throughput sequencing to address these gaps. Gut Microbes. 2012;3(3):203–20.
Rastelli M, Knauf C, Cani PD. Gut microbes and health: a focus on the mechanisms linking microbes, obesity, and related disorders. Obes Silver Spring Md. 2018;26(5):792–800.
Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99–103.
Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BAH, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535(7612):376–81.
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–6.
Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, et al. Dietary intervention impact on gut microbial gene richness. Nature. 2013;500(7464):585–8.
Turnbaugh PJ, Bäckhed F, Fulton L, Gordon JI. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3(4):213–23.
Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222–7.
•• Aron-Wisnewsky J, Prifti E, Belda E, Ichou F, Kayser BD, Dao MC, et al. Major microbiota dysbiosis in severe obesity: fate after bariatric surgery. Gut. 2018 Jun 13. This study demonstrates that severe obesity is associated with a dramatic increased prevalence of low MGR. Bariatric surgery is able to partially restore gut microbiota dysbiosis.
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55–60.
Allin KH, Tremaroli V, Caesar R, Jensen BAH, Damgaard MTF, Bahl MI, et al. Aberrant intestinal microbiota in individuals with prediabetes. Diabetologia. 2018;61(4):810–20.
Aydin Ö, Nieuwdorp M, Gerdes V. The gut microbiome as a target for the treatment of type 2 diabetes. Curr Diab Rep. 2018;18(8):55.
Debédat J, Amouyal C, Aron-Wisnewsky J, Clément K. Impact of bariatric surgery on type 2 diabetes: contribution of inflammation and gut microbiome? Semin Immunopathol. 2019;
Cani PD, Possemiers S, Van de Wiele T, Guiot Y, Everard A, Rottier O, et al. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut. 2009;58(8):1091–103.
Dewulf EM, Cani PD, Claus SP, Fuentes S, Puylaert PGB, Neyrinck AM, et al. Insight into the prebiotic concept: lessons from an exploratory, double blind intervention study with inulin-type fructans in obese women. Gut. 2013;62(8):1112–21.
Canfora EE, van der Beek CM, Hermes GDA, Goossens GH, Jocken JWE, Holst JJ, et al. Supplementation of diet with galacto-oligosaccharides increases bifidobacteria, but not insulin sensitivity, in obese prediabetic individuals. Gastroenterology. 2017;153(1):87–97.e3.
Koutnikova H, Genser B, Monteiro-Sepulveda M, Faurie J-M, Rizkalla S, Schrezenmeir J, et al. Impact of bacterial probiotics on obesity, diabetes and non-alcoholic fatty liver disease related variables: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2019;9(3):e017995.
Liou AP, Paziuk M, Luevano J-M, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5(178):178ra41.
Tremaroli V, Karlsson F, Werling M, Ståhlman M, Kovatcheva-Datchary P, Olbers T, et al. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab. 2015;22(2):228–38.
Brandt LJ, Aroniadis OC, Mellow M, Kanatzar A, Kelly C, Park T, et al. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107(7):1079–87.
Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107(5):761–7.
Kelly CR, de Leon L, Jasutkar N. Fecal microbiota transplantation for relapsing Clostridium difficile infection in 26 patients: methodology and results. J Clin Gastroenterol. 2012;46(2):145–9.
Mattila E, Uusitalo-Seppälä R, Wuorela M, Lehtola L, Nurmi H, Ristikankare M, et al. Fecal transplantation, through colonoscopy, is effective therapy for recurrent Clostridium difficile infection. Gastroenterology. 2012;142(3):490–6.
Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2011;53(10):994–1002.
Cui B, Feng Q, Wang H, Wang M, Peng Z, Li P, et al. Fecal microbiota transplantation through mid-gut for refractory Crohn’s disease: safety, feasibility, and efficacy trial results. J Gastroenterol Hepatol. 2015;30(1):51–8.
•• van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–15. This RCT is the first to demonstrate the efficacy of FMT to cure Clostridium difficile infection.
•• Youngster I, Sauk J, Pindar C, Wilson RG, Kaplan JL, Smith MB, et al. Fecal microbiota transplant for relapsing Clostridium difficile infection using a frozen inoculum from unrelated donors: a randomized, open-label, controlled pilot study. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;58(11):1515–22. This study demonstrated for the first time the efficacy of capsulized oral fecal microbiota transplantation.
Cammarota G, Masucci L, Ianiro G, Bibbò S, Dinoi G, Costamagna G, et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41(9):835–43.
Lee CH, Steiner T, Petrof EO, Smieja M, Roscoe D, Nematallah A, et al. Frozen vs fresh fecal microbiota transplantation and clinical resolution of diarrhea in patients with recurrent Clostridium difficile infection: a randomized clinical trial. JAMA. 2016;315(2):142–9.
Quraishi MN, Widlak M, Bhala N, Moore D, Price M, Sharma N, et al. Systematic review with meta-analysis: the efficacy of faecal microbiota transplantation for the treatment of recurrent and refractory Clostridium difficile infection. Aliment Pharmacol Ther. 2017;46(5):479–93.
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108(4):478–98 quiz 499.
Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20(Suppl 2):1–26.
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66(7):987–94.
König J, Siebenhaar A, Högenauer C, Arkkila P, Nieuwdorp M, Norén T, et al. Consensus report: faecal microbiota transfer - clinical applications and procedures. Aliment Pharmacol Ther. 2017;45(2):222–39.
Cammarota G, Ianiro G, Tilg H, Rajilić-Stojanović M, Kump P, Satokari R, et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66(4):569–80.
Borody TJ, Paramsothy S, Agrawal G. Fecal microbiota transplantation: indications, methods, evidence, and future directions. Curr Gastroenterol Rep. 2013;15(8):337.
Anderson JL, Edney RJ, Whelan K. Systematic review: faecal microbiota transplantation in the management of inflammatory bowel disease. Aliment Pharmacol Ther. 2012;36(6):503–16.
Zhang F-M, Wang H-G, Wang M, Cui B-T, Fan Z-N, Ji G-Z. Fecal microbiota transplantation for severe enterocolonic fistulizing Crohn’s disease. World J Gastroenterol. 2013;19(41):7213–6.
Rossen NG, MacDonald JK, de Vries EM, D’Haens GR, de Vos WM, Zoetendal EG, et al. Fecal microbiota transplantation as novel therapy in gastroenterology: a systematic review. World J Gastroenterol. 2015;21(17):5359–71.
Lin SC, Alonso CD, Moss AC. Fecal microbiota transplantation for recurrent Clostridium difficile infection in patients with solid organ transplants: an institutional experience and review of the literature. Transpl Infect Dis Off J Transplant Soc. 2018;16:e12967.
Kassam Z, Lee CH, Yuan Y, Hunt RH. Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol. 2013;108(4):500–8.
van Beurden YH, de Groot PF, van Nood E, Nieuwdorp M, Keller JJ, Goorhuis A. Complications, effectiveness, and long term follow-up of fecal microbiota transfer by nasoduodenal tube for treatment of recurrent Clostridium difficile infection. United Eur Gastroenterol J. 2017;5(6):868–79.
Smits LP, Bouter KEC, de Vos WM, Borody TJ, Nieuwdorp M. Therapeutic potential of fecal microbiota transplantation. Gastroenterology. 2013;145(5):946–53.
Drekonja D, Reich J, Gezahegn S, Greer N, Shaukat A, MacDonald R, et al. Fecal microbiota transplantation for Clostridium difficile infection: a systematic review. Ann Intern Med. 2015;162(9):630–8.
Kelly CR, Kahn S, Kashyap P, Laine L, Rubin D, Atreja A, et al. Update on fecal microbiota transplantation 2015: indications, methodologies, mechanisms, and outlook. Gastroenterology. 2015;149(1):223–37.
Youngster I, Russell GH, Pindar C, Ziv-Baran T, Sauk J, Hohmann EL. Oral, capsulized, frozen fecal microbiota transplantation for relapsing Clostridium difficile infection. JAMA. 2014;312(17):1772–8.
Bircher L, Schwab C, Geirnaert A, Lacroix C. Cryopreservation of artificial gut microbiota produced with in vitro fermentation technology. Microb Biotechnol. 2018;11(1):163–75.
Kao D, Roach B, Silva M, Beck P, Rioux K, Kaplan GG, et al. Effect of oral capsule- vs colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: a randomized clinical trial. JAMA. 2017;318(20):1985–93.
Cheminet G, Kapel N, Bleibtreu A, Sadou-Yaye H, Bellanger A, Duval X, et al. Faecal microbiota transplantation with frozen capsules for relapsing Clostridium difficile infections: the first experience from 15 consecutive patients in France. J Hosp Infect. 2018.
Gérard C, Vidal H. Impact of gut microbiota on host glycemic control. Front Endocrinol. 2019;10:29.
de Groot PF, Frissen MN, de Clercq NC, Nieuwdorp M. Fecal microbiota transplantation in metabolic syndrome: history, present and future. Gut Microbes. 2017;8(3):253–67.
Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JFWM, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913–916.e7.
•• Kootte RS, Levin E, Salojärvi J, Smits LP, Hartstra AV, Udayappan SD, et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab. 2017;26(4):611–619.e6. This study confirmed the efficacy of FMT to improve insulin sensitivity in a larger group of patients and demonstrated the major variability of response. The authors identified that low MGR before FMT was predictive of a good response to FMT.
Everard A, Belzer C, Geurts L, Ouwerkerk JP, Druart C, Bindels LB, et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci U S A. 2013;110(22):9066–71.
Plovier H, Everard A, Druart C, Depommier C, Van Hul M, Geurts L, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23(1):107–13.
Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO, et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut. 2015.
Jumpertz R, Le DS, Turnbaugh PJ, Trinidad C, Bogardus C, Gordon JI, et al. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am J Clin Nutr. 2011;94(1):58–65.
Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101(44):15718–23.
Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341(6150):1241214.
Aron-Wisnewsky J, Clément K. The gut microbiome, diet, and links to cardiometabolic and chronic disorders. Nat Rev Nephrol. 2015.
Kulecka M, Paziewska A, Zeber-Lubecka N, Ambrozkiewicz F, Kopczynski M, Kuklinska U, et al. Prolonged transfer of feces from the lean mice modulates gut microbiota in obese mice. Nutr Metab. 2016;13(1):57.
de Clercq NC, Frissen MN, Davids M, Groen AK, Nieuwdorp M. Weight gain after fecal microbiota transplantation in a patient with recurrent underweight following clinical recovery from anorexia nervosa. Psychother Psychosom. 2019;88(1):58–60.
Alang N, Kelly CR. Weight gain after fecal microbiota transplantation. Open Forum Infect Dis. 2015;2(1):ofv004.
Donor metabolic characteristics drive effects of faecal microbiota transplantation on recipient insulin sensitivity, energy expenditure and intesti... - PubMed - NCBI [Internet]. [cited 2019 Jun 3]. Available from: https://www-ncbi-nlm-nih-gov.gate2.inist.fr/pubmed/31147381
Angelberger S, Reinisch W, Makristathis A, Lichtenberger C, Dejaco C, Papay P, et al. Temporal bacterial community dynamics vary among ulcerative colitis patients after fecal microbiota transplantation. Am J Gastroenterol. 2013;108(10):1620–30.
Seekatz AM, Aas J, Gessert CE, Rubin TA, Saman DM, Bakken JS, et al. Recovery of the gut microbiome following fecal microbiota transplantation. mBio. 2014;5(3):e00893–14.
Hamilton MJ, Weingarden AR, Unno T, Khoruts A, Sadowsky MJ. High-throughput DNA sequence analysis reveals stable engraftment of gut microbiota following transplantation of previously frozen fecal bacteria. Gut Microbes. 2013;4(2):125–35.
Li SS, Zhu A, Benes V, Costea PI, Hercog R, Hildebrand F, et al. Durable coexistence of donor and recipient strains after fecal microbiota transplantation. Science. 2016;352(6285):586–9.
Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology. 2015;149(1):102–109.e6.
Paramsothy S, Paramsothy R, Rubin DT, Kamm MA, Kaakoush NO, Mitchell HM, et al. Faecal microbiota transplantation for inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis. 2017;11(10):1180–99.
Vermeire S, Joossens M, Verbeke K, Wang J, Machiels K, Sabino J, et al. Donor species richness determines faecal microbiota transplantation success in inflammatory bowel disease. J Crohns Colitis. 2016;10(4):387–94.
Shin N-R, Lee J-C, Lee H-Y, Kim M-S, Whon TW, Lee M-S, et al. An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Gut. 2014;63(5):727–35.
Lee H, Lee Y, Kim J, An J, Lee S, Kong H, et al. Modulation of the gut microbiota by metformin improves metabolic profiles in aged obese mice. Gut Microbes. 2017:1–11.
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature. 2015;528(7581):262–6.
Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Mannerås-Holm L, et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med. 2017;23(7):850–8.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63.
Wu GD, Chen J, Hoffmann C, Bittinger K, Chen Y-Y, Keilbaugh SA, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334(6052):105–8.
Kong LC, Holmes BA, Cotillard A, Habi-Rachedi F, Brazeilles R, Gougis S, et al. Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects. PLoS One. 2014;9(10):e109434.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444(7122):1022–3.
Groen AK, Nieuwdorp M. An evaluation of the therapeutic potential of fecal microbiota transplantation to treat infectious and metabolic diseases. EMBO Mol Med. 2017;9(1):1–3.
SL et.al Effect of vegan fecal microbiota transplantation on carnitine- and choline-derived trimethylamine-N-oxide production and vascular inflammation in P... - PubMed - NCBI [internet] [cited 2019 Apr 25]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29581220
Arbel LT, Hsu E, McNally K. Cost-effectiveness of fecal microbiota transplantation in the treatment of recurrent clostridium difficile infection: a literature review. Cureus. 2017;9(8):e1599.
Zhang T, Xiang J, Cui B, He Z, Li P, Chen H, et al. Cost-effectiveness analysis of fecal microbiota transplantation for inflammatory bowel disease. Oncotarget. 2017;8(51):88894–903.
Gundling F, Roggenbrod S, Schleifer S, Sohn M, Schepp W. Patient perception and approval of faecal microbiota transplantation (FMT) as an alternative treatment option for obesity. Obes Sci Pract. 2019;5(1):68–74.
Funding
Grant supports in this field were obtained by Ministry of Health and Solidarity (Assistance Publique-Hôpitaux de Paris: to JAW/PHRC-N Drifter, to KC/PHRC Micronaria), by European Union (Metacardis to KC HEALTH-F4-2012-305312, JPI MICRODIET Grant (5290510105) to KC and MN, EU Horizon 2020 grant (LITMUS 777377) to KC and MN) and by LeDucq Foundation consortium grant (17CVD01) to KC and MN. MN is also supported by a ZONMW-VIDI grant 2013 (016.146.327). JAW and KC are part of ICAN (Institute of Cardiometabolism and Nutrition Institute).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Judith Aron-Wisnewsky declares that she has no conflict of interest.
Karine Clément is on the Scientific Advisory Board of LNC Therapeutics, France.
Max Nieuwdorp is on the Scientific Advisory Board of Caelus Pharmaceuticals, the Netherlands.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Immunology, Transplantation, and Regenerative Medicine
Rights and permissions
About this article
Cite this article
Aron-Wisnewsky, J., Clément, K. & Nieuwdorp, M. Fecal Microbiota Transplantation: a Future Therapeutic Option for Obesity/Diabetes?. Curr Diab Rep 19, 51 (2019). https://doi.org/10.1007/s11892-019-1180-z
Published:
DOI: https://doi.org/10.1007/s11892-019-1180-z