Abstract
Suboptimal glycemic control is more common among non-Hispanic Blacks (NHBs) and Hispanics than non-Hispanic Whites (NHWs). Disparities in the performance of self-care behaviors may contribute to this. To synthesize knowledge on current self-care disparities, we reviewed studies from January 2011–March 2016 that included NHWs, NHBs, and Hispanics with type 2 diabetes in the USA. Self-care behaviors included diet, exercise, medications, self-monitoring of blood glucose (SMBG), self-foot exams, and not smoking. Of 1241 articles identified in PubMed, 25 met our inclusion criteria. These studies report consistent disparities in medication adherence. Surprisingly, we found consistent evidence of no disparities in exercise and some evidence of reverse disparities: compared to NHWs, Hispanics had healthier diets and NHBs had more regular SMBG. Consistent use of validated measures could further inform disparities in diet and exercise. Additional research is needed to test for disparities in self-foot exams, not smoking, and diabetes-specific problem solving and coping.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 29 million people in the USA are diagnosed with diabetes [1], and the rate of type 2 diabetes (T2D) is substantially higher among non-Hispanic Blacks (NHBs; 13.2 %) and Hispanics (12.8 %) than among non-Hispanic Whites (NHWs; 7.6 %) [1]. Once diagnosed, NHBs and Hispanics have worse glycemic control than NHWs [1–3]. Racial and ethnic minorities with T2D are also disproportionately affected by diabetes complications and premature mortality [4]. NHBs and Hispanics with T2D have higher rates of renal disease [5], retinopathy/blindness [5, 6], and amputation [7] than NHWs.
Causes of racial/ethnic disparities in T2D are multifactorial and multilevel [4, 8]. Some diabetes disparities are rooted in biology (e.g., differences in insulin resistance and beta cell function [9]), neighborhood and community contexts (e.g., built environments limiting outdoor activity [10, 11] and access to recreational facilities [12, 13], supermarkets [14–18], and quality food [17, 19–21]), and the health care system (e.g., provider bias [22–25], differential access to [23, 24, 26–29] and quality of medical care [23, 30, 31]). Culturally, NHBs and/or Hispanics with T2D may be less likely to trust providers’ medication recommendations, have less confidence in medications, and be less likely to prioritize physical activity or weight loss than NHWs [32–37]. Furthermore, racial/ethnic minorities with T2D disproportionately experience competing family responsibilities and priorities [38], financial strain [38, 39], and daily and chronic stressors [40–42].
All of these factors contribute to the disproportionate burden of T2D on racial/ethnic minorities in the USA, but adherence to self-care may be the most readily modifiable mechanism contributing to disparities in diabetes control. Among adults with T2D, engagement in self-care activities is associated with improved glycemic control and can prevent diabetes-related complications [43–46]. The American Association of Diabetes Educators (AADE) defines seven self-care behaviors essential for successful diabetes control, including healthy eating, being active, self-monitoring of blood glucose (SMBG), taking medication, problem-solving, healthy coping, and reducing risks through not smoking and regular self-foot exams [47]. Provision of diabetes self-management education and support to initiate and sustain these behaviors is associated with improved diabetes knowledge, self-care performance, glycemic control, weight loss, quality of life, healthy coping, and lower healthcare costs [48].
Although several individual studies report racial/ethnic disparities in self-care behaviors, to our knowledge, no one has synthesized and interpreted the available disparities evidence across self-care behaviors. Therefore, we conducted a systematic review of recent studies reporting on racial/ethnic disparities in self-care behaviors among adults with T2D in the USA. We focused our review on the largest racial/ethnic groups in the USA—NHWs, NHBs, and Hispanics.
Methods
In April 2016, we searched the MEDLINE/PubMed database to identify relevant studies published in the last 5 years. Only papers published in peer-reviewed journals from January 1, 2011 to March 31, 2016 with full-text articles available were included. We used the following search: (ethnic[tw] OR ethnicity[tw] OR race[tw] OR racial[tw] OR disparity[tw] OR disparities[tw] OR difference[tw] OR black[tw] OR African?American[tw] OR hispanic[tw] OR latino[tw] OR latina[tw]) AND (self-care[tw] OR self-management[tw] OR behavior[tw] OR adherence[tw]) AND diabetes[tw] AND (full text[sb]).
Included studies (1) were original human studies research articles with adults published in English, (2) were conducted with ≥50 % US sample, (3) sampled adults with T2D defined as ≥50 % of the sample, (4) assessed adherence to self-care (diet, exercise, SMBG, hypoglycemic medications, or other self-care behaviors including the following: self-foot exams, smoking, and diabetes-related problem solving or coping), and (5) reported on a difference or presented stratified data allowing for one or more of these comparisons: NHB (Black/African American) vs. NHW (White/Caucasian), Hispanic (Hispanic/Latino/a) vs. NHB, and Hispanic vs. NHW. To identify these studies, we first excluded review articles and meta-analyses and studies not in English using the PubMed filters. We then screened the titles and abstracts of the remaining articles, excluding non-empirical papers and articles presenting results of intervention studies. Next, we excluded studies conducted with children/adolescents, and then studies in which less than 50 % of the sample was from the USA or did not have T2D except when the subsample represented more than 500 patients meeting our criteria (i.e., from the USA or with T2D). Finally, we excluded studies not assessing adherence to the self-care behaviors defined above and not evaluating the specific disparities of interest. We used the inclusion/exclusion criteria described above to screen the titles and abstracts to exclude articles before proceeding to full-text review. We then reviewed the full text of those articles not excluded on the basis of information in the title or abstract.
Results
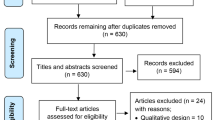
Our PubMed search resulted in 1241 articles; 126 were reviews or meta-analyses and 10 were not in English and excluded before screening. We screened 1105 titles and abstracts, and completed full-text review of 92 articles. One article was an animal study which was included in the PubMed results mistakenly [49]. One article was irretrievable for full-text review and was excluded [50]. As shown in Fig. 1, 25 articles representing 25 studies met criteria and were included in our review. Authors LSM and EB collected the following information from each eligible study: sample description, design (cross-sectional or longitudinal analysis of disparities), year(s) data were collected, racial/ethnic disparities assessed, self-care behaviors examined, and whether identified self-care discrepancies were unadjusted, adjusted, or both, and (if applicable) covariates included in adjusted analyses of disparities. Table 1 presents this information for each article. Table 2 presents the results (numerical when possible) of articles in Table 1, stratified by self-care behavior and racial/ethnic disparity(ies) explored. Table 2 presents adjusted results when available, and, when not available, unadjusted results. In both Tables 1 and 2, disparities are in the expected direction (e.g., NHBs performing less self-care than NHWs) unless otherwise denoted by the symbol R indicating the disparity is in the reverse direction (e.g., NHWs performing less self-care than NHBs).
PRISMA flow diagram depicting the exclusion and inclusion of articles. NHW non-Hispanic White, NWB non-Hispanic Black, SMBG self-monitoring of blood glucose, T2D type 2 diabetes, U.S. United States. Other self-care includes the following: self-foot care, not smoking, diabetes-specific problem solving and coping
The 25 included studies present data on 2,808,199 adults with T2D. Most studies (n = 23) examined NHB vs. NHW disparities, followed by Hispanic vs. NHW disparities (n = 16 studies) and Hispanic vs. NHB disparities (n = 12 studies). We included in our review disparities on the major self-care behaviors (i.e., diet, exercise, medication adherence, and SMBG) and other self-care, including self-foot exams, and not smoking. We sought to include diabetes-specific problem-solving and coping, but we found no papers examining racial/ethnic disparities in these constructs. Therefore, our review summarizes findings on racial/ethnic disparities in adherence to recommendations concerning diet, exercise, medications, SMBG, self-foot exams, and not smoking.
Diet
Seven articles compared diet self-care between NHB and NHW patients [51, 62••, 66•, 69, 72], NHB and Hispanic patients [60, 62••, 72], and/or NHW and Hispanic patients [62••, 63, 66•, 72]. In general, findings notably did not indicate disparities in diet. No significant disparities, unadjusted or adjusted, were noted for diet self-care between NHBs and NHWs [51, 66•, 69, 72]. There was a little evidence that Hispanics are more adherent to diet recommendations than NHBs. Hernandez et al. [60] found Hispanics scored higher on the Summary of Diabetes Self-care Activities (SDSCA) specific diet subscale (i.e., fruit/vegetable and high-fat food consumption)—though not on the general diet subscale (i.e., following a healthy eating plan) than NHBs—but this difference was not significant in adjusted analyses. Notably, there was substantial evidence of a reverse disparity between Hispanics and NHWs; all but one [72] of the studies found Hispanics adhere to healthier diets than NHWs. Orzech et al. [66•] found Hispanics report significantly higher rates of adherence to a diabetic diet plan than NHWs in unadjusted and adjusted analyses. Among patients not using insulin, Johnson et al. [62••] found Hispanics had more fruit/vegetable intake than NHWs. Kaplan et al. [63] also reported Hispanics had significantly healthier diets than NHWs.
There was substantial heterogeneity in the questions and measures used to assess dietary self-care behaviors between these groups. The only measure specifically validated to assess diet self-care among patients with diabetes was the SDSCA, which was used in two studies [51, 60]. Others used items from larger studies [62••, 63, 72] and unnamed measures [66•, 69] without evidence of prior validation. Studies evaluating disparities in diet self-care used relatively small samples with two exceptions [62••, 63]. Using the national Behavioral Risk Factor Surveillance System (BRFSS) data, Johnson et al. [62••] reported disparities between NHBs, NHWs, and Hispanics were nonsignificant after adjusting for covariates. Kaplan et al. [63] did not adjust for covariates. In short, no study presented an adjusted analysis finding less adherence to diet recommendations among minorities as compared to NHWs. Most studies found either no racial/ethnic differences in diet self-care [51, 66•, 69, 72], or found Hispanics had healthier diets than NHBs [60] or NHWs [62••, 63, 66•].
Exercise
Ten studies [51, 53••, 56, 58, 60, 62••, 63, 66•, 69, 72] assessed disparities in exercise or physical activity, with seven [53••, 56, 60, 62••, 66•, 69, 72] assessing adjusted disparities. Studies reporting NHBs performed less physical activity than NHWs showed small disparities that became nonsignificant after adjustment for covariates [53••, 58, 62••]. No studies found a significant disparity between Hispanics and NHBs. Evidence of a disparity in physical activity between Hispanics and NHWs was mixed. Two studies [66•, 72] found no disparity; two others [53••, 62••] reported small disparities that were not significant in adjusted analyses. The largest disparity between Hispanics and NHWs was identified by Kaplan et al. [63], who found that compared to NHWs, 14 % more Hispanics performed moderate to vigorous exercise three or more times per week in unadjusted analyses. The most robust examination of exercise disparities examined trends in physical activity from 2001 to 2010 among all three racial/ethnic groups [53••]. This study identified disparities between NHBs and NHWs and between Hispanics and NHWs, but noted disparities were nonsignificant after adjustment for covariates [53••]. This study provides the most compelling evaluation of physical activity disparities and found there were none. Of the seven [53••, 56, 60, 62••, 66•, 69, 72] examining adjusted disparities, only one [56] found disparities in physical activity after adjustment. Gavin et al. [56] examined differences in physical activity by race and gender and found more NHB men and Hispanic men reported regular exercise than other race/gender combinations (i.e., NHW men and women from all race/ethnic groups). Interestingly, however, NHB men had the lowest average score on the International Physical Activity Questionnaire, while Hispanic men had the highest levels of activity compared to other groups [56]. In other words, NHB men reported exercising regularly, but were participating in less rigorous exercise than other groups. Other studies with larger, representative samples either reported no disparities [62••, 72] or unadjusted evidence of reverse disparities (with either NHBs [56, 58] or Hispanics [56] reporting more physical activity than NHWs). Overall, evidence on physical activity indicates disparities are small and are not significant after adjustment for measured confounding variables.
Medication Adherence
Fourteen studies [51, 52, 54, 55, 57, 61, 64, 65, 67, 69–71, 73, 75] assessed medication adherence disparities, with twelve [51, 54, 55, 57, 61, 64, 65, 67, 69, 70, 73, 75] examining unadjusted and six [52, 54, 57, 67, 69, 71] examining adjusted disparities. Eight of the 12 studies testing unadjusted disparities found NHBs [54, 55, 57, 61, 64, 67, 75] and, separately, Hispanics [54, 55, 61, 64, 65] were less adherent in taking medications than NHWs. Three of the six studies testing adjusted disparities found NHBs [54, 67, 71] and, separately, Hispanics [54, 71] were less adherent to medications than NHWs.
Three studies found unadjusted disparities between NHBs and Hispanics [55, 61, 64]. In a representative cohort of US veterans, Egede et al. [55] linked disparities in medication adherence between NHBs, Hispanics, and NHWs to differential effects on mortality. Diabetes treatment (insulin with or without oral agents) varied across racial/ethnic minority groups, and, in turn, there was variable influence on the link between non-adherence and mortality by race [55]. Similarly, Hunt et al. [61] used data from a slightly larger cohort of US veterans, and found disparities in medication nonuse, use, and adherence. They also found nonadherent NHBs with a HbA1c <7 % had a higher mortality risk, whereas nonadherencce among NHWs only predicted mortality when HbA1c was greater than 9 % [61]. Nonadherent Hispanics and NHWs with HbA1c <7 % had a lower risk of mortality [61]. Finally, analyzing data from the National Health and Wellness Survey, Lopez et al. [64] reported Hispanics with T2D were the least adherent to medications compared to NHBs and NHWs, as well as other racial/ethnic minority groups with diabetes, and that non-adherence was associated with suboptimal glycemic control.
Overall, nearly half of the articles in this review assessed medication adherence; and, of these, the majority identified disparities between NHB, Hispanics, and NHWs. As shown in Table 2, this body of literature is consistent. Moreover, studies using nationally representative data linked disparities in medication adherence to disparities in glycemic control [64] and to disparities in mortality [55, 61].
Self-Monitoring of Blood Glucose
Eight studies [51, 53••, 59, 60, 62••, 68, 69, 74] assessed self-monitoring of blood glucose (SMBG) disparities. Four [53••, 59, 60, 69] found significant disparities after adjusting for covariates. In adjusted analyses, Quinn et al. [69] and Hernandez et al. [60] found NHBs reported higher engagement in SMBG than NHWs. The largest effect was reported by Quinn et al. [69] who found that NHBs had an adjusted odds ratio of 4.1, compared to NHWs, for excellent SMBG. Hernandez et al. [60] found NHBs reported greater adherence to SMBG than Hispanics (4.1 days versus 3.0 days based on SDSCA), and this disparity persisted after adjusting for patient-, disease-, and psycho-related factors. Yamashita et al. [74] and Johnson et al. [62••] also found Hispanics were less likely than both NHBs and NHWs to perform SMBG regularly, but only in unadjusted analyses. After adjustment for covariates, Johnson et al. [62••] found no disparities using a nationally representative data from the BRFSS. Two other studies [51, 68] did not find disparities in SMBG. Most of these were smaller studies, not examining adjusted disparities. In short, the cross-sectional data on SMBG is mixed. However, studies examining trends over time in SMBG indicate NHBs performing more [53••, 59], and Hispanics performing less [53••] SMBG than other groups. Chen et al. [53••] found improvements in SMBG for all race/ethnic groups from 2001–2010. The improvement among NHBs (54.9 to 74.8 %) was significantly larger than NHWs (58.6 to 63.0 %), reducing this disparity over time. However, Hispanics were still less likely (OR = 0.72) to engage in SMBG than NHWs, despite also increasing over time. Hardman et al. [59] examined NHWs and NHBs between 2000 and 2007 and found significant age-, SES-, and access to care-adjusted trends in personal diabetes management, which included SMBG, in all race/gender groups. The increasing trend in NHB men, in particular, was significantly larger than that of NHW men, such that the prevalence in NHB men crossed over that of NHW men.
Self-Foot Exams
Eight studies [51, 53••, 59, 60, 62••, 68, 69, 74] assessed disparities in self-foot exams, and four [53••, 59, 62••, 69] reported evidence of significant racial/ethnic disparities. Most reported that NHBs perform more regular self-foot checks than both NHWs [53••, 62••, 69] and Hispanics [62••] (among both insulin users and non-insulin users [62••]). Evidence of NHBs performing more self-foot care than NHWs was seen consistently over time. Using BRFSS data, Hardman et al. [59] reported significant increases from 2001 to 2007 in self-foot examinations as part of personal diabetes management among both NHBs and NHWs, with significantly more foot exams being performed by NHB men compared to NHW men. In contrast, Hispanics were less engaged in daily self-foot exams than both NHWs [62••, 74] and NHBs [74]. This disparity also persisted over time, with Hispanics less likely than NHWs to perform self-foot examinations in 2001 and 2010 [53••].
Not Smoking
Four studies [58, 60, 62••, 63] assessed smoking status as part of diabetes self-management. Glenn et al. [58] found NHBs are more likely to report never smoking than NHWs, but found similar rates of current smoking (each ∼29 %) in the Southern Community Cohort Study. Johnson et al. [62••] found NHWs smoked less than NHBs but this disparity did not persist in adjusted analyses. Studies consistently found that Hispanics report less smoking than both NHWs (unadjusted [63] and adjusted [62••]) and NHBs (adjusted [60]). Johnson et al. [62••] found Hispanics reported less smoking compared to NHWs, both among insulin users (adjusted odds of non-smoking; aOR = 3.2) and non-insulin users (aOR = 2.1). In the limited literature available, we found some evidence Hispanics smoke less than other groups, but little evidence of a smoking disparity between NHBs and NHWs.
The Role of Sociologic Status and Geographic Region
Several studies included in this review draw attention to the potential role of socioeconomic status (SES) and geographic variables in modifying the association between race/ethnicity and self-care behaviors. Of the 13 studies examining adjusted disparities, nine included a marker of SES (education [52, 53••, 56, 59, 60, 62••, 66•, 69], income [52, 53••, 56, 60, 62••, 66•], insurance [52, 60, 62••, 72]) and seven found at least one self-care disparity persisted despite adjustment for one or more markers of SES [53••, 56, 59, 60, 62••, 67, 69]. Two studies included region [54, 62••] or urban/rural residence [54] as covariates and both found self-care disparities persisted. Based on this evidence, differences in adherence to diabetes self-care cannot be fully explained by patients’ SES or region.
However, both SES and region do contribute to racial/ethnic disparities in self-care. Berkowitz et al. [52] conducted the most robust adjustment for SES by including food insecurity and social service use (e.g., SNAP or WIC programs). They found no adjusted disparities in adherence to medications, although other self-care behaviors were not studied. Orzech et al. [66•] found quantitative evidence of disparities in adherence to diet and exercise. Their qualitative analysis indicated having a low income contributes to high levels of food insecurity, which presented a significant barrier to dietary adherence among minority patients [66•]. Hernandez et al. [60] found Hispanics were significantly less likely than NHBs to regularly perform SMBG, and among Hispanic patients, health insurance status was a significant predictor of this behavior [60]. Income may not have a linear effect on adherence to SMBG, however. Chen et al. found those with the lowest incomes and, surprisingly, the highest incomes performed less SMBG [53••]. Egede et al. [54] found NHB and Hispanic patients had lower rates of medication adherence than NHW patients, but in adjusted analyses, rural/urban residence significantly modified the effect of race/ethnicity on medication adherence. Among NHW and NHB patients, rural residents were more adherent to medications than urban residents; in contrast, among Hispanic patients, rural residents were less adherent to medications than urban residents.
Conclusion
Recognizing the causes of racial/ethnic disparities in diabetes control are multifactorial and compounding, we reviewed and synthesized the recent literature on self-care disparities between NHW, NHB, and Hispanic adults in the USA. We found good evidence supporting disparities in medication adherence and evidence of no disparities in exercise. There was also good evidence of a reverse disparity for diet behavior (with Hispanics eating healthier diets than NHWs), SMBG (with NHBs more engaged in regular SMBG than NHWs), and some evidence of a reverse disparity in smoking (Hispanics smoking less than both NHWs and NHBs). Mixed evidence suggests NHBs may be more likely to engage in regular self-foot exams and SMBG than both NHWs and Hispanics, but more research is needed. We did not find, however, any studies examining disparities in diabetes-related problem solving or coping, which have been identified as central to self-care by the AADE. Studies examining disparities in diabetes-related problem solving and coping are needed and may further explain differential engagement in self-care behaviors.
Our review supports others’ [76–78] assertions that medication adherence may be a key contributor to disparities in clinical outcomes among adults with T2D. Findings of a disparity in medication adherence were consistent and several studies using nationally representative data linked racial/ethnic disparities in medication adherence to racial/ethnic disparities in glycemic control [64] and in mortality [55, 61]. In the decades prior to this review, national studies [37, 79] and reviews [80] have shown NHBs and Hispanics were less likely to adhere to the other self-care behaviors than NHWs. Two studies in our review examined trends over time, during 2001–2010, and indicated new evidence of narrowing and reversing disparities in some behaviors. Chen et al. [53••] reported NHBs experienced larger increases in SMBG than NHWs, narrowing and then reversing the disparity, and that Hispanics experienced larger increases in physical activity than other groups, closing the disparity with NHWs and surpassing NHBs. Using a composite measure including SMBG and self-foot exams, Hardman et al. [59] reported large increases in the performance of these behaviors among NHBs, surpassing NHWs even after adjustment for SES and access to care (Hispanics were not included in Hardman et al.’s analyses). Notably, several of the prior studies [37, 79] citing disparities in these self-care behaviors and both Chen et al. [53••] and Hardman et al. [59] used BRFSS data, thus providing additional support for the assertion that these disparties have recently reduced and/or reversed.
However, the evidence on disparities in diet and exercise behavior is weakened by the lack of consistently employed validated measures. Studies examining diet disparities often used items without citing prior validation. Only two studies used a measure specifically validated to assess diet adherence among persons with diabetes—the SDSCA. The SDSCA has been validated [81] and widely used in research, but may not provide a robust and objective assessment of diet behavior. The SDSCA asks about the frequency of eating certain foods and of following a “healthful eating plan” [81] that may be interpreted differently by patients of different races/ethnicities. Similarly, physical activity measured by the International Physical Activity Questionnaire (IPAQ) [82], which solicits a concrete specification of activity (counts of minutes spent performing different types of physical activity), yielded a finding that differed from asking participants how often they exercised [56]. The problem of measurement calls into question the validity of some studies’ findings about diet and exercise disparities. Medication adherence, on the other hand, has been assessed consistently across studies with medication possession ratios, prescription refill data, or validated scales, making it easier to synthesize and interpret disparities across studies.
Despite our thorough and systematic approach, some studies assessing disparities in adherence between NHWs, NHBs, and Hispanics may not have been identified and included in this review. We did not review any unpublished findings, so publication bias may have affected the number of studies we were able to review reporting no disparity in self-care. Second, we did not account for other racial/ethnic groups. Future research should synthesize findings on disparities with patients of other races/ethnicities in the USA. In addition, a meta-analysis was not possible given the variation in measurement across studies (with the exception of medication adherence). Finally, we did not examine disparities in accessing clinical care, but rather focused on patient-directed self-care. The Agency of Healthcare Quality and Research disparities report [31] indicates racial/ethnic disparities in obtaining HbA1c tests and provider-delivered foot and eye exams have widened. Chen et al. [53••], included in our review, also examined disparities in accessing these services from 2001 to 2010 and reported more receipt of some healthcare services among NHBs (i.e., annual foot and eye exams, diabetes self-management education) and Hispanics (i.e., annual eye exams). Notably, however, reverse disparities in accessing care may not (and have not yet) translated into reduced disparities in outcomes [83].
To our knowledge, this is the first systematic review to synthesize racial/ethnic disparities in self-care between adults with T2D in the USA. Our review suggests there is consistent and compelling evidence of disparities in medication adherence. There is also an accumulation of evidence suggesting a reverse disparity in diet and not smoking, with Hispanics eating healthier diets and smoking less than NHWs and NHBs, and a reverse disparity in self-foot exams, with NHBs performing more self-foot care than NHWs and Hispanics. We recommend future efforts to develop robust measures to assess dietary adherence and continued use of measures like the IPAQ to assess physical activity. We also recommend future studies examine racial/ethnic disparities in diabetes-related problem solving and coping that may be contributing to disparities in other self-care behaviors or may be other contributing causes of disparities in diabetes control and complications. Studies should continue assessing and adjusting for markers of socioeconomic status and region to continue to acknowledge and unpack the compounding effects of disadvantage on adherence behavior. Finally, based on the current evidence, additional efforts focused on reducing disparities in medication adherence among racial/ethnic minorities in the USA is warranted.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Center for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and its Burden in the United States. Atlanta: Department of Health and Human Services; 2014.
Herman WH, Dungan KM, Wolffenbuttel BH, et al. Racial and ethnic differences in mean plasma glucose, hemoglobin A1c, and 1, 5-anhydroglucitol in over 2000 patients with type 2 diabetes. J Clin Endocrinol Metab. 2009;94:1689–94.
Kirk JK, D’Agostino RB, Bell RA, et al. Disparities in HbA1c levels between African-American and non-Hispanic White adults with diabetes a meta-analysis. Diabetes Care. 2006;29:2130–6.
Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diabetes Rep. 2013;13:814–23.
Lanting LC, Joung IM, Mackenbach JP, et al. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients a review. Diabetes Care. 2005;28:2280–8.
Harris MI, Klein R, Cowie CC, et al. Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? A US population study. Diabetes Care. 1998;21:1230–5.
Young BA, Maynard C, Reiber G, et al. Effects of ethnicity and nephropathy on lower-extremity amputation risk among diabetic veterans. Diabetes Care. 2003;26:495–501.
Peek ME, Cargill A, Huang ES. Diabetes health disparities a systematic review of health care interventions. Med Care Res Rev. 2007;64:101S–56.
Hasson BR, Apovian C, Istfan N. Racial/ethnic differences in insulin resistance and beta cell function: relationship to racial disparities in type 2 diabetes among African Americans versus Caucasians. Curr Obes Rep. 2015;4:241–9.
Dulin-Keita A, Clay O, Whittaker S, et al. The influence of HOPE VI neighborhood revitalization on neighborhood-based physical activity: a mixed-methods approach. Soc Sci Med. 2015;139:90–9.
Sugiyama T, Howard NJ, Paquet C, et al. Do relationships between environmental attributes and recreational walking vary according to area-level socioeconomic status? J Urban Health. 2015;92:253–64.
Powell LM, Slater S, Chaloupka FJ, et al. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. Am J Public Health. 2006;96:1676–80.
Moore LV, Roux AVD, Evenson KR, et al. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34:16–22.
Morland K, Filomena S. Disparities in the availability of fruits and vegetables between racially segregated urban neighbourhoods. Public Health Nutr. 2007;10:1481–9.
Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33:S240–5.
Williams EM, Tayo BO, McLean B, et al. Where’s the kale? Environmental availability of fruits and vegetables in two racially dissimilar communities. Environ Justice. 2008;1:35–43.
Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966–2007. Prev Chronic Dis. 2009;6:A105.
Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36:74–81.e10.
Andreyeva T, Blumenthal DM, Schwartz MB, et al. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health Aff. 2008;27:1381–8.
Franco M, Roux AVD, Glass TA, et al. Neighborhood characteristics and availability of healthy foods in Baltimore. Am J Prev Med. 2008;35:561–7.
Cummins S, Smith DM, Taylor M, et al. Variations in fresh fruit and vegetable quality by store type, urban–rural setting and neighbourhood deprivation in Scotland. Public Health Nutr. 2009;12:2044–50.
Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26.
Shavers VL, Fagan P, Jones D, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102:953–66.
Smedley BD. The lived experience of race and its health consequences. Am J Public Health. 2012;102:933–5.
Van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40:I-140–51.
Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006;96:1300–7.
Fiscella K, Franks P, Doescher MP, et al. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–9.
El-Kebbi IM, Dunbar VG, Phillips LS, et al. Limited health care access impairs glycemic control in low income urban African Americans with type 2 diabetes. J Health Care Poor Underserved. 2005;16:734–46.
Shi L, Lebrun LA, Tsai J. Access to medical care, dental care, and prescription drugs: the roles of race/ethnicity, health insurance, and income. South Med J. 2010;103:509.
Johnson RL, Roter D, Powe NR, et al. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90.
2012 National Healthcare Disparities Report [article online], 2012. Available from http://archive.ahrq.gov/research/findings/nhqrdr/nhdr12/chap2a.html#diabetes. Accessed June 25 2016
Hatcher E, Whittemore R. Hispanic adults’ beliefs about type 2 diabetes: clinical implications. J Am Acad Nurse Pract. 2007;19:536–45.
Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep(Washington, DC: 1974). 2003;118:358–65.
Peek ME, Wilson SC, Gorawara-Bhat R, et al. Barriers and facilitators to shared decision-making among African-Americans with diabetes. J Gen Intern Med. 2009;24:1135–9.
Candib LM. Obesity and diabetes in vulnerable populations: reflection on proximal and distal causes. Ann Family Med. 2007;5:547–56.
Piette JD, Heisler M, Harand A, et al. Beliefs about prescription medications among patients with diabetes: variation across racial groups and influences on cost-related medication underuse. J Health Care Poor Underserved. 2010;21:349–61.
Thackeray R, Merrill RM, Neiger BL. Disparities in diabetes management practice between racial and ethnic groups in the United States. Diabetes Educ. 2004;30:665–75.
Russell BE, Gurrola E, Ndumele CD, et al. Perspectives of non-Hispanic Black and Latino patients in Boston’s urban community health centers on their experiences with diabetes and hypertension. J Gen Intern Med. 2010;25:504–9.
Jeon Y-H, Essue B, Jan S, et al. Economic hardship associated with managing chronic illness: a qualitative inquiry. BMC Health Serv Res. 2009;9:1.
Spencer MS, Kieffer EC, Sinco BR, et al. Diabetes-specific emotional distress among African Americans and Hispanics with type 2 diabetes. J Health Care Poor Underserved. 2006;17:88–105.
Morris T, Moore M, Morris F. Stress and chronic illness: the case of diabetes. J Adult Dev. 2011;18:70–80.
Wagner JA, Osborn CY, Mendenhall EA, et al. Beliefs about racism and health among African American women with diabetes: a qualitative study. J Natl Med Assoc. 2011;103:224.
American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37:S14.
Deakin T, McShane CE, Cade JE, et al. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2.
Gary TL, Genkinger JM, Guallar E, et al. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003;29:488–501.
Bolen SD, Chandar A, Falck-Ytter C, et al. Effectiveness and safety of patient activation interventions for adults with type 2 diabetes: systematic review, meta-analysis, and meta-regression. J Gen Intern Med. 2014;29:1166–76.
AADE7™ Self-Care Behaviors. The Diabetes Educator 2008;34:445–449
Standards of Medical Care in Diabetes—2016: Summary of Revisions. Diabetes Care 2016;39:S4–S5
Zangiabadi N, Mohtashami H, Hojatipour M, et al. The effect of Angipars on diabetic neuropathy in STZ-induced diabetic male rats: a study on behavioral, electrophysiological, sciatic histological and ultrastructural indices. Sci World J. 2014;2014:721547.
Sattler ELP, Lee JS, Bhargava V. Food insecurity and medication adherence in low-income older Medicare beneficiaries with type 2 diabetes. J Nutri Gerontol Geriatr. 2014;33:401–17.
Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13:335–41.
Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127:303–310.e303.
Chen R, Cheadle A, Johnson D, et al. US trends in receipt of appropriate diabetes clinical and self-care from 2001 to 2010 and racial/ethnic disparities in care. Diabetes Educ. 2014;40:756–66. This study examined trends in eight recommended diabetes clinical and self-care indicators, using BRFSS data from 2001 to 2010. Findings show that NHW and NHB experienced improvements in at least 3 indicators, while Hispanics were consistently less likely than NHW to receive or engage in most care.
Egede LE, Gebregziabher M, Hunt KJ, et al. Regional, geographic, and ethnic differences in medication adherence among adults with type 2 diabetes. Ann Pharmacother. 2011;45:169–78.
Egede LE, Lynch CP, Gebregziabher M, et al. Differential impact of longitudinal medication non-adherence on mortality by race/ethnicity among veterans with diabetes. J Gen Intern Med. 2013;28:208–15.
Gavin JR, Fox KM, Grandy S. Race/ethnicity and gender differences in health intentions and behaviors regarding exercise and diet for adults with type 2 diabetes: a cross-sectional analysis. BMC Public Health. 2011;11:533.
Gebregziabher M, Lynch CP, Mueller M, et al. Using quantile regression to investigate racial disparities in medication non-adherence. BMC Med Res Methodol. 2011;11:88.
Glenn KR, Slaughter JC, Fowke JH, et al. Physical activity, sedentary behavior and all-cause mortality among blacks and whites with diabetes. Ann Epidemiol. 2015;25:649–55.
Hardman K, Hunt KJ, Carter RE, et al. Diabetes management and vaccination rates in the Southeast United States, 2000 through 2007. Ethn Dis. 2011;21:13–9.
Hernandez R, Ruggiero L, Riley BB, et al. Correlates of self-care in low-income African American and Latino patients with diabetes. Health Psychol. 2014;33:597–607.
Hunt KJ, Gebregziabher M, Lynch CP, et al. Impact of diabetes control on mortality by race in a national cohort of veterans. Ann Epidemiol. 2013;23:74–9.
Johnson PJ, Ghildayal N, Rockwood T, et al. Differences in diabetes self-care activities by race/ethnicity and insulin use. Diabetes Educ. 2014;40:767–77. This study examined differences in diabetes self-care behaviors by race/ethnicity and insulin use, using data from the 2011 BRFSS. Racial/ethnic differences are found for each self-care activity among non-insulin users, but only for SMBG and self-foot checks among insulin users.
Kaplan SH, Billimek J, Sorkin DH, et al. Reducing racial/ethnic disparities in diabetes: the Coached Care (R2D2C2) project. J Gen Intern Med. 2013;28:1340–9.
Lopez JM, Bailey RA, Rupnow MF, et al. Characterization of type 2 diabetes mellitus burden by age and ethnic groups based on a nationwide survey. Clin Ttherapeutics. 2014;36:494–506.
Ngo-Metzger Q, Sorkin DH, Billimek J, Greenfield S, et al. The effects of financial pressures on adherence and glucose control among racial/ethnically diverse patients with diabetes. J Gen Intern Med. 2012;27:432–7.
Orzech KM, Vivian J, Huebner Torres C, et al. Diet and exercise adherence and practices among medically underserved patients with chronic disease: variation across four ethnic groups. Health Educ Behav. 2013;40:56–66. This study examined differences in adherence to diet and factors explaining self-reported daily diet and exercise practices across different ethnic groups. Food and exercise options were influenced by economic constraints, as well as ethnic and cultural familiarity with particular foods and types of activity.
Osborn CY, Cavanaugh K, Wallston KA, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16 Suppl 3:268–78.
Peek ME, Wagner J, Tang H, et al. Self-reported racial discrimination in health care and diabetes outcomes. Med Care. 2011;49:618–25.
Quinn CC, Royak-Schaler R, Lender D, et al. Patient understanding of diabetes self-management: participatory decision-making in diabetes care. J Diabetes Sci Technol. 2011;5:723–30.
Rolnick SJ, Pawloski PA, Hedblom BD, et al. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11:54–65.
Schmittdiel JA, Nichols GA, Dyer W, et al. Health care system-level factors associated with performance on Medicare STAR adherence metrics in a large, integrated delivery system. Med Care. 2015;53:332–7.
Vaccaro JA, Feaster DJ, Lobar SL, et al. Medical advice and diabetes self-management reported by Mexican-American. Black- and White-non-Hispanic adults across the United States. BMC Public Health. 2012;12:185.
Wong ES, Maciejewski ML, Liu CF. Does the association between prescription copayment increases and medication adherence differ by race? J Health Care Poor Underserved. 2013;24:1317–30.
Yamashita T, Kart CS, Noe DA. Predictors of adherence with self-care guidelines among persons with type 2 diabetes: results from a logistic regression tree analysis. J Behav Med. 2012;35:603–15.
Zhu VJ, Tu W, Marrero DG, et al. Race and medication adherence and glycemic control: findings from an operational health information exchange. AMIA Ann Symp Proc. 2011;2011:1649–57.
Heisler M, Faul JD, Hayward RA, et al. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167:1853–60.
Adams AS, Trinacty CM, Zhang F, et al. Medication adherence and racial differences in A1C control. Diabetes Care. 2008;31:916–21.
Osborn CY, Mayberry LS, Harrison BW. Medication nonadherence is a mechanism linking nonwhite race to worse glycemic control. Diabetes. 2015;64:A224.
Nwasuruba C, Khan M, Egede LE. Racial/ethnic differences in multiple self-care behaviors in adults with diabetes. J Gen Intern Med. 2007;22:115–20.
Kirk JK, Graves DE, Bell RA, et al. Racial and ethnic disparities in self-monitoring of blood glucose among US adults: a qualitative review. Ethn Dis. 2006;17:135–42.
Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50.
Booth ML, Ainsworth BE, Pratt M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;195:3508–81.
Bulger JB, Shubrook JH, Snow R. Racial disparities in African Americans with diabetes: process and outcome mismatch. Am J Manag Care. 2012;18:407–13.
Acknowledgments
This research was supported by the Vanderbilt Center for Diabetes Translation Research (DK092986-06). Dr. Mayberry is supported by K01DK106306 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Dr. Osborn is supported by K01DK087894 and R01DK100694 from NIDDK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lindsay Satterwhite Mayberry, Erin M. Bergner, Rosette J. Chakkalakal, Tom A. Elasy, and Chandra Y. Osborn declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lifestyle Management to Reduce Diabetes/Cardiovascular Risk
Rights and permissions
About this article
Cite this article
Mayberry, L.S., Bergner, E.M., Chakkalakal, R.J. et al. Self-Care Disparities Among Adults with Type 2 Diabetes in the USA. Curr Diab Rep 16, 113 (2016). https://doi.org/10.1007/s11892-016-0796-5
Published:
DOI: https://doi.org/10.1007/s11892-016-0796-5