Abstract
Type 1 diabetes (T1D) is a complex autoimmune disorder that results from the T cell-mediated destruction of the pancreatic β cells and is due to interactions between environmental and genetic factors. Although Arabs have one of the highest global incidence and prevalence rates of T1D, unfortunately, there is a dearth of information regarding the genetic epidemiology of T1D in the Arab world. Arabs share several HLA haplotypes with other ethnic groups, which confer either susceptibility or protection to T1D, but they have specific haplotypes that are distinctive from other ethnicities. Among different Arab countries, several non-HLA genes were reported to be associated with susceptibility to T1D, including CTLA4, CD28, PTPN22, TCRβ, CD3z, IL15, BANK1, and ZAP70. In Arab countries, consanguinity, endogamy, and first-cousin marriage rates are some of the highest reported worldwide and are responsible for the creation of several inbreeding communities within the Arab world that have led to an increase in homozygosity of both the HLA haplotypes and non-HLA genes associated with either protection or susceptibility to T1D among Arabs. Homozygosity reduces the HLA complexity and is expected to facilitate our understanding of the mode of inheritance of HLA haplotypes and provide valuable insight into the intricate genotype-phenotype correlations in T1D patients. In this review, based on literature studies, I will discuss the current epidemiological profile and molecular genetic risks of Arabs with T1D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 1 diabetes (T1D; MIM #222100) is the most common chronic metabolic disease in children, responsible for 5–10 % of the total cases of diabetes worldwide [1], and is suggested to increase globally by 3 % a year [2]. According to the Diabetes Atlas, 2015, more than 500,000 children developed T1D in 2015 (www.idf.org). The global annual incidence of T1D in the age group 0–14 years varies remarkably in different populations; for example, the three Nordic countries, Finland, Sweden, and Norway, are in the top three places in the list of countries with annual rates of 57.6, 43.1, and 32.8 per 100,000, respectively. In contrast, Venezuela has the lowest annual incidence rate (0.1/100,000) [3••]. The frequency of T1D varies greatly worldwide. Caucasians are considered to be at the greatest risk for T1D, with a frequency of approximately 0.4 [4], and the frequency is much lower among Asians, reaching less than 0.04 in Japanese populations [5]. Arabs have one of the highest incidence and prevalence of T1D worldwide.
T1D is characterized by immune destruction of the insulin-producing pancreatic islet β cells [6], resulting in insulin insufficiency. The cause of T1D remains unknown; however, first-degree relatives of T1D patients are at increased risk compared to the general population, and several other studies showing that approximately 10 % of patients with T1D cluster in families [7], the concordance rate in monozygotic twins for T1D is ~70 % [8, 9] and the heritability of T1D is estimated to be ~88 % [10], these factors add further evidence of a significant genetic contribution to T1D susceptibility. Nerup et al. [11] were the first to associate HLA inheritance with T1D; subsequently, scientists were able to demonstrate positive and negative correlations of particular HLA haplotypes to T1D [12–14]. HLA-DQ- and HLA-DRB1-containing genotypes were found to be responsible for approximately 50 % of the risk associated with developing T1D [15, 16]. HLA class I molecules [17] and other non-HLA genes, such as CTLA4, PTPN22, INS, and IL2RA [18], were also reported as potential predisposing genetic risk loci for T1D in different ethnic groups.
Epidemiology of Type 1 Diabetes in the Arab World
Who Is an Arab?
The Arab world is comprised of 22 Arab-speaking countries (Fig. 1), according to the World Bank latest classification for 2015 (http://data.worldbank.org). Arab regions include high-income countries, such as Bahrain, Kuwait, Oman, Saudi Arabia, Qatar, and United Arab Emirates; middle-income countries such as Algeria, Egypt, Iraq, Jordan, Lebanon, Libya, Morocco, Palestine, Somalia, Sudan, Syria, and Tunisia; and low-income countries such as Comoros, Djibouti, Mauritania, and Yemen. They occupy a large area extending from the Atlantic Ocean in the west to the Arabian Sea in the east. The Arab population is approaching 0.5 billion, and this region has been extensively exposed to many successive invaders from Turkey, Rome, and Europe, as well as traders and immigrants, which has contributed to the mixed ethnic demographic of the population.
Classification of Arab countries according to their income using the latest classification of the World Bank (Source: http://www.arabspatial.org/map)
Incidence and Prevalence in Arabs
Incidence
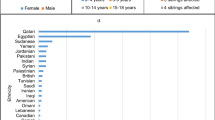
In the Middle East and North African (MENA) region, which is mostly Arabs (18 out of 21 countries), it is estimated that there are approximately 60,000 cases of T1D in children less than 15 years old. Several studies reported large variations in T1D incidence among Arab countries, ranging from a low of 2.54/100,000 in Oman [19] to a high of 29/100,000 in Saudi Arabia [20]. These variations can be attributed to the vast diversity of socioeconomic status among Arabs, wide geographical range, and differences in marriage culture practices. The reported incidence details for different Arab countries are summarized in Table 1 [21–29, 31]. According to the International Diabetes Federation (IDF)’s latest estimates for the incidence rates, 2015 (www.idf.org), Kuwait and Saudi Arabia are featured in the top 10 list of countries with the highest incidence rates in the world. Saudi Arabia and Egypt contribute almost half of the known cases in the MENA region [3••].
Does Sex Matter among People with Type 1 Diabetes in the Arab World?
Generally, T1D is characterized by a male/female ratio of close to 1, although there is a slight deviation in this ratio among different ethnic groups. Among Arab patients, the male/female ratio of patients with T1D in high-income countries is lower than that of the middle- and low-income countries (Table 1). Overall, there is a slight excess of women with T1D among Arabs within the age group 0–14 (Table 1); in contrast, patients from Europe show a slight male excess within the same age group [32]. However, there is no sex bias for T1D in Swedish patients [33].
Prevalence
The latest prevalence estimates according to the IDF atlas indicate that there are almost half a million children aged less than 15 years living with T1D worldwide (www.idf.org). Unfortunately, most of the epidemiological studies of T1D have investigated the disease incidence, few dealt with its prevalence, and most data sources do not distinguish between T1D and type 2 diabetes (T2D) in reporting prevalence. Therefore, it is difficult to separate the prevalence of the two subtypes of diabetes, which might explain the lack of data regarding the prevalence of T1D, particularly in Arab countries. A few studies have reported on T1D prevalence in children and adolescents in Algeria, Egypt, Kuwait, Saudi Arabia, and Sudan [30, 34–37], and it is not representative of the actual prevalence rates in the Arab world.
Patterson et al. [3••] have reported the number of children with T1D (in 1000s) globally, including Arab countries. They employed a comprehensive analysis of patients with T1D using variable sources of available data on the prevalence worldwide and determined the T1D prevalence among Arabs. Saudi Arabia features at the top of the list of prevalence of the disease in Arab countries, and Qatar and Kuwait show lower prevalence estimates than several of the middle-income countries, in contrast to their incidence estimates (Table 1), which are the highest in the Arab world together with Saudi Arabia. Overall, among all Arab countries, the highest observed prevalence was in the middle-income countries, headed by Egypt, Sudan, and Morocco. A complete and accurate snapshot of the epidemiological situation of diabetes will help to customize health care in regions where there is a lack of information available for T1D. With more thoughtful studies, it is anticipated that both of incidence and prevalence in Arab countries will be estimated at significantly higher levels.
Arabs are an Ideal Population in which to Study the Genetics of Type 1 Diabetes
Considering that T1D is a genetic disease, areas with a high incidence and prevalence of T1D should be a priority for genetic studies related to T1D to understand the genetic etiology of the disease and improve its prognosis. This makes the Arab world very interesting due to the distinctive genetic make-up of Arabs, resulting from highly prevalent endogamous and consanguineous marriages (10–70 %), with an extreme preference towards first-cousin marriage [38], which is still rising among Arabs and is responsible for the high prevalence of gene-based disorders in Arab countries [39]. For example, consanguineous marriage rates in Qatar increased from 41.8 to 54.5 % in just one generation, with first-cousin marriage of ~35 % [40]. Moreover, endogamous marriages approach 100 % in many Arab countries, especially in the Gulf States (Saudi Arabia, Bahrain, Kuwait, Oman, Qatar, and United Arab Emirates). In contrast, Finland and Norway, which top the list of countries for T1D prevalence, with Finland having the highest global annual incidence of T1D in children, IDF Atlas, 2015 (www.idf.org), have very low consanguineous mating rates compared to Arabs. In addition, the Norwegian [41] and Finnish [42] population show much lower frequency of first-cousin marriage, with rates of 0.2 and 0.17 %, respectively. These differences lead to variable genetic architecture between Nordics and Arabs, which likely results in a distinctive susceptibility or protective genetic profile between the two ethnic groups for T1D. Although environmental factors and socioeconomic background of patients with T1D are potentially important contributors to the variation between the two ethnic groups, considering the high disease heritability (88 %) and concordance rates in monozygotic twins (70 %), genetics of diabetes play a major role. Therefore, given the uncertainty of the etiology of T1D, high consanguinity rates across Arab countries are expected to contribute to our understanding of the molecular pathology of T1D.
Immunogenetics of Type 1 Diabetes among Arabs
The advances in sequencing technology and genotyping techniques have improved our understanding of the contribution of the HLA loci to T1D susceptibility in different ethnicities. Because the DQ and DR alleles exhibit a high degree of linkage disequilibrium (strong correlation) [15, 43], the associations of HLA alleles with T1D disease must be considered to be haplotype-specific, not allele-specific, because the haplotype context shows variable degrees of susceptibility and/or protection that are distinct from the individual alleles; for example, the DQB1*0302 allele is reported to be a critical susceptibility factor for T1D in Caucasians [44] but shows neutral and protective phenotypes when combined with other alleles in different ethnic groups (Table 2). The DQB1*0201 allele is almost universally reported to be associated with risk to T1D, including in Japanese populations [5], but in Arabs, it is associated with both susceptibility and protection, depending on the haplotype context (Table 2). Therefore, the HLA loci associated with either susceptibility or protection to T1D will be referred to in this manuscript in terms of haplotypes, not alleles.
Among Arabs, the DRB1*030101-DQB1*0201 haplotype is associated with increased susceptibility to T1D among individuals from Bahrain, Lebanon, and Tunisia [45, 48, 49], similar to Caucasians (Table 2) [46, 47], while the DRB1*040101-DQB1*0302 haplotype confers strong susceptibility in Tunisians and Bahrainis [49], shows a weak association in Caucasians [46, 47] and is protective among Lebanese [48]. However, the DRB1*040101-DQB1*050101 haplotype is protective among Lebanese but confers susceptibility to T1D in Bahrainis and is unknown in different ethnicities (Table 2). The strongest association between HLA region and T1D among Egyptians is observed with DRB1-DQA1-DQB1 haplotypes: the DRB1*0301-DRB3*0201-DQA1*0501-DQB1*0201 [51] and DRB1*04:02-DQA1*03-DQB1*03:02 [52] haplotypes confer susceptibility to T1D, and DRB1*04:03-DQA1*03-DQB1*03:02 is a resistant haplotype [52]. Both the protective and susceptible haplotypes are unique to the Egyptian population and have not been described in other ethnicities. In contrast, Moroccans seem to share the susceptible (DRB1*08-DQA1*0401-DQB1*0402) and protective (DRB1*07-DQA1*0201-DQB1*020 and DRB1*03-DQB1*02) haplotypes [53] with other Mediterranean populations, such as Algerians [63], Tunisians [49], French [54], and Spanish [47] populations. Although Arabs share several haplotypes with different ethnic groups (Table 2) [44, 46, 47, 54, 56, 58–60], they still have unique haplotypes which confer susceptibility and protection to T1D [45, 48–52, 62], which are distinctive from other ethnic groups (Table 2).
Among Arab patients with T1D, the c.49A>G polymorphism of the CTLA4 gene in the homozygous form (G/G genotype) is found to confer an increased risk for patients originating from Egypt [64, 65], Tunisia [66], Lebanon [67], and Morocco [68]. Interestingly, all Lebanese patients carrying the G/G genotype developed an early onset T1D compared to the heterozygous A/G genotype [69]. Among Tunisians, the rs3181096 gene polymorphism of the C allele of CD28 was associated with protection against T1D in the heterozygous form C/T and was significantly associated with the disease in homozygous CC carriers. Other variants in the PTPN22, TCRβ, CD3z, ZAP70 [70•], IL15, and BANK1 [71•] genes were found to be significantly associated with genetic susceptibility to T1D among Tunisians.
Homozygosity and Susceptibility to Type 1 Diabetes among Arabs
Although the pattern of inheritance of the HLA susceptibility genes is still debatable, there are studies that support mixed inheritance patterns that are either dominant or recessive [4, 6]. Others support the recessive inheritance theory [72, 73]. The DRB1*0405-DQB1*0401 haplotype is significantly higher in homozygous than in heterozygous alleles in both Japanese and Koreans patients [74], and the high-risk haplotype DRB1*04-DQB1*0302, which is found frequently in Caucasian patients, is associated with higher susceptibility to T1D in homozygous than heterozygous combinations, which has been noted in Filipino patients [75]. Among Tunisians, homozygosity for the DRB1*030101-DQB1*0201 haplotype represented the highest-risk genotype, while homozygosity for the DRB1*070101-DQB1*0201 haplotype was associated with a significantly decreased risk [50]. The frequency of the homozygous DRB1*03011-DQB1*0201 haplotype was higher in Bahraini than in Lebanese patients [48], and the homozygous haplotypes (DRB1*0301-DQB1*0201 and DRB1*0405-DQB1*0302) were strongly associated with T1D among Saudi patients [61].
The aspartic acid residue 57 of the HLA-DQB1 was found to be strongly associated with protection against T1D [76]. Haider et al. [77] studied the prevalence of the polymorphic amino acids at position 57 of the HLA-DQB1 allele in Kuwaiti children with T1D and found that the homozygous Ala/Ala is more prevalent among patients (34/55; 62 %) than heterozygotes with several combinations (19/55; 35 %). The study reported a high prevalence of homozygous Ala/Ala in different ethnic groups, such as Caucasians, African Americans, Chinese, Sardinians, and Norwegians, and it is the highest prevalence reported thus far.
To date, the studies performed to link the homozygous HLA haplotypes with susceptibility to T1D identified only 132 patients with homozygous HLA genotypes, and most of them are in Saudi Arabia (83/132); however, there is no mention in these studies of the familial relationship of the patients [61]. Endogamy is close to 100 % in Saudi Arabia and might be responsible for this frequency. Only 14 individuals had homozygous haplotypes, which were associated with protection against T1D in Lebanon and Tunisia.
Although the heterozygous combinations of several alleles and HLA haplotypes have been reported to correlate with increased susceptibility to T1D compared to homozygosity [6, 78, 79], the homozygosity of HLA haplotypes and the class I homozygosity of INS-IGF2 5ʹVNTR are responsible for the increased risk of T1D among Caucasian patients originating from Poland [80]. Because the homozygous and heterozygous HLA haplotypes in patients with T1D are in Hardy-Weinberg equilibrium, there is strong evidence suggesting that HLA susceptibility for T1D follows simple recessive inheritance [81]; however, this hypothesis has been rejected due to the excess of heterozygous rather than homozygous haplotypes in patients with T1D [79]. This is a perplexing scenario and needs further research to pinpoint the exact mode of HLA inheritance. Inbred unions among Arabs with a long familial history with T1D could provide a solution with a clearer segregation pattern of HLA haplotypes and therefore carry the potential to provide valuable insight to decode these situations.
Because approximately 50 % of the genetic risk of T1D is conferred by HLA genotypes, that leaves some 50 % which could be caused by non-HLA genes. The homozygosity of these genes, which is mostly observed in inbred communities, could provide valuable insight into disease prognosis and pathogenicity. For example, the c.49A>G polymorphism of CTLA4 gene was found to confer the highest susceptibility to T1D when observed in homozygous Arab patients from Tunisia [66], Egypt [64, 65], and Lebanon [67]. In this regard, this study will aid in discovery of novel genes and genetic variants that might be associated with T1D disease development and subsequently therapeutic development for T1D.
Interestingly, the patients in the studies reported here are mostly referred to as unrelated. The number of patients with T1D screened in this report is 1235 patients with T1D versus healthy controls of 1684 [45, 48–53, 55, 57, 62, 63, 77]. The observed homozygosity might be due to the endogamous practices among Arabs, which reach approximately 100 % in Gulf States. For example, women in Saudi Arabia are prohibited to marry men other than Arab men from the Gulf countries without special dispensation from the king (http://web.archive.org/web/20120614045804/http://travel.state.gov/travel/cis_pa_tw/tw/tw_931.html), and men require a government permit to marry a foreign woman, which is applicable to the six Gulf States. The prevalence of endogamy in other Arab countries is very high due to deep-entrenched, centuries-old traditions, which strongly favor marriage within the same Arab subcultures. Investigating the genetic etiology for T1D among even closer relatives and inbred Arab communities with high disease incidence is anticipated to provide more instructive homozygous combinations.
Genotype-Phenotype Correlation of Type 1 Diabetes
Establishing meaningful genotype-phenotype relationship for patients with T1D is important for prognosis and treatment of the disease. The ability to perform high-resolution HLA genotyping using deep sequencing [82•], screen for variants in potential candidate genes that might contribute to the pathogenicity of T1D, and map variations on the crystal structure of both susceptible HLA epitopes [83] and protective loci [84] has paved the way to sorting out the intricacies of the genotype-phenotype correlation for patients with T1D. At the present time, diagnosed patients with T1D are treated with insulin injections. However, studying inbred Arab communities may allow high-risk families to be offered heightened surveillance before onset based on carrier screening of genetic risk polymorphisms segregating in their families, or immunomodulatory prevention if such a strategy proves successful in the future.
The correlation between the different HLA genotypes and the clinical phenotypes of T1D is still enigmatic and has several challenges, including the population-specific haplotypes, geographical variation [85], etiological heterogeneity, and the complex nature of the highly polymorphic HLA loci. Therefore, the idea of reducing the complexity of HLA is quite appealing to help us to understand the HLA mode of inheritance and provide insights into the complex nature of these correlations. Consistent with this concept, the non-obese diabetic (NOD) mice, that spontaneously develop T1D and have served as a useful animal model for understanding the immunological foundation, genetic basis, and treatment, of T1D [86], are genetically homogenous (created from inbred colonies), while humans are diverse; therefore, these mice are very useful for studying the correlation between the genetic variations and clinical phenotypes of the disease. The human equivalents are those Arab inbred communities living in areas where the incidence and prevalence are very high and that are considered to be genetically homogenous. Unfortunately, one of these mines has not been earnestly tapped yet in the Arab world. However, the fear of spreading genetic diseases in Arab countries due to the prevalent consanguineous mating and endogamy has ignited a genomic revolution, which is being witnessed particularly in the Gulf region.
Genome Arabia
This Arab genomic revolution started recently with launching the “Genome Arabia” for example, Saudi Arabia started a genome project (SGP) in 2013 to sequence 100,000 Saudi genome (http://www.bbc.com/news/health-25216135). SGP aims to identify Saudi-specific genetic variants, which are linked to high incidence genetic diseases in Saudi Arabia, such as diabetes, deafness, cardiovascular, cancer, and neurodegenerative diseases. The SGP’s task is to establish a genotype-phenotype correlation for genetic disease and enable the creation of a foundation for personalized medicine. This will allow for therapeutic development for genetic disease based on the DNA blueprint of each Saudi individual, which will reduce the cost of healthcare, as the health care expenses in Saudi Arabia is related to human genetic disease tops US$30 billion annually. A few days after the SGP announcement, Qatar announced the intention to launch the Qatar Genome Project (QJP) and their plan to sequence all of their population (~300,000 citizens). Recently, they started a pilot sequencing sample of 3000 Qatari citizens (http://www.qatarbiobank.org.qa). As the SGP, the QJP, seeks for future protection of Qatari citizens from the spread of genetic diseases due to the endogamous and consanguineous marriage culture, and to facilitate future molecular diagnosis of coming generations in Qatar, where diabetes is a top priority disease in the Qatar national health strategy. The wealth of these data will, in the long-term, have global impact to understanding the molecular pathology of T1D.
Inbred Arab Communities and Rare Variant Discovery
A practical example for the benefit of studying the inbred communities among Arabs was provided by Verge et al. [87], who analyzed an inbred Bedouin Arab community living in Israel with a long history of first-cousin marriage. The family consisted of 19 close relatives affected with T1D, who carried rare predisposing haplotypes to the disease that have not been found in other families. A novel T1D susceptibility locus (IDDM17; MIM#603266) was mapped to chromosome 10 (10q25.1) [88] using linkage analysis of the 19 affected relatives. Of the 19 patients, 16 harbored a common haplotype (DRB1*0301-DQA1*0501-DQB1*0201) and an unusual haplotype, DRB1*0301-DQA1*0102-DQB1*0502 [87]. Interestingly, this common haplotype exists in different ethnic groups, including Caucasians [6, 47], and in 23 relatives within this extended family with T1D [89]. The unusual haplotype occurred disproportionately in individuals who test positive for islet cell autoantibodies. Interestingly, the Bedouin Arabs show a significantly lower frequency of T1D compared to the Israeli population; however, with the high rates of consanguinity (~50 %) and endogamy (~100 %) among Bedouin Arabs, these rare haplotypes have a much greater chance to occur, causing susceptibility to T1D. This is probably applicable not only to T1D but to all complex diseases, where “genetic simplicity” might provide significant insights into the genetic etiology of the disease through studying large multiplex families from homogenous populations.
Conclusive Versus Inconclusive Genotype-Phenotype Correlation for Type 1 Diabetes
Among Arabs, the haplotype DRB1*030101-DQB1*0201 (Table 2), which is shared with Caucasians, confers strong susceptibility to T1D in individuals from Bahrain, Lebanon, and Tunisia [45–49]. Unfortunately, in the “genetically wealthy” Arab states, where diabetes is a chronic problem, there are not enough reports to identify a conclusive genotype-phenotype correlation for patients with T1D. Nonetheless, a meaningful risk correlation could be drawn for the HLA haplotypes in Japanese for the high-risk haplotypes DRB1*0405-DQB1*0401 and DRB1*0901-DQB1*0303 [74, 90] and in Caucasians for the haplotypes DRB1*0301-DQB1*0201 and DRB1*0401-DQB1*0302 [46, 47].
However, this correlation is not straightforward for several reasons. Different haplotypes have different degrees of susceptibility and/or protection in different ethnic groups; for example, the DRB1*040101-DQB1*050101 haplotype is protective among Lebanese but susceptible or neutral among Bahrainis [48] and unknown in different ethnic groups (Table 2). This complicates the characterization of such relationships and might suggest other interfering genetic relationships, including epistatic gene interactions or genetic modifiers that might vary among different ethnic groups. Another challenge to these correlations pertains to the nature of the interaction of an uncharacterized number of genes with unidentified environmental factors, which together, cause the disease phenotype. Moreover, the incomplete penetrance and the missing heritability data may complicate such correlations, and finally, the complexity and lack of complete understanding of the mode of inheritance of HLA haplotypes still represent a barrier to the understanding of this relationship.
Looking Forward
Children with T1D represent a significant burden not only for their families but also for the healthcare systems in all countries, even for governments that have the means for treatment and intervention. Therefore, one of our priorities is to increase the predictability of the disease to improve the prognosis and treatment of T1D. This should start with a clear understanding of the nature of the relationship between the genetic variants, different HLA genotypes and the phenotypic characterizations and associated complications of T1D. However, large numbers of patients must be scrupulously characterized for their clinical presentation, disease-associated complications, and genetic background; it is likely that genome-wide association studies, using targeted deep sequencing and/or whole genome sequencing of well-characterized Arab patients, belonging to inbred communities with family history of the disease, in areas of elevated incidence and prevalence, will lead to the discovery of novel genes, rare variants, and modifier or epistatic genes. This may help in sorting out the mysteries of such correlations, leading to a clear-cut understanding of the HLA mode of inheritance and to novel insights of the molecular pathogenesis underlying T1D. Once novel-associated genetic factors of T1D have been identified, their direct contribution to the pathogenicity of T1D will still need to be validated.
Unfortunately, in the wealthy genetically Arab communities, there are rich genetic scenarios that are buried and still need to be discovered. Very few studies have dealt with the genetic risk factors that make Arabs susceptible to T1D. Policymakers and lead scientists in the Arab world, together with the international funding organizations that are interested in limiting the global spread of diabetes, should recruit more funds and carry out more field studies to discover what the genomic studies in Arab societies could offer by examining inbred Bedouin and tribal communities where disease prevalence is high. This should teach us a great deal about the genetic etiology of T1D, promoting a meaningful genotype-phenotype correlation to improve disease prognosis, increase the predictive ability for diagnosing T1D prenatally and in newborns, and provide effective molecular diagnostic approaches to the disease.
There is an urgent need to create a nationwide Arab registry for patients with diabetes, which can separate the data for both T1D and T2D and would provide the basis for further epidemiological efforts. The registry should aim to enroll each Arab family with diabetes in a single centralized database, which must be strictly regulated to protect patients’ privacy rights. It will collect patients’ information related to family history, including clinical, genetics, and epidemiological data. Establishing such a registry is important for reducing the health care cost and in saving not only Arab lives but lives on a global scale now and in the future.
Conclusion
This review article sheds light on the importance and benefits of studying the Arab population, since there is a high level of inbreeding which can result in recessive T1D risk variants having a large effect. Such populations would be useful not only for assessing the role existing T1D risk variants but also for identifying novel risk variants through linkage analysis, due to the availability of suitable sample groups to study and search for genetic determinants of T1D. Arabs represent an interesting mix of many other ethnicities across their history, which allowed for gene flow among Arabs, resulting in a more diverse gene pool. This admixture includes, but is not limited to, Caucasians, Africans, Iranians, Indians, Berbers, and Asians, and this was observed in shared susceptible and protective haplotypes. However, it appears that Arabs have a distinctive molecular genetics profile that confers either susceptibility or protection to T1D.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Daneman D. Type 1 diabetes. Lancet. 2006;367(9513):847–58. doi:10.1016/S0140-6736(06)68341-4.
DIAMOND Project Group. Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet Med. 2006;23:857–66.
Patterson C, Guariguata L, Dahlquist G, Soltesz G, Ogle G, Silink M. Diabetes in the young—a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes Res Clin Pract. 2014;103(2):161–75. doi:10.1016/j.diabres.2013.11.005. This study provides a thourough analysis of the prevalence estimates of type 1 diabetes worldwide.
Spielman RS, Baker L, Zmijewski CM. Gene dosage and suceptibility to insulin-dependent diabetes. Ann Hum Genet. 1980;44(Pt 2):135–50.
Awata T, Kuzuya T, Matsuda A, Iwamoto Y, Kanazawa Y. Genetic analysis of HLA class II alleles and susceptibility to type 1 (insulin-dependent) diabetes mellitus in Japanese subjects. Diabetologia. 1992;35(5):419–24.
Thomson G, Robinson WP, Kuhner MK, Joe S, MacDonald MJ, Gottschall JL, et al. Genetic heterogeneity, modes of inheritance, and risk estimates for a joint study of Caucasians with insulin-dependent diabetes mellitus. Am J Hum Genet. 1988;43(6):799–816.
Anaya JM, Castiblanco J, Tobon GJ, Garcia J, Abad V, Cuervo H, et al. Familial clustering of autoimmune diseases in patients with type 1 diabetes mellitus. J Autoimmun. 2006;26(3):208–14. doi:10.1016/j.jaut.2006.01.001.
Tattersall RB, Pyke DA. Diabetes in identical twins. Lancet. 1972;2(7787):1120–5.
Kyvik KO, Green A, Beck-Nielsen H. Concordance rates of insulin dependent diabetes mellitus: a population based study of young Danish twins. BMJ. 1995;311(7010):913–7.
Hyttinen V, Kaprio J, Kinnunen L, Koskenvuo M, Tuomilehto J. Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: a nationwide follow-up study. Diabetes. 2003;52(4):1052–5.
Nerup J, Platz P, Andersen OO, Christy M, Lyngsoe J, Poulsen JE, et al. HL-A antigens and diabetes mellitus. Lancet. 1974;2(7885):864–6.
Baisch JM, Weeks T, Giles R, Hoover M, Stastny P, Capra JD. Analysis of HLA-DQ genotypes and susceptibility in insulin-dependent diabetes mellitus. N Engl J Med. 1990;322(26):1836–41. doi:10.1056/NEJM199006283222602.
Pugliese A, Gianani R, Moromisato R, Awdeh ZL, Alper CA, Erlich HA, et al. HLA-DQB1*0602 is associated with dominant protection from diabetes even among islet cell antibody-positive first-degree relatives of patients with IDDM. Diabetes. 1995;44(6):608–13.
Trucco M, Dorman JS. Immunogenetics of insulin-dependent diabetes mellitus in humans. Crit Rev Immunol. 1989;9(3):201–45.
Jones EY, Fugger L, Strominger JL, Siebold C. MHC class II proteins and disease: a structural perspective. Nat Rev Immunol. 2006;6(4):271–82. doi:10.1038/nri1805.
Noble JA, Valdes AM, Cook M, Klitz W, Thomson G, Erlich HA. The role of HLA class II genes in insulin-dependent diabetes mellitus: molecular analysis of 180 Caucasian, multiplex families. Am J Hum Genet. 1996;59(5):1134–48.
Noble JA, Valdes AM, Varney MD, Carlson JA, Moonsamy P, Fear AL, et al. HLA class I and genetic susceptibility to type 1 diabetes: results from the type 1 diabetes genetics consortium. Diabetes. 2010;59(11):2972–9. doi:10.2337/db10-0699.
Polychronakos C, Li Q. Understanding type 1 diabetes through genetics: advances and prospects. Nat Rev Genet. 2011;12(11):781–92. doi:10.1038/nrg3069.
Soliman AT, al-Salmi IS, Asfour MG. Epidemiology of childhood insulin-dependent diabetes mellitus in the Sultanate of Oman. Diabet Med. 1996;13(6):582–6. doi:10.1002/(SICI)1096-9136(199606)13:6<582::AID-DIA114>3.0.CO;2-E.
Habeb AM, Al-Magamsi MS, Halabi S, Eid IM, Shalaby S, Bakoush O. High incidence of childhood type 1 diabetes in Al-Madinah, North West Saudi Arabia (2004–2009). Pediatr Diabetes. 2011;12(8):676–81. doi:10.1111/j.1399-5448.2011.00765.x.
Abduljabbar MA, Aljubeh JM, Amalraj A, Cherian MP. Incidence trends of childhood type 1 diabetes in eastern Saudi Arabia. Saudi Med J. 2010;31(4):413–8.
Kulaylat NA, Narchi H. A twelve year study of the incidence of childhood type 1 diabetes mellitus in the Eastern Province of Saudi Arabia. J Pediatr Endocrinol Metab. 2000;13(2):135–40.
Shaltout AA, Qabazard MA, Abdella NA, LaPorte RE, al Arouj M, Ben Nekhi A, et al. High incidence of childhood-onset IDDM in Kuwait. Kuwait Study Group of Diabetes in Childhood. Diabetes Care. 1995;18(7):923–7.
Shaltout AA, Moussa MA, Qabazard M, Abdella N, Karvonen M, Al-Khawari M, et al. Further evidence for the rising incidence of childhood Type 1 diabetes in Kuwait. Diabet Med. 2002;19(6):522–5.
Elamin A, Ghalib M, Eltayeb B, Tuvemo T. High incidence of type 1 diabetes mellitus in Sudanese children, 1991–1995. Ann Saudi Med. 1997;17(4):478–80.
Ajlouni K, Qusous Y, Khawaldeh AK, Jaddou H, Batiehah A, Ammari F, et al. Incidence of insulin-dependent diabetes mellitus in Jordanian children aged 0–14 y during 1992–1996. Acta Paediatr Suppl. 1999;88(427):11–3.
Kadiki OA, Roaeid RB, Bhairi AM, Elamari IM. Incidence of insulin-dependent diabetes mellitus in Benghazi, Libya (1991–1995). Diabetes Metab. 1998;24(5):424–7.
Kadiki OA, Roaeid RB. Incidence of type 1 diabetes in children (0–14 years) in Benghazi Libya (1991–2000). Diabetes Metab. 2002;28(6 Pt 1):463–7.
Vos C, Reeser HM, Hirasing RA, Bruining GJ. Confirmation of high incidence of type 1 (insulin-dependent) diabetes mellitus in Moroccan children in The Netherlands. Diabet Med. 1997;14(5):397–400. doi:10.1002/(SICI)1096-9136(199705)14:5<397::AID-DIA358>3.0.CO;2-J.
El-Ziny MA, Salem NA, El-Hawary AK, Chalaby NM, Elsharkawy AA. Epidemiology of childhood type 1 diabetes mellitus in Nile Delta, northern Egypt—a retrospective study. J Clin Res Pediatr Endocrinol. 2014;6(1):9–15. doi:10.4274/Jcrpe.1171.
Soliman AAM, Elsayed N. High incidence of childhood type 1 diabetes in Qatar between 2006 and 2011. Arch Dis Child. 2012;97:A185. doi:10.1136/archdischild-2012-302724.0639.
Karvonen M, Pitkaniemi M, Pitkaniemi J, Kohtamaki K, Tajima N, Tuomilehto J. Sex difference in the incidence of insulin-dependent diabetes mellitus: an analysis of the recent epidemiological data. World Health Organization DIAMOND Project Group. Diabetes Metab Rev. 1997;13(4):275–91.
Wandell PE, Carlsson AC. Time trends and gender differences in incidence and prevalence of type 1 diabetes in Sweden. Curr Diabetes Rev. 2013;9(4):342–9.
Al-Herbish AS, El-Mouzan MI, Al-Salloum AA, Al-Qurachi MM, Al-Omar AA. Prevalence of type 1 diabetes mellitus in Saudi Arabian children and adolescents. Saudi Med J. 2008;29(9):1285–8.
Bessaoud K, Boudraa G, Deschamps I, Hors J, Benbouabdallah M, Touhami M. Epidemiology of juvenile insulin-dependent diabetes in Algeria (Wilaya of Oran). Rev Epidemiol Sante Publique. 1990;38(2):91–9.
Elamin A, Omer MI, Hofvander Y, Tuvemo T. Prevalence of IDDM in schoolchildren in Khartoum, Sudan. Diabetes Care. 1989;12(6):430–2.
Moussa MA, Alsaeid M, Abdella N, Refai TM, Al-Sheikh N, Gomez JE. Prevalence of type 1 diabetes among 6- to 18-year-old Kuwaiti children. Med Princ Pract. 2005;14(2):87–91. doi:10.1159/000083917.
Tadmouri GO, Nair P, Obeid T, Al Ali MT, Al Khaja N, Hamamy HA. Consanguinity and reproductive health among Arabs. Reprod Health. 2009;6:17. doi:10.1186/1742-4755-6-17.
Al-Gazali L, Hamamy H, Al-Arrayad S. Genetic disorders in the Arab world. BMJ. 2006;333(7573):831–4. doi:10.1136/bmj.38982.704931.AE.
Bener A, Alali KA. Consanguineous marriage in a newly developed country: the Qatari population. J Biosoc Sci. 2006;38(2):239–46. doi:10.1017/s0021932004007060.
Magnus P, Berg K, Bjerkedal T. Association of parental consanguinity with decreased birth weight and increased rate of early death and congenital malformations. Clin Genet. 1985;28(4):335–42.
Jorde LB, Pitkanen KJ. Inbreeding in Finland. Am J Phys Anthropol. 1991;84(2):127–39.
Redondo MJ, Fain PR, Eisenbarth GS. Genetics of type 1A diabetes. Recent Prog Horm Res. 2001;56:69–89.
Erlich H, Valdes AM, Noble J, Carlson JA, Varney M, Concannon P, et al. HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: analysis of the type 1 diabetes genetics consortium families. Diabetes. 2008;57(4):1084–92. doi:10.2337/db07-1331.
Al-Harbi EM, Abbassi AJ, Tamim H, al-Jenaidi F, Kooheji M, Kamal M, et al. Specific HLA-DRB and -DQB alleles and haplotypes confer disease susceptibility or resistance in Bahraini type 1 diabetes patients. Clin Diagn Lab Immunol. 2004;11(2):292–6.
Gillespie KM, Gale EA, Bingley PJ. High familial risk and genetic susceptibility in early onset childhood diabetes. Diabetes. 2002;51(1):210–4.
Petrone A, Bugawan TL, Mesturino CA, Nistico L, Galgani A, Giorgi G, et al. The distribution of HLA class II susceptible/protective haplotypes could partially explain the low incidence of type 1 diabetes in continental Italy (Lazio region). Tissue Antigens. 2001;58(6):385–94.
Al-Jenaidi FA, Wakim-Ghorayeb SF, Al-Abbasi A, Arekat MR, Irani-Hakime N, Najm P, et al. Contribution of selective HLA-DRB1/DQB1 alleles and haplotypes to the genetic susceptibility of type 1 diabetes among Lebanese and Bahraini Arabs. J Clin Endocrinol Metab. 2005;90(9):5104–9. doi:10.1210/jc.2005-1166.
Stayoussef M, Benmansour J, Al-Irhayim AQ, Said HB, Rayana CB, Mahjoub T, et al. Autoimmune type 1 diabetes genetic susceptibility encoded by human leukocyte antigen DRB1 and DQB1 genes in Tunisia. Clin Vaccine Immunol. 2009;16(8):1146–50. doi:10.1128/CVI.00105-09.
Stayoussef M, Benmansour J, Al-Jenaidi FA, Said HB, Rayana CB, Mahjoub T, et al. Glutamic acid decarboxylase 65 and islet cell antigen 512/IA-2 autoantibodies in relation to human leukocyte antigen class II DR and DQ alleles and haplotypes in type 1 diabetes mellitus. Clin Vaccine Immunol. 2011;18(6):990–3. doi:10.1128/CVI.00073-11.
Gaber SA, Mazzola G, Berrino M, Canale L, Cornaglia M, Ghali I, et al. Human leukocyte antigen class II polymorphisms and genetic susceptibility of IDDM in Egyptian children. Diabetes Care. 1994;17(11):1341–4.
El-Amir MI, El-Feky MA, Laine AP, Harkonen T, El-Badawy O, Eltayeb AA, et al. Risk genes and autoantibodies in Egyptian children with type 1 diabetes—low frequency of autoantibodies in carriers of the HLA-DRB1*04:05-DQA1*03-DQB1*02 risk haplotype. Diabetes Metab Res Rev. 2015;31(3):287–94. doi:10.1002/dmrr.2609.
Izaabel H, Garchon HJ, Beaurain G, Biga M, Akhayat O, Bach JF, et al. Distribution of HLA class II alleles and haplotypes in insulin-dependent Moroccan diabetics. Hum Immunol. 1996;49(2):137–43.
Dubois-Laforgue D, Timsit J, Djilali-Saiah I, Boitard C, Caillat-Zucman S. Insulin-dependent diabetes mellitus in non-DR3/non-DR4 subjects. Hum Immunol. 1997;57(2):104–9.
Benseffaj N, Brick C, Atouf O, Bourhanbour DA, Sanae O, Essakalli M. Human leukocyte antigen (HLA) polymorphism and type 1 diabetes in the Moroccan population. Afr J Biotechnol. 2012;11(95):16126–31.
Keskin M, Aygun A, Pehlivan S, Keskin O, Kor Y, Balat A, et al. Trends in the frequency of HLA DR-DQ haplotypes among children and adolescents with type 1 diabetes mellitus in the Southeast Region of Turkey. J Clin Res Pediatr Endocrinol. 2012;4(4):189–92. doi:10.4274/jcrpe.768.
Fekih Mrissa N, Mrad M, Ouertani H, Baatour M, Sayeh A, Nsiri B, et al. Association of HLA-DR-DQ polymorphisms with diabetes in Tunisian patients. Transfus Apher Sci. 2013;49(2):200–4.
Chen BH, Chiang CH, Lin SR, Chao MG, Tsai ST. The influence of age at onset and gender on the HLA-DQA1, DQB1 association in Chinese children with insulin dependent diabetes mellitus. Hum Immunol. 1999;60(11):1131–7.
Cisse A, Chevenne D, Chauffert M, Ndiaye MR, Wade A, Trivin F. HLA-markers and diabetic retinopathy in the Senegalese population. Dakar Med. 1998;43(1):29–33.
Lee HC, Ikegami H, Fujisawa T, Ogihara T, Park SW, Chung YS, et al. Role of HLA class II alleles in Korean patients with IDDM. Diabetes Res Clin Pract. 1996;31(1–3):9–15.
Manan H, Angham AM, Sitelbanat A. Genetic and diabetic auto-antibody markers in Saudi children with type 1 diabetes. Hum Immunol. 2010;71(12):1238–42. doi:10.1016/j.humimm.2010.09.008.
Al-Hussein KA, Rama NR, Ahmad M, Rozemuller E, Tilanus MG. HLA-DPB1*0401 is associated with dominant protection against type 1 diabetes in the general Saudi population and in subjects with a high-risk DR/DQ haplotype. Eur J Immunogenet. 2003;30(2):115–9.
Djoulah S, Khalil I, Beressi JP, Benhamamouch S, Bessaoud K, Deschamps I, et al. The HLA-DRB1*0405 haplotype is most strongly associated with IDDM in Algerians. Eur J Immunogenet. 1992;19(6):381–9.
Mosaad YM, Auf FA, Metwally SS, Elsharkawy AA, El-Hawary AK, Hassan RH, et al. HLA-DQB1* alleles and genetic susceptibility to type 1 diabetes mellitus. World J Diabetes. 2012;3(8):149–55. doi:10.4239/wjd.v3.i8.149.
Saleh HM, Rohowsky N, Leski M. The CTLA4 -819 C/T and +49 A/G dimorphisms are associated with Type 1 diabetes in Egyptian children. Indian J Hum Genet. 2008;14(3):92–8. doi:10.4103/0971-6866.45001.
Benmansour J, Stayoussef M, Al-Jenaidi FA, Rajab MH, Rayana CB, Said HB, et al. Association of single nucleotide polymorphisms in cytotoxic T-lymphocyte antigen 4 and susceptibility to autoimmune type 1 diabetes in Tunisians. Clin Vaccine Immunol. 2010;17(9):1473–7. doi:10.1128/CVI.00099-10.
Ei Wafai RJ, Chmaisse HN, Makki RF, Fakhoury H. Association of HLA class II alleles and CTLA-4 polymorphism with type 1 diabetes. Saudi J Kidney Dis Transpl. 2011;22(2):273–81.
Bouqbis L, Izaabel H, Akhayat O, Perez-Lezaun A, Calafell F, Bertranpetit J, et al. Association of the CTLA4 promoter region (−1661G allele) with type 1 diabetes in the South Moroccan population. Genes Immun. 2003;4(2):132–7. doi:10.1038/sj.gene.6363933.
Zalloua PA, Abchee A, Shbaklo H, Zreik TG, Terwedow H, Halaby G, et al. Patients with early onset of type 1 diabetes have significantly higher GG genotype at position 49 of the CTLA4 gene. Hum Immunol. 2004;65(7):719–24. doi:10.1016/j.humimm.2004.04.007.
Ferjeni Z, Bouzid D, Fourati H, Stayoussef M, Abida O, Kammoun T, et al. Association of TCR/CD3, PTPN22, CD28 and ZAP70 gene polymorphisms with type 1 diabetes risk in Tunisian population: family based association study. Immunol Lett. 2015;163(1):1–7. doi:10.1016/j.imlet.2014.11.005. This study higlights the importance of the involvment of several SNPs in genes that are relevant to autoimmunity.
Zouidi F, Stayoussef M, Bouzid D, Fourati H, Abida O, Joao C, et al. Association of BANK1 and cytokine gene polymorphisms with type 1 diabetes in Tunisia. Gene. 2014;536(2):296–301. doi:10.1016/j.gene.2013.12.008. This study shows novel SNPs association with T1D in Tunisian Arabs.
Raum D, Awdeh Z, Alper CA. BF types and the mode of inheritance of insulin-dependent diabetes mellitus (IDDM). Immunogenetics. 1981;12(1–2):59–74.
Rich SS, Green A, Morton NE, Barbosa J. A combined segregation and linkage analysis of insulin-dependent diabetes mellitus. Am J Hum Genet. 1987;40(3):237–49.
Kawabata Y, Ikegami H, Kawaguchi Y, Fujisawa T, Shintani M, Ono M, et al. Asian-specific HLA haplotypes reveal heterogeneity of the contribution of HLA-DR and -DQ haplotypes to susceptibility to type 1 diabetes. Diabetes. 2002;51(2):545–51.
Bugawan TL, Klitz W, Alejandrino M, Ching J, Panelo A, Solfelix CM, et al. The association of specific HLA class I and II alleles with type 1 diabetes among Filipinos. Tissue Antigens. 2002;59(6):452–69.
Todd JA, Acha-Orbea H, Bell JI, Chao N, Fronek Z, Jacob CO, et al. A molecular basis for MHC class II—associated autoimmunity. Science. 1988;240(4855):1003–9.
Haider MZ, Shaltout A, Alsaeid K, Al-Khawari M, Dorman JS. High frequency of HLA-DQB1 non-Asp(57) alleles in Kuwaiti children with insulin-dependent diabetes mellitus. Hum Hered. 2000;50(4):242–6.
Platz P, Jakobsen BK, Morling N, Ryder LP, Svejgaard A, Thomsen M, et al. HLA-D and -DR antigens in genetic analysis of insulin dependent diabetes mellitus. Diabetologia. 1981;21(2):108–15.
Rotter JI, Anderson CE, Rubin R, Congleton JE, Terasaki PI, Rimoin DL. HLA genotypic study of insulin-dependent diabetes the excess of DR3/DR4 heterozygotes allows rejection of the recessive hypothesis. Diabetes. 1983;32(2):169–74.
Fendler W, Klich I, Cieslik-Heinrich A, Wyka K, Szadkowska A, Mlynarski W. Increased risk of type 1 diabetes in Polish children—association with INS-IGF2 5’VNTR and lack of association with HLA haplotype. Endokrynol Pol. 2011;62(5):436–42.
Larsen CE, Alper CA. The genetics of HLA-associated disease. Curr Opin Immunol. 2004;16(5):660–7. doi:10.1016/j.coi.2004.07.014.
Wang C, Krishnakumar S, Wilhelmy J, Babrzadeh F, Stepanyan L, Su LF, et al. High-throughput, high-fidelity HLA genotyping with deep sequencing. Proc Natl Acad Sci U S A. 2012;109(22):8676–81. doi:10.1073/pnas.1206614109. This is a useful a study to be used as a future platform for future HLA genotyping.
Roark CL, Anderson KM, Simon LJ, Schuyler RP, Aubrey MT, Freed BM. Multiple HLA epitopes contribute to type 1 diabetes susceptibility. Diabetes. 2014;63(1):323–31. doi:10.2337/db13-1153.
Siebold C, Hansen BE, Wyer JR, Harlos K, Esnouf RE, Svejgaard A, et al. Crystal structure of HLA-DQ0602 that protects against type 1 diabetes and confers strong susceptibility to narcolepsy. Proc Natl Acad Sci U S A. 2004;101(7):1999–2004. doi:10.1073/pnas.0308458100.
She JX. Susceptibility to type I diabetes: HLA-DQ and DR revisited. Immunol Today. 1996;17(7):323–9.
Kachapati K, Adams D, Bednar K, Ridgway WM. The non-obese diabetic (NOD) mouse as a model of human type 1 diabetes. Methods Mol Biol. 2012;933:3–16. doi:10.1007/978-1-62703-068-7_1.
Verge CF, Vardi P, Babu S, Bao F, Erlich HA, Bugawan T, et al. Evidence for oligogenic inheritance of type 1 diabetes in a large Bedouin Arab family. J Clin Invest. 1998;102(8):1569–75. doi:10.1172/JCI3379.
Babu SR, Bao F, Roberts CM, Martin AK, Gowan K, Eisenbarth GS, et al. Caspase 7 is a positional candidate gene for IDDM 17 in a Bedouin Arab family. Ann N Y Acad Sci. 2003;1005:340–3.
Eller E, Vardi P, McFann KK, Babu SR, Yu L, Bugawan TL, et al. Differential effects of DRB1*0301 and DQA1*0501-DQB1*0201 on the activation and progression of islet cell autoimmunity. Genes Immun. 2007;8(8):628–33. doi:10.1038/sj.gene.6364425.
Ikegami H, Kawaguchi Y, Yamato E, Kuwata S, Tokunaga K, Noma Y, et al. Analysis by the polymerase chain reaction of histocompatibility leucocyte antigen-DR9-linked susceptibility to insulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1992;75(5):1381–5. doi:10.1210/jcem.75.5.1358911.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hatem Zayed declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetics
Rights and permissions
About this article
Cite this article
Zayed, H. Genetic Epidemiology of Type 1 Diabetes in the 22 Arab Countries. Curr Diab Rep 16, 37 (2016). https://doi.org/10.1007/s11892-016-0736-4
Published:
DOI: https://doi.org/10.1007/s11892-016-0736-4