Abstract
Purpose of Review
Diabetes is a spectrum of clinical manifestations, including latent autoimmune diabetes in adults (LADA). However, it has been questioned whether LADA exists or simply is a group of misclassified type 1 diabetes (T1D) and type 2 diabetes (T2D) patients. This review will provide an updated overview of the genetics of LADA, highlight what genetics tell us about LADA as a diabetes subtype, and point to future directions in the study of LADA.
Recent Findings
Recent studies have verified the genetic overlap between LADA and both T1D and T2D and have contributed identification of a novel LADA-specific locus, namely, PFKFB3, and subtype-specific signatures in the HLA region. Genetic risk scores comprising T1D-risk variants have been shown to be a promising tool for discriminating diabetes subtypes and identifying patients rapidly progressing to insulin dependence.
Summary
Genetic data support the existence of LADA, but further studies are needed to fully determine the place of LADA in the diabetes spectrum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is a major health challenge, causing an estimated 1.6 million deaths in 2016, and is a severe economic burden, with an estimated cost of US$1.3 trillion in 2015 [1,2,3]. Diabetes is a heterogeneous disease, where the diagnostic categories range from the primarily autoimmune-related insulin-deficient type 1 diabetes (T1D), to the metabolically related type 2 diabetes (T2D). Recently, the World Health Organization (WHO) has included latent autoimmune diabetes in adults (LADA) in their classification of diabetes. According to WHO, LADA is defined as slowly evolving immune-mediated diabetes of adults, in the category of hybrid forms of diabetes [4]. LADA is characterized by the presence of autoantibodies, adult age of diagnosis, and preserved beta-cell function at the time of diagnosis. However, no consensus about diagnostic criteria exists for LADA, and it has even been questioned if LADA is a true diabetes subtype, or merely a group of misclassified T1D and T2D patients.
Phenotypically, LADA seems to be intermediate between T1D and T2D (Table 1) [5,6,7,8,9,10]. Similar to T2D, the primary risk factors for development of LADA are age, adiposity, and family history of diabetes [11, 12]. On the other hand, LADA has, like T1D, been shown to be characterized by insulitis. However, in contrast to T1D, where all islets are infiltrated [13, 14], only two-thirds of islet cells were infiltrated at the time of disease manifestation, both in LADA patients and in a rat model of LADA [15]. These morphological differences were accompanied by a shift in the presentation of immune cells and proinflammatory cytokines [15], which might explain the slower progression of insulin deficiency in LADA compared to T1D. With regard to complications, LADA patients seem most similar to T1D and are less likely to develop cardiovascular complications and early microvascular events compared to patients with T2D [16,17,18], likely due to a healthier metabolic profile. However, compared to T2D, LADA patients more often have difficulties achieving glycemic control [17, 19], resulting in worse long-term microvascular outcomes [17, 18].
In order to verify LADA as a diabetes subtype, and to improve the understanding of the pathophysiology of LADA, it is vital to identify markers that can assist in the diagnoses of LADA and separate LADA from other diabetes subtypes. Discrimination of diabetes subtypes and stratification with respect to disease progression is important, as these aspects have implications for choice of treatment and well-being of patients. Recent studies have indicated that markers of low-grade inflammation, including soluble tumor necrosis factor receptor type II (sTNFRII), could help differentiate between LADA, T1D, and T2D [20]. Also, the secretion pattern of proinsulin has been suggested to differ between diabetes subtypes [21]. However, these markers, as well as autoantibodies such as glutamic acid decarboxylase autoantibodies (GADA) [22], are dependent on timing in clinical sampling and disease progression. In contrast, genetic markers are stable over time and are not confounded by lifestyle, disease state, or medication and can easily be obtained from a blood sample. Hence, genetics have the potential to inform about pathogenic pathways characterizing LADA compared to T1D and T2D and maybe even to stratify LADA patients by identifying those with rapid decreasing beta-cell function who should be prioritized for early intervention.
This review provides an overview of the current knowledge of the genetics of LADA, discusses what genetics tells us about LADA as a diabetes subtype, and points to future directions in the genetic research of LADA.
Genetics of Latent Autoimmune Diabetes in Adults
Since the first reports of association between variants in the HLA region and T1D in the 1970s [23, 24], genetic predisposition to diabetes has been studied intensively. To date, more than 60 risk-associated loci have been identified for T1D [25,26,27], and for T2D more than 400 [28]. Increasing evidence is pointing towards a partial genetic overlap between T1D and T2D [29,30,31,32,33]. One of the most well-documented loci that are associated with both T1D and T2D is GLIS3, which encodes the GLIS family zinc finger 3. The functional link between genetic variation in GLIS3 and diabetes has been suggested to be fragile beta-cells, with increased apoptosis and senescence [34, 35]. A recent study assessed linkage disequilibrium (LD)-score regression and found positive genetic correlation between T1D and T2D. To ensure that the correlation between T1D and T2D was not explained by misclassified patients, these findings were replicated in restricted case groups. T1D was restricted to individuals with onset below the age of 17, treated with insulin from diagnosis, and with a body mass index (BMI) ≤ 30, whilst T2D was restricted to patients negative for GADA and treated without insulin for at least 1 year after diagnosis [32•]. The study further highlighted that particular T2D-relevant processes and genetic risk factors contribute to risk of T1D, likely via beta-cell stress by affecting islet function and through affecting insulin resistance [32•]. Taken together, these genetic studies favor the presentation of diabetes as a spectrum of phenotypes with partly overlapping etiology and genetic predisposition and adds to the emerging clinical picture of T1D and T2D being heterogeneous phenotypes [19, 36].
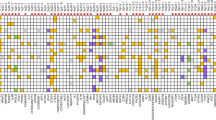
The precise positioning of LADA within this spectrum is still unclear. Progress in understanding the genetic contribution to LADA is less advanced than for T1D and T2D. Until recently, genetic studies of LADA were candidate-gene studies assessing T1D or T2D-associated variants. Due to small sample sizes, these studies had limited statistical power, and the findings were likely contaminated with false-positives. Within the last 5 years, larger samples of LADA patients have been compiled by collaboration across research groups, and a genome-wide association study (GWAS) has been conducted as well as a few larger candidate-gene studies and a meta-analysis (Table 2). Hence, a clearer picture of the genetic predisposition to LADA is starting to emerge. The best-validated genetic loci associated with LADA are described below (Table 3).
The Human Leukocyte Antigen Complex
Variation within the human leukocyte antigen (HLA) region remains the strongest genetic risk factor for T1D, and this locus contributes at least 40% of the heritability of T1D, primarily through variation in the HLA-DR and HLA-DQ genes [25, 26, 37]. It has consistently been shown that the frequency of HLA-risk alleles correlates with age at diagnosis of T1D, whereas the opposite has been shown for protective HLA alleles [33, 38].
The HLA region is also the strongest genetic predictor of LADA [5, 8, 39,40,41, 42•, 43••], with the strongest association shown in LADA patients with high GADA levels or LADA patients positive for two autoantibodies, GADA and insulinoma-associated antigen-2 autoantibodies (IA2A) [8, 42•, 43•, 44]. Compared to T1D, the effect sizes for T1D HLA-risk haplotypes in LADA are smaller, whilst the impact of T1D HLA-protective haplotypes is greater in LADA [8, 37, 39, 41•, 43•, 45••]. Interestingly, these differences are apparent, even when comparing LADA patients to T1D patients diagnosed in adulthood [8, 44]. Recent studies have indicated that the pattern of associated alleles in the HLA region might differ between T1D and LADA. In a stepwise conditional analysis, T1D was associated with independent signals for the HLA-DQB1*0302 allele, and in the HLA class I genes HLA-B*39, HLA-A, and HLA-G. LADA on the other hand showed no HLA class I association that was independent of the HLA-DQB1*0302 association [45••]. This observation is in line with reports of HLA class I markers, including (i) HLA-B*39 is associated with younger age at onset in T1D [46, 47]; (ii) HLA-B*3906 transgenic NOD mice show accelerated development of T1D; and (iii) HLA-B*3906 has been shown to mediate the development of CD8+ T cells, essential for T1D onset [48]. These HLA class I markers are thereby likely to contribute less to the genetic susceptibility to LADA.
The functional link between variation in the HLA region and autoimmune diabetes is through the role of the HLA proteins in the presentation of foreign- and self-derived antigens to immune cells, which activate the immune system and control T cell selection [49]. Genetic variation, particularly in HLA-DQB1, has been suggested to affect the affinity and stability of the antigen binding. Less efficient binding of pancreatic antigens might cause autoreactive T cells to escape negative selection in the thymus, which could induce an autoimmune reaction towards pancreatic beta-cells [50, 51].
Protein Tyrosine Phosphatase Non-Receptor Type 22
Protein tyrosine phosphatase non-receptor type 22 (PTPN22) is also a validated T1D-associated locus [25, 26, 52]. The association between the minor T-allele of the PTPN22 rs2476601 variant and LADA has been assessed in a number of smaller candidate-gene studies, and significant association was shown in the majority [8, 40, 42•, 53,54,55]. Recently, the association was replicated in a relatively large meta-analysis including 3187 patients with LADA [55] and a LADA GWAS comprising 2634 LADA patients [43••]. Compared to the reported effect size in T1D patients with an odds ratio (OR) of 1.95 (95% confidence interval (CI), 1.86–2.04) [52], the estimated effect in LADA patients is smaller, namely, an OR of 1.62 (95% CI, 1.48–1.78) [56]. Notably, the effect size has been suggested to be greater in LADA patients with high GADA levels [53] or positive for both GADA and IA2A [42•].
PTPN22 encodes a lymphoid tyrosine phosphatase, which is involved in negative selection of thymocytes and regulation of peripheral T cell activation [57,58,59]. The T1D-associated T-allele of the PTPN22 rs2476601 variant has been shown to be associated with reduced elimination of naïve B cells expressing autoreactive antibodies in the bone marrow and reduced negative selection of regulatory T cells in the thymus [60, 61], which may induce autoimmunity and thereby predispose to T1D and LADA.
Insulin
Insulin (INS) is also an established T1D-associated locus, estimated to account for around 10% of T1D heritability [25, 26, 62]. The INS rs689 T1D-associated allele is in near-perfect LD with the short class I variable number of tandem repeats (VNTR) in the INS promoter [63]. Association of the variant was initially reported with LADA in candidate-gene studies [40, 42•, 64] and subsequently confirmed in a relatively large meta-analysis [56], and in the LADA GWAS [43••]. The LADA-INS association has been suggested to be stronger in LADA patients positive for both GADA and IA2A [42•]. For T1D, association has been reported for different INS variants, but for rs689 or rs3842753, which are in high LD with each other, the reported effect sizes in T1D patients are greater than the estimated effect reported for LADA patients of an OR (95% CI) of 1.39 (1.29–1.48) [27, 56, 65••]. Functionally, the INS promoter VNTR has been shown to affect INS expression; hence, the T1D-associated class I VNTR is associated with lower INS expression in thymus [66, 67]. The lower level of insulin in the thymus reduces the deletion of autoreactive T cells targeting insulin antigens and thereby increases the risk of autoimmune destruction of insulin-producing beta-cells [68, 69].
The SH2B Adaptor Protein 3
In a recent candidate-gene study, and later in a GWAS, variants in the SH2B adaptor protein 3 (SH2B3) locus were found to be associated with LADA with an OR (95% CI) of 1.28 (1.19–1.38), again with a suggested larger effect size in LADA patients positive for both GADA and IA2A [42•, 43••]. This locus has also consistently been associated with T1D, with an effect size similar to the one reported for LADA [25, 26, 62]. The T1D-associated T-allele of the SH2B3 rs3184504 missense variant has been suggested to be the causal variant in the locus. This variant is in high LD with the lead SNPs identified in LADA-association studies (rs17696736 and rs7310615) [42•, 43••] and is predicted to disrupt the subcellular localization and function of the SH2B3 gene product [70]. However, it is a complex genomic region that is associated with a range of different diseases and conditions [71].
In humans, SH2B3 encodes the lymphocyte adaptor protein LNK, which is widely expressed across different tissues [72] and is involved in transduction and regulation of growth factor and cytokine receptor-mediated signaling [73]. Lack of LNK function in humans is linked to a range of phenotypes including triggered autoimmune processes [74], and in mice, Sh2b3 knock-out leads to adipose inflammation, as well as impaired glucose tolerance and insulin response [75]. These changes might predispose to T1D as well as LADA.
Transcription Factor 7-Like 2
Transcription factor 7-like 2 (TCF7L2) remains the strongest common genetic risk factor for T2D with an OR (95% CI) of 1.37 (1.35–1.39) [28, 76]. Based on functional studies and trans-ethnic association analyses, the intronic rs7903146 variant is thought to be the major causal variant in the TCF7L2 locus [28, 77, 78].
In candidate-gene studies, the TCF7L2 rs7903146 variant has shown association with LADA, despite some discrepancy between studies [41, 42•, 79, 80], and the association has been suggested to depend on GADA level, being strongest in LADA patients with low GADA levels [80, 81]. Association was not replicated in the LADA GWAS [43••]; however, in a recent meta-analysis comprising an even larger sample of LADA patients, association was reported with an OR (95% CI) of 1.19 (1.00–1.40) [56]. This meta-analysis revealed high heterogeneity between samples, supporting the observations from the GWAS, where the LADA-TCF7L2 association was shown to be highly dependent on selection of the control group. Hence, choosing a selected normal glucose-tolerant control population resulted in a stronger association signal than choosing a population-based control group. Moreover, the origin of the LADA patients might also affect the result, with strongest association signal observed among LADA patients from Northern Europe [43••].
Discrepant findings have also been reported with respect to the relationship between TCF7L2 and T1D. Most studies show no association between variation in TCF7L2 and T1D, neither in childhood nor in adult-onset T1D [30, 80, 82,83,84,85], and no association with age at onset of T1D [30, 82]. However, in a recent study assessing 8967 patients with T1D and 6076 control subjects, the TCF7L2 rs7903146 variant was associated with T1D, notably with opposite direction of effect to that reported for T2D [32•]. Association between the TCF7L2 variant and presence of autoantibodies has also been assessed. In children with T1D parents, the T2D-associated TCF7L2 allele was not associated with development of islet autoantibodies [84]. However, in 810 newly diagnosed T1D patients, association was observed between the T2D-associated TCF7L2 alleles and a milder autoimmune presentation at diagnosis in patients 12 years or older [86]. These T2D-associated TCF7L2 alleles have also been associated with slower progression of T1D, indicated by higher C-peptide levels [33, 86] and lower glucose levels during an oral glucose tolerance test [86]. Hence, TCF7L2 might affect the pathophysiological presentation of T1D and predispose to a milder autoimmune response as well as milder metabolic impact in T1D patients. Taken together, variation in TCF7L2 seems to play a role in disease presentation across the spectrum of diabetes subtypes.
The TCF7L2 gene product is a transcription factor and has been shown to regulate transcription of the proglucagon gene, which yields the product GLP-1 [87], to mediate GLP-1 induced beta-cell proliferation [88], and to affect insulin secretion [89,90,91]. In adipose tissue, rs7903146 has been shown to affect adipocyte development [92], as well as glucose and fatty acid metabolism [93]. Moreover, carriers of the rs7903146-risk genotype have been shown to have a reduced number of beta-cells [94]. Taken together, these alterations likely affect glucose homeostasis, adipose-tissue homeostasis, and risk of diabetes.
6-Phosphofructo-2-Kinase/Fructose-2,6-Biphosphatase 3
In the LADA GWAS, a novel signal was identified in the 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 (PFKFB3) locus on chromosome 10, where the rs1983890 C-allele was genome-wide significantly associated with LADA with an OR (95% CI) of 1.16 (1.14–1.32) [43•]. This genomic region is not associated with T2D [28] but harbors two well-established T1D-associated loci, namely, IL2RA and PRKCQ [25, 26]. However, the LADA signal is independent of these two T1D signals, as the LADA association remained significant when conditioning on the T1D-associated lead SNPs. DEPICT analysis indicated that PFKFB3 was the most likely functional candidate explaining the association signal in LADA [43•]. PFKFB3 encodes 6-phosphofructo-2-kinase/fructode-2,6-biphosphatase 3 and is a strong functional candidate to explain the signal. PFKFB3 is involved in regulation of glycolysis and insulin signaling [95] and is highly expressed in adipose tissue where it is a master regulator of adipocyte nutrient metabolism [96]. In mice, loss of PFKFB3 function in adipose tissue results in high-fat diet-induced systemic insulin resistance and inflammation of the adipose tissue [97], whereas PFKFB3 over-expression was protective for these conditions [98]. PFKFB3 is also involved in a highly conserved HIF1 α/PFKFB3-signaling pathway, which protects against cellular stress, including beta-cell stress [99, 100]. This pathway is activated in islets from adult T1D patients, with a fivefold increased PFKFB3 expression, where it delays cytokine-induced beta-cell death [100]. The exact role of the PFKFB3 locus in LADA pathogenesis remains to be determined. It could be hypothesized that LADA-associated variation in the PFKFB3 locus increases the activity of PFKFB3 and thereby induce the HIF1 α/PFKFB3-signaling pathway to delay beta-cell death, causing later and milder onset compared to childhood onset T1D. However, in a study of T1D and LADA patients, the PFKFB3 rs1983890 variant was neither associated with age at onset nor C-peptide level [33].
Genetic Risk Scores and Characterization of Diabetes Subtypes
Instead of assessing genetic variants separately, they can also be combined in genetic risk scores (GRS). The use of a GRS is likely to be a more promising way to translate genetic findings into prediction, identification of diabetes subtypes, and perhaps even into personalized treatment.
Genetic Risk Scores in Type 2 Diabetes
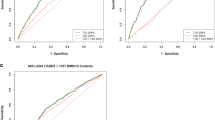
For T2D, GRS comprising different numbers of risk variants have been tested in their ability to predict the disease. However, the benefit from a GRS, compared to easily available factors such as age, BMI, sex, and family history, is very limited for T2D [101]. Most recently, a polygenic risk score comprising 7 million variants has been shown to identify 3.5% of the population at > 3 threefold increased risk of T2D. However, the screening performance of this score is poor with an area under the curve (AUC) of just 0.73 [102] and an estimated detection rate of only 13%, with a false discovery rate of 5%. These statistics mean that the score would incorrectly identify 5% of unaffected individuals as having T2D, while only correctly identifying 13% of individuals truly having T2D [103, 104]. Moreover, a T2D GRS has very limited power to discriminate T2D from T1D [42•, 105].
Genetic Risk Scores in Type 1 Diabetes
In contrast, a T1D GRS is far more powerful for prediction and discrimination of diabetes subtypes, due to the larger effect estimates of T1D-associated variants compared to T2D-associated variants. Hence, a score comprising 67 T1D-associated variants and including HLA interaction terms has an AUC of 0.93 for discriminating T1D from controls [65••] and is in UK Biobank data able to correctly identify 83% of T1D patients, and at the same time correctly identifying 89% of the background population as unaffected. Similarly, when discriminating T1D from T2D, the GRS correctly identified 83% of patients with T1D and correctly identified 88% of the T2D patients [65••]. Moreover, a T1D GRS comprising 30 variants has been shown to predict insulin deficiency among T1D and T2D patients diagnosed at 20–40 years of age [105], and among GADA-positive T2D patients, to identify those rapidly progressing to insulin treatment [106••]. Hence, among GADA-positive T2D patients, those with a high T1D GRS had a probability of 48% to require insulin treatment within 5 years of diagnosis, whereas those with the lowest score had a probability of just 18%. Yet, it should be noted that a probability of 48% among GADA-positive T2D patients with a high GRS means that the majority of these patients will not require insulin after 5 years [106••], and hence, the GRS is not readily clinically relevant. Interestingly, the probability of insulin treatment for GADA-positive individuals with a low T1D GRS is higher than the probability for insulin treatment for GADA-negative T2D patients, who have 7% risk regardless of the T1D GRS [106••]. This supports the notion that even the least T1D-like LADA patients differ from T2D patients.
Genetic Risk Scores in Latent Autoimmune Diabetes in Adults
In LADA patients, combined analyses of T1D- and T2D-associated variants showed enrichment of association for both sets of loci [43•], supporting the results from single-variant analyses of a genetic overlap between LADA and T1D as well as between LADA and T2D. In addition, LD-score regression supports a direct genetic correlation between LADA and T1D, and the key role of autoimmunity in LADA is further supported by genetic correlation between LADA and additional autoimmune conditions. LD-score regression also supports the genetic overlap between LADA and T2D, by direct genetic correlation between LADA and T2D, but also indicated by correlation between LADA and other metabolic phenotypes, including BMI [43•].
GRS have also been assessed in LADA patients. With respect to a T1D GRS comprising 69 variants, the AUC for LADA compared to control subjects was 0.67, whereas the AUC for a T2D GRS comprising 67 variants was 0.57. Hence, both scores have low predictive value for LADA. However, it was shown that the mean value of both scores for LADA patients differed significantly from both T1D and T2D patients as well as control subjects [42•], again indicating that both T1D and T2D risk variants are enriched among LADA patients. Moreover, the scores also differed according to the number of autoantibodies among the LADA patients; LADA patient only positive for GADA had a lower T1D score, and a higher T2D score than LADA patients positive for both GADA and IA2A [42•]. Clinical application of the T1D GRS in its current form for distinguishing diabetic subtypes seems limited as the distribution of the T1D GRS within T1D, T2D, LADA, and controls overlapped between all groups [42•]. However, a more advanced version of the T1D GRS [65••] might perform better in this discrimination. Of note, the distribution of the T1D GRS within LADA patients did not support a bimodal distribution of the T1D GRS, which might be expected if the group of LADA patients consisted only of misdiagnosed T1D and T2D patients.
Taken together, studies of GRS support the notion that both T1D-associated and T2D-associated variants contribute to the genetic susceptibility to LADA. However, to firmly classify LADA, as either a diabetes subtype distinct from both T1D and T2D, or a group of misdiagnosed T1D and T2D patients, further research is required.
Conclusions
Genetic studies seem to support the notion that diabetes is more than two easily separated groups of patients with either T1D or T2D, in line with what has been shown based on clinical data [19, 36].
Based on current knowledge, LADA seems to share genetic predisposition with both T1D and T2D (Tables 1 and 3). For HLA, PTPN22, INS, SH2B3, and TCF7L2, the variants associated with LADA overlap with those associated with either T1D or T2D, although the effect sizes are in general smaller for LADA.
Pathway and tissue enrichment analyses [43••], as well as functional observations, indicate a key role of the immune system in the pathogenesis of LADA. T1D-associated variants are likely linked to the autoimmune process in LADA, and T2D-associated variants likely add to the genetic burden increasing the susceptibility to LADA, thereby contributing to the intermediate phenotype of LADA. Recent studies have contributed interesting insights into the genetics of LADA. These findings include (i) an independent LADA GWAS signal, namely, PFKFB3 [43••], which might contribute to the slower disease progression in LADA compared to T1D, and (ii) HLA class I loci only showing independent association to T1D, and not LADA, when conditioning on the main HLA class II risk variants [45••]. These findings indicate that LADA differs genetically from T1D.
It has been heavily debated whether LADA truly is an independent subtype of diabetes, intermediate between T1D and T2D, a subtype of T1D, or whether it is a group of primarily T1D patients and some T2D patients with a false-positive autoantibody results. Genetic findings can be interpreted to support the existence of LADA. Hence, even among the most T1D-like LADA patients with high GADA levels or multiple autoantibodies, the HLA-risk alleles are not as common, and the T1D GRS is lower, when compared to T1D children [8, 42•], indicating that these patients are not simply misclassified T1D patients. Similarly, the most T2D-like LADA patients with low GADA levels, or only single autoantibody positivity, differ from T2D patients with a lower T2D-genetic load [42•], and a greater probability for insulin treatment [106••].
Interestingly, the hypothesis that LADA is simply a mixture of T1D patients and T2D patients with a false-positive autoantibody test was investigated in a study assessing similarities and differences in HLA association between T1D and LADA. A cohort of 714 T1D patients and 714 T2D patients were randomly sampled to generate a LADA sample, which was compared to 2219 control subjects. Analyses demonstrated that the generated LADA sample was much more T1D-like than the real LADA cohort with respect to HLA association [45••]. Additional studies assessing a simulated against a real cohort of LADA patients should test these aspects further. Moreover, to firmly establish the nature of LADA and to determine if it can be separated from T1D and T2D, large well-powered genetic-association studies assessing separate variants and GRS in LADA patients with a large spectrum of age at diagnosis, as well as numbers and levels of autoantibodies, are also warranted. Particularly, with optimization, GRS could become relevant both in terms of timely diagnosis, and for determination of disease management in LADA. In the future, partitioned GRS capturing specific intermediary disease-related phenotypes or pathways driving an individual’s disease progression might also be generated. Genetic clustering has already been used to characterize clusters of different underlying etiologies within T2D [28, 107], and similar analyses in a suitably sized cohort of LADA patients would be of great interest.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2014;2:56–64.
Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41:963–70.
https://www.who.int/news-room/fact-sheets/detail/diabetes; accessed June 20th 2020.
WHO, Classification of diabetes mellitus 2019. Available at: https://www.who.int/publications-detail/classification-of-diabetes-mellitus.
Tuomi T, Carlsson A, Li H, Isomaa B, Miettinen A, Nilsson A, et al. Clinical and genetic characteristics of type 2 diabetes with and without GAD antibodies. Diabetes. 1999;48:150–7.
Zinman B, Kahn SE, Haffner SM, O’Neill MC, Heise MA, Freed MI, et al. Phenotypic characteristics of GAD antibody-positive recently diagnosed patients with type 2 diabetes in North America and Europe. Diabetes. 2004;53:3193–200.
Hawa MI, Thivolet C, Mauricio D, Alemanno I, Cipponeri E, Collier D, et al. Metabolic syndrome and autoimmune diabetes: action LADA 3. Diabetes Care. 2009;32:160–4.
Andersen MK, Lundgren V, Turunen JA, Forsblom C, Isomaa B, Groop PH, et al. Latent autoimmune diabetes in adults differs genetically from classical type 1 diabetes diagnosed after the age of 35 years. Diabetes Care. 2010;33:2062–4.
Zhou Z, Xiang Y, Ji L, Jia W, Ning G, Huang G, et al. Frequency, immunogenetics, and clinical characteristics of latent autoimmune diabetes in China (LADA China study): a nationwide, multicenter, clinic-based cross-sectional study. Diabetes. 2013;62:543–50.
Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet. 2014;383:1084–94.
Hjort R, Ahlqvist E, Carlsson PO, Grill V, Groop L, Martinell M, et al. Overweight, obesity and the risk of LADA: results from a Swedish case–control study and the Norwegian HUNT Study. Diabetologia. 2018;61:1333–43.
Hjort R, Alfredsson L, Andersson T, Carlsson P-O, Grill V, Groop L, et al. Family history of type 1 and type 2 diabetes and risk of latent autoimmune diabetes in adults (LADA). Diabetes Metab. 2017;43:536–42.
Jörns A, Arndt T, Zu Vilsendorf AM, Klempnauer J, Wedekind D, Hedrich HJ, et al. Islet infiltration, cytokine expression and beta cell death in the NOD mouse, BB rat, Komeda rat, LEW.1AR1-iddm rat and humans with type 1 diabetes. Diabetologia. 2014;57:512–21.
Campbell-Thompson M, Fu A, Kaddis JS, Wasserfall C, Schatz DA, Pugliese A, et al. Insulitis and β-cell mass in the natural history of type 1 diabetes. Diabetes. 2016;65:719–31.
Jörns A, Wedekind D, Jähne J, Lenzen S. Pancreas pathology of latent autoimmune diabetes in adults (LADA) in patients and in a LADA rat model compared with type 1 diabetes. Diabetes. 2020;69:624–33.
Wod M, Thomsen RW, Pedersen L, Yderstraede KB, Beck-Nielsen H, Højlund K. Lower mortality and cardiovascular event rates in patients with latent autoimmune diabetes in adults (LADA) as compared with type 2 diabetes and insulin deficient diabetes: a cohort study of 4368 patients. Diabetes Res Clin Pract. 2018;139:107–13.
Maddaloni E, Coleman RL, Pozzilli P, Holman RR. Long-term risk of cardiovascular disease in individuals with latent autoimmune diabetes in adults (UKPDS 85). Diabetes Obes Metab. 2019;21:2115–22.
Maddaloni E, Coleman RL, Agbaje O, Buzzetti R, Holman RR. Time-varying risk of microvascular complications in latent autoimmune diabetes of adulthood compared with type 2 diabetes in adults: a post-hoc analysis of the UK Prospective Diabetes Study 30-year follow-up data (UKPDS 86). Lancet Diabetes Endocrinol. 2020;8:206–15.
Ahlqvist E, Storm P, Käräjämäki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6:361–9.
Castelblanco E, Hernandez M, Castelblanco A, Gratacos M, Esquerda A, Mollo A, et al. Low-grade inflammatory marker profile may help to differentiate patients with LADA, classic adult-onset type 1 diabetes, and type 2 diabetes. Diabetes Care. 2018;41:862–8.
Tong Y, Yang L, Shao F, Yan X, Li X, Huang G, et al. Distinct secretion pattern of serum proinsulin in different types of diabetes. Ann Transl Med. 2020;8:452.
Sørgjerd EP. Type 1 diabetes-related autoantibodies in different forms of diabetes. Curr Diabetes Rev. 2019;15:199–204.
Singal DP, Blajchman MA. Histocompatibility (HL-A) antigens, lymphocytotoxic antibodies and tissue antibodies in patients with diabetes mellitus. Diabetes. 1973;22:429–32.
Nerup J, Platz P, Andersen OO, Christy M, Lyngsoe J, Poulsen JE, et al. HL-A antigens and diabetes mellitus. Lancet. 1974;2:864–6.
Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, Erlich HA, et al. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 2009;41:703–7.
Bradfield JP, Qu HQ, Wang K, Zhang H, Sleiman PM, Kim CE, et al. A genome-wide meta-analysis of six type 1 diabetes cohorts identifies multiple associated loci. PLoS Genet. 2011;7:e1002293.
Onengut-Gumuscu S, Chen W-M, Burren O, Cooper NJ, Quinlan AR, Mychaleckyj JC, et al. Fine mapping of type 1 diabetes susceptibility loci and evidence for colocalization of causal variants with lymphoid gene enhancers. Nat Genet. 2015;47:381–6.
Mahajan A, Taliun D, Thurner M, Robertson NR, Torres JM, Rayner NW, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet. 2018;50:1505–13.
Eftychi C, Howson JM, Barratt BJ, Vella A, Payne F, Smyth DJ, et al. Analysis of the type 2 diabetes-associated single nucleotide polymorphisms in the genes IRS1, KCNJ11, and PPARG2 in type 1 diabetes. Diabetes. 2004;53:870–3.
Raj SM, Howson JM, Walker NM, Cooper JD, Smyth DJ, Field SF, et al. No association of multiple type 2 diabetes loci with type 1 diabetes. Diabetologia. 2009;52:2109–16.
Mahajan A, Go MJ, Zhang W, Below JE, Gaulton KJ, Ferreira T, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46:234–44.
• Aylward A, Chiou J, Okino M-L, Kadakia N, Gaulton KJ. Shared genetic risk contributes to type 1 and type 2 diabetes etiology. Hum Mol Genet. 2018. https://doi.org/10.1093/hmg/ddy314 Online ahead of print. Important study comprehensively examining the genetic overlap between type 1 and type 2 diabetes.
McKeigue PM, Spiliopoulou A, McGurnaghan S, Colombo M, Blackbourn L, McDonald TJ, et al. Persistent C-peptide secretion in type 1 diabetes and its relationship to the genetic architecture of diabetes. BMC Med. 2019;17:165.
Dooley J, Tian L, Schonefeldt S, Delghingaro-Augusto V, Garcia-Perez JE, Pasciuto E, et al. Genetic predisposition for beta cell fragility underlies type 1 and type 2 diabetes. Nat Genet. 2016;48:519–27.
Liston A, Todd JA, Lagou V. Beta-cell fragility as a common underlying risk factor in type 1 and type 2 diabetes. Trends Mol Med. 2017;23:181–94.
Battaglia M, Ahmed S, Anderson MS, Atkinson MA, Becker D, Bingley PJ, et al. Introducing the endotype concept to address the challenge of disease heterogeneity in type 1 diabetes. Diabetes Care. 2020;43:5–12.
Howson JM, Walker NM, Clayton D, Todd JA, Consortium T 1 DG. Confirmation of HLA class II independent type 1 diabetes associations in the major histocompatibility complex including HLA-B and HLA-A. Diabetes Obes Metab 2009:11 Suppl 1:31–45.
Sabbah E, Savola K, Ebeling T, Kulmala P, Vahasalo P, Ilonen J, et al. Genetic, autoimmune, and clinical characteristics of childhood- and adult-onset type 1 diabetes. Diabetes Care. 2000;23:1326–32.
Desai M, Zeggini E, Horton VA, Owen KR, Hattersley AT, Levy JC, et al. An association analysis of the HLA gene region in latent autoimmune diabetes in adults. Diabetologia. 2007;50:68–73.
Cervin C, Lyssenko V, Bakhtadze E, Lindholm E, Nilsson P, Tuomi T, et al. Genetic similarities between latent autoimmune diabetes in adults, type 1 diabetes, and type 2 diabetes. Diabetes. 2008;57:1433–7.
Luo S, Lin J, Xie Z, Xiang Y, Zheng P, Huang G, et al. HLA genetic discrepancy between latent autoimmune diabetes in adults and type 1 diabetes: LADA China study no. 6. J Clin Endocrinol Metab. 2016;101:1693–700.
• Mishra R, Chesi A, Cousminer DL, Hawa MI, Bradfield JP, Hodge KM, et al. Relative contribution of type 1 and type 2 diabetes loci to the genetic etiology of adult-onset, non-insulin-requiring autoimmune diabetes 2017:15:88. Study including interesting analysis of type 1 diabetes and type 2 diabetes genetic risk scores in LADA.
•• Cousminer DL, Ahlqvist E, Mishra R, Andersen MK, Chesi A, Hawa MI, et al. First genome-wide association study of latent autoimmune diabetes in adults reveals novel insights linking immune and metabolic diabetes. Diabetes Care 2018:11:2396–403. First genome-wide association study of LADA contributing with important findings, including the LADA-specific association in the PFKFB3 locus.
Pettersen E, Skorpen F, Kvaloy K, Midthjell K, Grill V. Genetic heterogeneity in latent autoimmune diabetes is linked to various degrees of autoimmune activity: results from the Nord-Trondelag Health Study. Diabetes. 2010;59:302–10.
•• Mishra R, Åkerlund M, Cousminer DL, Ahlqvist E, Bradfield JP, Chesi A, et al. Genetic discrimination between LADA and childhood-onset type 1 diabetes within the MHC. Diabetes Care 2020:43:418–25. Comprehensive analyses of the impact of variants in the HLA region in LADA and type 1 diabetes. The study identifies important genetic difference between LADA and type 1 diabetes.
Valdes AM, Erlich HA, Noble JA. Human leukocyte antigen class I B and C loci contribute to type 1 diabetes (T1D) susceptibility and age at T1D onset. Hum Immunol. 2005;66:301–13.
Nejentsev S, Howson JM, Walker NM, Szeszko J, Field SF, Stevens HE, et al. Localization of type 1 diabetes susceptibility to the MHC class I genes HLA-B and HLA-A. Nature. 2007;450:887–92.
Schloss J, Ali R, Racine JJ, Chapman HD, Serreze DV, DiLorenzo TP. HLA-B*39:06 efficiently mediates type 1 diabetes in a mouse model incorporating reduced thymic insulin expression. J Immunol. 2018;200:3353–63.
Pugliese A. Pathogenesis of type 1 diabetes: genetics. Int diabetes Monit. 2010;22:101–11.
Nepom GT, Kwok WW. Molecular basis for HLA-DQ associations with IDDM. Diabetes. 1998;47:1177–84.
Lee KH, Wucherpfennig KW, Wiley DC. Structure of a human insulin peptide-HLA-DQ8 complex and susceptibility to type 1 diabetes. Nat Immunol. 2001;2:501–7.
Peng H, Zhou M, Xu WD, Xu K, Zhai Y, Li R, et al. Association of PTPN22 C1858T polymorphism and type 1 diabetes: a meta-analysis. Immunol Investig. 2012;41:484–96.
Petrone A, Suraci C, Capizzi M, Giaccari A, Bosi E, Tiberti C, et al. The protein tyrosine phosphatase nonreceptor 22 (PTPN22) is associated with high GAD antibody titer in latent autoimmune diabetes in adults: non insulin requiring autoimmune diabetes (NIRAD) study 3. Diabetes Care. 2008;31:534–8.
Heneberg P, Kocková L, Čecháková M, Daňková P, Černá M. Autoimmunity-associated PTPN22 polymorphisms in latent autoimmune diabetes of the adult differ from those of type 1 diabetes patients. Int Arch Allergy Immunol. 2018;177:57–68.
Liu F, Liu J, Shan ZT, Li Q, Wang C, Ping PX, et al. The -1123G>C variant of PTPN22 gene promoter is associated with latent autoimmune diabetes in adult Chinese Hans. Cell Biochem Biophys. 2012;62:273–9.
Ramu D, Perumal V, Paul SFD. Association of common type 1 and type 2 diabetes gene variants with latent autoimmune diabetes in adults: a meta-analysis. J Diabetes. 2019;11:484–96.
Liu YC, Gu H. Cbl and Cbl-b in T-cell regulation. Trends Immunol. 2002;23:140–3.
Hill RJ, Zozulya S, Lu YL, Ward K, Gishizky M, Jallal B. The lymphoid protein tyrosine phosphatase Lyp interacts with the adaptor molecule Grb2 and functions as a negative regulator of T-cell activation. Exp Hematol. 2002;30:237–44.
Wu J, Katrekar A, Honigberg LA, Smith AM, Conn MT, Tang J, et al. Identification of substrates of human protein-tyrosine phosphatase PTPN22. J Biol Chem. 2006;281:11002–10.
Rieck M, Arechiga A, Onengut-Gumuscu S, Greenbaum C, Concannon P, Buckner JH. Genetic variation in PTPN22 corresponds to altered function of T and B lymphocytes. J Immunol. 2007;179:4704–10.
Sharp RC, Abdulrahim M, Naser ES, Naser SA. Genetic variations of PTPN2 and PTPN22: role in the pathogenesis of type 1 diabetes and Crohn’s disease. Front Cell Infect Microbiol. 2015;5:95.
Todd JA, Walker NM, Cooper JD, Smyth DJ, Downes K, Plagnol V, et al. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007;39:857–64.
Bennett ST, Lucassen AM, Gough SC, Powell EE, Undlien DE, Pritchard LE, et al. Susceptibility to human type 1 diabetes at IDDM2 is determined by tandem repeat variation at the insulin gene minisatellite locus. Nat Genet. 1995;9:284–92.
Desai M, Zeggini E, Horton VA, Owen KR, Hattersley AT, Levy JC, et al. The variable number of tandem repeats upstream of the insulin gene is a susceptibility locus for latent autoimmune diabetes in adults. Diabetes. 2006;55:1890–4.
•• Sharp SA, Rich SS, Wood AR, Jones SE, Beaumont RN, Harrison JW, et al. Development and standardization of an improved type 1 diabetes genetic risk score for use in newborn screening and incident diagnosis. Diabetes Care 2019:42:200–7. Important study demonstrating the utility of a type 1 diabetes genetic risk score in discriminating type 1 diabetes from population controls as well as patients with type 2 diabetes.
Pugliese A, Zeller M, Fernandez A Jr, Zalcberg LJ, Bartlett RJ, Ricordi C, et al. The insulin gene is transcribed in the human thymus and transcription levels correlated with allelic variation at the INS VNTR-IDDM2 susceptibility locus for type 1 diabetes. Nat Genet. 1997;15:293–7.
Vafiadis P, Bennett ST, Todd JA, Nadeau J, Grabs R, Goodyer CG, et al. Insulin expression in human thymus is modulated by INS VNTR alleles at the IDDM2 locus. Nat Genet. 1997;15:289–92.
Pugliese A. The insulin gene in type 1 diabetes. IUBMB Life. 2005;57:463–8.
Sparks AE, Chen C, Breslin MB, Lan MS. Functional domains of autoimmune regulator (AIRE) modulate INS-VNTR transcription in human thymic epithelial cells. J Biol Chem. 2016;291:11313–22.
Dale BL, Madhur MS. Linking inflammation and hypertension via LNK/SH2B3. Curr Opin Nephrol Hypertens. 2016;25:87–93.
Auburger G, Gispert S, Lahut S, Omür O, Damrath E, Heck M, et al. 12q24 locus association with type 1 diabetes: SH2B3 or ATXN2 ? World J Diabetes. 2014;5:316–27.
Maslah N, Cassinat B, Verger E, Kiladjian JJ, Velazquez L. The role of LNK/SH2B3 genetic alterations in myeloproliferative neoplasms and other hematological disorders. Leukemia. 2017;31:1661–70.
Devallire J, Charreau B. The adaptor Lnk (SH2B3): an emerging regulator in vascular cells and a link between immune and inflammatory signaling. Biochem Pharmacol. 2011;82:1391–402.
Perez-Garcia A, Ambesi-Impiombato A, Hadler M, Rigo I, LeDuc CA, Kelly K, et al. Genetic loss of SH2B3 in acute lymphoblastic leukemia. Blood. 2013;122:2425–32.
Mori T, Suzuki-Yamazaki N, Takaki S. Lnk/Sh2b3 regulates adipose inflammation and glucose tolerance through group 1 ILCs. Cell Rep. 2018;24:1830–41.
Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J, et al. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet. 2006;38:320–3.
Helgason A, Pálsson S, Thorleifsson G, Grant SFA, Emilsson V, Gunnarsdottir S, et al. Refining the impact of TCF7L2 gene variants on type 2 diabetes and adaptive evolution. Nat Genet. 2007;39:218–25.
Gaulton KJ, Nammo T, Pasquali L, Simon JM, Giresi PG, Fogarty MP, et al. A map of open chromatin in human pancreatic islets. Nat Genet. 2010;42:255–9.
Lukacs K, Hosszufalusi N, Dinya E, Bakacs M, Madacsy L, Panczel P. The type 2 diabetes-associated variant in TCF7L2 is associated with latent autoimmune diabetes in adult Europeans and the gene effect is modified by obesity: a meta-analysis and an individual study. Diabetologia. 2012;55:689–93.
Andersen MK, Sterner M, Forsén T, Käräjämäki A, Rolandsson O, Forsblom C, et al. Type 2 diabetes susceptibility gene variants predispose to adult-onset autoimmune diabetes. Diabetologia. 2014;57:1859–68.
Zampetti S, Spoletini M, Petrone A, Capizzi M, Arpi ML, Tiberti C, et al. Association of TCF7L2 gene variants with low GAD autoantibody titre in LADA subjects (NIRAD Study 5). Diabet Med. 2010;27:701–4.
Qu HQ, Polychronakos C. The TCF7L2 locus and type 1 diabetes. BMC Med Genet. 2007;8:51.
Field SF, Howson JM, Smyth DJ, Walker NM, Dunger DB, Todd JA. Analysis of the type 2 diabetes gene, TCF7L2, in 13,795 type 1 diabetes cases and control subjects. Diabetologia. 2007;50:212–3.
Winkler C, Raab J, Grallert H, Ziegler AG. Lack of association of type 2 diabetes susceptibility genotypes and body weight on the development of islet autoimmunity and type 1 diabetes. PLoS One. 2012;7:e35410.
Yu J, Steck AK, Babu S, Yu L, Miao D, McFann K, et al. Single nucleotide transcription factor 7-like 2 (TCF7L2) gene polymorphisms in antiislet autoantibody-negative patients at onset of diabetes. J Clin Endocrinol Metab. 2009;94:504–10.
Redondo MJ, Geyer S, Steck AK, Sosenko J, Anderson M, Antinozzi P, et al. TCF7L2 genetic variants contribute to phenotypic heterogeneity of type 1 diabetes. Diabetes Care. 2018;41:311–7.
Yi F, Brubaker PL, Jin T. TCF-4 mediates cell type-specific regulation of proglucagon gene expression by β-catenin and glycogen synthase kinase-3β. J Biol Chem. 2005;280:1457–64.
Liu Z, Habener JF. Glucagon-like peptide-1 activation of TCF7L2-dependent Wnt signaling enhances pancreatic beta cell proliferation. J Biol Chem. 2008;283:8723–35.
Florez JC, Jablonski KA, Bayley N, Pollin TI, De Bakker PIW, Shuldiner AR, et al. TCF7L2 polymorphisms and progression to diabetes in the diabetes prevention program. N Engl J Med. 2006;355:241–50.
Saxena R, Gianniny L, Burtt NP, Lyssenko V, Giuducci C, Sjogren M, et al. Common single nucleotide polymorphisms in TCF7L2 are reproducibly associated with type 2 diabetes and reduce the insulin response to glucose in nondiabetic individuals. Diabetes. 2006;55:2890–5.
Lyssenko V, Lupi R, Marchetti P, Del Guerra S, Orho-Melander M, Almgren P, et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest. 2007;117:2155–63.
Chen X, Ayala I, Shannon C, Fourcaudot M, Acharya NK, Jenkinson CP, et al. The diabetes gene and wnt pathway effector TCF7L2 regulates adipocyte development and function. Diabetes. 2018;67:554–68.
Kaminska D, Kuulasmaa T, Venesmaa S, Käkelä P, Vaittinen M, Pulkkinen L, et al. Adipose tissue TCF7L2 splicing is regulated by weight loss and associates with glucose and fatty acid metabolism. Diabetes. 2012;61:2807–13.
Kirkpatrick CL, Marchetti P, Purrello F, Piro S, Bugliani M, Bosco D, et al. Type 2 diabetes susceptibility gene expression in normal or diabetic sorted human alpha and beta cells: correlations with age or BMI of islet donors. PLoS One. 2010;5:e11053.
Duran J, Obach M, Navarro-Sabate A, Manzano A, Gómez M, Rosa JL, et al. Pfkfb3 is transcriptionally upregulated in diabetic mouse liver through proliferative signals. FEBS J. 2009;276:4555–68.
Atsumi T, Nishio T, Niwa H, Takeuchi J, Bando H, Shimizu C, et al. Expression of inducible 6-phosphofructo-2-kinase/fructose-2,6- bisphosphatase/PFKFB3 isoforms in adipocytes and their potential role in glycolytic regulation. Diabetes. 2005;54:3349–57.
Huo Y, Guo X, Li H, Wang H, Zhang W, Wang Y, et al. Disruption of inducible 6-phosphofructo-2-kinase ameliorates diet-induced adiposity but exacerbates systemic insulin resistance and adipose tissue inflammatory response. J Biol Chem. 2010;285:3713–21.
Huo Y, Guo X, Li H, Xu H, Halim V, Zhang W, et al. Targeted overexpression of inducible 6-phosphofructo-2-kinase in adipose tissue increases fat deposition but protects against diet-induced insulin resistance and inflammatory responses. J Biol Chem. 2012;287:21492–500.
Montemurro C, Nomoto H, Pei L, Parekh VS, Vongbunyong KE, Vadrevu S, et al. IAPP toxicity activates HIF1α/PFKFB3 signaling delaying β-cell loss at the expense of β-cell function. Nat Commun. 2019;10:2679.
Nomoto H, Pei L, Montemurro C, Rosenberger M, Furterer A, Coppola G, et al. Activation of the HIF1α/PFKFB3 stress response pathway in beta cells in type 1 diabetes. Diabetologia. 2020;63:149–61.
Udler MS, McCarthy MI, Florez JC, Mahajan A. Genetic risk scores for diabetes diagnosis and precision medicine. Endocr Rev. 2019;40:1500–20.
Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50:1219–24.
The risk-screening converter. Available from: https://www.lmsalpha.co.uk/rsc. Accessed June 20th 2020.
Wald NJ, Old R. The illusion of polygenic disease risk prediction. Genetics in Medicine. 2019;21:1705–7.
Oram RA, Patel K, Hill A, Shields B, McDonald TJ, Jones A, et al. A type 1 diabetes genetic risk score can aid discrimination between type 1 and type 2 diabetes in young adults. Diabetes Care. 2016;39:337–44.
•• Grubb AL, McDonald TJ, Rutters F, Donnelly LA, Hattersley AT, Oram RA, et al. A type 1 diabetes genetic risk score can identify patients with GAD65 autoantibody–positive type 2 diabetes who rapidly progress to insulin therapy. Diabetes Care 2019:42:208–14. Important study demonstrating the utility of a type 1 diabetes genetic risk score in discriminating GAD autoantibody positive type 2 diabetes patients rapidly progressing to insulin therapy.
Udler MS, Kim J, von Grotthuss M, Bonàs-Guarch S, Cole JB, Chiou J, et al. Type 2 diabetes genetic loci informed by multi-trait associations point to disease mechanisms and subtypes: a soft clustering analysis. PLoS Med. 2018;15:e1002654.
Funding
MKA was supported by a research grant from the Danish Diabetes Academy supported by the Novo Nordisk Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mette K. Andersen declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Genetics
Rights and permissions
About this article
Cite this article
Andersen, M.K. New Insights into the Genetics of Latent Autoimmune Diabetes in Adults. Curr Diab Rep 20, 43 (2020). https://doi.org/10.1007/s11892-020-01330-y
Published:
DOI: https://doi.org/10.1007/s11892-020-01330-y