Abstract
Purpose of Review
Endoscopic submucosal dissection (ESD) is recognized as a minimally invasive treatment for colorectal cancer. However, colorectal ESD has not been internationally accepted as a first-line therapeutic option due to technical difficulties and high complication rates. Non-lifting tumors present a further limitation of ESD. Colorectal endoscopic full-thickness resection (eFTR) with over-the-scope clips (OTSCs) shows great potential in patients for whom ESD is not possible and also for those who might have ESD-related complications. The present manuscript aims to discuss the complementary role of eFTR using OTSCs and the future development of eFTR with a novel suturing device.
Recent Findings
Colorectal eFTR is feasible and has acceptable en bloc and R0 resection rates and procedure-related adverse events. This technique is primarily used for non-lifting and recurrent adenomas, especially in lesions ≤ 2 cm. This approach offers the potential to decrease the postoperative morbidity and mortality associated with segmental colectomy while enhancing the diagnostic yield compared to that of current endoscopic techniques.
Summary
eFTR using OTSCs is a safe and effective procedure for treating colorectal non-lifting and recurrent adenoma. The indications may be expanded to include subepithelial tumors, carcinoid tumors, and neuromuscular GI disorders. eFTR using OTSCs is not recommended for large lesions (> 30 mm), but innovative methods and new devices for eFTR and suturing will overcome the limitations by allowing minimally invasive surgery for colorectal cancer in the near future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic resection, including polypectomy and endoscopic mucosal resection (EMR), is a widely recognized treatment for early gastrointestinal (GI) malignancy. Endoscopic submucosal dissection (ESD) is accepted as a minimally invasive treatment for early GI malignancies, but technical difficulties and an increased rate of complications have limited its applicability in the management of colorectal tumors. Colorectal ESD enables the en bloc resection of a specimen, but procedure-related complications are more frequently associated with ESD than with EMR [1, 2]. However, colorectal ESD has not been internationally accepted as a first-line therapeutic option because of the technical challenges associated with the procedure and the increased risk of adverse events such as perforation and bleeding [3].
Endoscopic full-thickness resection (eFTR) using over-the-scope clips (OTSCs) shows great potential for sparing patients from colorectal ESD and surgical resection [4•, 5•, 6••]. eFTR in the colon and rectum with a full-thickness resection device (FTRD; Ovesco Endoscopy AG, Tubingen, Germany) is increasingly gaining acceptance as an established technique in Western countries. The FTRD has been investigated for colon eFTR in preclinical and clinical studies [4•, 5•, 6••]. eFTR of the colon may decrease the postoperative morbidity and mortality associated with segmental colectomy while enhancing the diagnostic yield compared to that of current endoscopic techniques [7]. Recent developments in advanced eFTR using OTSCs will enable surgeons and endoscopists to challenge current clinical practices for colorectal cancer treatment.
Closure is required after eFTR and natural transluminal endoscopic surgery (NOTES). Endoscopic clips are often used for small mucosal defects but are not a suitable choice for large GI gaps. Many endoscopic closure devices have undergone testing and evaluation in the laboratory in animal models for closing large GI defects via minimally invasive surgical treatment and NOTES-associated procedures, including eFTR [7,8,9]. Given the limitations of OTSCs, suturing systems have been introduced. One of the first devices developed to accomplish this objective was the Overstitch Endoscopic Suturing System (Apollo Endosurgery, Austin, TX). Other endoscopic suturing devices have been tested as novel tools for achieving complete closure post-eFTR.
The present manuscript aims to discuss the complementary role of the eFTR using OTSCs and the future development of eFTR. Additionally, we focus on the possibility of achieving eFTR using novel suturing and closing devices.
Indications for Colorectal eFTR
The indications for colorectal eFTR according to previous reports are summarized in Table 1. The indications for eFTR are mainly (1) a non-lifting adenoma and (2) a recurrent tumor [6••, 10••, 11, 12•, 13••, 14•]. Additional indications include the following: (1) technically difficult ESD with a difficult anatomical location involving the appendix and diverticulum, (2) recurrent adenoma with severe fibrosis after endoscopic treatment, and (3) submucosal tumors including carcinoid tumors. These two aspects are considered to determine the need for eFTR for each lesion. Performing colorectal ESD is challenging in the presence of technically difficult lesions with severe fibrosis; recurrent lesions; lesions located at the bottom of the caecum, near the terminal ileum, and in the appendix; and large pedunculated polyps. Severe fibrosis, poor endoscopic operability, and submucosal deep invasion, which is a muscle-retracting sign of protrusion, are the most common reasons for incomplete resection and procedure-related perforations during colorectal ESD [15,16,17]. However, piecemeal resection is an important risk factor for local recurrence regardless of endoscopic resection [18]. eFTR with OTSCs has been described for recurrent adenocarcinoma [19] and rectal adenocarcinoma with SM (submucosal) invasiveness [20, 21].
eFTR may also be used for selected subepithelial lesions (e.g., neuroendocrine tumors) of limited size. Endoscopic treatment is considered curative for small carcinoid tumors with an extremely low risk of metastasis [22, 23]. Recently, ESD was reported to be an effective method for the treatment of rectal carcinoid tumors [19, 22, 23]. Lesions can become indications for eFTR when they are intermediate in size or massively invade the submucosal layer, which may result in tumor-positive margin resection. eFTR with OTSCs has been reported for subepithelial lesions, carcinoid tumors [24, 25], neuroendocrine tumors [26], gastrointestinal stromal tumors (GIST) [27], and B-cell lymphoma [28].
eFTR Using OTSCs
OTSCs (Ovesco Endoscopy AG, Tübingen, Germany) and Padlock clips (Aponos Medical, Kingston, NH, USA) are commercially available. OTSCs (Ovesco Endoscopy AG, Tübingen, Germany) have been effective for the closure of iatrogenic perforation [29] and GI bleeding [30, 31]. Several studies have demonstrated the successful use of OTSCs in the closure of acute GI perforations, anastomotic leaks, and GI fistulae [32••, 33]. We previously reported that OTSCs were useful in closing large defects and perforations after ESD (large defects > 20 mm, small defects ≤ 10 mm) [33, 34]. The advantage of OTSCs is that they can easily and rapidly completely close a mural defect compared to other devices. OTSCs may have limited efficacy in the following situations: (1) larger mural defects, (2) chronic inflammation, and (3) repeated attempts at closure. We previously reported successful use of OTSCs in GI bleeds, perforations, and fistulae. In our experience, large lesion size and tissue fibrosis were the major contributing factors in unsuccessful cases [33].
Schurr et al. and Von Rentlen et al. described several variations of a grasp-and-snare technique. They performed both pre- and post-resection closure using an OTSC (Ovesco Endoscopy, Tubingen, Germany). A tissue anchor (Ovesco, Endoscopy) was inserted through a double-channel gastroscope (2T160, Olympus, Hamburg, Germany) to grasp the bowel wall and create a pseudopolyp. The base of the pseudopolyp was ligated with an Endoloop (HX-400U- 30, Olympus) before snare resection. The advantage of this method is the ability to easily and rapidly resect the main lesion and quickly close the colon wall defect. These methods are also favorable for preventing peritoneal infection and the dissemination of cancer cells into the peritoneal cavity. A disadvantage of the grasp-and-snare technique is that it is difficult to produce a specimen with an adequate horizontal clearance margin.
Endoscopic resection of the target lesion by application of an OTSC followed by snare application has been described as a feasible strategy for tumor resection [4•, 5•, 6••]. The key steps of eFTR using an OTSC are as follows: (1) the lesion is pulled using tissue grasping forceps or a tissue anchor (Ovesco Endoscopy) into the distal cap of the OTSC; (2) the OTSC is then released at the base of the pseudopolyp, thus tightly grasping the base and securing the bowel wall; and (3) the pseudopolyp created by the OTSC is then resected using the snare while the OTSC maintains the integrity of the colonic wall.
The FTRD (Ovesco Endoscopy, Tübingen, Germany) is a modified device mounted on a long cap with a preloaded snare. The snare is placed in the open position, firmly linked to the cap and fixed to the outside of the endoscope. After deployment of the OTSC, the snare is tightened above the OTSC and smooth resection of the pseudopolyp is accomplished. The Padlock clip (Aponos Medical, Kingston, NH, USA) is another commercially available OTSC. The Padlock clip instantly returns to its original flat form when deployed, which might facilitate snare resection of the created pseudopolyp [35,36,37].
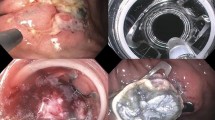
FTRDs are not commercially available in Eastern countries, including Japan. Recently, we were challenged to perform an eFTR using a needle knife (KD-650Q; Olympus, Tokyo, Japan) and OTSC system in animal models [36]. First, a 10-mm pocket was created in the colorectal mucosa using a needle knife until the muscle layer was reached. Next, after the artificial mucosal pocket had been anchored into the application cap with a retraction device (Anchor; Ovesco Endoscopy) that captured the exposed muscle layer, the OTSC was deployed. Finally, a full-thickness resection was completed with the snare (Fig. 1).
EFTR using ESD devices. First, 10-mm pocket created in colorectal mucosa using needle knife until muscle layer. Next, after artificial mucosal pocket has been anchored into the application cap with a retraction device (Anchor; Ovesco Endoscopy) that captured the exposed muscle layer, the OTSC is deployed. Finally, a full-thickness resection is completed with the snare
A potential indication for the removal of an OTSC could be its misplacement. A removal method for a released OTSC was reported using an Nd-YAG laser [6••] and a bipolar cutting device known as the remOVE System (Ovesco Endoscopy AG, Tübingen, Germany) [38].
Clinical Outcomes of Colonic eFTR with an FTRD
The outcomes following colorectal eFTR according to previous reports from single institutions studies are shown in Table 2. In these studies, the main indication for eFTR was the presence of residual or recurrent neoplasms. The median tumor size was 12–35 mm. The mean diameter of the resection specimen was 12.5–26 mm. The en bloc resection rate, R0 resection rate, and percentage of histologically confirmed full-thickness resections were 63–89.5, 75–100, and 50–100%, respectively. The procedure-related complications were as follows: immediate and delayed bleeding and perforation, appendicitis, and incomplete OTSC deployment. The complication rate was 0–11.5%.
According to a prospective multicentre trial by Schmidt et al., eFTR was a technically successful type of resection and the R0 resection rates were 89.5 and 76.9% [39••]. The median procedure time was 50 min (range 3–190 min), and the mean maximum lesion diameter was 15 mm (range 2–30 mm). The median duration of the hospital stay was 4 days (range 1–11 days), and prolonged hospital stays occurred due to adverse events. Full-thickness resection was histologically confirmed in 81% of cases, and the resection rate in the rectum was lower than that in the colon (66.7 vs. 83.9%, p = 0.056). Importantly, the R0 resection rate was significantly lower for lesions > 20 mm (58.1%) than for lesions ≤ 20 mm (81.2%; p = 0.00038). The adverse event rate was 9.95% with a 2.2% rate of emergency surgery. Regarding complications, perforation and postoperative bleeding occurred in 3.3 and 2.2% of cases, respectively. The surgical conversion rate was 2.2%.
Therapeutic Potential and Limitations of eFTR with an FTRD
ESD, which enables en bloc resection of large tumors, is accepted as a standard minimally invasive treatment for early GI malignancies. According to a Japanese multicentre retrospective analysis, the en bloc resection (endoscopic) and R0 resection (complete en bloc resection by histological methods) rates were 88.8 and 83.8%, respectively [7, 40]. Regarding complications, perforation and postoperative bleeding occurred in 4.8–4.9 and 1.5–1.6% of cases, respectively. Complications were strongly dependent on local expertise, lesion location and characteristics [15, 41]. Therefore, the complication rate appears acceptable but must also be considered in light of the respective indication.
Two retrospective studies comparing ESD vs. laparoscopic-assisted surgery for early colorectal neoplasm reported en bloc and curative resection rates of 100%, a mean procedure time of 90–106 min, and adverse event rates of 13.69–14.7% in a laparoscopic-assisted surgery group [42,44,44]. According to these results, eFTR is effective and safe for the treatment of colorectal neoplasm without lymph node metastasis.
The primary advantage of ESD over eFTR is a higher en bloc resection rate for large colonic lesions (> 20 mm). The FTRD cap is equipped with a modified 14-mm OTSC and enables the capture of more tissue, as it is longer and wider. In fact, the thickness, rigidity, and mobility of the colonic wall may differ among patients and is significantly dependent on anatomic location and the existence of fibrosis [10••]. Earlier studies evaluating an FTRD using OTSCs for the closure of defects were performed only for defects up to 3 cm in size [6••, 10••]. Outcome studies have demonstrated that eFTR defects up to 2.5–3 cm can be adequately closed using OTSCs in the majority of cases. Therefore, OTSCs allow full-thickness resection of GI tract lesions smaller than approximately 3 cm [10••]. The FTRD is not recommended for large lesions (> 30 mm). In cases of severe scarring due to inflammation, the maximum lesion size should be even smaller (20–25 mm) [10••]. eFTR on scar tissue results in decreased specimen volumes and often in lateral margins positive for scar tissue, especially when used on scars from polyps > 20 mm [13••]. Additionally, a large, flat, elevated lesion (e.g., laterally spreading tumor) is difficult to resect when using the FTRD. Furthermore, a lesion located in the lower rectum may be limited due to the fixation of the rectal wall in the perirectal tissue. Hybrid EMR-eFTR methods may be effective solutions for large polyps and laterally spreading tumors [11, 45].
Another limitation of the FTRD is that the lateral margins of the lesions are not easily visible circumferentially during retraction of the lesion into the cap [10••]. The marking probe is not clearly visible during retraction of the lesion into the cap, which leads to the risk of incomplete eFTR. In addition, marking the lesion using argon plasma coagulation (APC) may be preferred for increasing visibility during the retraction [12•].
A potential risk of the FTRD procedure may include accidental clipping of extracolonic structures. The cecum near the appendiceal orifice remains a challenging area of endoscopic resection [46]. According to previous studies, closure of the appendiceal orifice with the FTRD carries the potential risk of acute appendicitis and some cases require emergency surgery. Therefore, clinicians should be made aware of the risk of acute appendicitis so that their patients may be monitored to identify any serious conditions after eFTR. In another case, a misplaced OTSC that grasped the small intestine through an iatrogenic colonic perforation was reported [47]. To avoid unintended incorporation of organs adjacent to the colonic wall, it is crucial to exclusively use traction with the forceps or the tissue anchor to pull the target into the cap [10••].
New Endoscopic Suturing System and Future Perspective
Various endoscopic suturing devices have been tested as novel tools to achieve complete closure post-eFTR. The Overstitch Endoscopic Suturing System (Apollo Endosurgery, Austin, TX) is a disposable, single-use suturing device that is mounted onto a double-channel therapeutic endoscope and allows for the placement of either running or interrupted full-thickness sutures. It is currently the only widely available suturing device and the only Food and Drug Administration-approved commercially available device [48]. This suturing device has been used successfully for the closure of GI fistulae, stent anchorage, leaks, and perforations [49]. eFTR with the Overstitch system has been reported for rectal neuroendocrine tumors [50]. Kantsevoy et al. reported that closure of a large post-ESD mucosal defect in the colon using the Overstitch Endoscopic Suturing Device decreased treatment cost by eliminating the need for hospitalization [51]. In their study, primary closures of post-ESD ulcers were achieved after removing specimens larger than 30 mm in diameter. However, large eFTR defects induce a distinct luminal collapse, rendering endoscopic closure very difficult. We have previously reported the exposed eFTR using the ESD devices and suturing a large mucosal defect using a new suturing system and mechanical counter traction device in animal models [52, 53]. In suturing resection wounds > 30 mm, these devices enable the complete suture of a large mural defect. However, non-exposed eFTR is more reliable than exposed eFTR for preventing bacterial infection and cancer cell dissemination [54, 55]. We developed a non-exposed eFTR method using the double-armed bar suturing system (DBSS), which is a novel full-thickness suturing device that can be used with flexible endoscopes to overcome these problems [56, 57]. We aim to improve these devices such that large mural defects can be sutured more simply and rapidly. Finally, it is essential that endoscopists understand the surgical anatomy of the organs located on the outside of the colonic wall to establish colorectal eFTR and related procedures [8].
Conclusions
eFTR using an FTRD is a safe and effective procedure for treating colorectal non-lifting and recurrent adenoma. The indications may be expanded to include subepithelial tumors, carcinoid tumors, and neuromuscular GI disorders. eFTR can also be used for harvesting full-thickness specimens during diagnostic investigations of neuromuscular GI disorders, such as Hirschsprung’s disease, intestinal neuronal malformation, and chronic intestinal pseudo-obstruction (CIPO) [35, 36]. This approach allows full-thickness resection of GI tract lesions smaller than approximately 3 cm. The FTRD is not recommended for large lesions (> 30 mm), but innovative methods and new devices for eFTR and suturing will overcome the limitations of the FTRD by allowing minimally invasive surgery for colorectal cancer in the near future.
Abbreviations
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- GI:
-
Gastrointestinal
- OTS:
-
Over-the-scope
- OTSC:
-
Over-the-scope clip
- FTRD:
-
Full-thickness resection device
- eFTR:
-
Endoscopic full-thickness resection
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Saito Y, Sakamoto T, Nakajima T, Matsuda T. Colorectal ESD: current indications and latest technical advances. Gastrointest Endosc Clin N Am. 2014;24(2):245–55. https://doi.org/10.1016/j.giec.2013.11.005.
Saito Y, Yamada M, So E, Abe S, Sakamoto T, Nakajima T, et al. Colorectal endoscopic submucosal dissection: technical advantages compared to endoscopic mucosal resection and minimally invasive surgery. Dig Endosc. 2014;26(Suppl 1):52–61. https://doi.org/10.1111/den.12196.
Oda I, Suzuki H, Nonaka S, Yoshinaga S. Complications of gastric endoscopic submucosal dissection. Dig Endosc. 2013;25(Suppl 1):71–8. https://doi.org/10.1111/j.1443-1661.2012.01376.x.
• Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, et al. Multipurpose use of the ‘bear claw’ (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26(3):350–7. https://doi.org/10.1111/den.12145. This is an observational, open-label, retrospective, single-arm case series conducted at two hospitals with tertiary care endoscopy. The OTSC system is a useful device in a variety of clinical scenarios including the management of larger GI leaks and fistulas, GI bleeding, and full-thickness resection of tumors, even in very old and frail patients.
• Sarker S, Gutierrez JP, Council L, Brazelton JD, Kyanam Kabir Baig KR, Mönkemüller K. Over-the-scope clip-assisted method for resection of full-thickness submucosal lesions of the gastrointestinal tract. Endoscopy. 2014;46(09):758–61. https://doi.org/10.1055/s-0034-1365513. This was a retrospective, observational cohort study of patients undergoing endoscopic resection of submucosal lesions. This case series suggests that the OTSC system may be a valuable tool for the resection of submucosal lesions.
•• Fähndrich M, Sandmann M. Endoscopic full-thickness resection for gastrointestinal lesions using the over-the-scope clip system: a case series. Endoscopy. 2015;47(01):76–9. https://doi.org/10.1055/s-0034-1377975. This is retrospective, observational, open-label case study, a total of 17 patients underwent eFTR using OTSCs. The indications were carcinoids, incompletely resected colon cancers, recurrent fibrosed adenoma, and submucosal lesions. The technical success was 94 % (16 /17). The complete resection (R0) rate was 100 %. There were no complications.
Fujihara S, Mori H, Kobara H, Nishiyama N, Matsunaga T, Ayaki M, et al. Current innovations in endoscopic therapy for the management of colorectal cancer: from endoscopic submucosal dissection to endoscopic full-thickness resection. Biomed Res Int. 2014;2014:1–12. https://doi.org/10.1155/2014/925058.
Mori H, Kobara H, Nishiyama N, Fujihara S, Masaki T. Review of pure endoscopic full-thickness resection of the upper gastrointestinal tract. Gut Liver. 2015;9(5):590–600. https://doi.org/10.5009/gnl14380.
Schmidt A, Meier B, Caca K. Endoscopic full-thickness resection: current status. World J Gastroenterol. 2015;21(31):9273–85. https://doi.org/10.3748/wjg.v21.i31.9273.
•• Schmidt A, Bauerfeind P, Gubler C, Damm M, Bauder M, Caca K. Endoscopic full-thickness resection in the colorectum with a novel over-the-scope device: first experience. Endoscopy. 2015;47(8):719–25. This is retrospective, observational study at two tertiary referral centers. All resections were performed using the FTRD (full-thickness resection device). Indications for eFTR were recurrent or incompletely resected adenoma, untreated adenoma and nonlifting sign, adenoma involving the appendix, etc. The R0 resection rate was 75.0 % (18/24), and full-thickness resectionwas histologically confirmed in 87.5 %. There were no complications. https://doi.org/10.1055/s-0034-1391781.
Meier B, Caca K, Schmidt A. Hybrid endoscopic mucosal resection and full-thickness resection: a new approach for resection of large non-lifting colorectal adenomas (with video). Surg Endosc. 2017;31(10):4268–74. https://doi.org/10.1007/s00464-017-5461-9.
• Andrisani G, Pizzicannella M, Martino M, Rea R, Pandolfi M, Taffon C, et al. Endoscopic full-thickness resection of superficial colorectal neoplasms using a new over-the-scope clip system: a single-centre study. Dig Liver Dis. 2017;49:1–5. This is retrospective, observational, open-label case study, a total of 20 patients with superficial colorectalneoplasms, underwent EFTR using FTRD. The technical success rate was 100% (20/20). Mean size of the resected lesions was 26mm, ranging from 10 to 42mm.
•• Backes Y, Kappelle WF, Berk L, Koch AD, Groen JN, tot Nederveen WH, et al. Colorectal endoscopic full-thickness resection using a novel, flat-base over-the-scope clip: a prospective study. Endoscopy. 2017;49:1–2. This is a prospective study. Endoscopic full-thickness resection (eFTR) was performed using the Padlock clip. Indications for eFTR were mainly recurrent or incompletely resected adenoma, and nonlifting sign. Technical success rate and full-thickness resectionrate were 100 % (26/26) and 92 % (24/26). No complications occurred during the procedure.
• Valli PV, Mertens J, Bauerfeind P. Safe and successful resection of difficult GI lesions using a novel single-step full-thickness resection device (FTRD®). Surg Endosc. 2017; https://doi.org/10.1007/s00464-017-5676-9. This is retrospective, observational case study, a total of 60 patients underwent EFTR using FTRD. The technical success rate was 97% (58/60). The R0 resection rate was 88% (51/58) on histologically examination.
Sato K, Ito S, Kitagawa T, Kato M, Tominaga K, Suzuki T, et al. Factors affecting the technical difficulty and clinical outcome of endoscopic submucosal dissection for colorectal tumors. Surg Endosc. 2014;28(10):2959–65. https://doi.org/10.1007/s00464-014-3558-y.
Hayashi N, Tanaka S, Nishiyama S, Terasaki M, Nakadoi K, Oka S, et al. Predictors of incomplete resection and perforation associated with endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2014;79(3):427–35. https://doi.org/10.1016/j.gie.2013.09.014.
Toyonaga T, Tanaka S, Man-I M, East J, Ono W, Nishino E, et al. Clinical significance of the muscle-retracting sign during colorectal endoscopic submucosal dissection. Endosc Int Open. 2015;3(03):E246–51. https://doi.org/10.1055/s-0034-1391665.
Oka S, Tanaka S, Saito Y, Iishi H, Kudo SE, Ikematsu H, et al. Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol. 2015;110(5):697–707. https://doi.org/10.1038/ajg.2015.96.
Kobara H, Mori H, Chei L, Fujihara S, Nishiyama N, Masaki T. The advantage of an endoscopic submucosal tunneling technique for rectal carcinoid tumors. Gut Liver. 2017;11(5):735–7. https://doi.org/10.5009/gnl16580.
Fähndrich M, Heike M, Sandmann M. The Dortmund endoscopic full-thickness resection method: combination of the over-the-scope clip system and the Inoue cap. Endoscopy. 2014;46(Suppl 1 UCTN):E466. https://doi.org/10.1055/s-0034-1377548.
Di Mitri ML. One-session “2-step” technique for endoscopic full-thickness resection of a large rectal adenocarcinoma: when it is possible, overcome the lesion’s size. YMGE. American Society for Gastrointestinal Endoscopy; 2017.
Chen T, Yao LQ, Xu MD, Zhang YQ, Chen WF, Shi Q, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal carcinoids. Clin Gastroenterol Hepatol. 2016;14(4):575–81. https://doi.org/10.1016/j.cgh.2015.07.048.
Kaneko H, Hirasawa K, Koh R, Kobayashi R, Kokawa A, Tanaka K, et al. Treatment outcomes of endoscopic resection for rectal carcinoid tumors: an analysis of the resectability and long-term results from 46 consecutive cases. Scand J Gastroenterol. 2016;51(12):1489–94. https://doi.org/10.1080/00365521.2016.1216591.
Al-Bawardy B, Rajan E, Wong Kee Song LM. Over-the-scope clip-assisted endoscopic full-thickness resection of epithelial and subepithelial GIlesions. Gastrointest Endosc. 2017;85(5):1087–92. https://doi.org/10.1016/j.gie.2016.08.019.
Grauer M, Gschwendtner A, Schäfer C, Neumann H. Resection of rectal carcinoids with the newly introduced endoscopic full-thickness resectiondevice. Endoscopy. 2016;48(Suppl 1):E123–4. https://doi.org/10.1055/s-0042-104651.
Klare P, Burlefinger R, Neu B, Bajbouj M, Specht K, Schmid RM, et al. Over-the-scope clip-assisted endoscopic full-thickness resection after incomplete resection of a rectal neuroendocrine tumor. Endoscopy. 2015;47(Suppl 1 UCTN):E47–8. https://doi.org/10.1055/s-0034-1391301.
Probst A, Schaller T, Messmann H. Gastrointestinal stromal tumor of the colon - endoscopic treatment by full-thickness resection. Endoscopy. 2015;47(Suppl 1 UCTN):E460–1. https://doi.org/10.1055/s-0034-1392862.
Salerno R, Gherardi G, Paternò E, Ardizzone S. Endoscopic full-thickness resection of a submucosal right colon lesion. Endoscopy. 2016;48(S 01):E376–E7. https://doi.org/10.1055/s-0042-120338.
Khater S, Rahmi G, Perrod G, Samaha E, Benosman H, Abbes L, et al. Over-the-scope clip (OTSC) reduces surgery rate in the management of iatrogenic gastrointestinal perforations. Endosc Int Open. 2017;5(05):E389–E94. https://doi.org/10.1055/s-0043-104862.
Brandler J, Baruah A, Zeb M, Mehfooz A, Pophali P, Wong Kee Song L, et al. Efficacy of over-the-scope clips in management of high-risk gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2017; https://doi.org/10.1016/j.cgh.2017.07.020.
Wedi E, von Renteln D, Gonzalez S, Tkachenko O, Jung C, Orkut S, et al. Use of the over-the-scope-clip (OTSC) in non-variceal upper gastrointestinal bleeding in patients with severe cardiovascular comorbidities: a retrospective study. Endosc Int Open. 2017;5(09):E875–E82. https://doi.org/10.1055/s-0043-105496.
•• Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80(4):610–22. https://doi.org/10.1016/j.gie.2014.03.049. This is international multicenter study. A total of 188 patients (108 GI fistulae, 48 GI perforations, 32 GI leaks) were included. Long-term success of OTSC treatment was achieved in 60.2% of patients during a median follow-up of 146 days.
Kobara H, Mori H, Fujihara S, Nishiyama N, Chiyo T, Yamada T, et al. Outcomes of gastrointestinal defect closure with an over-the-scope clip system in a multicenter experience: an analysis of a successful suction method. World J Gastroenterol. 2017;23(9):1645–56. https://doi.org/10.3748/wjg.v23.i9.1645.
Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, et al. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19(18):2752–60. https://doi.org/10.3748/wjg.v19.i18.2752.
Valli PV, Pohl D, Fried M, Caduff R, Bauerfeind P. Diagnostic use of endoscopic full-thickness wall resection (eFTR)-a novel minimally invasive technique for colonic tissue sampling in patients with severe gastrointestinal motility disorders. Neurogastroenterol Motil. 2017;2017(59):e13153–6. https://doi.org/10.1111/nmo.13153.
Nishiyama N, Mori H, Kobara H, Fujihara S, Ayaki M, Miyai Y, et al. Minimal incision-assisted full-thickness sampling with over-the-scope clip targeting intestinalneuronal malformation. Endoscopy. 2017;49(S 01):E103–E4. https://doi.org/10.1055/s-0043-100626.
Dinelli M, Omazzi B, Andreozzi P, Zucchini N, Redaelli A, Manes G. First clinical experiences with a novel endoscopic over-the-scope clip system. Endosc Int Open. 2017;5(03):E151–E6. https://doi.org/10.1055/s-0043-101692.
Schmidt A, Riecken B, Damm M, Cahyadi O, Bauder M, Caca K. Endoscopic removal of over-the-scope clips using a novel cutting device: a retrospective case series. Endoscopy. 2014;46(09):762–6. https://doi.org/10.1055/s-0034-1365493.
•• Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag HJ, Messmann H, et al. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut. 2017:gutjnl-2016-313677. https://doi.org/10.1136/gutjnl-2016-313677. This is a non-randomized, prospective multicenter study. All resections were performed using the FTRD. Indications for eFTR were difficult adenomas (non-lifting and/or at difficult locations), early cancers and subepithelial tumours. R0 resection rate was 77.7%. In general, R0 resection rate was higher with lesions ≤2 cm vs >2 cm (81.2% vs 58.1%, p=0.0038). Adverse event rate was 9.9% with a 2.2% rate of emergency surgery.
Tanaka S, Terasaki M, Hayashi N, Oka S, Chayama K. Warning for unprincipled colorectal endoscopic submucosal dissection: accurate diagnosis and reasonable treatment strategy. Dig Endosc. 2013;25(2):107–16. https://doi.org/10.1111/den.12016.
Rahmi G, Hotayt B, Chaussade S, Lepilliez V, Giovannini M, Coumaros D, et al. Endoscopic submucosal dissection for superficial rectal tumors: prospective evaluation in France. Endoscopy. 2014;46(08):670–6. https://doi.org/10.1055/s-0034-1365810.
Kiriyama S, Saito Y, Yamamoto S, Soetikno R, Matsuda T, Nakajima T, et al. Comparison of endoscopic submucosal dissection with laparoscopic-assisted colorectal surgery for early-stage colorectal cancer: a retrospective analysis. Endoscopy. 2012;44(11):1024–30. https://doi.org/10.1055/s-0032-1310259.
Nakamura F, Saito Y, Sakamoto T, Otake Y, Nakajima T, Yamamoto S, et al. Potential perioperative advantage of colorectal endoscopic submucosal dissection versus laparoscopy-assisted colectomy. Surg Endosc. 2015;29(3):596–606. https://doi.org/10.1007/s00464-014-3705-5.
Silva GL, de Moura EG, Bernardo WM, Leite de Castro V, Morais C, Baba ER, et al. Endoscopic versus surgical resection for early colorectal cancer-a systematic review and meta-analysis. J Gastrointest Oncol. 2016;7(3):326–35. https://doi.org/10.21037/jgo.2015.10.02.
Fischer A, Knoop RF, Walker C, Thimme R, Richter-Schrag HJ. Resection of a large rectal polyp with the simultaneous combination of snare polypectomy and full-thickness resection device resection. Endoscopy. 2015;47(Suppl 1):E607–E8. https://doi.org/10.1055/s-0035-1569658.
Jacob H, Toyonaga T, Ohara Y, Tsubouchi E, Takihara H, Baba S, et al. Endoscopic submucosal dissection of cecal lesions in proximity to the appendiceal orifice. Endoscopy. 2016;48(09):829–36. https://doi.org/10.1055/s-0042-110396.
Loske G, Schorsch T, Daseking E, Martens E, Müller CT. Small intestine grasped by over-the-scope-clip during attempt to close an iatrogenic colonicperforation. Endoscopy. 2016;48(Suppl 1 UCTN):E26–7. https://doi.org/10.1055/s-0041-110594.
Stavropoulos SN, Modayil R, Friedel D. Current applications of endoscopic suturing. World J Gastrointest Endosc. 2015;7(8):777–89. https://doi.org/10.4253/wjge.v7.i8.777.
Sharaiha RZ, Kumta NA, DeFilippis EM, Dimaio CJ, Gonzalez S, Gonda T, et al. A large multicenter experience with endoscopic suturing for management of gastrointestinal defects and stent anchorage in 122 patients: a retrospective review. J Clin Gastroenterol. 2016;50:388–92. https://doi.org/10.1097/MCG.0000000000000336.
Azzolini F, Cecinato P, Iori V, De Marco L, Sassatelli R. Endoscopic full-thickness resection for suspected residual rectal neuroendocrine tumor and closure of the defect with a new suturing system. Endoscopy. 2015;47(Suppl 1):E556–7. https://doi.org/10.1055/s-0034-1393384.
Kantsevoy SV, Bitner M, Mitrakov AA, Thuluvath PJ. Endoscopic suturing closure of large mucosal defects after endoscopic submucosal dissection is technically feasible, fast, and eliminates the need for hospitalization (with videos). Gastrointest Endosc. 2014;79(3):503–7. https://doi.org/10.1016/j.gie.2013.10.051.
Mori H, Kobara H, Fujihara S, Nishiyama N, Rafiq K, Oryu M, et al. Feasibility of pure EFTR using an innovative new endoscopic suturing device: the double-arm-bar suturing system (with video). Surg Endosc. 2014;28(2):683–90. https://doi.org/10.1007/s00464-013-3266-z.
Mori H, Rafiq K, Kobara H, Fujihara S, Nishiyama N, Oryuu M, et al. Innovative noninsufflation EFTR: sufficient endoscopic operative field by mechanical counter traction device. Surg Endosc. 2013;27(8):3028–34. https://doi.org/10.1007/s00464-013-2846-2.
Mori H, Kobara H, Tsushimi T, Fujihara S, Nishiyama N, Matsunaga T, et al. Reduction effect of bacterial counts by preoperative saline lavage of the stomach in performing laparoscopic and endoscopic cooperative surgery. World J Gastroenterol. 2014;20(42):15763–70. https://doi.org/10.3748/wjg.v20.i42.15763.
Goto O, Shimoda M, Sasaki M, Kiguchi Y, Mitsunaga Y, Akimoto T, et al. Potential for peritoneal cancer cell seeding in endoscopic full-thickness resection for early gastric cancer. Gastrointest Endosc. 2017; https://doi.org/10.1016/j.gie.2017.08.036.
Mori H, Kobara H, Fujihara S, Nishiyama N, Ayaki M, Chiyo T, et al. Innovative pure non-exposed endoscopic full-thickness resection using an endoscopic suturing device. Gastrointest Endosc. 2016;84(1):178–9. https://doi.org/10.1016/j.gie.2016.02.001.
Mori H, Rahman A, Kobara H, Fujihara S, Nishiyama N, Ayaki M, et al. Current status of exposed endoscopic full-thickness resection and further development of non-exposed endoscopic full-thickness resection. Digestion. 2017;95(1):6–15. https://doi.org/10.1159/000452352.
Acknowledgements
This article is dedicated to the memory of Dr. Hirohito Mori, Dr. Hideki Kobara, and Dr. Noriko Nishiyama who were our teachers and role models. They were always the first to try innovative ideas and inspired those around them to never stop challenging themselves.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Surgery and Surgical Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Fujihara, S., Mori, H., Kobara, H. et al. Endoscopic Full-Thickness Resection for Colorectal Neoplasm: Current Status and Future Directions. Curr Colorectal Cancer Rep 14, 22–30 (2018). https://doi.org/10.1007/s11888-018-0399-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-018-0399-4