Abstract
Purpose of Review
The purpose of this article is to serve as a practical guide to computed tomography (CT)–guided pericardiocentesis and to discuss the role of this approach in current clinical practice. An overview of indications, technique, advantages, and limitations specific to CT-guided pericardiocentesis will be provided. The reader will have an enhanced understanding of the use of this imaging modality to guide pericardial drainage.
Recent Findings
Use of CT guidance to drain the pericardial space is safe, especially when adequate echocardiographic evaluation is precluded and when echocardiography-guided pericardiocentesis is deemed unsafe and or not feasible.
Summary
Our review and experience indicate that CT-guided pericardiocentesis is technically successful in more than 94% of patients, with a low risk (<1%) of significant complications. CT-guided pericardiocentesis is therefore a viable alternative when echocardiographic guidance is insufficient and can obviate the need for surgery in most patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The decision to drain a pericardial effusion is based on clinical need and the availability of the tools and expertise needed to safely perform the drainage. Although most cases of pericardial drainage are performed by cardiologists using echocardiography as a guide, computed tomography (CT) guidance can also be used. In this article, we will describe the role that CT guidance can play in pericardiocentesis.
Anatomy and Pathophysiology
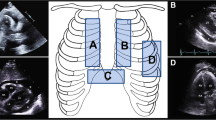
The pericardium, a fibroserous sac surrounding the heart, plays a crucial role in protecting and maintaining cardiac function. The serous visceral pericardium is adherent to the surface of the heart, and the fibrous parietal pericardium is loosely applied over it. This creates a virtual space between the two layers. The pericardial layers surround the cardiac chambers and blend with the adventitial layer of the great vessels at the base of the heart superiorly and with the central tendon within the diaphragm inferiorly. Physiologically, the space between the two layers, i.e., the pericardial sac, is small and normally contains 15 to 20 cc of fluid, which acts as a lubricant and minimizes friction between the two layers [1]. Except for the small spaces that exist along the pericardial recesses formed by reflections of the pericardium, elsewhere these two layers appear as one on imaging (Fig. 1A).
Axial CT images of the chest. A Normal pericardium, with the two layers of pericardium abutting one another and seen as a single layer (white arrow). B Pathological accumulation of fluid in the pericardial cavity separating the visceral (red line) and parietal (blue line) layers of the pericardium. Internal mammary vessels (interrupted white arrows) identified here should be avoided during pericardiocentesis
Pericardial effusion is defined as a greater than normal volume of fluid in the pericardial space. With pathological accumulation of fluid, the two pericardial layers are separated by the increase in the amount of collection in the pericardial space (Fig. 1B). The clinical significance of pericardial effusion is characterized by the effect it has on the diastolic filling of the cardiac chambers, particularly the right atrium and the right ventricle. Pericardial effusion may be classified based on the rate of fluid accumulation (slow vs rapid), the pattern of distribution around the cardiac chambers (localized vs. circumferential), the hemodynamic effect it has at the time of diagnosis (asymptomatic, mild-to-moderate symptoms, or tamponade), and its composition (transudative, exudative, hemorrhagic, or chylous).
Cardiac ultrasound (also called echocardiography) is a simple, widely available, semiquantitative tool that is effective in the initial diagnosis of pericardial effusion and in evaluating its effect on the heart chambers [2].
Echocardiography-Guided Pericardiocentesis
Pericardiocentesis, meaning puncture of the pericardial space to aspirate pericardial fluid, is used as an initial diagnostic assay to determine the composition of the fluid and the cause of accumulation. With adequate drainage of such fluid, therapeutic relief of symptoms can also be achieved. Subsequent therapy is then directed at the underlying etiology and is based on the recurrence of symptoms and follow-up imaging. Diagnostic indications may include suspected infectious or neoplastic etiology, whereas therapeutic indications may include cardiac tamponade that requires immediate drainage or symptomatic moderate to large pericardial effusions that are refractory to medical therapy.
Unguided (blind) percutaneous pericardiocentesis, commonly in use before the 1980s, was associated with mortality rates as high as 8.5% [3]. With the introduction of echocardiography in the 1970s, noninvasive visualization of the pericardial effusion and evaluation of its effect on cardiac function became possible. Since then, echocardiography has remained the predominant modality used to evaluate pericardial effusion and to assist in targeted pericardiocentesis.
Echocardiography allows for identification of the deepest accessible pocket suitable for aspiration. When such aspiration is deemed necessary, the operator uses the probe to select the optimal site for needle insertion in the chest wall (where the largest pericardial fluid accumulation is seen closest to the skin) and marks this site. The probe is then put aside and the operator inserts the needle toward the pericardial space while maintaining continuous aspiration using a syringe. Needle insertion is stopped at the first instance of fluid flash in the syringe. This technique is reported to have high success rates and a low incidence of minor (3.5%) and major (1.2%) complications [4]. However, with this technique, the advancing needle is not visualized in real time on the echocardiography monitor. Needle entry into the pericardial space is assumed once a flash of fluid is aspirated, and this warns the operator to stop any further needle push. Without this flash of fluid, the operator may continue to advance the needle and risk injuring underlying epicardium and myocardium. An alternative to this technique involves continuous visualization of needle progress from the subcutaneous tissues into the pericardial space using real-time echocardiographic guidance. With this technique, needle progress is adjusted as the entry into the pericardial space is visualized on the monitor in real time. However, this method requires the operator to have superior hand-hand-eye coordination. The operator uses one hand to hold the echocardiography probe and the other hand to advance the needle, all while watching the monitor and constantly adjusting the needle trajectory to match the intended path. For trained operators, this technique allows for effective drainage of the pericardial effusion, even among patients in acute distress. In a study assessing the use of this technique in patients with cardiac tamponade, real-time continuous visualization of the needle insertion using parasternal medial-to-lateral in-plane access allowed operators to successfully drain pericardial effusions within 4 to 6 min without complications [5].
Although these echocardiography-assisted techniques remain the mainstay approach for pericardial effusion drainage, these methods do have limitations. In such circumstances, a CT-guided approach should be considered as an alternative before surgical drainage is performed.
Limitations of Echocardiography-Guided Pericardiocentesis
During echocardiography, real-time visualization of the access needle is operator dependent. As such, failure rates are reported to be as high as 56% during early practice, although these numbers do improve modestly as operators gain experience [6]. Echocardiography guidance can also be limited by the narrow near-field visibility of commonly used probes and can be restricted by the presence of ribs, lungs, and artifacts. For example, needle visualization can be obscured by hyperinflated lungs in patients with chronic obstructive pulmonary disease; by subcutaneous emphysema secondary to trauma or infection; by subcutaneous air, chest wall bandages, or hematoma after surgery; or by increased subcutaneous and mediastinal fat in obese patients [7].
Interpretation of the feasibility of echocardiography-guided drainage can be highly subjective among operators. These procedures can be particularly difficult in patients who have just undergone open heart surgery, as the position of such patients cannot be easily changed to allow for adequate access to the chest wall. In addition, sonolucent fluid that is easily seen in spaces adjacent to the heart, such as pleural effusions seen in intercostal evaluation and ascites in subxiphoid evaluation, can be mistaken for pericardial effusion. Loculated posterior pericardial effusion can also be obscured by the lungs and mediastinum. In such cases, choosing an appropriate site to perform pericardiocentesis using echocardiography guidance is not possible. CT, on the other hand, can provide a cross-sectional overview of the entire pericardial space and the adjacent spaces. Acquisition of CT images is also not substantially affected by the operator, and the quality of such images is not affected by the patient-related factors described earlier.
Fat attenuates ultrasound echoes more than fluid does. This limits image quality in echocardiography, particularly when there is excess distribution of adipose tissue in the subcutaneous plane. This effect on images is worsened among patients who weigh more than 300 lbs because the ultrasound waves have to penetrate through the increased thickness of subcutaneous tissue to reach internal structures such as pericardial effusion [8]. X-rays, however, are less attenuated by fat. Thus, despite the presence of excess subcutaneous adipose tissue in obese patients, CT images can easily demonstrate the location of a pericardial effusion (Fig. 2).
A summary of scenarios with the preferred choice of imaging guidance for pericardiocentesis is provided in Table 1. The availability of resources and experts trained in using these imaging modalities will vary across institutions; thus, a collaborative approach is needed to identify the safest available method.
Merits of CT-Guided Pericardiocentesis
CT is an alternative imaging modality for guiding pericardiocentesis in patients with suboptimal acoustic windows. When the evaluation of potential needle entry site and trajectory is precluded by suboptimal echocardiographic evaluation, CT can allow the operator to identify a safe tract into the space. CT, unlike echocardiography, provides excellent differentiation among air, soft tissues, fluid, calcification, metal, and bones. For example, air in or adjacent to the pericardium is highly reflective of ultrasound waves and creates less discernible shadows, thus precluding evaluation of deeper anatomy. CT, on the other hand, can accurately display the distribution of air, allowing the operator to plan an access route to the pericardial space (Fig. 3). When echocardiography cannot guide an operator to manage pneumopericardium, as reported by Ibrahim et al. [9], even a tension pneumopericardium, requiring emergent drainage, can be easily accomplished using CT guidance. Similarly, pericardial calcification can cause significant acoustic shadowing in echocardiography and reduce the visibility of the pericardial space, whereas CT images accurately depict the presence and distribution of pericardial calcification and effusion and can therefore be used to guide needle insertion into the pericardial space [10].
Axial CT images (A, B, C, D) acquired during pericardiocentesis for pneumopericardium. A Axial CT image in lung window demonstrating accumulation of air anteriorly within the pericardial cavity. B, C, D Axial CT images in soft-tissue window demonstrating anterior needle entry (B), needle tip abutting the anterior pericardium (C), followed by drainage catheter placement (D). E, F Preprocedural (E) and postprocedural (F) chest radiographs demonstrate the presence (white arrow) and resolution of pneumopericardium, respectively
CT imaging also offers high-resolution anatomical detail of structures adjacent to the pericardial space such as the lungs, pleura, airway, great vessels, diaphragm, liver, and stomach. It can easily distinguish between pleural effusions and ascites that can be seen adjacent to these effusions. Images obtained after CT-guided pericardiocentesis also allow for compressive evaluation of any residual fluid within or outside the pericardial space. Research has shown that approximately 21% of patients undergoing CT-guided pericardiocentesis also require pleural drainage [11]. Because CT-guided pericardiocentesis is often performed by radiologists who are also trained in pleural drainage, drainage of both spaces can often be accomplished during the same procedure, allowing for quicker relief of symptoms. In addition, CT images acquired after pericardiocentesis facilitate early detection of complications. CT images can offer reassurance regarding minor complications such as small asymptomatic pneumothoraces, which are typically managed conservatively, and can allow operators to perform immediate drainage of symptomatic large pneumothoraces.
In imaging-guided pericardiocentesis with real-time visual feedback, needle detection in echocardiography images is difficult. Ultrasound echoes are scattered by the needle, which reduces the needle visibility, especially with linear or semilinear anatomical structures near the needle. In addition, difficulties with aligning the needle in one hand and the transducer in the other hand can lead to incorrect identification of the needle tip. Repeated manipulation and reinsertion of the needle can make the procedure more painful for the patient. Such repeated attempts can also result in inadvertent pericardial fenestrations and efflux of pericardial fluid into the thoracic cavity [12]. Identification of the needle tip and shaft is easier with CT, thus enabling calculated incremental advancement of the needle and earlier confirmation that the needle tip is in the pericardial space. Thus, with adequate training for operators, real-time CT-guided drainage can be an efficient tool to drain the pericardial space, especially as a phantom study demonstrated that CT-guided fluoroscopic procedure times were similar to those of ultrasound-based techniques [13].
Although most diagnostic echocardiography procedures are performed by cardiologists with occasional requests to also drain the pericardial space, most radiologists are trained to perform ultrasound-guided biopsies and drainage of collections. Radiologists who are comfortable using both ultrasound and CT guidance for drainage may opt to use continuous ultrasound guidance using curvilinear probes in intercostal or subcostal spaces to visualize the progress of the needle from the skin to the pericardial space in real time and then use CT guidance for placement of the guidewire and drainage catheter. CT imaging after the drainage procedure also helps in the evaluation and management of complications before patients are returned to their nursing unit for further monitoring. At the authors’ institution, radiologists routinely use a combination of ultrasound and CT to perform imaging-guided pericardiocentesis with high success rates and low complication rates [14]. To assist the operator in using both imaging modalities, screens displaying the ultrasound and CT images are typically positioned to the right of the patient lying on the CT scanning table, with the operator standing on the left side [7].
Echocardiography-guided pericardiocentesis is often performed through a left parasternal or subxiphoid access. Overlying lung can preclude the operator’s ability to choose a more lateral intercostal approach to drain a posterior pericardial effusion. CT guidance, however, offers additional access options to reach the pericardial space, as the distribution and nature of the pericardial effusion can be easily assessed on CT. Klein et al. [15] and Davit et al. [16] reported that approximately 25 to 46% of CT-guided accesses in their patients were through the intercostal space, 12 to 26% were through a right parasternal approach, and 15% were through a left subcostal approach. In parasternal approach, there is a risk of injury to internal mammary arteries; CT images can be used to locate (Fig. 1B) and plan a needle trajectory that can avoid these vessels. While using an intercostal approach, it is important to stay just above a rib, to avoid injury to intercostal arteries. CT is also of use for loculated pericardial effusions. When the effusion is loculated, especially in the postoperative setting, CT imaging allows precise evaluation of any residual pericardial fluid after initial pericardiocentesis and can assist in the drainage of additional loculations to achieve adequate symptom relief. CT imaging also allows operators to see the distribution of pericardial calcification and to identify interruptions in the calcification through which a needle could be guided to drain pericardial fluid.
Visualization of the needle tip during CT-guided procedures allows for adjustments in the needle trajectory, ensuring accurate access to the pericardial space and minimizing the risk of complications. This is achieved by either incrementally advancing the needle with intermittent acquisition of CT images (intermittent CT fluoroscopy) or continuously advancing the needle with uninterrupted acquisition of CT images (continuous CT fluoroscopy). With the intermittent technique, after each incremental needle push, multiple CT images, centered on the needle, are acquired. The operator reviews the images in the CT suite, makes immediate adjustments to the needle trajectory if needed, and then makes another short needle push. This process is repeated until the needle tip enters the pericardial space. With this technique, the operators either leave the procedure room or move away from the patient and CT gantry while images are being acquired to reduce their radiation exposure. In the continuous technique, there is steady insertion of the needle with frequent adjustments based on updated images acquired by uninterrupted CT scanning centered on the needle. Operators employing this technique often use forceps to hold the needle to avoid direct radiation exposure to their fingers, but they must remain in close proximity to the patient and CT gantry during this process and are thus exposed to higher radiation levels than they are when using the first technique.
While the echocardiography-guided technique requires the operator to hold the probe in one hand and the needle in the other, the CT-guided technique allows the operator to use both hands to make fine adjustments of the needle. Thus, for radiologists proficient in needle-based techniques such as aspirations, drainage catheter placements, and needle biopsies using CT guidance, CT-guided pericardiocentesis can be easily incorporated into their repertoire.
Step-by-Step Process of CT-Guided Pericardiocentesis
An overview of the step-by-step process for CT-guided pericardiocentesis used at our institution is shown in Fig. 4. This procedure is performed under continuous monitoring of vital signs by a dedicated nurse. For anxious patients, moderate sedation can be provided.
Axial CT images show step-by-step approach to access the pericardial sac during CT-guided pericardiocentesis. A A radiopaque grid is placed over the skin. B The needle trajectory between the skin entry site and the pleural effusion is planned with a left intercostal approach. C The tip of the needle (arrow) enters the pericardial effusion. D A drainage catheter (arrow) is placed in the posterior pericardial effusion
A radiopaque skin grid marker is placed on the skin surface over the left lower anterior chest wall. Initial surveillance CT images are then acquired. This allows the operator to plan a safe needle trajectory and choose the skin entry site, placing a mark at the site. The skin grid is then removed, and the procedure site is prepared and draped using sterile technique. Local anesthesia is achieved by intradermal and subcutaneous infiltration of 1–2% lidocaine hydrochloride. A 21G needle is then advanced approximately 2 to 3 cm into the tissue until the needle anchors into the soft tissues along the chosen path. The intermittent CT fluoroscopy technique is then used for needle guidance. The operator moves away from the CT gantry and the patient and triggers the radiation exposure pedal. This generates multiple contiguous axial images centered on the needle tip/entry site. After confirmation of satisfactory trajectory, the needle is advanced incrementally, with periodic acquisition of CT images to enable the fine adjustments needed to ensure safe entry into the pericardial space. A 0.018-inch diameter guidewire is then inserted through the needle into the pericardial space, and the placement is confirmed with CT images. Using the Seldinger technique, the operator then exchanges the needle for a 4F micropuncture catheter and removes the wire. Aspiration is then performed using this catheter. If placement of a drainage catheter is deemed necessary, a 0.035-inch diameter guidewire is then inserted. The micropuncture catheter is removed and a dedicated drainage catheter is placed over this guidewire. We use this micropuncture system, Seldinger technique, and tract dilation to minimize damage to the soft tissues and decrease the risk of bleeding. The catheter is secured to the skin with nonabsorbable sutures and then connected to a bag for external drainage. After adequate drainage of the pericardial fluid, CT images are acquired across the entire cardiac silhouette at the end of the procedure to assess for complications such as pneumothorax and hematoma, to ensure satisfactory positioning of the drainage catheter, and to document the presence or absence of residual effusion and undrained loculations.
Data on CT-Guided Pericardiocentesis
CT began to play an important role in the evaluation of pericardial effusion within the first decade of its introduction into clinical practice [17]. One of the early uses of CT guidance to place a needle into pericardial space is in a report by Sandring et al. [18]. They reported successful pericardial drainage using CT-guided puncture in three patients. Since then, a number of case series have reported the advantages of CT-guided pericardiocentesis (Table 2) [11, 14,15,16, 19,20,21,22,23,24,25, 26••, 27, 28•]. Table 2, which includes information from these case series (digitally accessible abstracts and full papers), summarizes the impact of CT guidance on draining the pericardial space. The indications for CT-guided pericardiocentesis in these studies ranged from acquiring a sample of the pericardial fluid for analysis in cases with unknown diagnoses to relieving symptoms in patients with known etiologies such as recent cardiac surgery. Failure was rare in these reports. In the few instances in which the pericardial space was not adequately drained using CT guidance, the challenge was attributed to septated/organized effusions [19, 20] or expanding chest wall hematoma [14]. In a systematic report limited to full papers reporting on at least 10 patients, Vilela et al. [29] found that the technical success rates of CT-guided pericardiocentesis ranged from 94 to 100%.
Complications during CT-guided procedures are rare and often minor, usually requiring no major interventions. In a large series of 1127 therapeutic echocardiography-guided pericardiocentesis procedures, 5 pneumothoraces requiring chest tube placement were reported [4]. Comparatively, among the 1065 CT-guided pericardiocentesis procedures summarized in Table 2, there was one reported large pneumothorax requiring drainage [16]. Significant pneumothoraces are rare, likely due to the ability of CT images to demonstrate pleural reflection and lung edges more clearly than echocardiography, thus allowing the operator to choose a needle trajectory away from the pleura. In echocardiography-guided pericardiocentesis, the risk of myocardial injury is also higher, with difficult procedures requiring multiple trials, especially in the presence of loculation [30]. Needle trajectory is often planned to be tangential to the myocardial contour, and with improved visualization of the needle tip, injury to the myocardium and cardiac chambers is rare (less than 1%) with CT-guided pericardiocentesis. Overall, CT allows for better detection and delineation of complications, including pneumothorax (small and large) and hematoma (mediastinal and subcutaneous). CT is also more effective in identifying the cause of nonfunctioning drainage catheters, such as incorrect placement or kinks in the catheter.
Limitations of CT-Guided Pericardiocentesis
CT scanners are usually located in the radiology department. When a patient requires CT-guided pericardiocentesis, the patient and any monitoring equipment therefore need to be moved. In emergent situations, efforts must be made to hemodynamically stabilize the patient to allow for transport, planning, and performance of the procedure. In addition, the availability of CT after hours and access to appropriately trained experts can be limited. This lack of portability and limited availability of trained operators can make this tool inaccessible to patients in need of emergent pericardiocentesis. Thus, echocardiography-guided pericardiocentesis still remains the first choice [31].
Unlike echocardiography-guided procedures, CT-guided procedures use ionizing radiation, thus exposing the patient and operators to radiation. In a report on CT-guided pericardiocentesis performed in 46 patients, the median total effective radiation exposure to the patient after each procedure was 3.3 (interquartile range 2.4–5.2) mSv [20]. CT-guided procedures are therefore not routinely recommended for pregnant patients, especially during the first trimester when the risk for fetal radiation-induced teratogenesis and intellectual disability is the highest [32]. While the main source of radiation exposure to the patient is the primary X-ray beam, the exposure to the operator is mostly from scatter radiation. To minimize this exposure to scatter radiation, operators should use the lowest possible number of CT image acquisition triggers to safely guide needle entry. Operators should also maintain a safe distance from the CT gantry during each such acquisition and should use personal shielding such as lead aprons, lead glasses, and thyroid shields at all times during the procedure [33].
Finally, unlike echocardiographic assessment, CT imaging can underestimate the degree of septations and in the presence of innumerable septations can result in failed drainage of fluid in spite of catheter placement [19, 20]. Thus, echocardiographic evaluation should always be performed before considering CT-guided procedures.
Conclusion
CT guidance represents a promising approach in pericardial interventions. This technique has the potential to improve the accuracy, safety, and success rates of pericardiocentesis, ultimately leading to better outcomes for patients with pericardial disorders, especially when echocardiography guidance is not feasible. Given the increasing number of invasive procedures performed and the importance of addressing pericardial effusions precisely and safely, CT-guided pericardiocentesis should be considered as a viable alternative to echocardiographic guidance.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levene G, Kaufman SA. The roentgen diagnosis of pericardial effusion, with special reference to the appearance of the barium-filled esophagus and the cardiohepatic angle. Radiology. 1951;57(3):373–83. https://doi.org/10.1148/57.3.373.
Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34(16):1186–97. https://doi.org/10.1093/eurheartj/ehs372.
Callahan JA, Seward JB, Nishimura RA, Miller FA Jr, Reeder GS, Shub C, et al. Two-dimensional echocardiographically guided pericardiocentesis: experience in 117 consecutive patients. Am J Cardiol. 1985;55(4):476–9. https://doi.org/10.1016/0002-9149(85)90397-2.
Tsang TS, Enriquez-Sarano M, Freeman WK, Barnes ME, Sinak LJ, Gersh BJ, et al. Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile, practice patterns, and outcomes spanning 21 years. Mayo Clin Proc. 2002;77(5):429–36. https://doi.org/10.4065/77.5.429.
Osman A, Wan Chuan T, Ab Rahman J, Via G, Tavazzi G. Ultrasound-guided pericardiocentesis: a novel parasternal approach. Eur J Emerg Med. 2018;25(5):322–7. https://doi.org/10.1097/MEJ.0000000000000471.
Chandraratna PA, Reid CL, Nimalasuriya A, Kawanishi D, Rahimtoola SH. Application of 2-dimensional contrast studies during pericardiocentesis. Am J Cardiol. 1983;52(8):1120–2. https://doi.org/10.1016/0002-9149(83)90544-1.
Karuppasamy K. Real-time image-guided pericardial drain placement. American College of Cardiology website. https://www.acc.org/Latest-in-Cardiology/Articles/2017/07/12/07/04/Real-Time-Image-Guided-Pericardial-Drain-Placement. Published July 12, 2017. Accessed 3 Aug 2023.
Uppot RN. Technical challenges of imaging & image-guided interventions in obese patients. Br J Radiol. 2018;91(1089):20170931. https://doi.org/10.1259/bjr.20170931.
Ibrahim AO, Jaber F, Alghizzawi M, Metzinger M, Asif T. CT-guided pericardiocentesis in a case of tension pneumopericardium and tamponade secondary to an enteropericardial fistula. J Am Coll Cardiol Case Rep. 2023;18:101909. https://doi.org/10.1016/j.jaccas.2023.101909.
Cosyns B, Plein S, Nihoyanopoulos P, Smiseth O, Achenbach S, Andrade MJ, et al. European Association of Cardiovascular Imaging (EACVI) position paper: multimodality imaging in pericardial disease. Eur Heart J Cardiovasc Imaging. 2015;16(1):12–31. https://doi.org/10.1093/ehjci/jeu128.
Palmer SL, Kelly PD, Schenkel FA, Barr ML. CT-guided tube pericardiostomy: a safe and effective technique in the management of postsurgical pericardial effusion. AJR Am J Roentgenol. 2009;193(4):W314–20. https://doi.org/10.2214/AJR.08.1834.
Hongo T, Sugiyama H, Naito H, Nakao A. Successful computed tomography-guided pericardiocentesis after performing a failed conventional transthoracic echocardiography-guided approach: a case report. J Emerg Med Case Rep. 2020;11(2):39–42. https://doi.org/10.33706/jemcr.632857.
Sheafor DH, Paulson EK, Kliewer MA, DeLong DM, Nelson RC. Comparison of sonographic and CT guidance techniques: does CT fluoroscopy decrease procedure time? AJR Am J Roentgenol. 2000;174(4):939–42. https://doi.org/10.2214/ajr.174.4.1740939.
Gallagher S, Syed F, Gurajala R, Gill A, Levitin A, Karuppasamy K. Real-time image-guided drainage of postsurgical pericardial effusion is an effective alternative to surgical window. J Vasc Interv Radiol. 2021;32(5):S153. https://doi.org/10.1016/j.jvir.2021.03.366.
Klein SV, Afridi H, Agarwal D, Coughlin BF, Schielke LH. CT directed diagnostic and therapeutic pericardiocentesis: 8-year experience at a single institution. Emerg Radiol. 2005;11(6):353–63. https://doi.org/10.1007/s10140-004-0389-5.
David S, Mansoubi H, Hoey E, Agrawal B, Tasker A. CT guided pericardiocentesis: a UK experience. ECR 2010. Poster No. C-0494. https://doi.org/10.1594/ecr2010/C-0494.
Tomoda H, Hoshiai M, Furuya H, Oeda Y, Matsumoto S, Tanabe T, et al. Evaluation of pericardial effusion with computed tomography. Am Heart J. 1980;99(6):701–6. https://doi.org/10.1016/0002-8703(80)90618-3.
Sandring KH, Müller C. CT-gestützte perkutane Punktion und Drainage von Perikardergüssen [CT-guided percutaneous puncture and drainage of pericardial effusion]. Radiol Diagn (Berl). 1989;30(6):643–6.
Ceviz M, Çolak A, Becit N, Kaya U, Ogul H. Computed tomography-guided drainage of pericardial effusion. Turk J Thorac Cardiovasc Surg. 2014;22(3):553–7.
Neves D, Silva G, Morais G, Ferreira N, Carvalho M, Gama Ribeiro V, et al. Computed tomography-guided pericardiocentesis - a single-center experience [erratum in Rev Port Cardiol. 2016;35(6):392. https://doi.org/10.1016/j.repc.2016.05.001]. Rev Port Cardiol. 2016;35(5):285–90. https://doi.org/10.1016/j.repc.2015.11.015.
Duvernoy O, Magnusson A. CT-guided pericardiocentesis. Acta Radiol. 1996;37(5):775–8. https://doi.org/10.1177/02841851960373P269.
Tam A, Ensor JE, Snyder H, Gupta S, Durand JB, Wallace MJ. Image-guided drainage of pericardial effusions in oncology patients. Cardiovasc Intervent Radiol. 2009;32(6):1217–26. https://doi.org/10.1007/s00270-009-9594-7.
Eichler K, Zangos S, Thalhammer A, Jacobi V, Walcher F, Marzi I, et al. CT-guided pericardiocenteses: clinical profile, practice patterns and clinical outcome. Eur J Radiol. 2010;75(1):28–31. https://doi.org/10.1016/j.ejrad.2010.04.012.
Syed F, Slaughter R, Tjahjadi C, Hansen M, Raffel O. Computed tomography guided pericardiocentesis in adults: a single centre experience of 44 procedures. Heart Lung Circ. 2011;20(suppl 2):S165. https://doi.org/10.1016/j.hlc.2011.05.411.
Nour-Eldin NA, Alsubhi M, Gruber-Rouh T, Vogl TJ, Kaltenbach B, Soliman HH, et al. CT-guided drainage of pericardial effusion after open cardiac surgery. Cardiovasc Intervent Radiol. 2017;40(8):1223–8. https://doi.org/10.1007/s00270-017-1624-2.
•• Ingber RB, Lodhi U, Mootz J, Siegel A, Al-Roubaie M, Greben C. Comparing outcomes of CT-guided percutaneous pericardial drainage with surgical pericardial window in patients with symptomatic pericardial effusions. Acad Radiol. 2023 Mar 14:S1076–6332(23)00087–9. https://doi.org/10.1016/j.acra.2023.02.014. Findings from this study suggest that complications from CT-guided percutaneous pericardial drainage are significantly lower compared to subxiphoid surgical pericardial window.
Bruning R, Muehlstaedt M, Becker C, Knez A, Haberl R, Reiser M. Computed tomography-fluoroscopy guided drainage of pericardial effusions: experience in 11 cases. Invest Radiol. 2002;37(6):328–32. https://doi.org/10.1097/00004424-200206000-00004.
• Khashper A, Shelef I, Taragin BH, Smolikov A. Therapeutic computed tomography-guided pericardiocentesis: lessons learned based on a 7-year single-center experience. J Comput Assist Tomogr. 2021 Jul-Aug 01;45(4):643–648. https://doi.org/10.1097/RCT.0000000000001190. Findings from this study suggest that CT-guided pericardiocentesis is safe and effective in managing patients requiring therapeutic pericardial drainages.
Vilela EM, Ruivo C, Guerreiro CE, Silva MP, Ladeiras-Lopes R, Caeiro D, et al. Computed tomography-guided pericardiocentesis: a systematic review concerning contemporary evidence and future perspectives. Ther Adv Cardiovasc Dis. 2018;12(11):299–307. https://doi.org/10.1177/1753944718792413.
Shaalan AM, Ezeldin TH, Elwakeel EE, Salem EF. Predictors of cardiac injury during pericardiocentesis. Egypt J Surg. 2022;41(3):1009–18. https://doi.org/10.4103/ejs.ejs_150_22.
Luis SA, Sinak LJ, Michelena HI, Kane GC. American College of Cardiology website. ACC.org. Imaging-guided pericardiocentesis: a comparison of echocardiographic versus computed tomography guided approaches. https://www.acc.org/latest-in-cardiology/articles/2020/10/13/12/36/imaging-guided-pericardiocentesis. Published October 13, 2020. Accessed 3 Aug 2023.
Committee Opinion No. 723: guidelines for diagnostic imaging during pregnancy and lactation [erratum in Obstet Gynecol. 2018;132(3):786. https://doi.org/10.1097/AOG.0000000000002858]. Obstet Gynecol. 2017;130(4):e210–6. https://doi.org/10.1097/AOG.0000000000002355.
Cheon BK, Kim CL, Kim KR, Kang MH, Lim JA, Woo NS, et al. Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management. Korean J Pain. 2018;31(4):244–52. https://doi.org/10.3344/kjp.2018.31.4.244.
Acknowledgements
The authors thank Megan Griffiths for her assistance in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bafna, K.R., Kalra-Lall, A., Gurajala, R.K. et al. Computed Tomography–Guided Pericardiocentesis: A Practical Guide. Curr Cardiol Rep 25, 1433–1441 (2023). https://doi.org/10.1007/s11886-023-01965-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01965-9