Abstract
Purpose of Review
This review provides the summary of the appropriate use of these modalities when caring for patients with Kawasaki disease at diagnosis and for long-term management.
Recent Findings
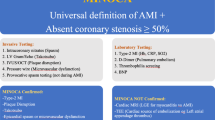
Kawasaki disease is an inflammatory syndrome of unknown etiology that can result in coronary artery dilations or aneurysms if left untreated in 25% of the patients and 3–5% in treated patients. In addition to coronary artery aneurysms, patients can have ventricular dysfunction, valvular regurgitation, aortic root dilation, and pericardial effusion due to inflammation of the myocardium. Noninvasive imaging modalities are important to these assessments.
Summary
Echocardiography is the first-line noninvasive evaluation of coronaries and function. Cardiac magnetic resonance imaging is useful for functional assessment in long-term follow-up. Distal coronaries, thromboses, and stenoses are best evaluated by cardiac computed tomography. Future research should demonstrate the effectiveness of advanced functional imaging in patients with Kawasaki disease and decreased radiation from cardiac computed tomography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease (KD) is an inflammatory syndrome of unknown etiology that can result in coronary artery dilations or aneurysms if left untreated in 25% of the patients [1•]. Even with appropriate treatment with intravenous immunoglobulin and other inflammatory modulatory agents, there remains 3–5% patients with coronary artery lesions (CAL) [1•]. In addition to CAL, patients can have ventricular dysfunction, atrioventricular valve regurgitation, and pericardial effusion. Thus, imaging evaluation in KD remains an important tool in the evaluation of these patients in the acute phase and long-term follow-up. The aim of this paper is to describe the noninvasive imaging evaluation of KD patients using echocardiography, computer tomography (CT), and cardiac magnetic resonance imaging (MRI) with the appropriate use of these modalities when accessing KD patients at diagnosis and long-term management.
Echocardiography
Echocardiography is an important noninvasive tool for the evaluation of the coronary arteries and ventricular function in KD patients at diagnosis and follow-up. Pericardial effusion (2%), valvular regurgitation (27%), and aortic root dilation (10%) have been seen in KD echocardiograms as a result of pancarditis during the acute phase in KD patients [2•]. Stress echocardiography has been used to induce ischemia in KD patients for long-term follow-up.
Coronary Arteries
Optimal coronary artery settings include lowering the gain and increasing the compression to achieve a more black and white image to help define the intima–lumen interface so that it is easier to measure the coronary arteries [3]. Color Doppler settings should start at Nyquist limit of 30 cm/s and gradually lowered until flow is detected in the coronary arteries [3]. High-frequency probes may not be sensitive to demonstrate color Doppler; thus, a lower frequency probe can be used. The most common sites of coronary artery aneurysms are proximal left anterior descending artery (LAD) and right coronary artery (RCA) and then left main coronary artery (LMCA) followed by the left circumflex artery [3]. The distal RCA, the junction between RCA and posterior descending arteries, and the junction of any marginal branches have been reported to have aneurysms [3]. Brown et al. used the corresponding CT images of the coronary arteries in the parasternal long and short-axis views and apical images to demonstrate the views that are seen in echocardiography [3]. Children less than 1 year of age and greater than 8 years of age are at highest risks of developing CAL. Patients with persistent fever after immunoglobulin (IVIG) therapy, male sex, and greater 10 days of fever are at the highest risk of developing aneurysms [3]. Thus, coronary imaging in KD patients at diagnosis and during hospitalization in addition to follow-up are critical in managing these patients.
Ventricular Function
Depressed ventricular function is present in 20% of the KD patients at diagnosis with associated CAL. Ventricular function evaluation includes systolic and diastolic evaluation such as left ventricular ejection fraction (LVEF), tissue Doppler imaging (TDI), strain imaging, and myocardial work (MW). Printz et al. evaluated 198 acute KD patients and found that ventricular dilation are present with higher Z-scores than normal and recovered at week 5 after acute diagnosis [2•]. They demonstrated that although left ventricular (LV) dysfunction occurred in 20% of the patients at baseline, the LV function improved rapidly over time [2•]. Patients with LV dysfunction at baseline were compared with those with normal LV function that had greater odds of having coronary artery dilation at baseline, 1 week, and at 5 weeks of follow-up [2•]. Tissue Doppler imaging allows for the assessment of systolic and diastolic dysfunction. Phadke et al. demonstrated that the tricuspid, septal, and mitral early diastolic velocities (E’) were predictive of IVIG resistance in KD patients indicating that this measure of diastolic measurement is a useful marker to differentiate KD patients at higher risk of IVIG resistance [4].
Strain imaging measures the percentage change in myocardial deformation, and strain rate defines the rate of deformation over time. Strain is a load-independent global measure of ventricular systolic function and closely related to myocardial contractility. Strain imaging can measure regional and global systolic function. McCandless et al. demonstrated that the longitudinal strain, longitudinal strain rate, and circumferential strain were decreased in 32 KD patients in the acute phase compared to controls [5]. Their subgroup analysis showed that the longitudinal and circumferential strain were decreased in KD patients with CAL and in KD patients with IVIG resistance compared to controls [5]. However, when they compared KD versus KD patients with CAL, there were no significant differences in the strain measurements [5]. They also did not find an significant difference in KD patients who were IVIG responders versus IVIG non-responders [5]. They concluded that the myocardial strain was more sensitive at detecting myocardial dysfunction than LVEF since the LVEF were all normal in their KD patients [5]. Frank et al. demonstrated that myocardial dysfunction in 41 KD patients is related to the initial inflammation from KD rather than as a result of coronary artery ischemia using LV strain analysis [6]. In this study, all patients’ LV strain was normal by 6 weeks of follow-up [6]. Sanchez et al. also demonstrated that the longitudinal and circumferential strain rate was all recovered by the convalescent phase in 103 KD patients [7].
Atrial strain imaging has been used to evaluate diastolic dysfunction in KD patients. Kang et al. evaluated the left atrial (LA) longitudinal strain in acute phase of 95 KD patients and found that LA reservoir function (filling of the LA) is depressed in KD patients compared to controls, but it has poor discriminating sensitivity of acute KD from controls [8]. They found that LA strain outperformed the traditional Doppler inflow velocities and TDI in differentiating KD patients from controls [8]. Their subsequent study demonstrated that LV reservoir function improved at long-term follow-up after 5 years [9].
The most recent advance in noninvasive evaluation of myocardial contractility and efficiency is myocardial work. Global myocardial work index (MWI) is calculated as the area of LV pressure–strain loops noninvasively [10]. Sabatino et al. demonstrated that KD patients with CAL have decreased MWI compared to controls despite normal LVEF and global longitudinal strain in KD patients indicating that MWI may a more sensitive marker of myocardial dysfunction [11]. They also demonstrated that the depressed MWI was independent of KD patients with CAL [11].
Stress Echocardiography
Stress echocardiography can be used in the long-term surveillance of KD patients. Exercise stress echocardiography is more physiologic, and dobutamine stress echocardiography has been used in KD patients with CAL. Pahl et al. demonstrated the feasibility of exercise stress echocardiography in 28 KD patient with CAL and found that 2 children had exercise-induced wall motion abnormalities [12]. These two patients underwent cardiac catheterization with angiography of the coronaries which demonstrated critical LAD stenosis [12]. Noto et al. used dobutamine stress echocardiography to evaluate 50 KD patients compared to angiography and demonstrated that in 19 out 21 patients, > 50% occlusion of coronaries had positive response to dobutamine stress echocardiography [13]. In their subsequent study, Noto et al. demonstrated that dobutamine stress echocardiography had prognostic value in predicting major adverse cardiac events in a 15-year follow-up of KD patients with CAL [14•]. The current recommendation from the American Heart Association statement is to perform stress testing for inducible ischemia in KD patients with coronary risk level of III, IV, and V [1•].
MRI
Coronary Artery Evaluation
Although coronary arteries can be well seen with MRI, CT has superior spatial resolution as well as improved visualization of calcifications and thrombus which often occur in these patients and has been shown to have higher accuracy in evaluating for coronary artery aneurysms than MRI [15]. If MRI is being used to evaluate for coronary artery involvement including aneurysms or stenosis, technique optimization must be performed including the use of intravenous contrast, usually gadolinium or a blood pool agent such as ferumoxytol, as well as ECG gating and respiratory navigation. Three-dimensional (3D) isotropic acquisition with voxel sizes 1 mm or smaller to allow for orthogonal and multiplanar reconstructions is recommended. Ferumoxytol-enhanced coronary MRA have been performed in adults demonstrating nice correlation with catheter angiogram data [16]. Some centers do vessel wall imaging of the coronary arteries including a recent study by Matsumoto et al. where they showed 3D turbo spin echo (TSE) equivalent to more standard vessel wall imaging with 2D dual inversion recovery (DIR) TSE in a small cohort of patients [17]. Other techniques which may show promise in KD include coronary vessel wall enhancement on 3D T1 gradient echo inversion recovery sequence performed 40 min after gadolinium administration with enhancement indicating active disease, demonstrated in adults with underlying atherosclerotic coronary artery disease and systemic lupus erythematosus [18].
Standard MRI
The traditional role of MRI is for the evaluation of ventricular function, wall motion abnormalities, and delayed myocardial enhancement, all of which can be affected with moderate to large coronary aneurysms and later with stenoses [19]. Studies have also shown areas of delayed enhancement in additional areas besides those supplied by affected coronary arteries with giant aneurysms suggesting additional microvascular component to abnormal myocardial perfusion [19, 20•]. Among patients with asymptomatic coronary artery occlusion and greater than 50% myocardial thickness delayed myocardial enhancement, decreases in systolic function were seen, while function was preserved in those without delayed enhancement or with less than 50% myocardial wall thickness delayed enhancement [21].
Stress Perfusion MRI
Stress perfusion MRI has been shown to be helpful in convalescent KD and demonstrates correlation of hypoperfusion and delayed myocardial enhancement in areas of moderate-to-severe stenosis resulting in areas of infarction [22]. Gadolinium dose is halved, with half given for rest the perfusion and the other half following administration of stress agent. Adenosine stress examinations are the most widely used with some groups using regadenoson in this setting with promising results [17, 22,23,24]. Perfusion has mostly been assessed visually for areas demonstrating hypoperfusion, but some groups have shown that more quantitative perfusion is feasible using myocardial perfusion reserve index and even automated quantitative myocardial perfusion [23, 24]. Friesen et al. also saw progression in decreased myocardial perfusion reserve index in those with coronary thrombus at onset [23]. Typically, perfusion scanning is performed on 2 or 3 slices, such as 2 short-axis slices and one slide in 4-chamber slice plane or one short-axis and one 4-chamber slice. Technical parameters must be optimized in order to get sufficient signal in this sequence optimized for temporal resolution and in pediatric patients with fast heart rates. Scan optimization techniques to improve stress perfusion imaging include 3D acquisition of the entire heart using parallel imaging technique of compressed sensing in healthy adults [25].
Other MRI Biomarkers
Other markers have been evaluated in KD patients and shown to be altered in including strain, particularly longitudinal strain, while other studies have not found significant difference in strain [20•, 23, 26, 27]. A subsequent study by Yao et al. found lower global strain rates and longitudinal strain in patients with KD with late gadolinium enhancement but not in those with KD without delayed enhancement [20•]. Increased stiffness of the aorta and main pulmonary artery by evaluating pulse wave velocity has also been seen in patients with KD compared to controls [28].
Computed Tomography
Coronary CT angiography (CTA) allows for the visualization of the entire coronary arterial system, much like cardiac catheterization angiography, but in a noninvasive manner. On modern second- and third-generation dual-source CT scanners, the spatial resolution is excellent at 0.24–0.3 mm, and the temporal resolution is remarkably fast at 66–75 ms [29•]. Technologic advances have reduced the radiation dose significantly compared to the previous era, making cardiac CT an outstanding choice for detailed coronary artery assessment in KD.
The main weakness of coronary CTA for KD is that the young patient population affected by KD may require sedation for optimized acquisition, as discussed below. This could mean that CTA is most useful in the longitudinal monitoring of patients with persistent coronary abnormalities once they are able to reliably cooperate with breath-holding instructions. Another weakness of CTA is the radiation exposure, despite recent advances, especially with serial examinations.
Protocol Selection for CTA
The determination of CTA protocol for coronary assessment is driven by the patient’s heart rate and scanner. Given the typical age range of 6 months to 5 years for those affected by acute KD, heart rates will typically fall in the range of 80–140 beats per minute (bpm). At the upper end of this range (> 120 bpm), scans will typically need to follow a retrospective ECG-gated spiral acquisition protocol, which requires the patient to be completely still and hold their breath. For children younger than 5–6 years old, these requirements nearly always prompt a need for anesthesia. The retrospective scan requires the greatest amount of radiation exposure of all the protocol types due to oversampling and acquisition throughout the cardiac cycle over multiple heart beats. Notably, it is possible to reduce the radiation dose at a prescribed portion of the cardiac cycle while maintaining full dose at the portion of the cardiac cycle of greatest interest. In patients with heart rates high enough (often infants and young children) that require a retrospective acquisition for optimal evaluation of subtle coronary stenoses, the high heart rate makes timing of the cardiac rest period unpredictable and dose modulation difficult to prescribe without potentially reducing the diagnostic quality of the scan. For this reason, we recommend using a conservative z-axis coverage confined to the potential locations of the coronary arteries when using a retrospective technique which limits radiation dose without risking scan quality.
. Some centers use a beta blocker for exceptionally high or widely variable heart rates to ensure a diagnostic scan. Some have suggested an oral beta blocker 30 min before scan time, while others favor an esmolol infusion during the scan due to its short half-life [30]. If using beta blockade, it would be prudent to ensure normal ventricular systolic function prior to initiation so as not to inadvertently lower the cardiac output, especially in heart rate–dependent infants.
For heart rates below 120 bpm, it is reasonable to attempt a prospective ECG-gated sequential protocol (i.e., “step-and-shoot”) which lowers the radiation dose somewhat to an average of 0.3–1 mSv but still requires an immobile patient and reliable breath-holding and therefore sedation in young children [29•]. This technique does not utilize oversampling/interpolation of data because it is usually an axial acquisition.
An ECG-triggered prospective high-pitch spiral scan (e.g., Flash/TurboFlash on Siemens second-/third-generation scanners) generally does not require complete immobility, breath-holding, or anesthesia and has the lowest radiation dose of the three protocols discussed (usually < 0.2–0.5 mSv) [29•]. As such, this scan is the typical “bread and butter” protocol in pediatric cardiac CTA for assessment of vascular anatomy. However, this type of scan is the most sensitive to motion in the small coronary arterial vessels. At heart rates greater than 80 bpm, this scan is not expected to achieve the resolution required for reliable measurements or assessment for distal aneurysms. Given the clear benefits of eliminating sedation and significantly reducing the radiation dose, some centers rely heavily on beta blockade to allow for utilization of this technique. For instance, Gellis et al. documented a clinical protocol at Boston Children’s Hospital with a third-generation dual-source scanner where all children with a resting heart rate over 70 bpm underwent beta blockade for coronary CTA [31]. In their study of 18 KD patients (aged 2–6 years) with known coronary aneurysms, a high-pitch spiral scan was performed on all patients with heart rate < 80 bpm. In total, 33% underwent a high-pitch spiral scan, 52% prospective step-and-shoot, and only 14% retrospective gated.
Coronary Arterial Aneurysms
Visualization of coronary arterial aneurysms by CTA is technically straightforward and provides excellent resolution to perform measurements throughout the coronary arterial system. To ensure inclusion of the distal coronary vasculature, the field of view should cover the entire heart, including the diaphragmatic surface. Although traditional invasive angiography is considered the “gold standard” for imaging of coronary arterial vessels in KD, multiple reports demonstrate that coronary CTA is equivalent at detecting and measuring aneurysms [32, 33]. Traditional angiography has an average radiation dose of 5–7 mSv [34], greatly exceeding that of modern coronary CTA. Additionally, cardiac catheterization carries an increased risk of pseudoaneurysm development at the femoral access site during the acute phase of KD [1•, 35]. Assessment by CTA during this timepoint allows for avoidance of that risk without a decrease in imaging quality. One benefit that cardiac catheterization holds over CTA is the ability to observe dynamic flow of contrast within the coronary vessels. In an attempt to overcome this, one study evaluated the performance of dynamic flow CTA in KD patients [36], a technique initially developed for the functional evaluation of stenoses in atherosclerotic coronary artery disease [37]. Utilizing this novel technique, Shimomiya et al. was able to quantify relative flow within the proximal and distal coronary arteries by observing upstrokes in contrast density in a pilot population of 6 adult patients with persistent coronary aneurysms. Although this technique exists purely in the research sphere currently, it has the potential to push the CTA evaluation of coronary aneurysms to a new functional level, although likely at the expense of increased radiation exposure.
Transthoracic echocardiography and coronary CTA demonstrate excellent agreement in coronary vessel and aneurysm measurements when assessing the proximal coronary arteries [31, 38]. Measurement discrepancies increase distally in the coronary vasculature, especially for the left coronary arterial system, with a bias toward measurements of distal aneurysms being smaller by CTA than echo [31]. Reliance on echocardiography for grading of distal aneurysms may result in following a more aggressive treatment plan than is warranted in up to 28% of cases. Further, echo may miss aneurysms altogether, with multiple reports demonstrating 33–55% of aneurysms detected by CTA missed by transthoracic echocardiography, with the majority of missed aneurysms being located in the distal coronary artery segments or left circumflex coronary artery [39,40,41,42].
Z-score regression equations in the literature are derived from echocardiographic measurements of proximal coronary arteries [43,44,45,46,47]. To date, there is no normative data for coronary diameters derived from CTA data for a pediatric population. Thus, the typical practice is application of echo Z-scores to CTA measurements. Although this practice is not ideal given possible differences in standard deviations between the methods, it is reassuring that there is excellent agreement in the measurements of proximal coronary vessels in small cohorts and that both inter- and intraobserver reliability is high for CTA measurements of coronary aneurysms in KD [31, 33, 48].
Although cardiac MR angiography is capable of demonstrating the entire coronary arterial system, the technique is much more laborious, and the resolution (both spatial and temporal) is less than with CTA [49]. In a single-center study evaluating 54 patients with KD who had undergone both CTA and CMR, half of the aneurysms detected by CTA were missed by CMR, including both proximal and distal aneurysms [15].
Coronary Aneurysm Complications (Thrombi, Calcification, Stenoses)
Coronary CTA is especially well-suited to evaluate for coronary arterial aneurysm complications including thrombus, calcification, and stenosis. The CTA evaluation for thrombi and calcification exceeds the capabilities of catheter-based angiography 6, cardiac MR angiography [15], and echocardiography [39]. One study describes a complementary role of echo and coronary CTA in identifying coronary aneurysm thrombi as each technique has different strengths, and the combined use of both modalities allows for more reliable thrombus detection: echo is better able to identify low-density thrombi, and CTA is better suited to detect distal thrombi [50]. In this study, of the 4 coronary thrombi missed by CTA, 3 were mural (LAD × 1, RCA × 2), and one was low-density (LMCA). All 6 of the thrombi missed by echo were in the distal RCA, 1 of which was completely occlusive.
Assessment of aneurysm calcification can have implications for prognostication as one study by Chen et al. demonstrated that calcified aneurysms were unlikely to regress. In their analysis of 37 coronary artery aneurysms in 18 patients, there were 14 that were calcified, and only one of these regressed during the study’s follow-up period of several years [48]. Typically, coronary aneurysm calcification is thought of as a late phenomenon and may be more relevant to the long-term follow-up of aneurysms. Kahn et al. [51] imaged KD patients an average of 2 decades after their initial KD course using a low radiation and non-contrast scan to quantify a coronary arterial calcification score, demonstrating that only those patients with persistent coronary abnormalities had calcified segments. Further, of the 24 patients in their cohort with persistent coronary aneurysms, only 5 did not have calcification, and 4 of these were imaged within 6 years of their initial KD course. This study raises the possibility that low radiation, non-contrast CT could be utilized to screen for persistent coronary aneurysms in patients with a remote childhood history of a possible KD illness. The sensitivity of such a screening technique would increase with time from initial KD illness. Tsuji et al. [52] demonstrated 10% incidence of aneurysm calcification at 10 years, 38% calcification at 20 years, and 72% calcification at 30 years post-initial KD illness in patients with persistent aneurysms.
Late stenoses occur in up to 15% of patients with coronary artery aneurysms [34], thus making reliable long-term imaging an important priority in the lifelong management of KD. Coronary CTA has equivalent capabilities to diagnose coronary artery stenoses compared to cardiac catheterization angiography [32] and can detect distal stenoses not seen by echocardiography [31, 39, 41] or MRI [15, 32]. Further, echo imaging windows become more difficult with age. Given the important implications of a new coronary stenosis for patient care, routine monitoring driven by patient symptoms with serial CTA is reasonable. This is especially true given adolescent and adult patients are most often able to cooperate with breath-holding, allowing for avoidance of anesthesia and minimization of radiation dose with a prospective step-and-shoot or, ideally, a high-pitch spiral scan.
Functional Assessment
Cardiac CT is capable of ventricular systolic function assessment using a retrospective ECG-gated technique and volumetric analysis. When utilizing modern CT scanners, there is excellent agreement between CT and MRI measurements of left and right ventricular volumes and ejection fraction in adult cohorts [53]. The main downside for using CT for functional analysis is the radiation exposure and contrast load. In patients with KD who already require a retrospective gated scan for assessment of the coronary arteries, adding a function analysis would simply require additional post-processing. To ensure accurate end-systolic and end-diastolic phase selection, it is recommended to reconstruct the CT data at 5% intervals into 20 phases of the entire cardiac cycle, although the ultimate accuracy of these phases will be dependent on both the temporal resolution of the CT scanner used and the patient’s heart rate.
Conclusions
In conclusion, echocardiography is the first line of noninvasive evaluation in KD patients during the acute presentation and is also important in long-term follow-up. Inducible ischemia can be performed using stress echocardiography. Cardiac MRI is useful in evaluating patients at the long-term follow-up for inducible ischemia and ventricular function when the acoustic window is poor for echocardiography. Coronary imaging from CT allows for the evaluation of the degree of stenosis in long-term follow-up to determine if the patient will require invasive coronary angiography and intervention. In instances where aneurysms are in the distal coronary vasculature or there is suspicion for stenosis or thrombus, coronary CTA can provide superior visualization of the entire coronary arterial tree. These noninvasive imaging modalities are crucial at diagnosis and long-term management of KD patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–99. https://doi.org/10.1161/CIR.0000000000000484. Important review article in Kawasaki disease.
• Printz BF, Sleeper LA, Newburger JW, Minich LL, Bradley T, Cohen MS, et al. Noncoronary cardiac abnormalities are associated with coronary artery dilation and with laboratory inflammatory markers in acute Kawasaki disease. J Am Coll Cardiol. 2011;57(1):86–92. https://doi.org/10.1016/j.jacc.2010.08.619. Echocardiographic parameters to read in Kawasaki disease.
Brown LM, Duffy CE, Mitchell C, Young L. A practical guide to pediatric coronary artery imaging with echocardiography. J Am Soc Echocardiogr. 2015;28(4):379–91. https://doi.org/10.1016/j.echo.2015.01.008.
Phadke D, Patel SS, Dominguez SR, Heizer H, Anderson MS, Glode MP, et al. Tissue Doppler imaging as a predictor of immunoglobulin resistance in Kawasaki disease. Pediatr Cardiol. 2015;36(8):1618–23. https://doi.org/10.1007/s00246-015-1206-5.
McCandless RT, Minich LL, Wilkinson SE, McFadden ML, Tani LY, Menon SC. Myocardial strain and strain rate in Kawasaki disease. Eur Heart J Cardiovasc Imaging. 2013;14(11):1061–8. https://doi.org/10.1093/ehjci/jet041.
Frank B, Davidson J, Tong S, Martin B, Heizer H, Anderson MS, et al. Myocardial strain and strain rate in Kawasaki disease: range, recovery, and relationship to systemic inflammation/coronary artery dilation. J Clin Exp Cardiolog. 2016;7(4). https://doi.org/10.4172/2155-9880.1000432.
Sanchez AA, Sexson Tejtel SK, Almeida-Jones ME, Feagin DK Jr, Altman CA, Pignatelli RH. Comprehensive left ventricular myocardial deformation assessment in children with Kawasaki disease. Congenit Heart Dis. 2019;14(6):1024–31. https://doi.org/10.1111/chd.12787.
Kang SJ, Kwon YW, Hwang SJ, Kim HJ, Jin BK, Yon DK. Clinical utility of left atrial strain in children in the acute phase of Kawasaki disease. J Am Soc Echocardiogr. 2018;31(3):323–32. https://doi.org/10.1016/j.echo.2017.11.012.
Kang SJ, Ha J, Hwang SJ, Kim HJ. Long term outcomes of left atrial reservoir function in children with a history of Kawasaki disease. J Cardiovasc Ultrasound. 2018;26(1):26–32. https://doi.org/10.4250/jcu.2018.26.1.26.
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J. 2012;33(6):724–33. https://doi.org/10.1093/eurheartj/ehs016.
Sabatino J, Borrelli N, Fraisse A, Herberg J, Karagadova E, Avesani M, et al. Abnormal myocardial work in children with Kawasaki disease. Sci Rep. 2021;11(1):7974. https://doi.org/10.1038/s41598-021-86933-5.
Pahl E, Sehgal R, Chrystof D, Neches WH, Webb CL, Duffy CE, et al. Feasibility of exercise stress echocardiography for the follow-up of children with coronary involvement secondary to Kawasaki disease. Circulation. 1995;91(1):122–8. https://doi.org/10.1161/01.cir.91.1.122.
Noto N, Ayusawa M, Karasawa K, Yamaguchi H, Sumitomo N, Okada T, et al. Dobutamine stress echocardiography for detection of coronary artery stenosis in children with Kawasaki disease. J Am Coll Cardiol. 1996;27(5):1251–6. https://doi.org/10.1016/0735-1097(95)00570-6.
• Noto N, Kamiyama H, Karasawa K, Ayusawa M, Sumitomo N, Okada T, et al. Long-term prognostic impact of dobutamine stress echocardiography in patients with Kawasaki disease and coronary artery lesions: a 15-year follow-up study. J Am Coll Cardiol. 2014;63(4):337–44. https://doi.org/10.1016/j.jacc.2013.09.021. Important study to read on dobutamine stress test.
van Stijn D, Planken N, Kuipers I, Kuijpers T. CT Angiography or cardiac MRI for detection of coronary artery aneurysms in Kawasaki disease. Front Pediatr. 2021;9: 630462. https://doi.org/10.3389/fped.2021.630462.
Chin MS, Steigner M, Yin W, Kwong RY, Siedlecki AM. Intraluminal assessment of coronary arteries with ferumoxytol-enhanced magnetic resonance angiography. JACC Cardiovasc Imaging. 2018;11(3):505–8. https://doi.org/10.1016/j.jcmg.2017.10.017.
Matsumoto K, Yokota H, Yoda T, Ebata R, Mukai H, Masuda Y, et al. Reproducibility between three-dimensional turbo spin-echo and two-dimensional dual inversion recovery turbo spin-echo for coronary vessel wall imaging in Kawasaki disease. Sci Rep. 2022;12(1):6835. https://doi.org/10.1038/s41598-022-10951-0.
Varma N, Hinojar R, D’Cruz D, Arroyo Ucar E, Indermuehle A, Peel S, et al. Coronary vessel wall contrast enhancement imaging as a potential direct marker of coronary involvement: integration of findings from CAD and SLE patients. JACC Cardiovasc Imaging. 2014;7(8):762–70. https://doi.org/10.1016/j.jcmg.2014.03.012.
Muthusami P, Luining W, McCrindle B, van der Geest R, Riesenkampff E, Yoo SJ, et al. Myocardial perfusion, fibrosis, and contractility in children with Kawasaki disease. JACC Cardiovasc Imaging. 2018;11(12):1922–4. https://doi.org/10.1016/j.jcmg.2018.06.009.
• Yao Q, Hu XH, He LL. Evaluation of comprehensive myocardial contractility in children with Kawasaki disease by cardiac magnetic resonance in a large single center. Quant Imaging Med Surg. 2022;12(1):481–92. https://doi.org/10.21037/qims-20-1402. Important cardiac magnetic resonance study in patients with Kawasaki disease.
Nakaoka H, Tsuda E, Morita Y, Kurosaki K. Cardiac function by magnetic resonance imaging in coronary artery occlusions after Kawasaki disease. Circ J. 2020;84(5):792–8. https://doi.org/10.1253/circj.CJ-19-0511.
Doan TT, Wilkinson JC, Loar RW, Pednekar AS, Masand PM, Noel CV. Regadenoson stress perfusion cardiac magnetic resonance imaging in children with Kawasaki disease and coronary artery disease. Am J Cardiol. 2019;124(7):1125–32. https://doi.org/10.1016/j.amjcard.2019.06.033.
Friesen RM, Schafer M, Jone PN, Appiawiah N, Vargas D, Fonseca B, et al. Myocardial perfusion reserve index in children with Kawasaki disease. J Magn Reson Imaging. 2018;48(1):132–9. https://doi.org/10.1002/jmri.25922.
Scannell CM, Hasaneen H, Greil G, Hussain T, Razavi R, Lee J, et al. Automated quantitative stress perfusion cardiac magnetic resonance in pediatric patients. Front Pediatr. 2021;9: 699497. https://doi.org/10.3389/fped.2021.699497.
Fair MJ, Gatehouse PD, Reyes E, Adluru G, Mendes J, Khan T, et al. Initial investigation of free-breathing 3D whole-heart stress myocardial perfusion MRI. Glob Cardiol Sci Pract. 2020;2020(3):e202038. https://doi.org/10.21542/gcsp.2020.38.
Zhou ZQ, Wen LY, Fu C, Yang Z, Fu H, Xu R, et al. Association of left ventricular systolic dysfunction with coronary artery dilation in Kawasaki disease patients: assessment with cardiovascular magnetic resonance. Eur J Radiol. 2021;145: 110039. https://doi.org/10.1016/j.ejrad.2021.110039.
Bratis K, Hachmann P, Child N, Krasemann T, Hussain T, Mavrogeni S, et al. Cardiac magnetic resonance feature tracking in Kawasaki disease convalescence. Ann Pediatr Cardiol. 2017;10(1):18–25. https://doi.org/10.4103/0974-2069.197046.
Schafer M, Truong U, Ivy DD, Fonseca B, Malone L, DiMaria M, et al. Children with Kawasaki disease present elevated stiffness of great arteries: phase-contrast MRI study. J Magn Reson Imaging. 2018;48(5):1228–36. https://doi.org/10.1002/jmri.26167.
• Secinaro A, Curione D, Mortensen KH, Santangelo TP, Ciancarella P, Napolitano C, et al. Dual-source computed tomography coronary artery imaging in children. Pediatr Radiol. 2019;49(13):1823–39. https://doi.org/10.1007/s00247-019-04494-2. Coronary artery imaging in Kawasaki disease.
Watanabe H, Kamiyama H, Kato M, Komori A, Abe Y, Ayusawa M. Appropriate use of a beta-blocker in paediatric coronary CT angiography. Cardiol Young. 2018;28(10):1148–53. https://doi.org/10.1017/S104795111800118X.
Gellis L, Castellanos DA, Oduor R, Gauvreau K, Dionne A, Newburger J, et al. Comparison of coronary artery measurements between echocardiograms and cardiac CT in Kawasaki disease patients with aneurysms. J Cardiovasc Comput Tomogr. 2022;16(1):43–50. https://doi.org/10.1016/j.jcct.2021.09.002.
Arnold R, Ley S, Ley-Zaporozhan J, Eichhorn J, Schenk JP, Ulmer H, et al. Visualization of coronary arteries in patients after childhood Kawasaki syndrome: value of multidetector CT and MR imaging in comparison to conventional coronary catheterization. Pediatr Radiol. 2007;37(10):998–1006. https://doi.org/10.1007/s00247-007-0566-2.
Tsujii N, Tsuda E, Kanzaki S, Kurosaki K. Measurements of coronary artery aneurysms due to Kawasaki disease by dual-source computed tomography (DSCT). Pediatr Cardiol. 2016;37(3):442–7. https://doi.org/10.1007/s00246-015-1297-z.
Singhal M, Gupta P, Singh S, Khandelwal N. Computed tomography coronary angiography is the way forward for evaluation of children with Kawasaki disease. Glob Cardiol Sci Pract. 2017;2017(3):e201728. https://doi.org/10.21542/gcsp.2017.28.
Gurofsky RC, Sabharwal T, Manlhiot C, Redington AN, Benson LN, Chahal N, et al. Arterial complications associated with cardiac catheterization in pediatric patients with a previous history of Kawasaki disease. Catheter Cardiovasc Interv. 2009;73(6):809–13. https://doi.org/10.1002/ccd.21892.
Shimomiya Y, Nagao M, Yamasaki Y, Shirasaka T, Kondo M, Kojima T, et al. Dynamic flow imaging using 320-detector row CT and motion coherence analysis in coronary aneurysms associated with Kawasaki disease. Cardiol Young. 2018;28(3):416–20. https://doi.org/10.1017/S1047951117002293.
Nagao M, Yamasaki Y, Kamitani T, Kawanami S, Sagiyama K, Yamanouchi T, et al. Quantification of coronary flow using dynamic angiography with 320-detector row CT and motion coherence image processing: detection of ischemia for intermediate coronary stenosis. Eur J Radiol. 2016;85(5):996–1003. https://doi.org/10.1016/j.ejrad.2016.02.027.
Dusad S, Singhal M, Pilania RK, Suri D, Singh S. CT coronary angiography studies after a mean follow-up of 3.8 years in children with Kawasaki disease and spontaneous defervescence. Front Pediatr. 2020;8:274. https://doi.org/10.3389/fped.2020.00274.
Singhal M, Pilania RK, Jindal AK, Gupta A, Sharma A, Guleria S, et al. Distal coronary artery abnormalities in Kawasaki disease: experience on CT coronary angiography in 176 children. Rheumatology (Oxford). 2022. https://doi.org/10.1093/rheumatology/keac217.
van Stijn D, Planken RN, Groenink M, Streekstra GJ, Kuijpers TW, Kuipers IM. Coronary artery assessment in Kawasaki disease with dual-source CT angiography to uncover vascular pathology. Eur Radiol. 2020;30(1):432–41. https://doi.org/10.1007/s00330-019-06367-6.
Jrad M, Ben Salem F, Barhoumi C, Lassoued F, Frikha W, Boukriba S, et al. The role of computed tomography coronary angiography in Kawasaki disease: comparison with transthoracic echocardiography in a 25-case retrospective study. Pediatr Cardiol. 2019;40(2):265–75. https://doi.org/10.1007/s00246-018-2044-z.
Singhal M, Singh S, Gupta P, Sharma A, Khandelwal N, Burns JC. Computed tomography coronary angiography for evaluation of children with Kawasaki disease. Curr Probl Diagn Radiol. 2018;47(4):238–44. https://doi.org/10.1067/j.cpradiol.2017.09.013.
McCrindle BW, Li JS, Minich LL, Colan SD, Atz AM, Takahashi M, et al. Coronary artery involvement in children with Kawasaki disease: risk factors from analysis of serial normalized measurements. Circulation. 2007;116(2):174–9. https://doi.org/10.1161/CIRCULATIONAHA.107.690875.
Olivieri L, Arling B, Friberg M, Sable C. Coronary artery Z score regression equations and calculators derived from a large heterogeneous population of children undergoing echocardiography. J Am Soc Echocardiogr. 2009;22(2):159–64. https://doi.org/10.1016/j.echo.2008.11.003.
Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr. 2011;24(1):60–74. https://doi.org/10.1016/j.echo.2010.10.004.
Kobayashi T, Fuse S, Sakamoto N, Mikami M, Ogawa S, Hamaoka K, et al. A new Z score curve of the coronary arterial internal diameter using the lambda-mu-sigma method in a pediatric population. J Am Soc Echocardiogr. 2016;29(8):794–801 e29. https://doi.org/10.1016/j.echo.2016.03.017.
Lopez L, Colan S, Stylianou M, Granger S, Trachtenberg F, Frommelt P, et al. Relationship of echocardiographic Z scores adjusted for body surface area to age, sex, race, and ethnicity: the Pediatric Heart Network Normal Echocardiogram Database. Circ Cardiovasc Imaging. 2017;10(11). https://doi.org/10.1161/CIRCIMAGING.117.006979.
Chen PT, Lin MT, Chen YS, Chen SJ, Wu MH. Computed tomography predict regression of coronary artery aneurysm in patients with Kawasaki disease. J Formos Med Assoc. 2017;116(10):806–14. https://doi.org/10.1016/j.jfma.2017.07.001.
Kim JW, Goo HW. Coronary artery abnormalities in Kawasaki disease: comparison between CT and MR coronary angiography. Acta Radiol. 2013;54(2):156–63. https://doi.org/10.1258/ar.2012.120484.
Xu YM, Chu YQ, Li XM, Wang C, Ma QM, Yu XN, et al. The complementary relationship between echocardiography and multi-slice spiral CT coronary angiography in the diagnosis of coronary artery thrombosis in children with Kawasaki disease. Front Pediatr. 2021;9:670887. https://doi.org/10.3389/fped.2021.670887.
Kahn AM, Budoff MJ, Daniels LB, Oyamada J, Gordon JB, Burns JC. Usefulness of calcium scoring as a screening examination in patients with a history of Kawasaki disease. Am J Cardiol. 2017;119(7):967–71. https://doi.org/10.1016/j.amjcard.2016.11.055.
Tsujii N, Tsuda E, Kanzaki S, Ishizuka J, Nakashima K, Kurosaki K. Late wall thickening and calcification in patients after Kawasaki disease. J Pediatr. 2017;181(167–71): e2. https://doi.org/10.1016/j.jpeds.2016.10.026.
Maffei E, Messalli G, Martini C, Nieman K, Catalano O, Rossi A, et al. Left and right ventricle assessment with Cardiac CT: validation study vs. Cardiac MR Eur Radiol. 2012;22(5):1041–9. https://doi.org/10.1007/s00330-011-2345-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
Jone, PN., Romanowicz, J., Browne, L. et al. Imaging Evaluation of Kawasaki Disease. Curr Cardiol Rep 24, 1487–1494 (2022). https://doi.org/10.1007/s11886-022-01768-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01768-4