Abstract
Purpose of Review
Heart failure has substantial effects on health-related quality of life. Maintaining or improving quality of life is an important goal of heart failure therapy, and many patients value better quality of life over greater longevity.
Recent Findings
The symptoms and functional severity of heart failure, medical comorbidities, and depression are the strongest predictors of poor quality of life. Guideline-recommended medical and behavioral interventions for HF, including exercise training and cardiac rehabilitation, self-care interventions, and treatment of depression, can help to improve quality of life.
Summary
Heart failure is, in most cases, a progressive condition with a poor prognosis. However, poor quality of life is not inevitable, and a variety of medical, surgical, and nonpharmacological interventions can help to maintain or improve quality of life in patients with heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improved quality of life (QoL) is one of the most important treatment outcomes for patients with heart failure (HF). Time trade-off utility studies suggest that many patients with HF would be willing to trade between 3 and 12 months of longevity for better QoL [1, 2]. Patients with relatively severe symptoms tend to be more willing than patients with milder symptoms to trade longevity for a better quality of life [2].
Assessment of Quality of Life
A variety of instruments have been used to assess HF-specific QoL in the context of research, but a recent systematic review [3] found only two that met stringent criteria for reliability, validity, sensitivity to change, and other clinically relevant characteristics. The 21-item Minnesota Living with Heart Failure Questionnaire (MLHFQ) [4] assesses the impact of typical signs and symptoms of HF on functioning and QoL, including dyspnea, fatigue, and peripheral edema, as well as physical and social limitations such as difficulty with walking, climbing stairs, performing work-related tasks, or engaging in recreational activities. Each item is rated on a six-point scale ranging from 0 (none or not applicable) to 5 (very much), and the total score ranges from 0 to 105 with higher scores indicating worse QoL. The 23-item Kansas City Cardiomyopathy Questionnaire (KCCQ) [5] assesses physical and social limitations, symptoms, self-efficacy (i.e., confidence in HF self-care abilities), and the impact of HF on lifestyle and enjoyment of life. A 12-item short form of the KCCQ is also available [6]. On both the full and the short form KCCQ, the item ratings are summed and transformed onto a 0–100 scale on which higher scores reflect better health status. Thus, higher scores have opposite meanings on the MLHFQ and the KCCQ.
Although both instruments have excellent psychometric properties and are widely used in HF research, they also have relative strengths and weaknesses. Both instruments were recently evaluated for inclusion in the International Consortium for Health Outcomes Measurement (ICHOM) standardized patient-centered outcomes measurement set for patients with HF. The ICHOM working group chose the short form KCCQ-12, primarily because of its superior sensitivity to change and relative ease of use [7].
Correlates of QoL in Patients with Heart Failure
Severity of illness is a complex construct in HF. Biomarkers such as NT-proBNP and physiological indexes such as the left ventricular ejection fraction (LVEF) are used to measure certain aspects of the severity of HF. Severity can also be assessed in terms of observable signs, self-reported symptoms, and functional impairment. The New York Heart Association (NYHA) class is a widely reported index of the symptomatic or functional severity of HF. Patients in NYHA class I have no HF-related limitations of physical activity. In contrast, patients in class IV are unable to engage in any physical activity without discomfort, and they experience HF symptoms such as shortness of breath even at rest. The physiological and functional dimensions of HF severity are intercorrelated but only moderately, and QoL correlates more strongly with the symptoms and functional severity of HF than it does with biomarkers and physiological measures. In a recent study, mean KCCQ scores were 85, 70, 55, and 45 in patients with NYHA class I, II, III, and IV heart failure, respectively (p < 0.001) [8••]. A difference of five points or more on the KCCQ is clinically meaningful [9], so the QoL differences between NYHA classes are substantial. In short, patients who are severely impaired by HF report much worse QoL than patients who are less impaired.
Most patients with HF have multiple medical comorbidities, and many have depression, anxiety, or other psychiatric comorbidities. Medical comorbidities that degrade QoL in HF include diabetes, anemia, and chronic obstructive pulmonary disease (COPD) [10]. Depression is more strongly (negatively) associated with poor QoL in HF than any other comorbidity, and in some studies, it has been even more strongly associated than NYHA class with QoL [11].
Depression is also associated with poor QoL after implantation of a left ventricular assist device (LVAD). In a recent Registry Evaluation of Vital Information for Ventricular Assist Devices in Ambulatory Life (REVIVAL) report, depression accounted for most of the effect of comorbidities on QoL, and depressed patients scored an average of 25 points lower on the KCCQ than their nondepressed counterparts [12].
Changes in QoL over Time
Heart failure is a chronic, progressive disorder that reduces life expectancy by an average of 1 month per year after the initial diagnosis [13]. Medical treatments and implanted devices can help to maintain or improve QoL, but QoL may decline nevertheless as HF progresses. A recent Change the Management of Patients with Heart Failure (CHAMP-HF) registry study of outpatients with HF with reduced left ventricular ejection fraction (HFrEF) analyzed changes over 12 months in NYHA class and KCCQ scores. Approximately 21% of the patients were in a better (lower) NYHA class at 12 months than at baseline and 14% were in a worse (higher) NYHA class; 48% had better (higher) KCCQ score at 12 months, and 27% had a worse (lower) KCCQ score. An improvement of at least 5 points on the KCCQ was an independently predictor of fewer HF hospitalizations and lower mortality [8••].
A recent study of the Alberta, Canada Heart Failure Aetiology and Analysis Team (HEART) cohort compared 169 patients with HFrEF and 191 patients with HF and preserved ejection fraction (HFpEF) to healthy controls and to patients who were at risk for developing HF. Median KCCQ scores at baseline were 73 in the HFpEF and 82 in the HFrEF groups, compared to 95 in the at-risk patients and 100 in the healthy control group (p < 0.0001). Twelve months later, 28% of the patients with HFpEF showed a ≥ 5-point improvement on the KCCQ and 37% showed a ≥ 5-point worsening; in contrast, 34% of the patients with HFrEF showed a ≥ 5-point improvement on the KCCQ and 27% showed a ≥ 5-point worsening (p < 0.0001). This suggests that QoL is more likely to improve and less likely to deteriorate over 12 months in patients with HFrEF than in those with HFpEF. In the cohort as a whole, deterioration in QoL was associated with higher age, medical comorbidities (atrial fibrillation, coronary artery disease, COPD, anemia), higher body mass index, higher biomarkers of HF severity (BNP, NT-proBNP), HF signs and symptoms (peripheral edema, shortness of breath, fatigue, jugular venous distension), echocardiographic markers of diastolic dysfunction, and higher LVEF (consistent with worse QoL in patients with HFpEF than in those with HFrEF). Decreasing KCCQ scores predicted shorter time to rehospitalization or death in patients with HFpEF. There was a similar but statistically nonsignificant pattern in patients with HFrEF [14•].
The Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training (HF-ACTION) trial provided an opportunity to study the clinical impact of changes in QoL in a substantially larger group of patients. The KCCQ was repeatedly administered to participants in HF-ACTION to assess HF-specific QoL. After combining the exercise training and usual care arms, complete baseline and 3-month KCCQ data were obtained on 2,038 patients. KCCQ scores worsened by ≥ 5 points over 3 months in 23% and improved by ≥ 5 points in 45% of these patients. Changes in KCCQ scores predicted all-cause mortality, the combined end point of all-cause mortality or all-cause hospitalization, and the combined end point of cardiovascular mortality or HF hospitalization [15].
Although worsening QoL is associated with an increased risk of hospital readmissions, hospitalization seems to have relatively little impact on QoL for most patients with HF. Data from the Trans-European Network-Home-Care Management System (TEN-HMS) trial were recently used to examine pre- to post-hospitalization changes in general health-related QoL. Hospitalization had little effect on QoL even when length of stay and time spent in intensive care were included in multivariable models [16].
Effects of Medications and Surgical Interventions on QoL
The goals of medical care for heart failure include slowing the progression of the disease, prolonging survival, reducing symptoms, increasing functional capacity, and improving quality of life. Advances in medical therapeutics, including beta blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and aldosterone antagonists, have made these goals achievable for many patients with HFrEF [17]. Unfortunately, the same cannot be said for patients with HFpEF. Clinical practice guidelines recommend many of the same treatments for HFpEF as for HFrEF, but highly effective treatments for HFpEF are not yet available [18].
Despite acknowledging that QoL is an important goal of treatment, the current guidelines of the American College of Cardiology (ACC) and the American Heart Association (AHA) for the management of heart failure [19, 20] have relatively little to say about QoL outcomes. Like the ACC/AHA guidelines, the European Society of Cardiology (ESC) guidelines [21] emphasize the effects of various treatments on mortality and hospital readmissions, but they also address QoL and other outcomes of at least some of the most widely used treatments. For example, the ESC guidelines indicate that cardiac resynchronization therapy (CRT) yields significant improvements in quality-adjusted life years (QALYs) in patients with moderate to severe HF, with one-third of the change in QALYs attributable to increased longevity and two-thirds attributable to improved QoL.
Iron deficiency is a common problem in patients with HF, and it can cause both anemia and skeletal muscle weakness. Citing two major trials (FAIR-HF and CONFIRM-HF) and a meta-analysis of randomized controlled trials (RCTs) for patients with HFrEF [22], the ESC guidelines recommend intravenous iron therapy to improve symptoms, functional capacity, and QoL in patients with iron deficiency.
Several recent trials have shown that sodium-glucose cotransporter-2 (SGLT2) inhibitors improve clinical outcomes in patients with HFrEF, with or without diabetes [23,24,25,26]. Although these agents also promote weight loss, the relationship between SGLT2-related weight loss and QoL has not been reported.
Patients who do not respond to standard medical therapies for HF or who have advanced HF may receive an implantable left ventricular assist device (LVAD) to support circulation, either as a destination therapy or as a bridge to heart transplantation [27]. The Risk Assessment and Comparative Effectiveness of Left Ventricular Assist Device and Medical Management (ROADMAP) trial showed that patients with advanced HF who received an LVAD had better 1-year survival and physical functioning than patients who were randomized to optimal medical management. LVAD therapy improved QoL, but this effect was moderated by baseline QoL; patients with poor QoL at the time of implantation showed improved QoL, but patients who had relatively good QoL at baseline did not improve [28].
Many cardiac patients with implanted devices experience difficulties in returning to preoperative functional status as well as with altered body image and device-related distress [29]. A recent study of 101 LVAD clinic outpatients showed that 19 months (on average) after surgery, device acceptance was highly variable. Lower device acceptance was associated with younger age (r = 0.36, p < 0.001), depression (r = −0.50, p < 0.001), anxiety (r = −0.50, p < 0.001), and lower quality of life on (r = 0.54, p < 0.001). There was no significant relationship between device acceptance and time since implantation, suggesting that poor acceptance is not a transient problem. Although body image concerns contributed to the overall effect of device acceptance on these patient-reported outcomes, difficulties with return to function and device-related distress were the main drivers of these effects [30]. This suggests that interventions targeting these aspects of LVAD acceptance could help to decrease distress and improve QoL.
The ESC guidelines recommend LVAD implantation in advanced HFrEF, but they do not specifically identify improved QoL as a potential benefit. In contrast, and based on limited evidence, they note that heart transplantation improves QoL in carefully selected recipients with advanced HF [21].
Behavioral Interventions
Early trials of exercise training for patients with HF yielded inconsistent evidence of benefit. The more recent and more definitive HF-ACTION trial demonstrated that relative to usual care alone, exercise training reduces mortality and hospitalizations in medically stable outpatients with HFrEF, although the benefit is modest [31]. The HF-ACTION intervention included 36 supervised, group-based exercise sessions over 3 months followed by a home-based, individual exercise program. This is similar to typical cardiac rehabilitation programs for patients with HF. Quality of life was a secondary outcome of ACTION-HF. The KCCQ overall summary score at 3 months was the primary health status outcome measure. The exercise training group improved approximately 2 points more on the KCCQ by 3 months than the usual care group (p < 0.001). There was no additional improvement in KCCQ scores after 3 months, but the improvement in QoL persisted over a median 2.5-year follow-up [32]. Relative to patients in the usual care group, the patients in the exercise training arm also showed somewhat larger improvements in depression at 3 and 12 months [33].
Exercise training for patients with HF is usually provided by center-based, home-based, or hybrid cardiac rehabilitation programs. Multiple RCTs and meta-analyses have found limited evidence that cardiac rehabilitation decreases mortality and hospitalization, but more consistent evidence that it improves QoL and depression [34,35,36,37,38]. Cardiac rehabilitation can improve QoL both in HFrEF [35] and in HFpEF [39], although there has been less research on rehabilitation for the latter. For a variety of reasons, only about 10% of patients with HF are referred for cardiac rehabilitation. Referrals are gradually increasing over time, but many eligible patients are still not being referred for rehabilitation [40]. In addition, adherence to the exercise regimen is highly variable among patients with HF who enroll in cardiac rehabilitation [41]. In the HF-ACTION trial, adherence declined over time, particularly during the home-based phase of the intervention [32]. Given the beneficial effects of exercise on QoL, depression, and clinical events, interventions to improve adherence to cardiac rehabilitation in general and home-based rehabilitation in particular could help to improve QoL in heart failure.
The Framingham Heart Study showed that obesity increases the risk of incident HF by 5% in men and 7% in women for every one-point increase in body mass index (BMI) [42]. Paradoxically, obesity is associated with a lower risk of mortality in patients who have already developed HF, and there is little evidence that weight loss interventions improve QoL or are beneficial in other ways for patients with HF. Consequently, the ESC guidelines do not recommend weight loss interventions for patients with moderate obesity, although they do suggest that weight loss may improve symptoms, exercise capacity, and QoL in patients with HF and severe obesity (i.e., BMI ≥ 35).
Self-care of HF encompasses two sets of behaviors. Self-care maintenance behaviors include routine daily activities such as symptom monitoring, adherence to medical treatment regimens, and physical exercises that can help to promote physiological and functional stability and to slow the progression of HF. Self-care management behaviors include adaptive responses to HF symptoms when they occur or worsen, such as taking an extra dose of a prescribed diuretic if ankle swelling increases or contacting one’s physician for advice [43]. Longitudinal studies have shown that better self-care predicts better QoL in patients with HF, an effect that is explained in part by the effects of self-care on depression [44, 45]. In addition, a recent study found that self-care reduces the negative effects of HF symptoms and depression on QoL [46]. A patient-level meta-analysis of 20 studies found that self-care interventions improve QoL in patients with HF [47].
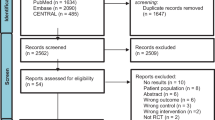
Given the negative effects of depression [48•], treatment of depression is an obvious strategy for improving QoL in patients with HF. However, the two largest RCTs showed that neither sertraline [49] nor escitalopram [50], two well-established antidepressants, is efficacious for comorbid major depression in HF. In contrast, a trial of cognitive behavior therapy showed that it was superior to usual care alone for improving depression, QoL, and other patient-reported outcomes in outpatients with HF and comorbid major depression. As shown in Fig. 1, the participants scored an average of approximately 45 on the KCCQ at baseline; at 6 months, the KCCQ scores were approximately 55 in the usual care group and 63 in the intervention group, for an 8.5-point difference between the groups (p = 0.02). The improvement in QoL tracked with improvement in depression. Starting from a baseline score of approximately 30 on the Beck Depression Inventory (consistent with moderately severe depression), participants in the intervention arm dropped to approximately 13 by 6 months, compared to 17 in the usual care arm (p = 0.008) [51]. Additional trials are needed to evaluate the benefits of cognitive behavior therapy for patients with HF, as well as to test pharmacological and interventional strategies such as transcranial magnetic stimulation that may benefit patients with HF and depression who do not respond to standard first-line antidepressant medications such as sertraline.
Depression and QoL outcomes of a trial of cognitive behavior therapy for major depression in patients with HF. The Beck Depression Inventory (BDI-II; score range, 0–63; higher scores represent worse depression) was used to assess depression, and the Kansas City Cardiomyopathy Questionnaire (KCCQ; score range, 0–100; higher scores represent better quality of life) was used to assess QoL (source: Freedland KE, et al. JAMA Intern Med 2015;175(11):1773–1782) [47]
Conclusions
Heart failure has very negative effects on QoL, and for many patients, maintenance or improvement of QoL is of equal or greater importance as longevity as the overarching goal of treatment. Severe symptoms and functional impairments, comorbidities such as COPD, and depression are major determinants of QoL in HF. QoL often decreases as HF progresses, but certain medical therapies and implantable devices have been shown to improve QoL. Exercise training and cardiac rehabilitation, interventions to improve HF self-care, and interventions for depression are also clinically valuable approaches for improving QoL in patients with HF. Nevertheless, there is a critical need for research to develop more effective interventions to improve QoL as the population ages and the prevalence of HF increases. Tailored exercise programs, interventions for depression, and blended collaborative care interventions [52] are some of the most promising candidates.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
Kraai IH, Vermeulen KM, Luttik ML, Hoekstra T, Jaarsma T, Hillege HL. Preferences of heart failure patients in daily clinical practice: quality of life or longevity? Eur J Heart Fail. 2013;15(10):1113–21.
Stevenson LW, Hellkamp AS, Leier CV, Sopko G, Koelling T, Warnica JW, et al. Changing preferences for survival after hospitalization with advanced heart failure. J Am Coll Cardiol. 2008;52(21):1702–8.
Kelkar AA, Spertus J, Pang P, Pierson RF, Cody RJ, Pina IL, et al. Utility of patient-reported outcome instruments in heart failure. JACC Heart Fail. 2016;4(3):165–75.
Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota living with heart failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J. 1992;124(4):1017–25.
Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City cardiomyopathy questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–55.
Spertus JA, Jones PG. Development and validation of a short version of the Kansas City cardiomyopathy questionnaire. Circ Cardiovasc Qual Outcomes. 2015;8(5):469–76.
Burns DJP, Arora J, Okunade O, Beltrame JF, Bernardez-Pereira S, Crespo-Leiro MG, et al. International Consortium for Health Outcomes Measurement (ICHOM): standardized patient-centered outcomes measurement set for heart failure patients. JACC Heart Fail. 2020;8(3):212–22.
•• Greene SJ, Butler J, Spertus JA, Hellkamp AS, Vaduganathan M, DeVore AD, et al. Comparison of New York Heart Association class and patient-reported outcomes for heart failure with reduced ejection fraction. JAMA Cardiol. 2021. https://doi.org/10.1001/jamacardio.2021.0372. This prospective study found that improvement in quality of life was independently associated with decreased mortality and a reduced risk of heart failure hospitalization.
Spertus JA, Jones PG, Sandhu AT, Arnold SV. Interpreting the Kansas City cardiomyopathy questionnaire in clinical trials and clinical care: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76(20):2379–90.
Comín-Colet J, Martín Lorenzo T, González-Domínguez A, Oliva J, Jiménez MS. Impact of non-cardiovascular comorbidities on the quality of life of patients with chronic heart failure: a scoping review. Health Qual Life Outcomes. 2020;18(1):329.
Baert A, De Smedt D, De Sutter J, De Bacquer D, Puddu PE, Clays E, et al. Factors associated with health-related quality of life in stable ambulatory congestive heart failure patients: systematic review. Eur J Prev Cardiol. 2018;25(5):472–81.
Cascino TM, Kittleson MM, Lala A, Stehlik J, Palardy M, Pamboukian SV, et al. Comorbid conditions and health-related quality of life in ambulatory heart failure patients: REVIVAL (Registry Evaluation of Vital Information for VADs in Ambulatory Life REVIVAL). Circ Heart Fail. 2020;13(5):e006858.
James S, Barton D, O’Connell E, Voon V, Murtagh G, Watson C, et al. Life expectancy for community-based patients with heart failure from time of diagnosis. Int J Cardiol. 2015;178:268–74.
• Sepehrvand N, Savu A, Spertus JA, Dyck JRB, Anderson T, Howlett J, et al. Change of health-related quality of life over time and its association with patient outcomes in patients with heart failure. J Am Heart Assoc. 2020;9(17): e017278. https://doi.org/10.1161/jaha.120.017278. This analysis of data from the Alberta Heart Failure Aetiology and Analysis Team (HEART) cohort showed that decline in quality of life predicts adverse outcomes over 12 months in patients with HFpEF.
Luo N, O’Connor CM, Cooper LB, Sun JL, Coles A, Reed SD, et al. Relationship between changing patient-reported outcomes and subsequent clinical events in patients with chronic heart failure: insights from HF-ACTION. Eur J Heart Fail. 2019;21(1):63–70.
Albuquerque de Almeida F, Al MJ, Koymans R, Riistama J, Pauws S, Severens JL. Impact of hospitalisation on health-related quality of life in patients with chronic heart failure. Health Qual Life Outcomes. 2020;18(1):262.
Mentz RJ, Felker GM. Contemporary medical therapy for heart failure patients with reduced ejection fraction. In: Felker GM, Mann DL, editors. Heart failure: a companion to Braunwald’s heart disease. Fourth edition. ed. Philadelphia, PA: Elsevier; 2020. p. 520–48.
Fedson S, Misra A, Deswal A. Treatment of heart failure with preserved ejection fraction. In: Felker GM, Mann DL, editors. Heart failure: a companion to Braunwald’s heart disease. Fourth edition. ed. Philadelphia, PA: Elsevier; 2020. p. 568–85.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–61.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128(16):1810–52.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Jankowska EA, Tkaczyszyn M, Suchocki T, Drozd M, von Haehling S, Doehner W, et al. Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure: a meta-analysis of randomized controlled trials. Eur J Heart Fail. 2016;18(7):786–95.
Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384(2):117–28.
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–24.
Petrie MC, Verma S, Docherty KF, Inzucchi SE, Anand I, Belohlávek J, et al. Effect of dapagliflozin on worsening heart failure and cardiovascular death in patients with heart failure with and without diabetes. JAMA. 2020;323(14):1353–68.
Brandt EJ, Ross JS, Grady JN, Ahmad T, Pawar S, Bernheim SM, et al. Impact of left ventricular assist devices and heart transplants on acute myocardial infarction and heart failure mortality and readmission measures. PloS One. 2020;15(3):e0230734.
Stehlik J, Estep JD, Selzman CH, Rogers JG, Spertus JA, Shah KB, et al. Patient-reported health-related quality of life is a predictor of outcomes in ambulatory heart failure patients treated with left ventricular assist device compared with medical management: results from the ROADMAP Study (Risk Assessment and Comparative Effectiveness of Left Ventricular Assist Device and Medical Management). Circ Heart Fail. 2017;10(6).
Burns JL, Serber ER, Keim S, Sears SF. Measuring patient acceptance of implantable cardiac device therapy: initial psychometric investigation of the Florida Patient Acceptance Survey. J Cardiovasc Electrophysiol. 2005;16(4):384–90.
Tosto C, Adamo L, Craddock H, Di Blasi M, Girgenti R, Clemenza F, et al. Relationship between device acceptance and patient-reported outcomes in left ventricular assist device (LVAD) recipients. Sci Rep. 2019;9(1):10778.
O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–50.
Flynn KE, Piña IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1451–9.
Blumenthal JA, Babyak MA, O’Connor C, Keteyian S, Landzberg J, Howlett J, et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA. 2012;308(5):465–74.
Kamiya K, Sato Y, Takahashi T, Tsuchihashi-Makaya M, Kotooka N, Ikegame T, et al. Multidisciplinary cardiac rehabilitation and long-term prognosis in patients with heart failure. Circ Heart Fail. 2020;13(10):e006798.
Bjarnason-Wehrens B, Nebel R, Jensen K, Hackbusch M, Grilli M, Gielen S, et al. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: the Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): a systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27(9):929–52.
Taylor RS, Walker S, Smart NA, Piepoli MF, Warren FC, Ciani O, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: individual participant meta-analysis. J Am Coll Cardiol. 2019;73(12):1430–43.
Taylor RS, Long L, Mordi IR, Madsen MT, Davies EJ, Dalal H, et al. Exercise-based rehabilitation for heart failure: Cochrane systematic review, meta-analysis, and trial sequential analysis. JACC Heart Fail. 2019;7(8):691–705.
Imran HM, Baig M, Erqou S, Taveira TH, Shah NR, Morrison A, et al. Home-based cardiac rehabilitation alone and hybrid with center-based cardiac rehabilitation in heart failure: a systematic review and meta-analysis. J Am Heart Assoc. 2019;8(16):e012779.
Gomes-Neto M, Durães AR, Conceição LSR, Roever L, Liu T, Tse G, et al. Effect of aerobic exercise on peak oxygen consumption, VE/VCO(2) slope, and health-related quality of life in patients with heart failure with preserved left ventricular ejection fraction: a systematic review and meta-analysis. Curr Atheroscler Rep. 2019;21(11):45.
Golwala H, Pandey A, Ju C, Butler J, Yancy C, Bhatt DL, et al. Temporal trends and factors associated with cardiac rehabilitation referral among patients hospitalized with heart failure: findings from Get With the Guidelines-Heart Failure Registry. J Am Coll Cardiol. 2015;66(8):917–26.
Deka P, Pozehl B, Williams MA, Yates B. Adherence to recommended exercise guidelines in patients with heart failure. Heart Fail Rev. 2017;22(1):41–53.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347(5):305–13.
Riegel B, Dickson VV, Faulkner KM. The situation-specific theory of heart failure self-care: revised and updated. J Cardiovasc Nurs. 2016;31(3):226–35.
Musekamp G, Schuler M, Seekatz B, Bengel J, Faller H, Meng K. Does improvement in self-management skills predict improvement in quality of life and depressive symptoms? A prospective study in patients with heart failure up to one year after self-management education. BMC Cardiovasc Disord. 2017;17(1):51.
Kessing D, Denollet J, Widdershoven J, Kupper N. Self-care and health-related quality of life in chronic heart failure: a longitudinal analysis. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2017;16(7):605–13.
Auld JP, Mudd JO, Gelow JM, Hiatt SO, Lee CS. Self-care moderates the relationship between symptoms and health-related quality of life in heart failure. J Cardiovasc Nurs. 2018;33(3):217–24.
Jonkman NH, Westland H, Groenwold RH, Agren S, Atienza F, Blue L, et al. Do self-management interventions work in patients with heart failure? An individual patient data meta-analysis Circulation. 2016;133(12):1189–98.
• Patel N, Chakraborty S, Bandyopadhyay D, Amgai B, Hajra A, Atti V, et al. Association between depression and readmission of heart failure: a national representative database study. Prog Cardiovasc Dis. 2020;63(5):585–90. https://doi.org/10.1016/j.pcad.2020.03.014. This analysis of data from the Nationwide Readmission Database found that depression predicts a higher risk of all-cause readmission in patients hospitalized with heart failure.
Jiang W, O’Connor C, Silva SG, Kuchibhatla M, Cuffe MS, Callwood DD, et al. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): a randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. Am Heart J. 2008;156(3):437–44.
Angermann CE, Gelbrich G, Stork S, Gunold H, Edelmann F, Wachter R, et al. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683–93.
Freedland KE, Carney RM, Rich MW, Steinmeyer BC, Rubin EH. Cognitive behavior therapy for depression and self-care in heart failure patients: a randomized clinical trial. JAMA Intern Med. 2015;175(11):1773–82.
Herbeck Belnap B, Anderson A, Abebe KZ, Ramani R, Muldoon MF, Karp JF, et al. Blended collaborative care to treat heart failure and comorbid depression: rationale and study design of the Hopeful Heart Trial. Psychosom Med. 2019;81(6):495–505.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Psychological Aspects of Cardiovascular Diseases
Rights and permissions
About this article
Cite this article
Freedland, K.E., Rich, M.W. & Carney, R.M. Improving Quality of Life in Heart Failure. Curr Cardiol Rep 23, 159 (2021). https://doi.org/10.1007/s11886-021-01588-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01588-y