Abstract
In our effort to cover the interesting aspects of coronary anomalies, we have limited this chapter to a succinct discussion of only three critical issues in the field. First, a unified nomenclature acceptable to the multiple groups involved in this subject is urgently needed: To improve clarity and communication, we must abandon divisive attitudes. We propose a rational, practical scheme that could work well for everybody. Second, the recent acquisition of sound experience in screening populations at risk (elite athletes, military recruits) has led us to recognize that screening magnetic resonance images can reliably identify all high-risk coronary artery anomalies, such that this pathology could potentially be eradicated as a cause of sudden cardiac death in athletes (15–33% of all causes); only 1.5% of the total participating population will require secondary evaluation of severity. Third, the pathophysiology of various types of anomalies can now be recognized as related to coronary stenosis, which affects a few high-risk anomalies, mainly anomalous origin from the right sinus of Valsalva with intramural course (ACAOS-IM). The search for optimal imaging (more than functional testing) has recently led us to prefer intravascular ultrasonography of the ectopic intramural coronary trunk when ACAOS-IM is suspected or advanced exertional activities are involved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Coronary artery stenosis
- Anomalous left coronary artery
- Heart defects, congenital
- Sudden cardiac death
- Diagnostic screening programs
- Diagnostic imaging
Introduction
In this chapter, we provide updates on several critical issues that experts on coronary artery anomalies (CAAs) are currently discussing: (a) A rational nomenclature scheme for CAAs is urgently needed and is potentially available. (b) A core parameter of CAA pathophysiology was recently established, such that the severity of coronary stenosis can now be confidently and consistently established as the single essential factor for evaluating clinical manifestations and risk in CAAs. (c) Prospective screening to detect CAAs in athletes and military recruits is achievable and may substantially lower sudden cardiac death (SCD) rates in these populations.
CAA Nomenclature
Nomenclature is particularly relevant in view of the persistent hodge-podge of terms and acronyms that too frequently confuses clinical service providers. In this regard, for the past 20 years, our group has supported a specific and descriptive staged nomenclature scheme for CAAs (in an initialism style) that brings new clarity to the subject. In particular:
-
1.
The initialism begins with the letter indicating the coronary artery involved, either right (R-) or left (L-).
-
2.
The presence of ectopic origin of the coronary artery, ie, anomalous origin from the right sinus of Valsalva (ACAOS-), follows.
-
3.
The initialism ends with the path the ectopic artery takes to cross to the destination territory, which may be intramural (IM, the only prognostically serious course), prepulmonic (PP), intraseptal (IS), retroaortic (RA), or retrocardiac (RC). See Figs. 8.1 and 8.2. The CAA type and its implicit risk are defined more by this path than by ectopy.
Schematic illustrations of L-ACAOS-IM and L-ACAOS-IS on a coronal plane. (a) An intramural course features a proximal left main coronary artery trunk “attached” (intramural) to the aortic wall (segment in red), whereas (b) in an intraseptal course, the proximal segment of the left main coronary artery is initially extramural/off the aortic root (in yellow) and then intramyocardial at the supraventricular crista and intraventricular septum (in green). ANT anterior side, DIAG diagonal branch of the LAD, IAS interatrial septum, L left sinus of Valsalva, L-ACAOS-IM left coronary artery with anomalous origin from the right sinus of Valsalva and intramural course, L-ACAOS-IS left coronary artery with anomalous origin from the right sinus of Valsalva and intraseptal course, LA left atrium, LAD left anterior descending coronary artery, LT left side, NC noncoronary sinus, OM obtuse marginal coronary artery, OTRV right ventricular outflow tract, PA pulmonary artery, POST posterior side, R right sinus of Valsalva, RA right atrium, RT right side
Magnetic resonance imaging and preferred imaging planes for L-ACAOS-IS and L-ACAOS-IM. (a) In a case of L-ACAOS-IS, the long left main coronary artery trunk (black arrowhead) originates from a common niche with the right coronary artery (white arrow) and follows an oblique course (extramural, separated from the aortic wall) that eventually crosses the RVOT before entering the interventricular septum. (b) In L-ACAOS-IM, the long left main coronary artery trunk is shown to be adjacent to the aortic wall (black arrowhead) in this image taken at the sino-tubular junction, and its early bifurcation is seen. (c) Schematic drawings of the different preferred planes for computed tomography angiography of the L-ACAOS-IM course (left panel) and the L-ACAOS-IS course (right panel); the IM plane is at or about the level of the sino-tubular junction and the ostium of the ectopic artery (this plane also passes across the pulmonary valve), whereas the IS course is better seen in a plane that goes from the origin of the left coronary artery to the right ventricular outflow tract (infundibular). Mild variations are possible in individual cases, and the observer should follow the discipline of initially establishing the expected specific planes for each variant and then following the left main coronary artery above or below that plane (the specific plane is variable and usually not totally apparent in any single tomographic plane). Ao aorta, AoR aortic root, L-ACAOS-IM left coronary artery with anomalous origin from the right sinus of Valsalva and intramural course, L-ACAOS-IS left coronary artery with anomalous origin from the right sinus of Valsalva and intraseptal course, LV left ventricle, MPA main pulmonary artery, PAV pulmonary valve, RA right atrium, RVOT right ventricular outflow tract
ACAOS-IM is characterized by: (1) a tangential origin (usually, but not always, ectopic from the opposite sinus: see also the cases of high-origin and the proper site of origin with IM course [1]); (2) frequently a slit-like orifice; and (3) a constant proximal course within the aortic wall, where the vessel becomes compressed at varying degrees during the cardiac cycle, in different individuals and at different times in their lives. On the contrary, L-ACAOS-IS always implies a straight-down initial epicardial course (a partial interarterial course that is always extramural) directed towards the supraventricular crista of the right ventricle, and then the interventricular septum, before emerging epicardially at the anterior interventricular sulcus and joining the epicardial left anterior descending and circumflex coronary arteries. This anomaly is mostly benign (see Figs. 8.1 and 8.2). An early origin of the first septal branch off the left main coronary artery is a distinctive pathognomonic sign in angiography. The other anomalous courses are essentially benign and extramural.
These concise initialisms quickly and effectively convey essential initial clues as to the pathology involved. Conversely, alternative nomenclatures seem to be generally unhelpful in clarifying the nature of the CAA and its intrinsic prognostic risk. Initialisms like AAOCA (anomalous aortic origin of a coronary artery) or AOCA (anomalous origin of a coronary artery) are simplified versions of our common nomenclature scheme that may be more confusing than useful. Many current investigators prefer subdivisions into consistent clinical entities.
CAA Screening
For several decades, cardiologists and medical organizations have debated and issued statements on the role of CAAs in precipitating SCD in athletes and military recruits and on the use of screening to prevent SCD in similar populations [2, 3]. Candidates for athletic or otherwise strenuous activity are uniquely amenable to routine, accurate preparticipation screening, given that syncopal emergencies and especially SCD are frequently the first symptoms of high-risk congenital conditions. Until such symptoms manifest, these candidates typically continue to train and compete, thereby progressively increasing their risk.
In order to be acceptable, preventive screening must be effective, affordable, and preferentially able to achieve definite primary diagnoses of potentially high-risk CAA(s) in 1 encounter. We have come to realize that prospective screening can indeed be done accurately, cost-effectively, and justifiably in large populations by using new, precise screening methods, such as cardiac magnetic resonance imaging (MRI) [4]. A key reason for MRI-based primary screening is that traditional screening programs (essentially based on history and physical examination plus occasional electrocardiography) generally perform too poorly to be justifiable as a primary program [4]. Indeed, history and physical alone are inadequate for identifying most high-risk cardiovascular conditions, and ACAOS-IM in particular. In contrast, MRI can be as accurate as an autopsy (and in fact has been termed virtual autopsy), requires only a 10–15 min acquisition time, is done without intravenous drugs or contrast agents, and does not induce significant complications.
A recent MRI-based screening study executed under the direction and supervision of the Texas Heart Institute in Houston may now enable the introduction of MRI as a novel basis for general primary screening of candidates for sports activities. In that study of 5169 adolescents (aged 11–18 years) examined by MRI, 1.5% were carriers of potentially high-risk cardiovascular conditions (cardiomyopathies, CAAs, or electrocardiographic abnormalities) [5]. We recognize that this initial study was preliminary, focusing only on the prevalence of high-risk cardiovascular conditions in sports candidates, and had no planned mortality endpoint [5, 6]. A historical study of US military recruits (6.3 million candidates) conducted by Eckart and colleagues [7] found that 33% of SCD events were caused by only one CAA type: L-ACAOS-IM. That population was screened by history and physical, and autopsy was performed on all.
Such new findings lay a strong foundation for restructuring screening programs for elite athletes and military recruits, who are under the supervision and responsibility of schools, sports organizations, or military administrations. Dedicated screening centers could eventually be organized within a comprehensive, integrated network of facilities with trained personnel who could in most cases complete a thorough screening without the need for extensive secondary expert evaluation, except for the rare cases in which a high-risk CAA is discovered at primary screening. In the unlikely event of a positive finding, the individual should be referred for specific expert evaluation (again, probably required in only 1.5% of total cases for the general population of sports candidates). The cost of a screening MRI in a dedicated high-volume center (organized to screen more than 20 cases/day) [4] was expected to be approximately US$200 [5]—the cost of a pair of basketball shoes.
Dedicated screening centers could facilitate the planning and execution of large-scale prospective and controlled studies on mortality risk in MRI-based screening aimed to acquire the evidence necessary to formulate and validate new protocols for effective screening to prevent SCD [6]. Such studies are vital for understanding the incidence of and mortality risk for each specific CAA and the circumstances that precipitate SCD.
Evaluating CAA Severity
If screening identifies potentially severe forms of L-ACAOS-IM, experts can be engaged electively to conduct secondary evaluations to determine the nature and severity of the anomaly. The information gained can be used to reliably advise candidates and to justify selective intervention or disqualification from sports activities.
Anatomical CAAs are numerous and dyshomogeneous (reported as present in 5.6% of patients undergoing cardiac catheterization [8]), but they are mostly clinically benign. Sports cardiologists are more likely to look for L-ACAOS-IM than for the generally benign myocardial bridges or other forms of ACAOS.
L-ACAOS-IM Pathophysiology
Given its inherent relation to intramural course, the term L-ACAOS-IM implies that a coronary artery has been irreversibly misplaced inside the aortic wall during its prenatal development. Under the radial force of the aortic wall, the coronary lumen cannot acquire a circular diameter, which is the most effective shape for a given circumference. After birth, an L-ACAOS-IM will always feature an ovaloid cross-section and will always be narrowed to some degree. The degree of luminal narrowing is at its least during the diastolic phase and at its worst in the systolic phase, even when the individual is at rest.
The simplest way to measure the severity of stenosis is by using the ratio of the widest and narrowest inner diameters in diastole: A ratio of more than 2:1 is indicative of potentially significant stenosis. The length of the stenotic segment is not usually a significant measure of severity, given that the critical site of maximal hemodynamic severity is usually short (less than 3 mm); it is the best site for measuring stenosis for interventional decisions.
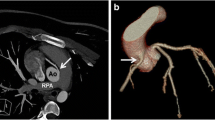
Computerized axial tomography obtained at the aortopulmonary window (the Angelini-Cheong sign [9], see Fig. 8.3) can be useful for grossly quantifying the degree of stenosis. Intravascular ultrasound (IVUS) produces in-vivo video of great precision (30 images per second) and is therefore the most precise and useful method for measuring dynamic stenosis in L-ACAOS-IM in the selected patients. Transthoracic echocardiography produces less-precise measurements due to intrinsic limited precision, but especially because the position of a given planar sectioning is not known (ideally, it should be orthogonal to the luminal axis).
Computed tomography angiograms from a young athlete with unrecognized L-ACAOS-IM who had syncope and chest pain during athletic activities. (a) A vertical cross-section at the level of the aortopulmonary window shows the passage of the ectopic left coronary artery above the sino-tubular junction (white arrow); this is highly suggestive of intramural lateral compression (the Angelini/Cheong sign). (b) A horizontal cross-section above the sino-tubular junction shows the proximal contiguous position of the left main coronary artery trunk (probable intramural course, white arrowhead). Intravascular ultrasound is the definitive method for quantifying severity in L-ACAOS-IM. Ao aorta, L-ACAOS-IM left coronary artery with anomalous origin from the right sinus of Valsalva and intramural course, PA pulmonary artery
In practice, stenotic severity should be obtained during both end-systole and end-diastole [1, 10] and compared with distal reference values (the formula for stenotic area: distal cross-sectional area minus the proximal worse-stenosis cross-sectional area, divided by the distal cross-sectional area). The stenosis spectrum in diastole ranges from 20% to 80% in L-ACAOS-IM and 30–100% in R-ACAOS-IM, being about 10% worse in systole than in diastole. After observing more than 100 cases, including IVUS imaging correlated with symptomatology, we recently proposed that stenosis of more than 50% in L-ACAOS-IM or 60% in R-ACAOS-IM during diastole is suggestive of significant stenosis. Correlations between such data and clinical manifestations vary greatly (especially related to exercise habits); in borderline cases, the SAD test (bolus administration of 500 mL saline solution, plus infusion of atropine 0.5 mg and dobutamine up to 40 μg/kg/min) can be used to simulate actual exertion [10].
The elasticity of the aortic root varies from patient to patient and could be an important parameter to evaluate, especially to explain the progression of symptoms with aging. Systolic values are important to evaluate in athletes, especially because exercise (in the young, more than in the old) leads to significant relative increase in systolic time due to tachycardia (when the systolic time can increase from only 30% of total cardiac cycle time to 70%, as the heart rate reaches approximately 200 beats/min during maximal increase in oxygen demand). Aortic root size increases with aging and the onset of hypertension [1].
L-ACAOS-IS Pathophysiology
In cases of L-ACAOS-IS, the discussion is even more fundamental: (1) An IS (or infundibular) course does not feature stenosis, as can be shown by angiography or IVUS, if the diagnostic procedure is properly protected from guidewire-related spasm by administration of intracoronary nitroglycerin; (2) Advancing a relatively stiff, straight pressure-guidewire through the tortuous intramyocardial anatomy of the L-ACAOS-IS can frequently induce significant coronary spasm that is commonly visible on angiography and the corresponding pressure-wire recordings (Figs. 8.4 and 8.5). Tendency-to-spasm is clearly increased in cases of L-ACAOS-IS, while approximately 30% of these patients will have spontaneous angina that is responsive to nitroglycerin. Incidentally, clinical presentations of spontaneous spasms are relatively frequent in all ACAOS types [1]. We have reviewed the few reported pilot cases of pressure-wire studies (mostly pediatric cases) [11, 12], and our impression is that the recently claimed “frequent” stenoses were not really present at baseline but were artifactual and would have resolved after nitroglycerin administration or wire removal [11, 13], as shown in Figs. 8.4 and 8.5.
Still images from coronary angiograms taken at four different times. (a) Baseline imaging, before any drugs or advancement of coronary wire, normal LCA angiography, with small LAD and dominant RCA; asymptomatic state. (b) Passing a guidewire into the LCA resulted in critical new narrowing at the proximal LAD (epicardial) and chest pain onset, which was relieved promptly by intracoronary nitroglycerin (100 μg, not shown). (c) Three minutes after nitroglycerin, acetylcholine infusion of 50 mcg was followed by chest pain; angiography shows severe LM stenosis, followed by further recurrent stenoses at the LAD (with slow run-off). (d) After intracoronary nitroglycerin, the LM and LAD stenoses disappeared and chest pain resolved. This case was interpreted as demonstrating unusual response with coronary spasm, both to mechanical guidewire stimulation and to ACh administration. Calcium antagonists were administered for long-term treatment (clinically successful). See Fig. 8.5 for pressure readings from the same study. ACH acetylcholine, LAD left anterior descending coronary artery, LCA left coronary artery, LM left main coronary artery, RCA right coronary artery
Pressure-wire gradients (iFR) at the distal position to the origin of the left anterior descending coronary artery. The simple passing of the pressure wire created a mild gradient that increased after ACh testing and resolved completely after NTG administration. a Mild initial gradient while passing the wire (corresponding to the angiogram in Fig. 8.4b). (b) Gradient at the time of ACh testing, indicating severe stenosis of the left main trunk and left anterior descending coronary artery, which shows slow runoff (corresponding to Fig. 8.4c). (c) Gradient after NTG administration, indicating that all stenoses were eliminated; the gradient is absent with the sensor kept distal (corresponding to Fig. 8.4d). ACh acetylcholine, iFR instantaneous wave-free ratio, NTG nitroglycerin
We acknowledge that more experience with L-ACAOS-IS is needed, and prospective controlled studies will have to be performed before strong recommendations can be established. Cardiologists interested in coronary anomalies see L-ACAOS-IS fairly frequently in their adult patients, and they consider spontaneous spastic manifestations to be generally benign if treated with vasodilators [1].
Comments on Pathophysiological Differences Between L-ACAOS-IM and L-ACAOS-IS Studied by Pressure Wire
Recently, some authors have tentatively proposed that the severity of stenosis in L-ACAOS-IM and L-ACAOS-IS can be evaluated more simply by measuring intracoronary pressures (functional flow reserve [FFR] or instantaneous wave-free ratio [iFR]) [11, 12], but spastic complications can increase with this approach, especially in L-ACAOS-IS. Also, FFR (mean gradient through the full cardiac cycle) and iFR (gradient in diastole) have been initially validated only in patients who had atherosclerotic coronary artery disease and mild-to-moderate stenoses on angiography. The practical conclusion of such studies has been that an FFR <0.80 or an iFR <0.89 is associated with more frequent early clinical events in these patients [14,15,16]: Specifically, within a 1-year follow-up, the incidence of mortality, acute myocardial infarction, urgent percutaneous coronary intervention, and cardiac death globally increased in such patients with acquired coronary artery disease [14, 15]. A decreased maximal vasodilatory capacity is not equivalent to proof of resting ischemia, if not during maximal exertion.
Unfortunately, at present there are no prospective or controlled studies that compare prognosis in L-ACAOS-IM versus L-ACAOS-IS; however, Eckart and colleagues [7] reported no cases of L-ACAOS-IS in military recruits. As noted, the systolic and diastolic cross-sectional areas differ from each other only in L-ACAOS-IM, whereas L-ACAOS-IS does not result in coronary narrowing other than that induced by superimposed spasm. In ACAOS-IM, disease progression is quite subtle and difficult to quantitate (especially during a limited 1-year follow-up interval [15]). In young athletes, progression of symptoms is mainly related to exercise habits.
An additional disturbing and objectionable notion has appeared in clinical practice related to ACAOS: the use of the term interarterial course (i.e., located in the free space between the aorta and pulmonary artery) that supposedly may or may not have the IM features we described. Besides the fact that the nature of interarterial course has never been clearly defined, this feature would apparently also include the IM variety (an objectionable confusion of 2 different entities). In reality, especially from our IVUS-based investigative position, the concept that other entities with interarterial course are possible and frequent is not credible; still, 10–15% of patients submitted to surgery “for ACAOS” are not found to have IM course at surgical inspection, and a significant proportion of similar patients (having unroofing or reimplantation of a coronary artery) also have pulmonary translocation [11, 13, 17, 18]. This is difficult to explain, indeed! Clearly, pulmonary artery translocation will not be able to affect IM course inside the aortic wall (the active compressive force is the aortic systolic expansion).
The suspicion is that some clinicians have maintained the early concept of “scissor effect” affecting the ectopic arteries identified as located between the aorta and the pulmonary artery. We do not believe that such stenotic entities exist as an independent entity, and we suggest that much better imaging (especially IVUS) is urgently and routinely needed in all patients recommended for surgery, if doubts persist. The only pass inside the interarterial space is in the proximal IS epicardial course (Fig. 8.1), and neither IM nor IS has any functional result from an interarterial course or a scissor effect. The only relationship that L-ACAOS-IM arteries have with the pulmonary artery is at the level of intramural course, which is inside the aortic wall; the only relationship that L-ACAOS-IS has with the pulmonary artery is by its subpulmonic pass at the right ventricular infundibulum. No scissors can be seen in either of these instances.
References
Angelini P, Uribe C. Anatomic spectrum of left coronary artery anomalies and associated mechanisms of coronary insufficiency. Catheter Cardiovasc Interv. 2018;92:313–21. https://doi.org/10.1002/ccd.27656.
Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the american heart association council on nutrition, physical activity, and metabolism: endorsed by the american college of cardiology foundation. Circulation. 2007;115:1643–455. https://doi.org/10.1161/CIRCULATIONAHA.107.181423.
Rizzo S, De Gaspari M, Frescura C, Padalino M, Thiene G, Basso C. Sudden death and coronary artery anomalies. Front Cardiovasc Med. 2021;8:636589. https://doi.org/10.3389/fcvm.2021.636589.
Angelini P, Muthupillai R, Cheong B, Paisley R. We have plenty of reasons to propose new, updated policies for preventing sudden cardiac death in young athletes. J Am Heart Assoc. 2020;9:e014368. https://doi.org/10.1161/JAHA.119.014368.
Angelini P, Cheong BY, Lenge De Rosen VV, Lopez A, Uribe C, Masso AH, et al. High-risk cardiovascular conditions in sports-related sudden death: prevalence in 5,169 schoolchildren screened via cardiac magnetic resonance. Tex Heart Inst J. 2018;45:205–13. https://doi.org/10.14503/THIJ-18-6645.
Angelini P, Muthupillai R, Lopez A, Cheong B, Uribe C, Hernandez E, et al. Young athletes: preventing sudden death by adopting a modern screening approach? A critical review and the opening of a debate. Int J Cardiol Heart Vasc. 2021;34:100790. in press.
Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141:829–34. https://doi.org/10.7326/0003-4819-141-11-200412070-00005.
Angelini P, Villason S, Chan AV, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Baltimore MD: Lippincott Williams & Wilkins; 1999. p. 27–150.
Cheong BYC, Angelini P. Magnetic resonance imaging of the myocardium, coronary arteries, and anomalous origin of coronary arteries. In: Willerson JT, Holmes Jr DR, editors. Coronary artery disease. London: Springer; 2015. p. 283–337.
Angelini P, Uribe C, Monge J, Tobis JM, Elayda MA, Willerson JT. Origin of the right coronary artery from the opposite sinus of valsalva in adults: characterization by intravascular ultrasonography at baseline and after stent angioplasty. Catheter Cardiovasc Interv. 2015;86:199–208. https://doi.org/10.1002/ccd.26069.
Doan TT, Zea-Vera R, Agrawal H, Mery CM, Masand P, Reaves-O'Neal DL, et al. Myocardial ischemia in children with anomalous aortic origin of a coronary artery with intraseptal course. Circ Cardiovasc Interv. 2020;13:e008375. https://doi.org/10.1161/CIRCINTERVENTIONS.119.008375.
Driesen BW, Warmerdam EG, Sieswerda GT, Schoof PH, Meijboom FJ, Haas F, et al. Anomalous coronary artery originating from the opposite sinus of valsalva (acaos), fractional flow reserve–and intravascular ultrasound-guided management in adult patients. Catheter Cardiovasc Interv. 2018;92:68–75. https://doi.org/10.1002/ccd.27578.
Bigler MR, Ashraf A, Seiler C, Praz F, Ueki Y, Windecker S, et al. Hemodynamic relevance of anomalous coronary arteries originating from the opposite sinus of valsalva-in search of the evidence. Front Cardiovasc Med. 2020;7:591326. https://doi.org/10.3389/fcvm.2020.591326.
Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek JKJJ, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703–8. https://doi.org/10.1056/NEJM199606273342604.
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van't Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24. https://doi.org/10.1056/NEJMoa0807611.
Baumann S, Chandra L, Skarga E, Renker M, Borggrefe M, Akin I, et al. Instantaneous wave-free ratio (ifr((r))) to determine hemodynamically significant coronary stenosis: a comprehensive review. World J Cardiol. 2018;10:267–77. https://doi.org/10.4330/wjc.v10.i12.267.
Jegatheeswaran A, Devlin PJ, McCrindle BW, Williams WG, Jacobs ML, Blackstone EH, et al. Features associated with myocardial ischemia in anomalous aortic origin of a coronary artery: a congenital heart surgeons' society study. J Thorac Cardiovasc Surg. 2019;158:822–34.e3. https://doi.org/10.1016/j.jtcvs.2019.02.122.
Mainwaring RD, Murphy DJ, Rogers IS, Chan FP, Petrossian E, Palmon M, et al. Surgical repair of 115 patients with anomalous aortic origin of a coronary artery from a single institution. World J Pediatr Congenit Heart Surg. 2016;7:353–9. https://doi.org/10.1177/2150135116641892.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Angelini, P., Uribe, C. (2023). Coronary Artery Anomalies: An Updated Discussion on Nomenclature, Pathophysiology, and Screening. In: Butera, G., Frigiola, A. (eds) Congenital Anomalies of Coronary Arteries. Springer, Cham. https://doi.org/10.1007/978-3-031-36966-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-36966-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36965-0
Online ISBN: 978-3-031-36966-7
eBook Packages: MedicineMedicine (R0)