Abstract
Purpose of Review
The surgical management of constrictive pericarditis has evolved from a partial pericardiectomy via a thoracotomy approach to a more extensive removal of the pericardium. This review summarizes the published studies regarding surgical management of pericardial disease, focusing on the surgical technique of radical pericardiectomy for constrictive pericarditis.
Recent Findings
Anterior phrenic to phrenic resection without the use of cardiopulmonary bypass has been performed in many centers. This approach achieves improvement in symptoms; however, there are patients who have progressive constriction of the remaining pericardium requiring a completion pericardiectomy. Recent studies show that the survival and functional outcome is superior after a complete pericardiectomy.
Summary
Our approach is to perform a complete pericardiectomy using cardiopulmonary bypass. In experienced centers, the outcomes have significantly improved with careful selection of patients, advances in pre- and postoperative care, and refinement in surgical techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical treatment for pericarditis was first suggested by Delorme in 1898 [1]. He initially proposed lysis of the intrapericardial adhesions, and then eventually advocated resection of a portion of the pericardium. In 1913, the first pericardiectomy via a left anterolateral thoracotomy was performed in Germany by Rehn and Sauerbruch with improvement in symptoms [2]. The first successful “decortication of the heart” in the USA was performed in 1928 at Massachusetts General Hospital by Dr. Churchill on an 18-year-old girl [3]. Since then, the surgery has evolved from a limited thoracotomy incision with partial excision of the pericardium above the phrenic nerve to a complete resection of the entire pericardium.
Indication for Pericardiectomy
The most common indication for pericardiectomy is constrictive pericarditis (CP) which is characterized by inflammation followed by fibrosis or calcification, thickening, and loss of the normal elasticity of the pericardial sac which leads to impaired filling of the ventricles and diastolic heart failure. Usually, it affects the parietal pericardium; however, the visceral pericardium can also be affected with calcified spikes reaching deep into the myocardium. In “developed” countries, the most common causes are idiopathic, likely due to prior viral pericarditis, post-cardiac surgery, and post-radiation. Tuberculosis is now a rare cause of CP in developed countries, whereas it is a major cause of CP in “developing” countries [4, 5]. Recently, pericardiectomy for chronic recurrent pericarditis is increasing. Surgical treatment is considered when conventional medical therapy, aspirin, NSAIDS, colchicine, and corticosteroids, and alternative treatment options such as azathioprine, intravenous human immunoglobulins, and anakinra have failed or if the patients with complications are requiring high dose of steroids [6]. Large single-center series have demonstrated reduced risk of recurrence and medication use after pericardiectomy for recurrent pericarditis [7, 8].
Complete Resection Versus Anterior Phrenic to Phrenic Resection
Although multiple single-center studies report the benefit of pericardiectomy, there has been no consensus on a standardized surgical technique, which has varied widely from surgeon to surgeon and institution to institution. In addition, as the surgical risk is considered to be high, there is hesitancy to operate on patients with mild symptoms. However, patients with advanced disease are prone to multiple complications and seem not to benefit from surgery [8, 9]. The historical approach, left-sided anterolateral thoracotomy, is done less commonly, as the right-sided pericardium could not be effectively removed. In many centers, pericardiectomy is mainly performed via bilateral thoracotomy with anterior phrenic to phrenic resection of the pericardium without the use of cardiopulmonary bypass due to the technical difficulties in exposing and resecting the diaphragmatic and left lateral portion below the phrenic nerve. Significant improvement in symptoms has been reported, with risk thought to be less than that of more aggressive approaches [10, 11].
However, the anterior portion is only one part of the entire pericardium. Chowdhury et al. [12] reported that survival and functional outcome after complete pericardiectomy was superior compared with that after partial pericardiectomy. Some patients develop progressive constriction of the remaining posterior and diaphragmatic pericardium causing recurrent symptoms resulting in the need for redo pericardiectomy. Cho et al. [13••] reported a series of 41 patients requiring completion pericardiectomy for recurrent constriction after pericardiectomy. The mortality was higher than what would be expected for a primary operation and suggested that a complete resection at the time of the initial pericardiectomy should be done. In our institution, the routine procedure is to perform a complete pericardiectomy, and it is our opinion that, especially in patients who have chronic recurrent pericarditis, partial pericardiectomy should not be performed. Resection of the pericardium should be as thorough as possible to remove the nidus for inflammation if it can be achieved safely.
Cardiopulmonary Bypass
Avoiding the use of cardiopulmonary bypass (CPB) was the preferred approach in many centers due to a perception that pericardiectomy was a high-risk procedure with increased risk of bleeding complications. There are reports that the use of CPB resulted in significantly increased mortality, and the trend was to avoid CPB unless necessary for hemodynamic compromise or bleeding [14]. In most centers, CPB is often utilized as a rescue strategy for catastrophic bleeding, hemodynamic instability, or to allow for concomitant procedures. In light of this fact, CPB use should be considered a marker for increased severity and risk, not a risk factor by itself. It is of note that Chowdhury et al. reported 338 cases of radical pericardiectomy, and only 7 cases were done with CPB. Similarly, in our institution, prior to 2008, an aggressive pericardiectomy was performed with bilateral anterior thoracotomy without the use of CPB. The range of opinion on CPB seems to be (1) to avoid at all cost, (2) to use when necessary to repair bleeding or perform concomitant procedures, or (3) to use routinely to facilitate complete resection. We believe that CPB alone does not increase procedural risk or negatively affect survival, but instead it aids in avoidance of accidental cardiac injury, facilitates maintenance of end-organ perfusion during the dissection of the lateral left ventricle and diaphragmatic surface, and allows for more controlled complete resection. Cho et al. [15] suggest that the use of CPB may allow to better adjust the volume status and to prevent ventricular overload and distension once the constriction is relieved.
Preoperative Evaluation
In addition to obtaining the patient’s history, echocardiography, MRI, and simultaneous left and right heart catheterization are the gold standard in the diagnosis. Restrictive cardiomyopathy and constrictive pericarditis are often challenging to differentiate, and commonly patients have both components (mixed disease) especially in radiation heart disease. In patients with a greater component of restrictive cardiomyopathy, pericardiectomy may not improve hemodynamics or symptoms. Long-term survival is poor, and this must be taken into consideration when planning for surgery. Computed tomographic (CT) imaging is useful in identifying areas of heavy calcium deposits, proximity of cardiac structures including prior bypass grafts.
In inflammatory pericarditis, our experience is that surgery is best performed when the acute inflammation has settled down with anti-inflammatory treatment. Biomarkers such as CRP/ultrasensitive CRP and erythrocyte sedimentation rate can be used to monitor the degree of inflammation. The presence or absence of late pericardial enhancement on gadolinium enhancement MRI will provide information regarding the degree of ongoing inflammation and T2-STIR imaging will evaluate pericardial edema. The use of chronic steroids is associated with increased risk of infection; however, less than 10–20 mg per day of prednisone use usually does not increase the risk of infection.
Tricuspid Regurgitation
Because of the potential for right ventricle (RV) annular size to increase after pericardiectomy, tricuspid repair should be considered in all patients with more than mild tricuspid valve regurgitation (TR). The presence of moderate to severe TR is associated with increased risk of early mortality [16]. Beckman et al. reported that in his series, 12 patients who had more than moderate TR had a 50% survival. Although the addition of a tricuspid valve repair did not alter the short-term outcome, the authors suggested that significant tricuspid regurgitation should be repaired, as this procedure can be performed quickly with low additional risk, as persistent TR is associated with worse long-term survival [17, 18]. Functional tricuspid regurgitation is likely a marker of RV dysfunction and dilatation, which will get worse when the constriction is released and the RV and the tricuspid annulus further dilate [19]. Our approach is to repair more than moderate TR.
Surgical Technique
Previously, at the Cleveland Clinic, pericardiectomy was done through a bilateral thoracotomy with occasional use of CPB. Since 2008, we have changed our approach to median sternotomy and with the routine use of CPB, with aggressive radical resection of the pericardium and pedicalization (removing the pericardium from the phrenic nerve completely leaving a small amount of fat) of both phrenic nerves.
Details of the Operation
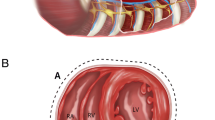
Zoll-pads are placed in all cases. An oscillating saw is used to enter the sternum as there is a high possibility that the underlying structures are adherent to the sternum. Both pleural spaces are widely opened and the phrenic nerves are identified. The pericardium is divided above the lower portion of the RV where the epicardial fat pad is thick and the chances of injury to important structures are low (Fig. 1). The aorta and superior vena cava (SVC) are exposed first, as the pericardium over the aorta and SVC is relatively spared from significant calcification and adhesions (Fig. 2). Systemic heparin is given, cannulas are placed in the aorta and SVC, and partial bypass is initiated (Fig. 3). Rongeurs and bone shears may be needed in cases of heavy calcifications. Once the appropriate plane is identified, the right atrium is dissected free from the adhesions down to the level of the pulmonary veins, and the inferior vena cava (IVC) is cannulated to go on full CPB. The right phrenic nerve is identified and freed from the pericardium with blunt dissection as a fat pedicle, and then the pericardium is completely resected around the IVC. The left side and the diaphragmatic surface of the heart are dissected in a similar manner down to the level of the left pulmonary veins and behind the heart to the oblique sinus. The left phrenic nerve is dissected and preserved in a similar fashion (Fig. 4). Heavy calcification that invades the myocardium, and in cases of effusive constrictive pericarditis, complete resection may have an increased risk of injury to the coronary arteries. In these cases, the constricting layers of the epicardium or calcified pericardium can be incised with multiple crossing incisions in a waffle-like pattern to allow for full expansion of the heart. Injury to small coronary epicardial arteries can be oversewn with fine suture; however, an injury to a major branch may require coronary bypass grafting. In cases with severe adhesions, a thin strip of the pericardium is left attached to the fat pedicle of the phrenic nerve; however, the need for this is rare. The pericardium is then freed from the diaphragm, esophageal fat pad, left inferior pulmonary ligament, and posterior mediastinum, completely freeing the IVC and left PVs, removing large portions of the pericardium as a single sheet using electrocautery at a low-energy setting (Fig. 5). We routinely use the irrigated bipolar cautery and this enables complete hemostasis of the raw tissue even when on CPB with full heparinization. Sharp edges of calcium need to be carefully debrided, as they may erode into the internal thoracic arteries etc. and cause an abrupt increase in bleeding. In addition to large-bore chest tubes, thin drains are left in both pleural spaces, as they will continue to drain for number of days until the coagulopathy and volume overload is corrected, and may need to be discharged with them.
It should be emphasized that complete removal of the pericardium in cases of active inflammation or effusive constrictive disease can be difficult, as there can be intense inflammation of the epicardium and epicardial fat. The surgeon must be careful in achieving a complete resection as possible without going so deep as to injure epicardial veins and arteries which are quite superficial. In general, the appropriate layer is clear when the underlying heart expands and contracts well without tethering.
Postoperative Management
Avoiding RV distension with the use of low-dose inotropes, fluid restriction, and atrial pacing if needed are some of the basic strategies. The target is not to achieve a normal cardiac output, rather a slightly higher cardiac output than prior to surgery. There is no need to increase the inotropic support with a marginal cardiac index as long as the CVP and the PA pressures have improved. Patients with low cardiac index pre- and postoperatively have worse outcome, which indicates a greater component of restriction than constriction, as in post-radiation mixed disease. In patients who have cardiac cirrhosis, we have experienced severe vasoplegia lasting for the first couple days, despite improvement in cardiac output. A unique complication following pericardiectomy can happen when severe constriction is released and the ventricle is suddenly volume loaded leading to distension of the heart. This phenomenon is seen when pericardiectomy is done without the use of CPB, and RV constriction is released prior to releasing the LV constriction, resulting in RV overload and distension, causing actin-myosin dissociation of the sarcomeres. Once this happens, the ventricle may have severe dysfunction leading rapidly to cardiogenic shock, cardiac arrest, and death and only ECMO insertion in a timely manner is the main salvage in this situation. Beckman et al. [17] focused on patients requiring ECMO post-pericardiectomy, and found that patients who had signs of RV failure, hepatic congestion, and malnutrition were at high risk for needing ECMO support. Pulmonary hypertension is not directly caused by constriction; rather, it is caused by the underlining disease process, such as prior radiation therapy resulting in lung fibrosis. The weak RV will have difficulty handling the high pulmonary pressures. Strategies to decrease RV afterload such as optimizing the ventilator settings, treating the acid-base imbalance, and use of inhaled prostacyclin or nitric oxide may be needed, thus avoiding drugs that may cause pulmonary vasoconstriction. If no sign of recovery, early ECMO implantation is crucial to avoid irreversible damage to the ventricle.
Outcomes
The mortality rate varies among the studies, from 0 to 18% [5, 7, 9, 10, 12, 14, 17, 20, 21, 22•, 23,24,25,26,27,28,29]. Murashita et al. published the results of pericardiectomy performed for various indications since 1936 at the Mayo Clinic which showed that the 30-day mortality was 13.5% prior to 1990, 5.2% after 1990 (p < 0.001). Early mortality has improved; however, the 5- and 10-year survival has worsened, and this is most likely influenced by the underlying disease and comorbidities and elevated risk of the patients who underwent pericardiectomy in the recent era. Khandaker et al. reported the outcome of patients who underwent pericardiectomy for persistent relapsing pericarditis after failed medical management and showed excellent results: 0% perioperative mortality and 3% morbidity, proving that pericardiectomy itself is a low-risk procedure. The major determinant of long-term survival for constrictive pericarditis is etiology, as pointed out by several reports [18, 20]. Idiopathic constriction has excellent short- and long-term results, whereas post-radiation and post-surgical constriction had worse early and late outcomes [13••]. Bertog et al. [18] from our institution reported that the 7-year survival of idiopathic CP, post-cardiac surgery, and post-radiation was 88%, 66%, and 27%, respectively. Similarly, Szabo et al. [25] reported 81%, 50%, and 0% at 5 years, respectively.
Radiation can cause additional adhesions and will affect all the structures that are within the radiation field causing fibrosis and calcification of the valve, aorta, coronary artery, pericardium, myocardium, intervalvular fibrosa, lungs, and diaphragm. Patients who underwent prior cardiac surgery have adhesions and may have coronary bypass grafts that need to be carefully dissected out which makes the operation challenging. Furthermore, the underlying cardiac disease may determine the long-term survival. These issues should be kept in mind when selecting patients for surgery. Idiopathic constriction may benefit from early operation, post-radiation patients may require extreme caution, and we rarely offer surgery unless there are significant valve or coronary diseases that can be corrected at the time of operation.
At the Cleveland Clinic, in recent series, 601 patients underwent pericardiectomy within the period 1977 to 2013. Overall in-hospital mortality was 6%: 1.1% for idiopathic pericarditis, 9.7% postoperative, and 27% post-radiation. One-, 5-, 10-, 15-, and 20-year survival was 87%, 73%, 60%, 45%, and 30%, respectively. There were no differences in survival based on the completeness of resection or use of CPB. Even with the aggressive resection and the use of CPB, reoperation for bleeding was low (3.8%). With the advances in the postoperative management, the need for IABP and ECMO was low, 2.6% and 1.7%, respectively.
Conclusions
The outcome of pericardiectomy has varied between institutions and the era of the operation, and has shown considerable improvement in short-term outcome in experienced centers. The long-term outcome is determined by the underlying etiology, the comorbidity, and the myocardial reserve, and patients need to be carefully selected. We advocate aggressive removal of the entire pericardium, especially in patients who have relapsing pericarditis, as it will not increase the operative risk and may improve the long-term outcome. The use of cardiopulmonary bypass should be considered not only for rescue, but for support to improve the quality of operation. Further study needs to be done whether our new approach translates to better long-term survival and long-term symptomatic relief.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Delorme E. Sur un traitement chirurgical: De la symphyse cardopéricardique. Gaz Des Hôp. 1898;71:1150–1.
Rehn L. Ueber pericardiale Verwachsungen. Med Klin. 1920;16:991.
Churchill ED. Decortication of the heart (Delorme) for adhesive pericarditis. Arch Surg. 1929;19:1457.
Mutyaba AK, Balkaran S, Cloete R, du Plessis N, Badri M, Brink J, et al. Constrictive pericarditis requiring pericardiectomy at Groote Schuur Hospital, Cape Town, South Africa: causes and perioperative outcomes in the HIV era (1990-2012). J Thorac Cardiovasc Surg. 2014;148(6):3058–65 e1.
George TJ, Arnaoutakis GJ, Beaty CA, Kilic A, Baumgartner WA, Conte JV. Contemporary etiologies, risk factors, and outcomes after pericardiectomy. Ann Thorac Surg. 2012;94(2):445–51.
Imazio M, Lazaros G, Brucato A, Gaita F. Recurrent pericarditis: new and emerging therapeutic options. Nat Rev Cardiol. 2016;13(2):99–105.
Gillaspie EA, Stulak JM, Daly RC, Greason KL, Joyce LD, Oh J, et al. A 20-year experience with isolated pericardiectomy: analysis of indications and outcomes. J Thorac Cardiovasc Surg. 2016 Aug;152(2):448–58.
Khandaker MH, Schaff HV, Greason KL, Anavekar NS, Espinosa RE, Hayes SN, et al. Pericardiectomy vs medical management in patients with relapsing pericarditis. Mayo Clin Proc. 2012 Nov;87(11):1062–70.
Avgerinos D, Rabitnokov Y, Worku B, Neragi-Miandoab S, Girardi LN. Fifteen-year experience and outcomes of pericardiectomy for constrictive pericarditis. J Card Surg. 2014;29(4):434–8.
Nishimura S, Izumi C, Amano M, Imamura S, Onishi N, Tamaki Y, et al. Long-term clinical outcomes and prognostic factors after pericardiectomy for constrictive pericarditis in a Japanese population. Circ J. 2017;81(2):206–12.
Nataf P, Cacoub P, Dorent R, Jault F, Bors V, Pavie A, et al. Results of subtotal pericardiectomy for constrictive pericarditis. Eur J Cardiothorac Surg. 1993;7(5):252–5 discussion 5-6.
Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, et al. Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques. Ann Thorac Surg. 2006;81(2):522–9.
•• Cho YH, Schaff HV, Dearani JA, Daly RC, Park SJ, Li Z, et al. Completion pericardiectomy for recurrent constrictive pericarditis: importance of timing of recurrence on late clinical outcome of operation. Ann Thorac Surg. 2012;93(4):1236–40 This study highlights the importance of radical pericardiectomy vs partial pericardiectomy.
Rupprecht L, Putz C, Florchinger B, Zausig Y, Camboni D, Unsold B, et al. Pericardiectomy for constrictive pericarditis: an institution’s 21 years experience. Thorac Cardiovasc Surg. 2018;66:645–50.
Cho YH, Schaff HV. Surgery for pericardial disease. Heart Fail Rev. 2013;18(3):375–87.
Gongora E, Dearani JA, Orszulak TA, Schaff HV, Li Z, Sundt TM 3rd. Tricuspid regurgitation in patients undergoing pericardiectomy for constrictive pericarditis. Ann Thorac Surg. 2008;85(1):163–70 discussion 70-1.
Beckmann E, Ismail I, Cebotari S, Busse A, Martens A, Shrestha M, et al. Right-sided heart failure and extracorporeal life support in patients undergoing pericardiectomy for constrictive pericarditis: a risk factor analysis for adverse outcome. Thorac Cardiovasc Surg. 2017;65(8):662–70.
Bertog SC, Thambidorai SK, Parakh K, Schoenhagen P, Ozduran V, Houghtaling PL, et al. Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. J Am Coll Cardiol. 2004;43(8):1445–52.
Johnson TL, Bauman WB, Josephson RA. Worsening tricuspid regurgitation following pericardiectomy for constrictive pericarditis. Chest. 1993;104(1):79–81.
Busch C, Penov K, Amorim PA, Garbade J, Davierwala P, Schuler GC, et al. Risk factors for mortality after pericardiectomy for chronic constrictive pericarditis in a large single-centre cohort. Eur J Cardiothorac Surg. 2015;48(6):e110–6.
Lin X, Xu RY, Liu JZ, Chen W, Chen LF, Yang PH, et al. Effect of right heart systolic function on outcomes in patients with constrictive pericarditis undergoing pericardiectomy. Chin Med J. 2016;129(2):154–61.
• Murashita T, Schaff HV, Daly RC, Oh JK, Dearani JA, Stulak JM, et al. Experience with pericardiectomy for constrictive pericarditis over eight decades. Ann Thorac Surg. 2017;104(3):742–50 Large series study regarding the outcome of pericardiectomy which demonstrated that the long-term survival is determined by the etiology of constriction.
Zhu P, Mai M, Wu R, Lu C, Fan R, Zheng S. Pericardiectomy for constrictive pericarditis: single-center experience in China. J Cardiothorac Surg. 2015;10:34.
Kang SH, Song JM, Kim M, Choo SJ, Chung CH, Kang DH, et al. Prognostic predictors in pericardiectomy for chronic constrictive pericarditis. J Thorac Cardiovasc Surg. 2014;147(2):598–605.
Szabo G, Schmack B, Bulut C, Soos P, Weymann A, Stadtfeld S, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg. 2013;44(6):1023–8 discussion 8.
Tiruvoipati R, Naik R, Loubani M, Billa G. Surgical approach for pericardiectomy: a comparative study between median sternotomy and left anterolateral thoracotomy. Interact Cardiovasc Thorac Surg. 2003;2(3):322–6.
Thompson JL, Burkhart HM, Dearani JA, Cetta F, Oh JK, Schaff HV. Pericardiectomy for pericarditis in the pediatric population. Ann Thorac Surg. 2009;88(5):1546–50.
Lin Y, Zhou M, Xiao J, Wang B, Wang Z. Treating constrictive pericarditis in a chinese single-center study: a five-year experience. Ann Thorac Surg. 2012;94(4):1235–40.
Tokuda Y, Miyata H, Motomura N, Araki Y, Oshima H, Usui A, et al. Outcome of pericardiectomy for constrictive pericarditis in Japan: a nationwide outcome study. Ann Thorac Surg. 2013;96(2):571–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Shinya Unai and Douglas R. Johnston declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pericardial Disease
Rights and permissions
About this article
Cite this article
Unai, S., Johnston, D.R. Radical Pericardiectomy for Pericardial Diseases. Curr Cardiol Rep 21, 6 (2019). https://doi.org/10.1007/s11886-019-1092-1
Published:
DOI: https://doi.org/10.1007/s11886-019-1092-1