Abstract
Purpose of Review
A number of recent observational analyses have assessed clinical outcomes associated with digoxin use in patients with atrial fibrillation. In this review, we review these data and provide suggestions on the contemporary use of digoxin in patients with atrial fibrillation as supported by the recent evidence.
Recent Findings
Observational data from clinical trials and registries have provided variable results on the safety and efficacy of chronic digoxin use in patients with atrial fibrillation. In general, results have been consistent with an associated increase in adverse clinical outcomes with digoxin use in atrial fibrillation patients without heart failure. In atrial fibrillation patients with heart failure, while the weight of evidence suggested an associated risk with digoxin therapy, the results are inconsistent.
Summary
In patients with atrial fibrillation without heart failure, digoxin should generally be avoided. In atrial fibrillation patients with heart failure, digoxin should generally be reserved for patients that do not achieve adequate rate control or are not tolerant of other rate control therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Digoxin is a cardiac glycoside that inhibits the sodium-potassium adenosine triphosphatase (ATPase), mainly in cardiac tissue, and has been used as a therapeutic in patients with cardiovascular conditions for over 200 years. Clinical indications for which digoxin is used include atrial fibrillation and heart failure. While one large, randomized controlled trial has been conducted assessing the safety and efficacy of digoxin in ambulatory patients in normal sinus rhythm with chronic heart failure [1], there are no randomized controlled trial data that have assessed the safety and efficacy of digoxin on clinical outcomes in patients with atrial fibrillation (AF). Subsequently, a number of observational analyses have been published in recent years which have assessed the association of digoxin use on clinical outcomes in patients with AF.
The purpose of this review will be to present these data on digoxin use and outcomes in patients with AF and to provide suggestions regarding the contemporary use of digoxin as a ventricular rate control agent in AF.
Guideline Recommendations for Digoxin as a Ventricular Rate Control Agent
While the recent American Heart Association/American College of Cardiology/Heart Rhythm Society Practice Guidelines on AF state that digoxin is not usually a first-line medication for ventricular rate control [2], observations from contemporary clinical trials evaluating oral anticoagulant therapies for stroke prevention in patients with AF have reported baseline digoxin use in approximately one out of every three patients, highlighting how commonly digoxin is prescribed for ventricular rate control [3,4,5]. The Guidelines do provide favorable recommendations for chronic digoxin use in patients with heart failure. The Guidelines give a Class I Recommendation (Level of Evidence (LOE): C) for digoxin being effective to control resting heart rate in patients with heart failure with reduced ejection fraction (HFrEF) and a Class IIa Recommendation (LOE: B) for digoxin use in combination with beta blockers (or non-dihydropyridine calcium channel blocker in patients with heart failure with preserved ejection fraction (HFpEF)) as a reasonable strategy to control resting and exercise heart rate [2]. Lastly, the Guidelines provide a Class I (LOE: B) Recommendation for intravenous digoxin to control heart rate acutely in patients with heart failure [2].
Digoxin Use and Outcomes in Atrial Fibrillation
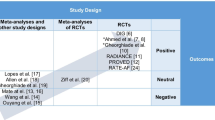
Post hoc analyses of randomized clinical trials and registries have been the primary sources of data on chronic digoxin use and associated outcomes in patients with AF. A summary of these data can be viewed in Tables 1 and 2.
Clinical Trial Observations on Digoxin Use and Outcomes in Atrial Fibrillation
An initial post hoc analysis of the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) trial, which randomized patients with AF to a rate or rhythm control strategy, raised concern over the safety of digoxin use [20]. Results from this initial analysis showed digoxin use was associated with an increased risk of death (HR, 1.42 (1.09–1.86)). Subsequently, two additional post hoc analyses of the AFFIRM data each assessing digoxin use on clinical outcomes were published [6, 7].
The first analysis, which analyzed digoxin using a time-dependent treatment indicator, showed digoxin use to be associated with an increase in all-cause mortality, cardiovascular mortality, and arrhythmic mortality [6]. The association of digoxin use and all-cause mortality was observed in both patients with and those without heart failure. The second analysis utilized propensity score matching as opposed to a time-dependent treatment methodology based upon the reasoning that time-dependent changes to digoxin were likely to have not occurred randomly and it was likely that changes in digoxin were related to changing or worsening clinical condition [7]. The results of this analysis found that digoxin use was not associated with an increase in mortality in the propensity-matched cohort. In addition, baseline digoxin use was not associated with all-cause mortality in either propensity-matched patients with heart failure (adjusted HR, 1.08 (0.69–1.69)) or those without heart failure (adjusted HR, 1.08 (0.80–1.47)).
Observations on digoxin use and outcomes have been published from several clinical trials comparing non-vitamin K oral anticoagulants (NOACs) to warfarin for stroke prevention in patients with AF. The first of these was a post hoc analysis of the Stroke Prevention using an Oral Thrombin Inhibitor in atrial Fibrillation (SPORTIF) III and V trials which randomized patients with AF to warfarin or ximelagatran [8]. After adjustment, digoxin use was associated with an increased risk of all-cause mortality (HR, 1.58 (1.29–1.94)).
More recently, observations from contemporary trials of NOACs vs. vitamin K antagonists have provided further evidence assessing digoxin use and outcomes in patients with AF. The first report came from the Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compare with Vitamin K Antagonism for Prevention of Stroke and Embolism (ROCKET AF) trial [9]. At baseline, 37% of patients were receiving digoxin. After adjustment, digoxin use was associated with an increase in all-cause mortality (HR, 1.17 (1.04–1.32)) and sudden death (HR, 1.36 (1.08–1.70)). In this analysis, the increase in all-cause mortality associated with digoxin use was seen in both patients with and patients without heart failure.
The association of digoxin use and outcomes observed in the Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48 (ENGAGE AF-TIMI 48) was subsequently published [10]. Outcomes in patients with and without heart failure were assessed utilizing three statistical techniques including Cox proportional hazards modeling, propensity matching, and inverse probability treatment weighting (IPTW). After propensity matching, patients with heart failure, digoxin use was associated with a significant increase in the risk for all-cause death (HR, 1.31 (1.19–1.43)) and sudden cardiac death (HR, 1.58 (1.36–1.85)). In patients without heart failure, digoxin use was not associated with a statistically significant increase in all-cause death (HR, 1.16 (0.98–1.36)), although an increase in sudden cardiac death associated with digoxin was observed (HR, 1.90 (1.36–2.65)). Similar results for the outcomes above were also observed using Cox proportional hazards modeling and IPTW.
Most recently, clinical trial observations of digoxin use from the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial have been published [11•]. In this analysis, baseline use of digoxin was not associated with an increased risk of all-cause mortality (HR, 1.09 (0.96–1.23)). However, similar to previous analyses of digoxin use in atrial fibrillation and heart failure [21, 22], this analysis did show an associated increased risk of mortality in digoxin users with higher serum concentrations (defined as ≥ 1.2 ng/mL) (HR, 1.56 (1.20–2.04)). In addition, patients who were started on digoxin during the conduct of the trial were observed to have an increased risk of death and sudden cardiac death, and these results were observed in both patients with and patients without heart failure.
Registry Observations of Digoxin Use and Outcomes in Atrial Fibrillation
Data from large observational registries on the use of digoxin and outcomes in patients with AF have also recently been published with varying results. One of the initial registry reports on digoxin use in AF came from the Registry of Information and Knowledge about Swedish Heart Intensive Care (RIKS-HIA) [13]. Notably, the cohort of patients in this analysis was enrolled after admission to a coronary care unit in Sweden and survived to hospital discharge. After 1 year of follow-up, results showed that compared with patients not receiving digoxin, digoxin use was associated with a higher mortality rate in patients with AF without heart failure (RR, 1.42 (1.29–1.56)) while no significant association was observed in AF patients with heart failure.
An analysis from the Stockholm Cohort study of Atrial Fibrillation (SCAF) enrolled hospitalized patients (that survived to discharge) or outpatients that had received a diagnosis of AF or atrial flutter [14]. This analysis reported no association of digoxin use on adjusted risk for mortality in patients (HR, 1.10 (0.94–1.28)). In contrast, registry data from a large national health registry in Taiwan compared outcomes in AF patients receiving an agent for rate control to patients with atrial fibrillation no receiving rate control treatments [15]. After adjustment, use of beta blocker and calcium channel blocker therapy was associated with a lower risk of mortality compared to patients not receiving rate control treatment while digoxin use was associated with an increased risk of mortality (HR, 1.12 (1.10–1.14)). Similar results were observed in patients with and without heart failure.
An analysis from the contemporary US Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) showed in patients with heart failure that neither prevalent nor incident digoxin use was associated with mortality [18]. However, this analysis did show an association between incident digoxin use and mortality in patients without heart failure (HR, 1.99 (1.12–3.56)). Similar results were observed in patients with no previous heart failure or digoxin use in the AnTicoagulation and Risk factors In Atrial fibrillation-Cardiovascular Research Network (ATRIA-CVRN) study [17]. Results from this analysis showed incident digoxin use to be independently associated with a higher risk of death (HR, 1.63 (1.56–1.71). In addition, among digoxin-treated patients with a measured serum digoxin concentration, the mean serum digoxin concentration was higher in patients who died compared to those that did not die (1.15 vs. 0.94 ng/mL; p < 0.001).
Lastly, the experience from the Retrospective Evaluation and Assessment of Therapies in AF (TREAT-AF) study represents one of the largest observations to date [16•]. This analysis included patients with newly diagnosed AF within 90 days seen in an outpatient setting. The results showed that digoxin use was independently associated with mortality (HR, 1.26 (1.23–1.29)). Similar results were observed after propensity matching and were not modified by heart failure status.
Summary of Evidence
Over the last 10 years, multiple observational analyses have assessed the safety of digoxin in patients with heart failure with varying results. Given the observational nature of these data, there are inherent limitations including the lack of randomization to digoxin therapy (aimed at reducing unmeasured patient variables) and the lack of blinding, although some analysis have done blinded adjudication of events. Specifically, patients receiving digoxin were generally older and had a higher burden of co-morbid medical conditions. Therefore, in spite of the sophisticated statistical techniques utilized in these analyses, residual confounding or confounding by indication cannot be excluded. Lastly, most of the analyses to date did not include data on the digoxin dose or serum concentrations, thus, limiting the ability to assess the relationship between digoxin exposure and clinical outcomes across the different analyses.
In light of the inconsistent results published to date, a systematic review with the aim to assess the association of digoxin use on mortality in patients with AF was recently published [23]. This review, which included 16 studies, reported digoxin use was associated with an increase in all-cause mortality (pooled HR, 1.27 (CI 1.19–1.36)) and the effect size was larger in AF patients without heart failure (pooled HR, 1.47 (1.25–1.73)) than AF patients with heart failure (pooled HR, 1.21 (1.07–1.36)) (Pinteraction = 0.06).
Current Role for Digoxin in the Management of Atrial Fibrillation
The most consistent finding in the observations to date has been an association with digoxin use on adverse outcomes in AF patients without heart failure while results have been more inconsistent in patients with heart failure. In light of the current evidence, we would suggest attempting to avoid digoxin use for ventricular rate control in AF patients without heart failure unless patients are intolerant of other rate control agents. In patients with heart failure (HFrEF), we would suggest limiting digoxin use to those patients that do not achieve adequate rate control on beta blocker therapy or are intolerant of beta blocker therapy. In addition, when digoxin is used, careful attention should be paid to appropriate dosing and monitoring. Furthermore, based on the current evidence, we suggest targeting a lower serum digoxin concentration (less than 1.0 ng/mL).
The evidence presented and discussed in this review have largely been in ambulatory AF patients receiving chronic digoxin therapy. However, clinical questions regarding digoxin therapy for acute heart rate control frequently occur. A recent systematic review attempted to provide further insight into digoxin therapy for acute ventricular rate control [24]. A total of 28 trials, with a mean follow-up of 18 h were included. Results showed digoxin to be superior to placebo for acute ventricular rate control but inferior to beat blockers, calcium channel blockers, and amiodarone. Therefore, in patients with AF presenting with an indication for acute ventricular rate control who are intolerant of other rate control medications, digoxin therapy could be attempted. This strategy is consistent with current Guideline recommendations for intravenous digoxin therapy for acute rate control in patients with heart failure [2].
Conclusion
A number of observational analyses have been published over the past decade assessing digoxin use and outcomes in patients with AF. Results have been inconsistent in patients with heart failure and have generally associated digoxin use and with adverse outcomes in patients without heart failure. Finally, the current observations support targeting lower serum digoxin concentrations in patients with AF. The limitations in the available data and the inconsistency in results highlight the need for a randomized controlled trial to provide further clarity on the role of digoxin in patients with atrial fibrillation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Digitalis Investigation G. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336(8):525–33.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Whitbeck MG, Charnigo RJ, Khairy P, Ziada K, Bailey AL, Zegarra MM, et al. Increased mortality among patients taking digoxin--analysis from the AFFIRM study. Eur Heart J. 2013;34(20):1481–8.
Gheorghiade M, Fonarow GC, van Veldhuisen DJ, Cleland JG, Butler J, Epstein AE, et al. Lack of evidence of increased mortality among patients with atrial fibrillation taking digoxin: findings from post hoc propensity-matched analysis of the AFFIRM trial. Eur Heart J. 2013;34(20):1489–97.
Gjesdal K, Feyzi J, Olsson SB. Digitalis: a dangerous drug in atrial fibrillation? An analysis of the SPORTIF III and V data. Heart. 2008;94(2):191–6.
Washam JB, Stevens SR, Lokhnygina Y, Halperin JL, Breithardt G, Singer DE, et al. Digoxin use in patients with atrial fibrillation and adverse cardiovascular outcomes: a retrospective analysis of the Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF). Lancet. 2015;385(9985):2363–70.
Eisen A, Ruff CT, Braunwald E, Hamershock RA, Lewis BS, Hassager C et al. Digoxin use and subsequent clinical outcomes in patients with atrial fibrillation with or without heart failure in the ENGAGE AF-TIMI 48 Trial. J Am Heart Assoc. 2017;6(7).
• Lopes RD, Rordorf R, De Ferrari GM, Leonardi S, Thomas L, Wojdyla DM, et al. Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol. 2018;71(10):1063–74. This analysis from the ARISTOTLE trial showed in atrial fibrillation patients taking digoxin, the risk of death was independently associated with serum digoxin concentrations.
Mulder BA, Van Veldhuisen DJ, Crijns HJ, Tijssen JG, Hillege HL, Alings M, et al. Digoxin in patients with permanent atrial fibrillation: data from the RACE II study. Heart Rhythm. 2014;11(9):1543–50.
Hallberg P, Lindback J, Lindahl B, Stenestrand U, Melhus H, group R-H. Digoxin and mortality in atrial fibrillation: a prospective cohort study. Eur J Clin Pharmacol. 2007;63(10):959–71.
Friberg L, Hammar N, Rosenqvist M. Digoxin in atrial fibrillation: report from the Stockholm Cohort study of Atrial Fibrillation (SCAF). Heart. 2010;96(4):275–80.
Chao TF, Liu CJ, Tuan TC, Chen SJ, Wang KL, Lin YJ, et al. Rate-control treatment and mortality in atrial fibrillation. Circulation. 2015;132(17):1604–12.
• Turakhia MP, Santangeli P, Winkelmayer WC, Xu X, Ullal AJ, Than CT, et al. Increased mortality associated with digoxin in contemporary patients with atrial fibrillation: findings from the TREAT-AF study. J Am Coll Cardiol. 2014;64(7):660–8. This article represents one of the largest observational studies to date assessing digoxin use in patients with atrial fibrillation.
Freeman JV, Reynolds K, Fang M, Udaltsova N, Steimle A, Pomernacki NK, et al. Digoxin and risk of death in adults with atrial fibrillation: the ATRIA-CVRN study. Circ Arrhythm Electrophysiol. 2015;8(1):49–58.
Allen LA, Fonarow GC, Simon DN, Thomas LE, Marzec LN, Pokorney SD, et al. Digoxin use and subsequent outcomes among patients in a contemporary atrial fibrillation cohort. J Am Coll Cardiol. 2015;65(25):2691–8.
Pastori D, Farcomeni A, Bucci T, Cangemi R, Ciacci P, Vicario T, et al. Digoxin treatment is associated with increased total and cardiovascular mortality in anticoagulated patients with atrial fibrillation. Int J Cardiol. 2015;180:1–5.
Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, et al. Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. Circulation. 2004;109(12):1509–13.
Hohnloser SH, Halperin JL, Camm AJ, Gao P, Radzik D, Connolly SJ, et al. Interaction between digoxin and dronedarone in the PALLAS trial. Circ Arrhythm Electrophysiol. 2014;7(6):1019–25.
Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM. Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA. 2003;289(7):871–8.
Qureshi W, O'Neal WT, Soliman EZ, Al-Mallah MH. Systematic review and meta-analysis of mortality and digoxin use in atrial fibrillation. Cardiol J. 2016;23(3):333–43.
Sethi NJ, Nielsen EE, Safi S, Feinberg J, Gluud C, Jakobsen JC. Digoxin for atrial fibrillation and atrial flutter: a systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. PLoS One. 2018;13(3):e0193924.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jeffrey B. Washam declares no conflicts of interest.
Manesh R. Patel reports grants and personal fees from Bayer Pharmaceuticals, Janssen, and AstraZeneca; and grants from HeartFlow and NHLBI.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Washam, J.B., Patel, M.R. Is There Still a Role for Digoxin in the Management of Atrial Fibrillation?. Curr Cardiol Rep 20, 105 (2018). https://doi.org/10.1007/s11886-018-1047-y
Published:
DOI: https://doi.org/10.1007/s11886-018-1047-y