Abstract
Objective
The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study showed that rhythm-control treatment of patients with atrial fibrillation (AF) offered no survival advantage over a rate-control strategy. In a subgroup analysis of that study, it was found that digoxin increased the death rate [relative risk (RR) = 1.42), but it was suggested that this may have been attributable to prescription of digoxin for patients at greater risk of death, such as those with congestive heart failure (CHF). No study has investigated a priori the effect of digoxin on mortality in patients with AF. This study aimed to address this question.
Methods
Using data from the Registry of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS-HIA), we studied the 1-year mortality among patients admitted to coronary care units with AF, CHF, or AF+CHF with or without digoxin (n = 60,764) during 1995–2003. Adjustment for differences in background characteristics and other medications and treatments was made by propensity scoring.
Results
Twenty percent of patients with AF without CHF in this cohort were discharged with digoxin. This group had a higher mortality rate than the corresponding group not given digoxin [adjusted RR 1.42 (95% CI 1.29–1.56)], whereas no such difference was seen among patients with CHF with or without AF, although these patients had a nearly three-times higher mortality.
Conclusion
The results suggest that long-term therapy with digoxin is an independent risk factor for death in patients with AF without CHF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Digoxin is widely used in clinical practice for treatment of congestive heart failure (CHF) and atrial fibrillation (AF). Whereas the efficacy of digoxin in AF has been disputed, the drug’s beneficial effects in CHF include reduced symptoms, improvement in New York Heart Association (NYHA) class, increased exercise time, modestly increased left ventricular ejection fraction (LVEF), increased cardiac output, and decreased CHF hospitalizations [6, 13, 36]. Furthermore, digoxin withdrawal has been found to be associated with an increased hospitalization rate and decreased LVEF [22, 37].
The Digitalis Investigation Group (DIG) trial tested the effect of digoxin versus placebo on survival in 7,788 patients with CHF and normal sinus rhythm [1]. In both treatment groups, the all-cause mortality was 35% and cardiovascular mortality 30%. There was a trend toward decreased mortality caused by CHF in the digoxin group, but this was offset by an increase in deaths from other causes that included deaths presumed to result from arrhythmias. Whereas the trial showed that digoxin reduced the risk of hospitalization because of worsening CHF [1], confirming the results of previous trials [22, 37], the drug did not appear to influence the quality of life [18].
Digoxin is also commonly used for the treatment of AF, although no trial has tested the effect of digoxin on mortality in this indication. The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study [41] showed that use of a rhythm-control strategy in the treatment of patients with AF offered no survival advantage over a rate-control strategy, but at the same time, it was found by chance in a later subgroup analysis that digoxin appeared to increase the death rate [relative risk (RR) = 1.42] [5]. It was suggested that this may have been attributable to prescription of digoxin for patients at greater risk of death, such as those with congestive heart failure, but this could not be proven. Thus, further studies are needed to test the effect of digoxin on mortality in patients with AF. In the present study, we investigated the 1-year mortality rate among patients admitted to coronary care units in Sweden with AF, CHF or AF+CHF during a 9-year period and those prescribed or not prescribed digoxin with the aim of testing the effect of long-term digoxin treatment on mortality in patients with AF compared with those with CHF. This study is the first to investigate the effect of digoxin on mortality in maintenance therapy of AF, despite the drug having been used in that indication for over a century.
Methods
This was a cohort study. Data for the study patients were obtained from the Registry of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS-HIA), for the period between January 1995 and December 2003. RIKS-HIA contains prospectively collected and detailed information on all patients admitted to most coronary care units at Swedish hospitals, as previously described [34]. We obtained 1-year mortality data by combining information from the RIKS-HIA database with that from the National Cause of Death Registry, which includes the vital status of all Swedish citizens. The register and the merging with registries were approved by an ethics committee and the National Board of Health and Welfare.
Inclusion/exclusion criteria
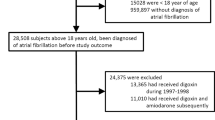
An overview of the inclusion of patients is given in Fig. 1. The study subjects consisted of three categories: (a) patients with AF, (b) patients with CHF, and (c) patients with AF+CHF. The AF group consisted of patients with an electrocardiogram (ECG) finding of AF on admission or at discharge, and patients with a discharge diagnosis of AF [International Center for Disease Control (ICD) 10 I48] without a concomitant diagnosis of CHF or pulmonary edema. The CHF group consisted of patients with a medical history of CHF, a diagnosis of CHF at discharge (ICD 10 H50.0, H50.1, or H50.9), or pulmonary edema on admission without concomitant AF. The AF+CHF group consisted of patients with an ECG finding of AF on admission or at discharge or patients with a discharge diagnosis of AF, with a concomitant medical history of CHF, a diagnosis of CHF at discharge, or pulmonary edema on admission. Patients who died during their hospital stay were excluded from the analyses. This was done because this was a study of the long-term effect of digoxin on mortality, so that patients who were the most likely to have died due to other reasons, i.e., due to cardiac disease per se quickly after being admitted to hospital, were excluded. Information on digoxin therapy was lacking in 20% of the cases but varied considerably between reporting hospitals. Therefore, only patients with a known digoxin therapy status derived from hospitals with missing data for <25% regarding digoxin therapy were included, giving a total number of 82,127 patients.
Statistical analyses
The AF, CHF, and AF+CHF groups were each divided into two subgroups according to digoxin therapy. The 1-year mortality rates following admission to the coronary care unit were determined for each category and compared between those who were prescribed digoxin and those who were not. A further division by sex was also made, as a sex-based difference in mortality among patients taking digoxin has been reported [25]. The average relative risk (RR) of death in patients discharged with digoxin compared with those without digoxin was estimated using Cox regression analysis. Separate estimates of RR were also calculated for men and women. Since this was not a randomized controlled clinical trial, we did not know each patient’s probability of receiving digoxin therapy as we would have done otherwise. To estimate these probabilities and account for baseline heart disease severity, we applied a propensity score method [27] using logistic regression analysis. Propensity scoring is a well-established method used in cohort studies such as this one and has been used extensively [4, 19, 20, 38]. Similar propensity score methods have also been applied in other studies of data from the RIKS-HIA database [32–35]. Simply put, propensity score is a measure of the likelihood that a patient would have been treated using their covariate scores and can be thought of as a balancing score [28]. By using the probability that a subject would have been treated (the propensity score) to adjust the estimate of the treatment effect, we created a quasiexperiment, mimicking a randomized trial. For instance, we find two subjects with the same propensity score, one treated, one a control. We can think of these two subjects as “randomly assigned” to each group, since they have the same probability of being in either group, given their covariates. Thus, propensity scores summarize all the information from the covariates in one single number, namely, the probability of being assigned to the treatment given the covariates and thereby offer advantages over more common methods of adjustments, especially if the adjustments involve a large number of covariates. Propensity scores can be used, along with variables that could not be balanced, as predictors in a regression model. Separate regressions can be fitted by propensity score quintile to estimate the treatment effect within quintile, as well as the overall treatment effect. The total number of patients available for complete case analyses in the adjusted model was 60,764 (AF = 21,459, CHF = 22,345, AF+CHF = 16,960). The variables included in the logistic regression analysis were: age, sex, smoking status, diabetes mellitus, hypertension, medications on admission [angiotensin-converting enzyme (ACE) inhibitors, diuretics, nitroglycerin, beta-blockers, acetylsalicylic acid/platelet inhibitors, lipid-lowering drugs, anticoagulant drugs], history of CHF, admission ECG (ST elevation, left bundle branch block), pacemaker, and continuous positive airway pressure (CPAP). Several two-way interactions were included after selection by a stepwise procedure using the Akaike information criteria (AIC) for inclusion/exclusion. All included variables and interactions are shown in Table 1. When analyzing possible sex-based differences, sex was excluded from the propensity score. The propensity score was then entered, together with digoxin and other discharge treatments (ACE inhibitors, diuretics, nitroglycerin, beta-blockers, acetylsalicylic acid/platelet inhibitors, lipid-lowering drugs, anticoagulant drugs) in the Cox regression analysis to adjust for differences between the digoxin and nondigoxin patients regarding the variables listed above. We thus compared patients with a similar probability of receiving digoxin to distinguish between the risk of having digoxin treatment and the risk of having the indication for which digoxin was given. For all statistical analyses R, version 2.2.1 (R foundation for Statistical Computing, Vienna, Austria) was used. As of 1999, registration of data on LVEF was voluntary, and serum (s-)creatinine was introduced as a compulsory variable at the end of 2002. These two variables, known to be associated with mortality [10, 23], were therefore not included in the propensity score. However, in patients for whom data on LVEF and s-creatinine were available, we tested whether they still affected mortality beyond the variables already included in the propensity score. This was done by comparing the RR of death between patients prescribed and those not prescribed digoxin among patients with LVEF < 30% and LVEF > 30% and among patients with s-creatinine values that were low [<85 μmol/l (female), <95 μmol/l (male)], normal [85–105 μmol/l (female), 95–115 μmol/l (male)], or elevated [>105 μmol/l (female), >115 μmol/l (male)]. Also, as it has been suggested that digoxin may be harmful in patients with acute myocardial infarction (AMI) [30], we further investigated whether or not patients who had suffered AMI, defined as a discharge diagnosis of AMI, still influenced the effect of digoxin on mortality after adjustment for propensity score and for discharge treatments. This was done by comparing the RR for death between those prescribed and those not prescribed digoxin among patients with and without AMI.
Results
Unadjusted patient characteristics distributed according to whether or not patients were discharged with digoxin are shown in Table 2. After applying the propensity score, the digoxin/no digoxin groups were well balanced with respect to the collected baseline risk factors (Table 3). The likelihood of being discharged with digoxin, irrespective of digoxin therapy at the time of admission, decreased significantly for each year: from 37% in 1995 to 20% in 2003. Patients with AF had an overall 1-year mortality of 9.8%, compared with 23.9% for CHF and 27.3% for AF+CHF.
Patients with AF
The estimated 1-year cumulative mortality in patients with AF discharged with and without digoxin is shown in Fig. 2. Patients who were discharged with digoxin did worse than those who did not receive the drug. After adjustment, RR for death was 1.42 [95% confidence interval (CI) 1.29–1.56]. There was no statistically significant sex-based difference [RR for death among women 1.34 (95% CI 1.17–1.53) and among men 1.51 (95% CI 1.33–1.71)].
One-year estimated cumulative mortality—atrial fibrillation. Estimated cumulative mortality in patients discharged with (dashed line) and without (solid line) digoxin. The left figure shows the crude cumulative mortality, and the right shows the cumulative mortality adjusted for propensity score and other discharge treatments. RR relative risk (95% confidence interval)
Patients with CHF
The estimated 1-year cumulative mortality in patients with CHF discharged with and without digoxin is shown in Fig. 3. Patients who received digoxin at the time of discharge did somewhat worse than those who did not receive the drug. After adjustment, RR for death was 1.11 (95% CI 1.04–1.19). There was no statistically significant sex-based difference [RR for death among women 1.04 (95% CI 0.94–1.16) and among men 1.17 (95% CI 1.07–1.28)].
One-year estimated cumulative mortality—congestive heart failure. Estimated cumulative mortality in patients discharged with (dashed line) and without (solid line) digoxin. The left figure shows the crude cumulative mortality, and the right shows the cumulative mortality adjusted for propensity score and other discharge treatments. RR relative risk (95% confidence interval)
Patients with AF+CHF
The estimated 1-year cumulative mortality in patients with AF+CHF discharged with and without digoxin is shown in Fig. 4. There was no difference between patients who were discharged with digoxin and those who did not receive the drug. after adjustment, RR for death was 1.00 (95% CI 0.94–1.06). No significant sex-based difference was observed [RR for death among women 1.04 (95% CI 0.95–1.14) and among men 0.98 (95% CI 0.91–1.06)].
One-year estimated cumulative mortality—atrial fibrillation + congestive heart failure. Estimated cumulative mortality in patients discharged with (dashed line) and without (solid line) digoxin. The left figure shows the crude cumulative mortality, and the right shows the cumulative mortality adjusted for propensity score and other discharge treatments. RR relative risk (95% confidence interval)
Effects of LVEF and s-creatinine
After adjustment for propensity score and discharge treatments, neither LVEF nor s-creatinine significantly affected the RR for death between patients discharged with and without digoxin. In patients with LVEF ≤ 30% (449 received digoxin, 1,166 did not receive digoxin) and in those with LVEF > 30% (1,292 received digoxin, 5,195 did not receive digoxin), the RRs for death were 1.06 (95% CI 0.86–1.31) and 1.14 (95% CI 0.98–1.32), respectively, after adjustment. In patients with low s-creatinine (422 received digoxin, 1,635 did not receive digoxin), normal s-creatinine (469 received digoxin, 1,672 did not receive digoxin) and high s-creatinine (602 received digoxin, 2,233 did not receive digoxin), the RRs for death were 1.23 (95% CI 0.91–1.66), 1.22 (95% CI 0.94–1.58), and 0.98 (95% CI 0.83–1.16), respectively, after adjustment.
Effect of acute myocardial infarction
In patients with and without AMI, the RRs for death were 1.17 (95% CI 1.10–1.24) (4,743 received digoxin, 15,453 did not receive digoxin), and 1.10 (95% CI 1.04–1.16) (11,654 received digoxin, 28,817 did not receive digoxin), respectively, after adjustment.
Stratification by propensity score quintiles
The RR for death according to whether or not patients received digoxin stratified by propensity score quintile is shown in Table 4. There was a significant interaction between propensity score quintile and digoxin treatment in the AF and CHF groups so that lower quintiles were associated with higher RRs for death.
Discussion
This study showed that 23% of all patients in coronary care units in Sweden with AF without CHF were discharged with digoxin. At the same time, the adjusted overall RR for death was found to be 1.42 (95% CI 1.29–1.56) in these patients compared with those who did not receive the drug. On the other hand, digoxin therapy did not alter the overall mortality in patients with CHF, a finding in agreement with the results of the DIG trial [1]. Although there was a statistically significant difference in patients with CHF without AF, it was small and of doubtful relevance, albeit stratification by propensity score quintile suggests that digoxin could have a detrimental effect in those with the lowest baseline cardiac risk. The observed increase in mortality among patients with AF in this study was thus identical to that seen in the AFFIRM trial (RR = 1.42) [5]. In that study, digoxin was found en passant to be the sole rate-control drug that was significantly related to survival: it increased the death rate. It was suggested that rather than reflecting a deleterious effect of digoxin on survival, the result might have been explainable by prescription of digoxin for patients at greater risk of death, such as those with CHF [5]. The results of our study indicate, however, that the latter theory is unlikely and instead suggest that digoxin is an independent risk factor for death among patients with AF without CHF on long-term therapy with this drug.
Why does the effect of digoxin on mortality differ between the groups? We cannot give a definite answer to that question, but a possible explanation may be that the combination of a positive inotropic and negative chronotropic effect of digoxin is beneficial, or at least not harmful, in patients with CHF, whereas it may be of more harm than benefit in those without CHF. Possible other effects may include baroreceptor function [39] and neuroendocrine activation [9]. For instance, the DIG trial showed that the digoxin effect of decreasing the hospitalization rate in CHF patients was more pronounced in patients with more severe CHF [1]. Furthermore, in that trial, no difference in total mortality was found between the digoxin-assigned and placebo-assigned groups, suggesting that the lower mortality from CHF deaths in the digoxin group could have been counterbalanced by an increase in deaths not due to CHF. Deaths from “other causes,” presumed to be due to arrhythmias, were significantly higher in the digoxin (15%) than in the placebo group (13%) [29]. This leaves us with the question of whether patients without CHF, who thus would not benefit from the lower mortality from CHF, would only be exposed to a negative influence of digoxin on mortality. In this respect, the observed close correlation between a decreased LVEF and a decreased Na+, K+-ATPase concentration is interesting [21], suggesting that reduction of Na+, K+-ATPase in patients with CHF might serve compensatory purposes, with effects comparable to those of digoxin treatment. Although not the primary aim of the present study, it is interesting to note that the RRs for death in patients with AF and to some extent in patients with CHF was higher in the lowest propensity score quintiles, i.e., in those with the lowest baseline cardiac risk.
Although still widely used in clinical practice, perhaps on account of the theoretical advantage of its positive inotropic effect and its modifying effect on the ventricular rate and its obvious and beneficial short-term effects in the emergency setting, there is no evidence to suggest that digoxin has any effect on cardioversion in AF either in the presence or absence of CHF [2, 7, 12, 15] or any effect in suppressing recurrent AF [8]. During exercise and in patients with increased sympathetic activity, digoxin alone does not control the ventricular response unless large doses that are likely to produce intoxication are used [11, 17, 26]. Digoxin is generally not recommended as first-line therapy for management of AF, except in patients with concomitant CHF or left ventricular dysfunction [8]. In persistent AF, there are more effective alternatives, such as calcium channel blocking agents and beta-blockers [8], although digoxin is usually considered potentially useful as add-on therapy [16]. The present study did not address the effect of digoxin on mortality in the emergency setting, but the results cast doubts on the use of this drug for long-term treatment of AF in the absence of CHF.
A cohort study cannot be compared with a prospective randomized trial but it deserves to be pointed out that the strength of the present study includes the fact that it reflects the normal patient clientele, in that our patient cohort comprised unselected, consecutive patients, although strict generalizability is limited to patients discharged from coronary care units. There were no exclusions due to presence or absence of specific risk factors or co-morbidities. The representativeness of the cohort was also strengthened by the fact that the patients were recruited from the general population at centres with different levels of care, including 73 of the 76 coronary care units within the whole of Sweden.
Limitations
Several limitations to this study need to be considered. First, the RIKS-HIA database does not include serum digoxin concentrations or digoxin doses. It may be argued that the higher observed mortality among patients with AF discharged with digoxin compared with those with CHF discharged with this drug could be due to a comparably higher dose in the former group. Subgroup analyses of the DIG trial have recently shown a relation between serum digoxin level and mortality [3, 24]. In men, the risk of death increased significantly with digoxin levels >1 ng/ml, whereas a digoxin level of 0.5 to 0.8 ng/ml was associated with a decrease in mortality [24]. Corresponding values in women were =1.2 ng/ml and 0.5 to 0.9 ng/ml, respectively [3]. Although we did not have information on the doses of digoxin given to the patients in our study, the findings in patients with concomitant AF and CHF, who were probably given a dose similar to that in patients with AF alone, argues against the possibility of a dose-related difference in mortality.
Second, although our results are based on a large cohort and have been adjusted for many confounding factors, a cohort study cannot compensate for all confounders and hence cannot replace a randomized controlled trial. Propensity analyses are inherently limited by the number and accuracy of the variables evaluated. Nevertheless, propensity scoring is a well-established tool that enables excellent matching of baseline characteristics [14], and moreover, there are limitations to randomized controlled trials also; for example, strict inclusion and exclusion criteria may limit the applicability of the study results to other, perhaps more typical, patient populations.
Third, for the majority of our patients the RIKS-HIA database did not include data on renal function or LVEF, two important determinants of mortality [10, 23]. However, among those patients for whom these variables were available, they did not affect the adjusted mortality estimates, indicating that our propensity score was satisfactory.
Fourth, we had no information about whether or not individual patients continued on digoxin therapy, or any other drug therapy, including combination therapy. It could be argued that patients who received digoxin at discharge were later switched to beta-blocker therapy. However, if this was the case, it would bias the results toward the null and cannot explain the findings in the AF group.
Fifth, data on antiarrhythmic therapy was not included in the analysis, as this variable was excluded from the RIKS-HIA database in 2004. At that time,antiarrhythmic therapy had been included as a general term, and an overall of 5% of the population had been on such treatment. With this low usage, other antiarrhythmic therapy, even if it differed extremely after adjustment between those who received digoxin and those who did not, is unlikely to explain the results.
Conclusion
Digoxin is widely used for treatment of AF and CHF, for short-term as well as long-term use. Among individuals aged 75 years and older, almost 20% were on medication with digoxin in 1996 [40]. Despite the declining use in the last few years, digoxin is still one of the most frequently prescribed drugs. It was listed twice among the top 200 prescriptions in 2000 [31]. This was also noted in our study. Our results indicate, however, that Swedish citizens admitted to coronary care units for AF without CHF and who are discharged with digoxin have an increased mortality compared with those not given the drug.
Ideally, these findings should be confirmed in prospective randomized controlled trials, but as such trials have no commercial interest, they are unlikely ever to be performed. In conclusion, the results of the present study indicate that digoxin is an independent risk factor for death among AF patients admitted to coronary care units and placed on long-term therapy with this drug, whereas there seems to be no excess risk in those with CHF.
References
Garg R, Gorlin R, Smith T, Yusuf S, on behalf of the Digitalis Investigation Group (1997) The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 336(8):525–533
Hornestam B, on behalf of the Digitalis in Acute Atrial Fibrillation (DAAF) Trial Group (1997) Intravenous digoxin in acute atrial fibrillation. Results of a randomized, placebo-controlled multicentre trial in 239 patients. Eur Heart J 18(4):649–654
Adams KF Jr, Patterson JH, Gattis WA, O’Connor CM, Lee CR, Schwartz TA, Gheorghiade M (2005) Relationship of serum digoxin concentration to mortality and morbidity in women in the digitalis investigation group trial: a retrospective analysis. J Am Coll Cardiol 46(3):497–504
Brener SJ, Lytle BW, Casserly IP, Schneider JP, Topol EJ, Lauer MS (2004) Propensity analysis of long-term survival after surgical or percutaneous revascularization in patients with multivessel coronary artery disease and high-risk features. Circulation 109(19):2290–2295
Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, Josephson RA, Kellen JC, Klein RC, Krahn AD, Mickel M, Mitchell LB, Nelson JD, Rosenberg Y, Schron E, Shemanski L, Waldo AL, Wyse DG (2004) Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Study. Circulation 109(12):1509–1513
Eichhorn EJ, Gheorghiade M (2002) Digoxin. Prog Cardiovasc Dis 44(4):251–266
Falk RH, Knowlton AA, Bernard SA, Gotlieb NE, Battinelli NJ (1987) Digoxin for converting recent-onset atrial fibrillation to sinus rhythm. A randomized, double-blinded trial. Ann Intern Med 106(4):503–506
Fuster V, Ryden LE, Asinger RW, Cannom DS, Crijns HJ, Frye RL, Halperin JL, Kay GN, Klein WW, Levy S, McNamara RL, Prystowsky EN, Wann LS, Wyse DG (2001) ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to develop guidelines for the management of patients with atrial fibrillation) developed in collaboration with the North American Society of Pacing and Electrophysiology. Eur Heart J 22(20):1852–1923
Gheorghiade M, Ferguson D (1991) Digoxin. A neurohormonal modulator in heart failure? Circulation 84(5):2181–2186
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351(13):1296–1305
Gold H, Cattell M, Greiner T (1953) Clinical pharmacology of digoxin. J Pharmacol Exp Ther (109):45–47
Hou ZY, Chang MS, Chen CY, Tu MS, Lin SL, Chiang HT, Woosley RL (1995) Acute treatment of recent-onset atrial fibrillation and flutter with a tailored dosing regimen of intravenous amiodarone. A randomized, digoxin-controlled study. Eur Heart J 16(4):521–528
Jaeschke R, Oxman AD, Guyatt GH (1990) To what extent do congestive heart failure patients in sinus rhythm benefit from digoxin therapy? A systematic overview and meta-analysis. Am J Med 88(3):279–286
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150(4):327–333
Jordaens L, Trouerbach J, Calle P, Tavernier R, Derycke E, Vertongen P, Bergez B, Vandekerckhove Y (1997) Conversion of atrial fibrillation to sinus rhythm and rate control by digoxin in comparison to placebo. Eur Heart J 18(4):643–648
Khairy P, Nattel S (2002) New insights into the mechanisms and management of atrial fibrillation. Cmaj 167(9):1012–1020
Koh KK, Kwon KS, Park HB, Baik SH, Park SJ, Lee KH, Kim EJ, Kim SH, Cho SK, Kim SS (1995) Efficacy and safety of digoxin alone and in combination with low-dose diltiazem or betaxolol to control ventricular rate in chronic atrial fibrillation. Am J Cardiol 75(1):88–90
Lader E, Egan D, Hunsberger S, Garg R, Czajkowski S, McSherry F (2003) The effect of digoxin on the quality of life in patients with heart failure. J Card Fail 9(1):4–12
Lindenauer PK, Pekow P, Wang K, Gutierrez B, Benjamin EM (2004) Lipid-lowering therapy and in-hospital mortality following major noncardiac surgery. JAMA 291(17):2092–2099
Macaubas C, de Klerk NH, Holt BJ, Wee C, Kendall G, Firth M, Sly PD, Holt PG (2003) Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet 362(9391):1192–1197
Norgaard A, Bagger JP, Bjerregaard P, Baandrup U, Kjeldsen K, Thomsen PE (1988) Relation of left ventricular function and Na,K-pump concentration in suspected idiopathic dilated cardiomyopathy. Am J Cardiol 61(15):1312–1315
Packer M, Gheorghiade M, Young JB, Costantini PJ, Adams KF, Cody RJ, Smith LK, Van Voorhees L, Gourley LA, Jolly MK (1993) Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. RADIANCE Study. N Engl J Med 329(1):1–7
Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS, Granger CB (2006) Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J 27(1):65–75
Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM (2003) Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA 289(7):871–878
Rathore SS, Wang Y, Krumholz HM (2002) Sex-based differences in the effect of digoxin for the treatment of heart failure. N Engl J Med 347(18):1403–1411
Redfors A (1971) The effect of different digoxin doses on subjective symptoms and physical working capacity in patients with atrial fibrillation. Acta Med Scand 190(4):307–320
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika (70):41–55
Rubin DB (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127(8 Pt 2):757–763
Ruelaz RA, Rahimtoola SH (2005) Was it digoxin toxicity?...very likely. J Card Fail 11(2):87–90
Spargias KS, Hall AS, Ball SG (1999) Safety concerns about digoxin after acute myocardial infarction. Lancet 354(9176):391–392
Steimer W, Muller C, Eber B (2002) Digoxin assays: frequent, substantial, and potentially dangerous interference by spironolactone, canrenone, and other steroids. Clin Chem 48(3):507–516
Stenestrand U, Tabrizi F, Lindback J, Englund A, Rosenqvist M, Wallentin L (2004) Comorbidity and myocardial dysfunction are the main explanations for the higher 1-year mortality in acute myocardial infarction with left bundle-branch block. Circulation 110(14):1896–1902
Stenestrand U, Wallentin L (2002) Early revascularisation and 1-year survival in 14-day survivors of acute myocardial infarction: a prospective cohort study. Lancet 359(9320):1805–1811
Stenestrand U, Wallentin L (2001) Early statin treatment following acute myocardial infarction and 1-year survival. JAMA 285(4):430–436
Stenestrand U, Wallentin L (2003) Fibrinolytic therapy in patients 75 years and older with ST-segment-elevation myocardial infarction: one-year follow-up of a large prospective cohort. Arch Intern Med 163(8):965–971
Tauke J, Goldstein S, Gheorghiade M (1994) Digoxin for chronic heart failure: a review of the randomized controlled trials with special attention to the PROVED (Prospective Randomized Study of Ventricular Failure and the Efficacy of Digoxin) and RADIANCE (Randomized Assessment of Digoxin on Inhibitors of the angiotensin Converting Enzyme) trials. Prog Cardiovasc Dis 37(1):49–58
Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK (1993) Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. PROVED Investigative Group. J Am Coll Cardiol 22(4):955–962
Wang PS, Schneeweiss S, Avorn J, Fischer MA, Mogun H, Solomon DH, Brookhart MA (2005) Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med 353(22):2335–2341
Vardas PE, Kanoupakis EM, Kochiadakis GE, Simantirakis EN, Marketou ME, Chlouverakis GI (1998) Effects of long-term digoxin therapy on heart rate variability, baroreceptor sensitivity, and exercise capacity in patients with heart failure. Cardiovasc Drugs Ther 12(1):47–55
Wills P, Fastbom J, Claesson CB, Cornelius C, Thorslund M, Winblad B (1996) Use of cardiovascular drugs in an older Swedish population. J Am Geriatr Soc 44(1):54–60
Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, Kellen JC, Greene HL, Mickel MC, Dalquist JE, Corley SD (2002) A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 347(23):1825–1833
Acknowledgements
We thank the Swedish Heart Lung Foundation for funding this study (grant #20040494). We also thank Karl Michaelsson, MD, PhD, at Uppsala University Hospital, for valuable feedback concerning the statistical analyses.
Conflict of Interest Statement
This study was funded partly by the Swedish Heart-Lung Foundation, but the foundation had no active role in the study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Hallberg, P., Lindbäck, J., Lindahl, B. et al. Digoxin and mortality in atrial fibrillation: a prospective cohort study. Eur J Clin Pharmacol 63, 959–971 (2007). https://doi.org/10.1007/s00228-007-0346-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0346-9