Abstract
Anger and other negative emotions can precipitate sudden death, as shown in studies of population stressors. Clinical studies of patients with implantable defibrillators demonstrate that anger can trigger ventricular arrhythmias. Long-term negative emotions also increase vulnerability to arrhythmias. Mechanisms linking anger and arrhythmias include autonomic changes, which alter repolarization, possibly enhanced in patients with sympathetic denervation, which in turn trigger potentially lethal polymorphic ventricular tachycardias. Interventions which decrease negative emotions and resultant autonomic responses may be therapeutic in patients with implantable cardioverter defibrillators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An understanding of the role of stress and emotion in the genesis of arrhythmias and sudden cardiac death may point the way toward novel strategies for prevention. Evidence from population, clinical, and mechanistic studies continues to accumulate that anger, stress, and other negative emotions can precipitate ventricular arrhythmias and sudden death.
Acute Triggering of Ventricular Arrhythmia by Emotion
In 2003, the NY Times reported the sad story of “A 57-year-old Harlem woman preparing to leave for her longtime city government job died of a heart attack yesterday morning after police officers broke down her door and threw a concussion grenade into her apartment, the police commissioner said. They were acting on what appeared to be bad information about guns and drugs in the apartment… Ms. Spruill initially declined medical attention, although she told the captain that she had a heart condition. An ambulance was requested, and she went into cardiac arrest on the way to Harlem Hospital Center, where she died at 7:50 a.m” [1]. As described by Engel in 1971, anecdotal accounts of people dying suddenly in the throes of extreme emotion go back to the Bible [2].
Triggering of Sudden Cardiac Death
Epidemiological studies of population stressors such as earthquake and war have confirmed the ability of acute psychological stress to trigger sudden death. Some of the earliest data addressing the impact of stress came from the Northridge earthquake in 1994, with six times the incidence of sudden cardiac deaths on the day of the quake compared to days prior to and following. The vast majority of these (21/24) were unrelated to physical exertion, implying it was the psychological impact of the disaster which led to the increase in mortality [3•]. More recently, the Great East Japan earthquake and tsunami of 2011 resulted in an increase in out-of-hospital cardiac arrest not just in the areas most affected [4] but also in areas without direct damage [5], confirming the impact of psychological stress. War similarly increases mortality beyond the direct effects [6]. Less life-altering disasters can also trigger sudden death. For example, in an analysis of daily death and stock performance data from Shanghai’s Center for Disease Control and Prevention and Stock Exchange respectively, daily coronary death rates fluctuated with daily stock changes [7]. Even World Cup soccer matches have been associated with increased sudden death incidence in population studies [8].
Triggering of Ventricular Arrhythmia
Sudden death can be due to either acute ischemia or primary arrhythmia, and to what extent these stress-induced deaths were due to ischemia, for which the impact of stress has been long-described, cannot be determined. However, studies of patients with implantable cardioverter-defibrillators (ICDs), which convert potentially lethal arrhythmias back to sinus rhythm by delivering either a shock or anti-tachycardia pacing, while saving data about the event, have demonstrated similar impacts of stress on ventricular arrhythmias not associated with ischemia. In one case report, ICD interrogation in a patient receiving the device for primary prevention revealed a first and only episode of ventricular tachycardia (VT), converted with anti-tachycardia pacing, of which the patient was unaware, which had occurred while her sister-in-law’s casket was being lowered into the ground [9]. Population stressors also lead to increases in ICD-treated ventricular arrhythmias. For example, the World Trade Center attacks on 9/11/2001 were associated with twofold increase in ventricular arrhythmias in 30 days following the attacks, not just in New York City [10] but in Florida as well [11]. Similar increases in tachyarrhythmias in ICD patients were described after the Great East Japan earthquake [12]. And, similar to sudden death [8] and myocardial infarction [13], World Cup soccer increases ICD-treated ventricular arrhythmias [14].
Prospective studies of triggering factors in patients with ICDs have provided further evidence of emotional triggering of arrhythmia [15]. We [16•] asked ICD patients to record in a diary their activities and emotions in 15 min and 2 h prior to any ICD shocks they received over the course of a year’s follow-up. Subjects ranked their levels of anger and other emotions on a 5-point Likert scale and reported what they were doing. They then filled out a similar diary 1 week later at the same time of day. One hundred seven shocks were reported by 42 patients. Higher levels of anger, dichotomized at level 3 or above, were more common pre-shock, occurring 15 % of the time, but were reported in just 3 % of diaries during control periods. Anger was significantly associated with the 15 min preceding shock [16•]. Anger-triggered arrhythmias, defined as those preceded by an anger level of 3 or above, were more likely to be polymorphic, PVC-initiated, and pause-dependent, than those not preceded by anger [17]. Anger is known to increase PVC burden in animals [18] and humans [19], and it is likely that anger triggered the PVCs which then triggered polymorphic VT. As these characteristics are associated with more malignant arrhythmias, this suggests that anger not only increases the frequency but also the lethality of ventricular arrhythmia. In the multicenter TOVA trial, or “Triggers of Ventricular Arrhythmia,” currently under analysis, anger was similarly associated with an increase in ventricular arrhythmias [20].
Studies in the electrophysiology laboratory have further demonstrated the role of negative emotion in facilitating arrhythmia induction. In one of the first studies to evaluate the role of stress in arrhythmia, in 1973 [21], Lown investigated the inducibility of arrhythmia using programmed stimulation in a dog model in which stress was created by lifting the animal in a sling conditioned to be a noxious stimulus. In rested animals, only 1 premature ventricular contraction (PVC) could be induced and required a high output of 35 mA. In the sling, 2 PVCs were induced, using just 5 mA. In a similar study in humans, we later evaluated the effects of mental stress on induced arrhythmias in patients with a history of known ventricular arrhythmias and ICDs [15, 22]. All patients had had VT which was terminated with anti-tachycardia pacing at previous EP studies. Many patients had VT induced earlier in the protocol, using fewer extra-stimuli. Arrhythmias induced during mental stress were faster than those induced at rest and were harder to terminate. In some cases, an identical VT which had been pacer-terminated in the baseline state required shock for termination during anger-recall, suggesting that autonomic changes due to the anger had altered properties of conduction and refractoriness of the VT circuit, eliminating the excitable gap.
Happiness and Triggering
Whether happiness promotes or protects against triggering of acute cardiovascular events is less clear. As described by Engel, anecdotally happiness has been described to trigger cardiac events, and the study of death and stock changes showed a U-shaped curve, with increases in the stock market also associated with increases in death rates [7]. Anecdotally, one of this author’s first catheterizations as a fellow was for a patient suffering a myocardial infarction shortly after winning the Connecticut lottery. However, in one study of patients with the Long QT syndrome, happiness was associated with a decreased incidence of arrhythmic events [23], and we have found happiness to be protective against episodes of atrial fibrillation [24]. Overall, happiness decreases risk of cardiovascular disease [25] and mortality, independently of negative affect [26]. Many although not all ambulatory studies of positive affect show physiological changes of decreased heart rate and blood pressure, providing mechanistic data to support the clinical benefits seen [27•]. As described by Dockray and Steptoe, “positive affect” is not a single construct but includes components of activation (e.g., ecstasy) versus deactivation (e.g., serenity) and failure to take these components into account may explain the variability in findings overall [27•].
Long-Term Factors and Arrhythmia Vulnerability
Long-term negative emotion due to chronic psychopathological illness can also increase vulnerability to arrhythmia in patients with ICDs. Studies have shown individuals with higher levels of depression [28] or anxiety [29] at baseline are more likely to experience ventricular arrhythmias treated by the ICD in long-term follow-up, even after controlling for clinical variables. Those individuals characterized by both anxiety and the “Type D” personality—the tendency to experience emotional and social distress in combination with emotional non-expression—are particularly vulnerable to future arrhythmia [30]. In our diary study, individuals with psychological profile characterized by anger or anxiety were more likely to experience triggering of arrhythmias by these emotions [31].
Understanding the Pathophysiological Links Between Emotion and Arrhythmia
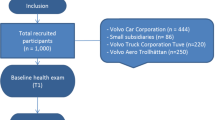
These clinical and epidemiological data linking negative emotion with arrhythmia, in the absence of ischemia, suggest that the autonomic changes associated with emotion can directly alter electrophysiological properties of ventricular myocardium resulting ventricular arrhythmia. Understanding the pathway from negative emotion to lethal ventricular arrhythmia is the subject of ongoing research by us and others. As depicted in Fig. 1 and described in detail below, we hypothesize a pathway in which negative emotion leads to autonomic changes, which increases heterogeneity of repolarization particularly in patients with vulnerability due to heterogenous cardiac denervation due to myocardial infarction or more diffuse cardiomyopathic processes. These changes in repolarization lead to polymorphic ventricular arrhythmia, resulting in sudden death or in appropriate shock in those whose arrhythmic risk has already been mitigated through ICD placement.
Emotion Influences Autonomic Activity
The impact of emotion on autonomic activity, the first step in this cascade, has been long described [15]. Negative emotion increases catecholamine levels [31] and decreases vagal output [32]. Chronic stressors such as depression alter long-term autonomic balance [33]. In animal studies, these autonomic changes—sympathetic activation and vagal withdrawal—increase vulnerability to, or even directly induce, ventricular arrhythmias. In animal models of infarction, direct sympathetic stimulation of the ventricles via stellate ganglion stimulation induces fibrillation [34], demonstrated as early as 1964 by Han et al., and higher levels of vagal activity are protective against ischemic arrhythmias [35].
Autonomic Activity Influences Repolarization
As we and others have demonstrated, these autonomic changes then influence cardiac repolarization. In order to investigate how acute increases in sympathetic activity might influence repolarization, Toivonen [36] asked medical residents to wear Holters while on-call and recorded the times of pages which awakened them from sleep. During periods of stress, when the residents had been awakened from sleep and were returning pages, the QT interval was relatively longer for a given HR, than during the same HR in the absence of stress.
We used a laboratory mental stress protocol (anger recall and mental arithmetic) to evaluate effects of mental stress on three surface measures of heterogeneity of repolarization, well-known to be an important factor in arrhythmogenesis: T-wave alternans (TWA), T-wave amplitude, and area, using time-domain methodology. In this study, 33 patients with ICDs and a history of ventricular arrhythmias underwent a mental stress protocol including mental arithmetic and anger recall. TWA increased from 22 at baseline to 29 uV during mental stress (p < 0.001). All other measures of heterogeneity also increased with stress. In a similar study by Kop et al., mental-stress was also seen to increase TWA. This group performed simultaneous SPECT-perfusion imaging, and so were able to confirm that the effect of anger on TWA was independent of ischemia [37•]. In our study, the increase in TWA correlated with increases in catecholamines, but there was minimal increase in heart rate with mental stress, suggesting a direct autonomic effect on TWA. Prior studies have also suggested that sympathetic activation may increase TWA beyond the effects of heart rate. In experimental studies, stimulation of the stellate ganglion increases TWA, while stellectomy decreases it [38]. In clinical studies, TWA induced with exercise is greater than that with atrial pacing at the same heart rate [39], implying an effect of sympathetic activity beyond that of increasing heart rate. Further, intravenous beta-blockade [40] decreases the magnitude of TWA.
In order to look in a physiologically detailed fashion at the impact of stress on repolarization, Taggart et al. asked patients undergoing invasive electrophysiology studies (for SVTs) to watch a stressful movie (“Vertical Limit”) after positioning of recording catheters in the heart and measured activation recovery intervals, a surrogate for action potential duration prior to, and then during, the movie. Activation recovery intervals decreased during stress, with regional difference between right and left ventricles [41]. Further study by this group found that these electrophysiological changes with stress were exaggerated at short coupling intervals and thus particularly relevant to arrhythmia initiation by premature beats [42]. The subjects in these studies had normal ventricles, and the changes seen were not associated with induction of arrhythmia. However, in patients with structurally and thus electrically abnormal hearts, it is highly likely that this decrease in repolarization time would be non-uniform, perhaps increasing baseline heterogeneity as suggested by the TWA studies.
Potential Role of Heterogeneous Sympathetic Denervation
We hypothesize that heterogeneity of sympathetic denervation, such as occurs after myocardial infarction or in other cardiomyopathies, may enhance vulnerability to sympathetically driven increases in repolarization heterogeneity. Clinical studies show that sympathetic denervation as measured by I-123 meta-iodobenzylguanidine (MIBG) imaging is a marker for vulnerability to ventricular arrhythmias [43]. Beta receptor activation alters transmembrane currents which alter repolarization [44]. Experimental studies demonstrate that areas of denervated myocardium develop arrhythmias when exposed to catecholamines [45], such as those that increase with mental stress. In a pilot study, we performed MIBG imaging in 5 patients with decreased ejection fraction and history of myocardial infarction at rest and, on a separate day, during a mental stress protocol, finding a decrease in heart-to-mediastinal ratio, as well as changes in heterogeneity of catecholamine uptake, during stress, a finding not seen in normal controls [46]. Whether and how denervation plays a role linking emotion and arrhythmia is an important avenue of future research.
Prognostic Importance of Stress-Induced Changes
The effect of anger on TWA in the laboratory was predictive of arrhythmias in real life. In a follow-up of our study of anger and TWA [47], we found that anger-induced TWA was a significant predictor of arrhythmia, with likelihood of ICD-treated ventricular arrhythmia for those in the top quartile of anger-induced in the lab of over 10 times that of other patients (CI 1.6–113, p < 0.05.) Anger-induced TWA remained predictive after controlling for standard predictors of arrhythmia such as ejection fraction, prior clinical arrhythmia, and wide QRS. Prior studies of the predictive value of TWA have shown mixed results, and a recent consensus study concludes that “there is as yet no definitive evidence that it can guide therapy” [48]. Our study was limited by size, inclusion of mainly men, and using treated arrhythmias as an outcome in an era prior to current evidence-based programming [49]. However, the high predictive value seen here raises an intriguing possibility—laboratory mental stress-invoked TWA may be an better probe of arrhythmia-risk, as this modality measures the interaction of trigger and substrate which may lead to arrhythmogenesis (rather than substrate alone) [15].
Implications for Novel Therapies
Multiple studies have investigated whether educational and psychological interventions utilizing a variety of psychoeducational methods—groups, phone interventions, cognitive behavioral therapy—can improve outcomes for ICD patients, with the first 15 of these reviewed in a 2012 American Heart Association Scientific Statement [50]. While limited in size, and inclusion of predominantly patients receiving the ICD for secondary prevention, most have found improvements in psychosocial outcomes such as anxiety and depression. Those found most effective included components that enhance information and also teach life skills for living with the device as well as general stress-management techniques. While not specifically geared toward anger prevention, stress management may enhance anger-management skills. Other modalities in addition to traditional CBT, such as complementary approaches, have also shown potential benefit. Toise et al. randomized ICD patients to yoga classes, versus usual care, and found that yoga improved anxiety and patient acceptance of the ICD [51]. In a small pilot study, Freedenburg compared anxiety and depression in adolescents with ICDs before and after a mindfulness-based stress reduction (MBSR) program, finding significant improvements [52]. Based on the overall benefits of positive affect, the ongoing “Positive psychotherapy to improve autonomic function and mood in ICD Patients (PAM-ICD)” will randomize patients to quality of life therapy (QOLT), another novel intervention, versus education alone [53].
Interestingly, preliminary findings from several small studies suggest that interventions aimed at psychological health and stress management may decrease arrhythmia frequency, in addition to improving quality of life. For example, Chevalier [54] randomized 70 patients after ICD implant to receive small-group cognitive behavioral therapy for 3 months. In the treatment group, anxiety was lower at 3 and 12 months in the treatment group, but increased in the untreated. Physiologic measures suggested an improvement in sympathovagal balance with the psychotherapy, with heart rate variability higher, and heart rate lower. Ventricular arrhythmias treated with the ICD were less frequent in the group receiving the intervention at 3 and 12 months, although the 12-month comparison did not reach significance, likely due to the small numbers enrolled. Also, while not powered to see changes in arrhythmia frequency, the yoga study above found a non-significant reduction in ventricular arrhythmias [51].
Our group has recently completed follow-up in the RISTA trial—Reducing Vulnerability to Implantable Cardioverter Defibrillator Shock-Treated Ventricular Arrhythmias [15, 55]—which randomized 300 ICD patients to an 8-week stress reduction program or usual care, to determine if reducing negative emotion can reduce arrhythmia frequency, and data analysis will begin shortly. This study is also evaluating whether stress reduction can attenuate the increases in TWA with laboratory stress which we have previously described (data analysis underway). Further research is needed to determine most effective stress-reducing modalities, whether complementary modalities such as yoga, or traditional modalities such as cognitive behavioral therapy, for reducing arrhythmia-frequency in patients with ICDs.
Conclusions
Anger and other negative emotions can precipitate sudden death, as shown in studies of population stressors. Clinical studies of patients with implantable defibrillators demonstrate that anger can trigger ventricular arrhythmias. Long-term negative emotions also increase vulnerability to arrhythmias. Mechanisms linking anger and arrhythmias include autonomic changes, which alter repolarization, possibly enhanced in patients with sympathetic denervation, which in turn trigger potentially lethal polymorphic ventricular tachycardias. Interventions which decrease negative emotions and resultant autonomic responses may be therapeutic in patients with implantable cardioverter defibrillators.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Rashbaum W, New York Times. Woman dies after police mistakenly raid her apartment. 2003.
Engel GL. Sudden and rapid death during psychological stress. Annal Int Med. 1971;74:771–82.
Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334:413–9. This study is among the first and most rigorous to demonstrate an association between a population stressor and sudden cardiac death.
Kitamura T, Kiyohara K, Iwami T. The great east Japan earthquake and out-of-hospital cardiac arrest. N Engl J Med. 2013;369:2165–7.
Kiyohara K, Kitamura T, Iwami T, Nishiyama C, Kawamura T. Impact of the Great East Japan earthquake on out-of-hospital cardiac arrest with cardiac origin in non-disaster areas [corrected]. J Epidemiol Community Health (1979). 2015;69:185–8.
Meisel SR, Kutz I, Dayan KI, et al. Effect of Iraqi missile war on incidence of acute myocardial infarction and sudden death in Israeli civilians. Lancet. 1991;338:660–1.
Ma W, Chen H, Jiang L, Song G, Kan H. Stock volatility as a risk factor for coronary heart disease death. Eur Heart J. 2011;32:1006–11.
Katz E, Metzger J-T, Marazzi A, Kappenberger L. Increase of sudden cardiac deaths in Switzerland during the 2002 FIFA World Cup. Int J Cardiol. 2006;107:132–3.
Sweeney MO, Quill TE. Clustering of sudden death and aborted cardiac arrest associated with a family grief reaction. Heart Rhythm. 2007;4:952–55.
Steinberg JS, Arshad A, Kowalski M, et al. Increased incidence of life-threatening ventricular arrhythmias in implantable defibrillator patients after the World Trade Center attack. J Am Coll Cardiol. 2004;44:1261–4.
Shedd OL, Sears SF, Harvill JL, et al. The World Trade Center attack: increased frequency of defibrillator shocks for ventricular arrhythmias in patients living remotely from New York City. J Am Coll Cardiol. 2004;44:1265–7.
Nakano M, Kondo M, Wakayama Y, et al. Increased incidence of tachyarrhythmias and heart failure hospitalization in patients with implanted cardiac devices after the Great East Japan earthquake disaster. Circ J. 2012;76:1283–5.
Wilbert-Lampen U, Leistner D, Greven S, et al. Cardiovascular events during World Cup soccer. [see comment]. N Engl J Med. 2008;358:475–83.
Kondo Y, Linhart M, Schwab JO, Andrie RP. Incidence of ventricular arrhythmias during World Cup football 2014 in patients with implantable cardioverter defibrillator. Int J Cardiol. 2015;187:307–8.
Lampert R. Behavioral influences on cardiac arrhythmias. Trends Cardiovasc Med. 2016;26:68–77.
Lampert R, Joska T, Burg M, Batsford W, McPherson C, Jain D. Emotional and physical precipitants of ventricular arrhythmia. Circulation. 2002;106:1800–5. This study was the first to demonstrate the association between anger and ventricular arrhythmias, in patients with implantable cardioverter-defibrillators.
Stopper M, Joska T, Burg MM, et al. Electrophysiologic characteristics of anger-triggered arrhythmias. Heart Rhythm. 2007;4:268–73. see comment.
Sgoifo A, Stilli D, Aimi B, Parmigiani S, Manghi M, Musso E. Behavioral and electrocardiographic responses to social stress in male rats. Physiol Behav. 1994;55:209–16.
Stamler JS, Goldman ME, Gomes J, Matz D, Horowitz SF. The effect of stress and fatigue on cardiac rhythm in medical interns. J Electrocardiography. 1992;25:333–8.
Albert CM, Lampert R, Conti JB, et al. Episodes of anger trigger ventricular arrhythmias in patients with implantable cardioverter defibrillators. Circulation. 2006;114:II–831.
Lown B, Verrier R, Corbalan R. Psychologic stress and threshold for repetitive ventricular response. Science. 1973;182:834–6.
Lampert R, Jain D, Burg MM, Batsford WP, McPherson CA. Destabilizing effects of mental stress on ventricular arrhythmias in patients with implantable cardioverter-defibrillators. Circulation. 2000;101:158–64.
Lane RD, Reis HT, Peterson DR, Zareba W, Moss AJ. Happiness and stress alter susceptibility to cardiac events in Long QT Syndrome. Ann Noninvasive Electrocardiol. 2009;14:193–200.
Lampert R, Jamner L, Burg M, et al. Triggering of symptomatic atrial fibrillation by negative emotion. J Am Coll Cardiol. 2014;64:1533–4.
Tindle HA, Chang YF, Kuller LH, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120:656–62.
Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56.
Dockray S, Steptoe A. Positive affect and psychobiological processes. Neurosci Biobehav Rev. 2010;35:69–75. This article describes the importance of positive affect in influencing health outcomes.
Whang W, Albert CM, Sears Jr SF, et al. Depression as a predictor for appropriate shocks among patients with implantable cardioverter-defibrillators: results from the Triggers of Ventricular Arrhythmias (TOVA) study. J Am Coll Cardiol. 2005;45:1090–5.
Habibović M, Pedersen SS, Van Den Broek KC, et al. Anxiety and risk of ventricular arrhythmias or mortality in patients with an implantable cardioverter defibrillator. Psychosom Med. 2013;75:36–41.
van den Broek KC, Nyklicek I, van der Voort PH, Alings M, Meijer A, Denollet J. Risk of ventricular arrhythmia after implantable defibrillator treatment in anxious type d patients. J Am Coll Cardiol. 2009;54:531–7.
Burg MM, Lampert R, Joska T, Batsford W, Jain D. Psychological traits and emotion-triggering of ICD shock-terminated arrhythmias. Psychosom Med. 2004;66:898–902.
Bernardi L, Wdowczyk-Szulc J, Valenti C, et al. Effects of controlled breathing, mental activity, and mental stress with or without verbalization on heart rate variability. J Am Coll Cardiol. 2000;35:1462–9.
Vaccarino V, Lampert R, Bremner JD, et al. Depressive symptoms and heart rate variability: evidence for a shared genetic substrate in a study of twins. Psychosom Med. 2008;70:628–36.
Han J, Garcia de Jalon P, Moe GK. Adrenergic effects on ventricular vulnerability. Circ Res. 1964;14:516–24.
Cerati D, Schwartz PJ. Single cardiac vagal fiber activity, acute myocardial ischemia, and risk for sudden death. Circ Res. 1991;69:1389–401.
Toivonen L, Helenius K, Viitasalo M. Electrocardiographic repolarization during stress from awakening on alarm call. J Am Coll Cardiol. 1997;30:774–9.
Kop WJ, Krantz DS, Nearing BD, et al. Effects of acute mental stress and exercise on T-wave alternans in patients with implantable cardioverter defibrillators and controls. Circulation. 2004;109:1864–9. This study demonstrates that anger increases T-wave alternans, a measure of repolarization heterogeneity, likely an important mechanism in the effect of anger on arrhythmogenesis.
Nearing BD, Huang AH, Verrier RL. Dynamic tracking of cardiac vulnerability by complex demodulation of the T wave. Science. 1991;252:437–40.
Hohnloser SH, Klingenheben T, Zabel M, Yg L, Albrecht P, Cohen RJ. T wave alternans during exercise and atrial pacing in humans. J Cardiovasc Electrophysiol. 1997;8:987–93.
Rashba EJ, Cooklin M, MacMurdy K, et al. Effects of selective autonomic blockade on T-wave alternans in humans. Circulation. 2002;105:837–42.
Child N, Hanson B, Bishop M, et al. Effect of mental challenge induced by movie clips on action potential duration in normal human subjects independent of heart rate. Circ Arrhythm Electrophysiol. 2014;7:518–23.
Finlay MC, Lambiase PD, Ben-Simon R, Taggart P. Effect of mental stress on dynamic electrophysiological properties of the endocardium and epicardium in humans. Heart Rhythm. 2016;13:175–82.
Jacobson AF, Senior R, Cerqueira MD, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212–21.
Rubart M, Zipes DP. Mechanisms of sudden cardiac death. J Clin Investig. 2005;115:2305–15.
Gardner RT, Wang L, Lang BT, et al. Targeting protein tyrosine phosphatase sigma after myocardial infarction restores cardiac sympathetic innervation and prevents arrhythmias. Nat Commun. 2015;6:6235.
Hashemi Zanouz T, Liu YH, Sandoval V, et al. Cardiac sympathetic heterogeneity as measured by I-123 MIBG imaging in patients with ischemic cardiomyopathy. Society for Nuclear Medicine and Molecular Imaging. 2015. abstract.
Lampert R, Shusterman V, Burg M, Batsford W, McPherson C, Soufer R. Anger-induced T-wave alternans predicts future ventricular arrhythmias in patients with implantable cardioverter-defibrillators. J Am Coll Cardiol. 2009;53:774–8.
Verrier RL, Klingenheben T, Malik M, et al. Microvolt T-wave alternans physiological basis, methods of measurement, and clinical utility—consensus guideline by International Society for Holter and Noninvasive Electrocardiology. J Am Coll Cardiol. 2011;58:1309–24.
Moss AJ, Schuger C, Beck CA, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Eng J Med. 2012;367:2275–83.
Dunbar SB, Dougherty CM, Sears SF, et al. Educational and psychological interventions to improve outcomes for recipients of implantable cardioverter defibrillators and their families. Circulation. 2012;126:2146–72.
Toise SC, Sears SF, Schoenfeld MH, et al. Psychosocial and cardiac outcomes of yoga for ICD patients: a randomized clinical control trial. Pacing Clin Electrophysiol. 2014;37:48–62.
Freedenberg VA, Thomas SA, Friedmann E. A pilot study of a mindfulness based stress reduction program in adolescents with implantable cardioverter defibrillators or pacemakers. Pediatr Cardiol. 2015;36:786–95.
Serber ER, Fava JL, Christon LM, et al. Positive psychotherapy to improve autonomic function and mood in ICD patients (PAM-ICD): rationale and design of an RCT currently underway. Pace-Pacing and Clin Electrophysiol. 2016;39:458–70.
Chevalier P, Cottraux J, Mollard E, et al. Prevention of implantable defibrillator shocks by cognitive behavioral therapy: a pilot trial. Am Heart J. 2006;151:191e1–6.
Donahue RG, Lampert R, Dornelas E, Clemow L, Burg MM, Investigators R. Rationale and design of a randomized clinical trial comparing stress reduction treatment to usual cardiac care: the Reducing Vulnerability to Implantable Cardioverter Defibrillator Shock-Treated Ventricular Arrhythmias (RISTA) trial. Psychosom Med. 2010;72:172–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rachel Lampert declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain primary reports of any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Psychological Aspects of Cardiovascular Diseases
Rights and permissions
About this article
Cite this article
Lampert, R. Mental Stress and Ventricular Arrhythmias. Curr Cardiol Rep 18, 118 (2016). https://doi.org/10.1007/s11886-016-0798-6
Published:
DOI: https://doi.org/10.1007/s11886-016-0798-6