Abstract
Purpose of Review
This review seeks to review up to date literature surrounding the chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) to provide an overview of the subject. The review includes current understandings of the syndrome, the use of UPOINT, novel treatment strategies and future targets for management.
Recent Findings
Using the US National Institute of Health Chronic Prostatitis Symptom Index helps clinicians to monitor prostatitis symptoms, whilst using UPOINT as guidance of therapies based on patient phenotype(s) has advanced our ability to treat patients suffering with CP/CPPS. Furthermore, novel treatments look beyond traditional prostatic targets to treat CP/CPPS.
Summary
Whilst the use of UPOINT has opened up new targets for the treatment of CP/CPPS, more work is needed to both improve the quality of trials assessing them, as well as further elucidate the underlying pathophysiology behind this troublesome syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate pathologies causing lower urinary tract symptoms and pelvic pain adversely affect the quality of life of men of all ages. Prostatitis is a common condition with a prevalence of up to 9% within the general male population. Epidemiological date shows that prostatitis symptoms have a similar prevalence to ischaemic heart disease and diabetes mellitus [1]. Despite the prevalence of prostatitis-type symptoms, little is still known about the underlying pathophysiology.
For considerable time, treatment of prostatitis symptoms focussed on the use of antibiotics (even in the absence of infection) and anti-inflammatories (even when no inflammation is present) [2]. More recently, the use of prostate-focussed therapies have also been employed. Most often this involved the use of an α-blocker. Anecdotal evidence from physicians and patients suggests an improvement in symptoms [2, 3].This would appear a sensible approach as prostatitis suggests a prostatic origin for the symptoms. Despite this, evidence from multiple studies shows the efficacy of such treatments to be modest at best, especially when used as monotherapy [4].
A major advance in the diagnosis and management of prostatitis came in the late 1990s with the development of the US National Institute of Health (NIH) prostatitis classification system [5]. NIH category III is defined as non-bacterial chronic prostatitis (CP), also known as chronic pelvic pain syndrome (CPPS), reflecting the possibility of extra-prostatic therapeutic targets [2, 6••].
CP/CPPS can be defined as a urological pain or discomfort and/or sexual dysfunction that is present for at least 3 of the past 6 months in the absence of uropathogenic bacteria [7]. CP/CPPS has significant morbidity on patients, who can experience negative cognitive, sexual and emotional connotations.
Further developments in the management of the prostatitis syndromes came with the development of the NIH chronic prostatitis symptom index (NIH-CPSI). This has given physicians an objective scoring system for diagnosis as well as response to therapies.
To date, little is still known about the pathophysiology of CP/CPPS. The lack of a known and effective monotherapy for CP/CPPS makes treatment challenging for both the physician and the patient. Contemporary strategies suggest targeting therapies at the individuals phenotype by subdividing CP/CPPS into six distinct phenotypes based on the patients predominant symptom. This system, developed in 2009 by Shoskes et al., known as UPOINT looks at the six most common symptoms found in CP/CPPS, namely urinary, psychosocial, organ specific, infection, neurological/systemic or tenderness [8]. Crucially, the UPOINT system recognises that the majority of CP/CPPS symptoms are in fact unrelated to the prostate gland itself, but rather are manifestations of chronic pain arising from the pelvis.
Diagnosis
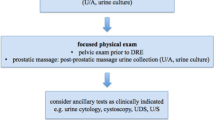
Careful examination and investigation are required to diagnose CP/CPPS. Given that there is no investigation for a definitive diagnosis of CP/CPPS, diagnosis will instead rely on patient history, symptoms and careful exclusion of differential diagnoses.
Examination of the abdomen may reveal a distended bladder and a DRE can assess the size and tenderness of the gland. Further palpation of the pelvic musculature (both externally and on DRE) can assess for pelvic muscle tenderness [7].
Urine dipstick testing combined with MSU can confirm the presence of either a UTI or haematuria [9].
Chronic bacterial prostatitis is an important differential diagnosis to exclude. The ‘gold standard’ is felt to be the four glass (Meares-Stamey) test, whereby microscopy is undertaken on urine from the urethra, bladder and prostate as well as expressed prostatic secretions [9]. Further investigations to exclude differential diagnoses include PSA testing from prostate cancer, STI screening, urodynamics and/or cystoscopy for bladder outlet obstruction and urethral stricture and MRI if a prostatic abscess is suspected.
Antibiotics, Alpha-Blockers and Anti-Inflammatories (AAA Therapy)
These medications, either as contemporaneous treatment or individual treatments at different times, have been the mainstay of management for chronic prostatitis since the 1960s.
Antibiotics are known to be effective in treating bacterial prostatitis. However, less than 10% of men who receive a diagnosis of prostatitis have a positive urine/semen culture [10]. The fact that antibiotics are commonly prescribed for chronic prostatitis and appear to be effective in some men may be due to a failure to culture an infective organism that is present. However, there are many cases of chronic prostatitis, which are non-bacterial, yet antibiotics still have a positive effect on symptoms in some men. One theory that could explain this phenomenon is the reduction of pro-inflammatory cytokine levels induced by fluoroquinolones, a commonly prescribed group of antibiotics for prostatitis [11, 12].
Alpha-blockers are known to target alpha-adrenergic receptors in the bladder neck and prostatic urethra [13]. The principal theory behind how they work in prostatitis involves increased relaxation of the bladder neck, which prevents turbulent voiding, and reflux of urine into the prostatic ducts. This reflux is postulated to cause prostatic inflammation [14].
Anti-inflammatories (usually NSAIDs) are prescribed for men with chronic prostatitis in the expectation that the reduction of inflammation within the gland will reduce symptom scores. Again, the theory of how they work in prostatitis is borrowed from our general knowledge of how anti-inflammatories can reduce circulating cytokine and prostaglandin levels, thereby reducing inflammation [15, 16].
When given as a combination, AAA therapy has been associated with significant improvements in Chronic Prostatitis Symptom Index (CPSI) scores in men with chronic prostatitis/chronic pelvic pain syndrome [4]. The most efficacious combination of medications appears to be alpha-blockers and antibiotics, which, in a systematic review of the chronic prostatitis literature, was found to produce the greatest difference in symptom, pain and quality of life scores [17]. The main issues when interpreting the data from these systematic reviews surround treatment variation and heterogeneity between research papers. It does appear that, when data is pooled, several therapies including AAA treatment individually and as a combination, finasteride, steroids and phytotherapy treatments have a positive effect on chronic prostatitis symptoms [18]. However, frequently, the well-conducted individual trials fail to show efficacy [19, 20]. Indeed, when individual alpha-blocker therapy and AAA therapy were compared in a trial, no difference was found. In addition, as well as medical therapy both surgical techniques such as prostatic massage and neuromodulatory techniques have been put forward as effective treatment in recent years [21, 22]. This tends to muddy the waters still further and may explain why proper consensus on this complex condition remains elusive and why CP/CPPS causes such symptomatic misery in some men. Whilst the disease mechanism remains poorly understood, targeted and efficacious treatment will be difficult.
UPOINT
A major advance in the treatment of CP/CPPS came in 2009 with the advent of UPOINT. Before this, the syndrome had been treated in broadly the same manner for the preceding 50 years. Shoskes et al. developed a novel system whereby CP/CPPS patients were subclassified according to their predominant symptom. This has allowed clinicians to both more accurately test hypotheses as well as treat patients [8]. Further work shows that not only does UPOINT discriminate between different clinical phenotypes, but also that the number of positive domains appears to correlate with the overall NIH-CPSI score [23•]. Further subdomains have since been proposed such as catastrophizing and depression in psychosocial, or voiding and storage for urinary.
Multiple trials looking into validating the use of UPOINT clinically suggest that the extended approach is beneficial to patients. A multimodal approach focussing on an individual’s phenotype leads to a significant improvement in both symptoms and quality of life.
A prospective study of 100 men who were positive for three or more UPOINT domains looked into NIH-CPSI score changes when treated as per their UPOINT phenotypes. Nearly 84% had a 6 point change in their NIH-CPSI score with the biggest changes in score being found in areas relating to pain, urinary symptoms and quality of life [24, 25].
Contemporary Therapy—The Use of Non-Pharmacological Treatments
The use of pharmacological treatments for CP/CPPS is well documented. Given that the underlying aetiology remains poorly understood and traditional treatments are often ineffective, new treatments are needed. Contemporary treatments are looking beyond the prostate for therapeutic targets, and many involve non-pharmacological treatments.
Acupuncture
Acupuncture is a component of traditional Chinese medicine and is thought to be able to modulate inflammation and the immune system. Studies looking at the efficacy of acupuncture in the treatment of CP/CPPS found it to be effective, especially in the management of pain [26]. Evidence suggests acupuncture may work by reducing prostatic inflammation as seen by a reduction in IL-1β in prostatic fluid. Whilst acupuncture is effective in improving pain symptoms, there has not been any demonstrated benefit in using acupuncture for management of urinary symptoms [27•].
Exercise
A 2015 prospective cohort study among men in the health professionals was conducted with the objective of examining the relation between physical activity and incidence of CP/CPPS in a large cohort of men. Leisure-time physical activity, including type and intensity of activity, was measured; and findings from this study, the first large scale and most comprehensive study to date on this association, suggest that higher levels of leisure-time physical activity may lower risk of CP/CPPS in middle-age and older men. Sedentary behaviour, measured as time spent watching television, was not associated with risk of CP/CPPS [28]. Aerobic exercise is shown to be superior to motion or stretching type exercises in improving pain symptoms [29]. It is thought that exercise reduces pain symptoms in CPPS through anti-inflammatory properties as well as decreasing the sensitivity to pain through changes in neuroendocrine and autonomic nerve function [28, 30].
Cognitive Behavioural Therapy
CP/CPPS can have a significant psychosocial burden for affected men. Sufferers describe significant impact on their quality of life, with pain impacting on both physical and mental health [31]. It has been shown that there is a link between the cognitive aspects of CP/CPPS (such as catastrophizing) and the physical outcomes (such as pain and perceived disability) [32]. With CP/CPPS being a chronic pain type syndrome, the goal of the clinician is to ameliorate pain. Despite this, conventional therapies have struggled to successfully treat such symptoms.
Cognitive behavioural therapy (CBT) offers an alternative route for managing CP/CPPS symptoms. When phenotypically classified using the UPOINT domains up to 34–37% of patients will score in the psychosocial domain [33]. This would suggest that effective psychological therapies could be an effective treatment for CP/CPPS patients. Furthermore, the development of CP/CPPS specific CBT programs could be of great benefit in patients who have failed to improve with standard medical therapies.
Physiotherapy
Physiotherapy has long been known to be beneficial in controlling pain symptoms in skeletal muscle pathologies. For the management of CP/CPPS, multiple physiotherapeutic management strategies have been proposed. These include acupuncture, posterior tibial nerve stimulation (PTNS), perineal extracorporeal shock wave therapy (ESWT) and aerobic exercise [34].
Clinical trials assessing the efficacy of ESWT and PTNS in patients with NIH category III B CP/CPPS found a clinically significant decrease in NIH-CPSI score. Sonoelectromagnetic therapy (SEMT) showed no significant decrease in NIH-CPSI score but did manage to improve quality of life [21, 34].
Phytotherapies
Plant-based remedies play a role in the management of many health conditions. Of all the prostatitis syndromes, phytotherapies have shown the most promise in the management of CP/CPPS. It is felt that many phytotherapies possess antioxidant and anti-inflammatory abilities, and it is through this that these plant-based therapies provide their clinical benefit.
The bioflavonoid quercetin is both anti-inflammatory and antioxidant and may be lacking in the diet of many CP/CPPS sufferers. This is because the food produce that is high in quercetin are those most prone to reproduce symptoms, such as tea, red wine and citrus fruits [35]. A double-blind trial found that the quercetin group had 35% improvement in NIH-CPSI score, compared to only 7% in the placebo group. This study also showed quercetin reduces leucocyte count to a greater degree than placebo [36]. A smaller group of patients had isoprostane levels measured. This compound is known to cause bladder contraction. With quercetin, the level of isoprostane reduced, along with a reduction in prostaglandin E2 and a rise in endorphins [36, 37].
A recent study by Morgia et al. looked at the efficacy of two phytotherapies—Calendula and Curcumina. Calendula is known to possess multiple qualities, including anti-inflammatory, antioxidant and immunostimulant effects and because of this has been investigated for use in wound healing, jaundice and as an antispasmodic. Curcumina is known to modulate pro-inflammatory cytokine pathways such as TNF-α, COX-2 and IL-1β. This phase II clinical trial demonstrated that a suppository containing both Curcumina and Calendula extract was able to produce clinical benefit by reducing pain and improve voiding and urinary symptoms after 1 month [38•].
Other phytotherapies that under investigated for CP/CPPS have had much less research. A rye pollen extract known as Cernilton has been investigated for use in BPH, but more recently studies have looked into its role in managing CP/CPPS. A randomised, double-blind phase III trial of 139 men found pain, quality of life and NIH-CPSI scores all improved with 12 weeks of treatment compared to placebo [18].
Other plant-based therapies, including traditional Chinese medicine therapies (such as Ningmitai and Qian-Yu decoction) have been investigated more recently and have been shown to be beneficial in symptom control in CP/CPPS sufferers. These studies, however, have been on a very small sample population, limiting the validity of the results [39, 40].
Surgery
Whilst CP/CPPS can be a debilitating illness for men, it is often found that pharmacological, as well as non-pharmacological therapies are ineffective. Surgery has long been investigated as a novel model of CP/CPPS management. Such surgical management includes both transurethral resection (TURP) as well as radical prostatectomy.
TURP procedures were investigated as long ago as the 1980s, when 49 patients underwent ‘radical TURP’—transurethral resection of the gland down to the capsule. Barnes et al. found 67% of patients had a good response (absence of infection and symptoms) at 1 year [41]. Despite this, radical TURP for CP/CPPS is no longer advocated [42•].
More recently, focus has moved towards radical prostatectomy in the management of CP/CPPS. In the early 1990s, Frazier et al. found that three out of five men had complete resolution of their disabling perineal pain after total prostatovesiculectomy [43]. More recently, Krongrad et al. reported early results from a phase II trial looking into laparoscopic radical prostatectomy for men with treatment refractory CP/CPPS. After six patients, Krongrad reports a drop in median NIH-CPSI score from 35 pre-surgery to 7.5 at 12 months post-surgery [44].
More recently, four patients with NIH class III prostatitis who were refractory to frontline therapies underwent robotic radical prostatectomy. All patients had significant reduction in symptoms, with a fall in median NIH-CPSI score from 30 pre-surgery to 5 at final follow-up (median of 34 months) [42•].
Whilst the above results are promising, they include very limited data of only nine patients. Nonetheless, the results from both small studies suggest further evaluation of both surgeries with wider ranging prospective trials. The current data on surgery in the management of CP/CPPS is so scanty that it was not included in a recent Cochrane literature review [45]. More work is clearly required before definitive conclusions can be made regarding the role of surgery in CP/CPPS management.
Future Therapeutic Targets
Prostatitis has been a clinical enigma for decades, causing frustration to both the patient and urologist. Since the advent of NIH classification and more recently the development of UPOINT phenotyping, there has been a great deal of research into CP/CPPS. Unfortunately to date, there has been minimal progress in the understanding of this debilitating illness, nor in our understanding in the pathophysiology behind it. Current research is looking to new therapeutic targets in the hope that progress is made in the management of CP/CPPS.
A Canadian study has recently looked into the use of intraprostatic injections of onabutuliniumtoxin A (onaBoNT-A) in the treatment of refractory CP/CPPS. By injecting onaBoNT-A transurethrally into the prostate of 43 men, it was shown to be effective in reducing pain symptoms in CP/CPPS sufferers with 72% reporting a 6-point change in NIH-CPSI score at 3 months. These improvements, however, were not durable, with only 37% still recording a 6-point decrease in NIH-CPSI score at 1 year [46].
Ultrasound has been investigated for the treatment of CP/CPPS. There have been numerous studies looking at the use of ultrasound enhancement of topically applied medicines, a process known as phonophoresis. Tantawy et al. identified pumpkin seed oil as being high in antioxidant, especially D7-sterols. Previous research has found such phytochemicals found in pumpkin seed oil blocks the conversion of testosterone to dihydrotestosterone by inhibiting 5α-reductase [47]. Phonophoresis using pumpkin seed oil, when compared to simple ultrasound reduced NIH-CPSI score as well as improving voiding. Ultrasound itself, also reduced NIH-CPSI score when compared to placebo procedure to a lesser extent [48].
Pentoxifylline is a xanthine derivative used in the treatment of muscle pain in patients with peripheral vascular disease. With oxidative stress being highly elevated in CP/CPPS patients, pentoxifylline has been evaluated as a treatment. In rat models, a significant decrease in inflammatory markers (such as TNF-α), PSA and histopathological changes (such as leucocyte infiltration) in the group treated with pentoxifylline [49]. Whilst promising, these results are yet to be tested and replicated in human trials.
Whilst oestrogen receptor-α (ERα) is thought to have a role in prostatic inflammation, ERβ may have an immunoprotective role limiting tissue damage by modulating the immune system [50]. Indeed, many different animal models of disease have demonstrated the anti-inflammatory effects of ERβ [51, 52]. A recent rat model has shown the relative increase in ERα to ERβ leading to the development of non-bacterial prostatic inflammation. By using 3α Andriol (a major metabolite of dihydrotestosterone), researchers were able to increase the relative expression of ERβ to ERα, leading to suppression of prostatic inflammatory changes [53••].
Whilst all of the above therapeutic targets are at an early stage of investigation, it remains promising that CP/CPPS is still at the forefront of researchers’ minds. With continuing work in this area, the future of CP/CPPS suffers remains optimistic.
Conclusions
Although no clear underlying pathology is agreed for CP/CPPS, there are different treatment approaches that have been used to overcome the symptoms of this challenging condition. One of the main pillars in managing this group of patients is proper counselling to explain the challenges and necessity for more than one line of treatments to achieve improvements. Less invasive followed by more invasive techniques are recommended along with applying the multidisciplinary concept.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sandhu J, Tu HYV. Recent advances in managing chronic prostatitis/chronic pelvic pain syndrome. F1000Res. 2017;6:F1000 Faculty Rev-1747.
Nickel JC, Shoskes DA. Phenotypic approach to the management of the chronic prostatitis/chronic pelvic pain syndrome. BJUI. 2010;106:1252–63.
Nickel JC. The three as of chronic prostatitis therapy: antibiotics, α-blockers and anti-inflammatories. What is the evidence? BJUI. 2004;94:1230–3.
Thankkinstian A, Attia J, Anothaisintawee T, Nickel JC. α-blockers, antibiotics and anti-inflammatories have a role in the management of chronic prostatitis/chronic pelvic pain syndrome. BJUI. 2012;110:1014–22.
Krieger JN, Lee SW, Jeon J, Cheah PY, Liong ML, Riley DE. Epidemiology of prostatitis. Int J Antimicrob Agents. 2007;31(Suppl1):S85–90.
•• Anderson RU, Wise D, Nathanson BH. Chronic prostatitis and/or chronic pelvic pain as a psychoneuromuscular disorder - a meta-analysis. Urology. 2018;120:23–9 Current evidence showing benefit of treating CP/CPPS as psychoneuromuscular disorder.
DeWitt-Foy ME, Nickel JC, Shoskes DA. Management of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol Focus. 2019;5(1):2–4.
Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009;73(3):538–42.
Rees J, Abrahams M, Doble A, Cooper A. Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJUI. 2015;116:509–25.
Lipsky BA, Byren I, Hoey CT. Treatment of bacterial prostatitis. CID. 2010;50:1641–52.
Tsivkovskii R, Sabet M, Tarazi Z, Griffith DC, Lomovskaya O, Dudley MN. Levofloxacin reduces inflammatory cytokine levels in human bronchial epithelia cells: implications for aerosol MP-376 (levofloxacin solution for inhalation) treatment of chronic pulmonary infections. FEMS Immunol Med Microbiol. 2011;61(2):141–6.
Ogino H, Fujii M, Ono M, Maezawa K, Kizu J, Hori S. In vivo and in vitro effects of fluoroquinolones on lipopolysaccharide-induced pro-inflammatory cytokine production. J Infect Chemother. 2009;15(3):168–73.
Roehrborn CG. Alfuzosin: overview of pharmacokinetics, safety, and efficacy of a clinically uroselective α-blocker. Urology. 2001;58(6):55–63.
Kirby RS, Lowe D, Bultitude MI, Shuttleworth KE. Intraprostatic urinary reflux: an etiological factor in abacterial prostatitis. Br J Urol. 1982;54:729–31.
Duclos AJ, Lee CT, Shoskes DA. Current treatment options in the management of chronic prostatitis. Ther Clin Risk Manag. 2007;3(4):507–12.
Hochreiter WW. Anti-inflammatory therapies for chronic prostatitis. Eur Urol Suppl. 2003;2(2):30–3.
Anothaisintawee T, Attia J, Nickel CJ, Thammakraisorn S, et al. Management of chronic prostatitis/chronic pelvic pain syndrome: a systematic review and network meta-analysis. JAMA. 2011;305(1):78–86.
Wagenlehner FM, Schneider H, Ludwig M, Schnitker J, et al. A pollen extract (Cernilton) in patients with inflammatory chronic prostatitis-chronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebo-controlled phase 3 study. Eur Urol. 2009;56(3):544–51.
Nickel JC, Shoskes DA, Wagenlehner FM. Management of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): the studies, the evidence, and the impact. World J Urol. 2013;31(4):747–53.
Bates SM, Hill VA, Anderson JB, Chapple CR, et al. A prospective, randomized, double-blind trial to evaluate the role of a short reducing course of oral corticosteroid therapy in the treatment of chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2007;99(2):355–9.
Kessler TM, Mordasini L, Weisstanner C, Jüni P, da Costa BR, Wiest R, et al. Sono-electro-magnetic therapy for treating chronic pelvic pain syndrome in men: a randomized, placebo-controlled, double-blind trial. PLoS One. 2014;9(12):e113368.
Ateya A, Fayez A, Hani R, Zohdy W, Gabbar MA, Shamloul R. Evaluation of prostatic massage in treatment of chronic prostatitis. Urology. 2006;67(4):674–8.
• Magri V, Wagenlehner F, Perletti G, Schneider S. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: sexual function domain improves correlations. J Urol. 2010;184(6):2339–45 Creation of sexual function domain further helps corrolate UPOINT to clinical phenotyping.
Shoskes DA, Nickel JC, Kattan MW. Phenotypically directed multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome: a prospective study using UPOINT. Urology. 2010;75(6):1249–53.
Guan X, Zhao C, Ou ZY, Wang L, et al. Use of the UPOINT phenotype system in treating Chinese patients with chronic prostatitis/chronic pelvic pain syndrome: a prospective study. Asian J Androl. 2015;17(1):120–3.
Qin Z, Wu J, Zhou J, Liu Z. Systematic review of acupuncture for chronic prostatitis/chronic pelvic pain syndrome. Medicine (Baltimore). 2016;95(11):e3095.
• Liu BP, Wang YT, Chen SD. Effect of acupuncture on clinical symptoms and laboratory indicators for chronic prostatitis/chronic pelvic pain syndrome: a systematic review and meta-analysis. Int Urol Nephrol. 2016;48(12):1977–91 Meta analysis suggesting the benefits of use of acupuncture in CP/CPPS.
Zhang R, Chomistek AK, Dimitrakoff JD, Giovannucci EL, et al. Physical activity and chronic prostatitis/chronic pelvic pain syndrome. Med Sci Sports Exerc. 2015;47(4):757–64.
Giubilei G, Mondaini N, Minervini A, Saieva C, Lapini A, Serni S, et al. Physical activity of men with chronic prostatitis/chronic pelvic pain syndrome not satisfied with conventional treatments--could it represent a valid option? The physical activity and male pelvic pain trial: a double-blind, randomized study. J Urol. 2007;177(1):159–65.
Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98(4):1154–62.
Nickel JC, Tripp DA, Chuai S, Litwin, et al. Psychosocial variables affect the quality of life of men with chronic prostatitis/chronic pelvic pain syndrome. BJUI. 2007;101:59–64.
Tripp DA, Nickel CJ, Wang Y, Litwin MS, et al. Catastrophizing and pain-contingent rest predict patient adjustment in men with chronic prostatitis/chronic pelvic pain syndrome. J Pain. 2006;7(10):697–708.
Brünahl CA, Klotz SGR, Dybowski C, Riegel B. Combined cognitive-behavioural and physiotherapeutic therapy for patients with chronic pelvic pain syndrome (COMBI-CPPS): study protocol for a controlled feasibility trial. Trials. 2018;19(1):20.
Magistro G, Wagenlehner FM, Grabe M, Weidner W, et al. Contemporary management of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2016;69(2):286–97.
Nickel CJ, Shoskes DA, Roehrborn CG, Moyad M. Nutraceuticals in prostate disease: the urologist’s role. Rev Urol. 2008;10(3):192–206.
Shoskes DA, Zeitlin SI, Shahed A, Rajfer J. Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology. 1999;54(6):960–3.
Shahed AR, Shoskes DA. Oxidative stress in prostatic fluid of patients with chronic pelvic pain syndrome: correlation with gram positive bacterial growth and treatment response. J Androl. 2000;21(5):669–75.
• Morgia G, Russo GI, Urzi D, Privitera S, et al. A phase II, randomized, single-blinded, placebo-controlled clinical trial on the efficacy of Curcumina and Calendula suppositories for the treatment of patients with chronic prostatitis/chronic pelvic pain syndrome type III. Arch Ital Urol Androl. 2017;89(2):110–3 RCT showing benefit of using phytotherapies for CP/CPPS.
Jin C, Chen Z, Zhang J. Meta-analysis of the efficacy of Ningmitai capsule on the treatment of chronic prostatitis in China. Medicine(Baltimore). 2018;97(33):e11840.
Zhang K, Zeng X, Chen Y, Zhao R, Wang H, Wu J. Therapeutic effects of Qian-Yu decoction and its three extracts on carrageenan-induced chronic prostatitis/chronic pelvic pain syndrome in rats. BMC Complement Altern Med. 2017;17(1):75.
Barnes RW, Hadley HL, O’Donoghue EP. Transurethral resection of the prostate for chronic bacterial prostatitis. Prostate. 1982;3(3):215–9.
•• Chopra S, Satkunasivam R, Aron M. Feasibility of robotic radical prostatectomy for medication refractory chronic prostatitis/chronic pelvic pain syndrome: initial results. Indian J Urol. 2016;32(3):238–41 Case report on the use of surgery for CP/CPPS in appropriately selected patients.
Frazier HA, Spalding TH, Paulson DF. Total prostatoseminal vesiculectomy in the treatment of debilitating perineal pain. J Urol. 1992;148(2):409–11.
Krongrad A, Shenghan L. Laparoscopic prostatectomy for severely symptomatic treatment-refractory chronic prostatitis: preliminary observations from an ongoing phase II clinical trial. UroToday Int J. 2011;4(2):1944–5784.
Franco JVA, Turk T, Xiao YT, Iakhno S, et al. Non-pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome: a Cochrane systematic review. Cochrane Database Syst Rev. 2018;1:CD01255.
Abdel-Meguid TA, Mosli HA, Farsi H, Alsayyad A, Tayib A, Sait M, et al. Treatment of refractory category III nonbacterial chronic prostatitis/chronic pelvic pain syndrome with intraprostatic injection of onabotulinumtoxin A: a prospective controlled study. Can J Urol. 2018;25(2):9273–80.
Hong H, Kim CS, Maeng S. Effects of pumpkin seed oil and saw palmetto oil in Korean men with symptomatic benign prostatic hyperplasia. Nutr Res Pract. 2009;3(4):323–7.
Tantawy SA, Elgohary HM, Kamel DM. Trans-perineal pumpkin seed oil phonophoresis as an adjunctive treatment for chronic nonbacterial prostatitis. Res Rep Urol. 2018;10:95–101.
Hajighorbani M, Ahmadi-Hamedani M, Shahab E, Hayati F, et al. Evaluation of the protective effect of pentoxifylline on carrageenan-induced chronic non-bacterial prostatitis in rats. Inflammopharmacology. 2017;25(3):343–50.
Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008;73(3):233–44.
Tiwari-Woodruff S, Voskuhl RR. Neuroprotective and anti-inflammatory effects of estrogen receptor ligand treatment in mice. J Neurol Sci. 2009;286(1–2):81–5.
Acar D, Cayan S, Aktaş S, Tek M. The effect of tamoxifen on bladder functions and histology, and the role of estrogen receptor beta in a rat chemical cystitis model. Neurourol Urodyn. 2007;26(2):309–16.
•• Mizoguchi S, Mori K, Wang Z, Liu T, Funahashi Y, Sato F, et al. Effects of estrogen receptor β stimulation in a rat model of non-bacterial prostatic inflammation. Prostate. 2017;77(7):803–11 New research with promising novel target for management of CP/CPPS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Inflammatory/Infectious Bladder Disorders
Rights and permissions
About this article
Cite this article
Farmer, T., Johnston, M., Milica, A. et al. Chronic Prostatitis/Chronic Pelvic Pain Syndrome: a Literature Review of NIH III Prostatitis. Curr Bladder Dysfunct Rep 14, 83–89 (2019). https://doi.org/10.1007/s11884-019-00508-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-019-00508-9