Abstract
Purpose of Review
This review summarizes the pathophysiology of calcific aortic valve stenosis (CAVS) and surveys relevant clinical data and basic research that explain how CAVS arises.
Recent Findings
Lipoprotein(a) [Lp(a)], lipoprotein-associated phospholipase A2 (Lp-PLA2), oxidized phospholipids (OxPL), autotaxin, and genetic driving forces such as mutations in LPA gene and NOTCH gene seem to play a major role in the development of CAVS. These factors might well become targets of medical therapy in the coming years.
Summary
CVAS seems to be a multifactorial disease that has much in common with coronary artery disease, mainly regarding lipidic accumulation and calcium deposition. No clinical trials conducted to date have managed to answer the key question of whether Lp(a) lowering and anti-calcific therapies confer a benefit in terms of reducing incidence or progression of CAVS, although additional outcome trials are ongoing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
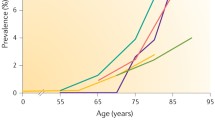
Calcific aortic valve stenosis (CAVS) is the most frequent cause of aortic valve disease, which leads to dyspnea, angina, syncope, heart failure, and, eventually, death. Up to one third of elderly patients have echocardiographic evidence of aortic valve sclerosis, which is the earliest stage of CAVS [1]. There are some commonalities between CAVS and atherosclerosis, such as risk factors (age, male sex, smoking, hyperlipidemia, hypertension, type II diabetes mellitus, and obesity) and histopathological manifestations, not forgetting that coronary artery disease is present in about 50% of patients with CAVS. Nevertheless, there has been so far no means of preventing CAVS onset or progression. For example, Simvastatin and Ezetimibe in Aortic Stenosis (SEAS) [2], Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression (SALTIRE) [3], and Aortic Stenosis Progression Observation: Measuring Effects of Rosuvastatin (ASTRONOMER) [4••] trials failed to show that the reduction of LDL cholesterol (with rosuvastatin compared with placebo) would reduce the incidence of CAVS progression or need for aortic valve replacement (AVR) in patients with mild-to-moderate CAVS, being these patients followed by watchful waiting until the need for AVR (either surgical or transcatheter). On the other hand, it was recently showed in the ASTRONOMER trial that high levels of lipoprotein(a) [Lp(a)] and the oxidized phospholipids (OxPL) it carries predict echocardiographically determined progression of CAVS and the need for AVR [4••]. It is well-known that increased Lp(a) levels are associated with increased risk for atherosclerosis [5]. These findings, along with novel therapies to substantially reduce circulating Lp(a) levels, have generated excitement about the possibility of a medical therapy for CAVS.
Lp(a) and CAVS
Lp [a] is an atherogenic lipoprotein particle that consists of a cholesterol-rich particle analogous to low-density lipoprotein that carries a substantial amount of proinflammatory and procalcifying oxidized phospholipids and has been associated with CAVS [6].
Kamstrup et al. [7] carried out a study whose purpose was to determine whether elevated lipoprotein(a) levels are prospectively associated with increased risk of calcific aortic valve stenosis (CAVS). They gathered data from 2 prospective general population studies with around 90,000 patients in which they conducted observational studies. Elevated Lp(a) levels were associated with higher multivariable adjusted hazard ratios for CAVS.
Arsenault et al. [8] carried out a study whose objective was to determine whether lipoprotein(a) levels were associated with an increased risk of developing CAVS. Serum lipoprotein(a) levels were measured in 17,553 individuals, and, among these, 118 developed CAVS during a mean follow-up of 11.7 years. Compared with participants in the bottom lipoprotein(a) tertile, those in the top lipoprotein(a) tertile had a higher risk of CAVS (hazard ratio, 1.57; 95% confidence interval, 1.02–2.42) after adjusting for age, sex, and smoking.
Yu et al. [9] showed that Lp(a) significantly increased calcium deposition and expression of chondro-osteogenic mediators, demonstrating a causal effect for Lp(a) in aortic valve calcification. In a second study, Yu et al. [10] aimed to determine the effects of Lp(a) on human aortic valve interstitial cells (HAVICs) in diseased human aortic valves. They examined the effects of Lp(a) on HAVICs mineralization and oxidant formation. They observed that HAVICs incubated with either LDL or Lp(a) had significantly higher calcium deposition compared with control (P < 0.001), with Lp(a) having the most significant effect (P < 0.01).
Després et al. [11•] conducted a study to estimate the prevalence of Lp(a) in patients from 2 echocardiography laboratories with CAVS and to determine if individuals with elevated Lp(a) but without CAVS display higher aortic valve microcalcification. They recruited 214 patients with CAVS from Montreal and 174 patients with CAVS and 108 controls from Québec City, Canada. In a second group of individuals with high (≥ 75 nmol/L, n = 27) or low (< 75 nmol/L, n = 28) Lp(a) levels, 18F-NaF positron emission tomography (PET)/computed tomography (CT) was performed to determine the difference in mean tissue-to-background ratio (TBR) of the aortic valve. Patients with CAVS had 62.0% higher Lp(a) (median = 28.7, interquartile range (8.2–116.6) vs 10.9 (3.6–28.8) nmol/L, P < 0.0001). Individuals without CAVS but elevated Lp(a) had 40% higher mean TBR compared with individuals with low Lp(a) levels (mean TBR = 1.25 ± 0.23 vs. 1.15 ± 0.11, P = 0.02).
Lipoprotein-Associated Phospholipase A2 (Lp-PLA2) and CAVS
Studies have indicated that calcific aortic valve diseased tissues are infiltrated by lipids and that inflammation may play a role in the pathobiology [12, 13]. Mahmut et al. [12] hypothesized that lipoprotein-associated phospholipase A2 (Lp-PLA2) is expressed in CAVS and may play a role in the mineralization of valve interstitial cells, since it generates lysophosphatidylcholine (LPC), which is the product of Lp-PLA2 activity that modulates inflammation and has been shown to promote mineralization of vascular smooth muscle cells. LPC was also documented on the mineralization of valve interstitial cell cultures. Analyses of CAVS and control non-mineralized aortic valves revealed that Lp-PLA2 was increased by 4.2-fold in mineralized aortic valves. Higher expression of Lp-PLA2 in stenotic aortic valves was confirmed by quantitative polymerase chain reaction, immunohistochemistry, and enzymatic Lp-PLA2 activity.
The PROGRESSA study [13] recruited patients with CAVS prospectively to examine the relationship between Lp-PLA2 activity and the progression rate of aortic stenosis. There was no significant association between plasma Lp-PLA2 activity or mass and stenosis progression in the whole cohort. However, increased Lp-PLA2 activity was associated with a faster stenosis progression rate in the subset of patients with mild aortic stenosis. These findings provided a certain impetus for the elaboration of a randomized trial targeting Lp-PLA2 activity in patients with early stages of CAVS.
OxPL and CAVS
Kamstrup et al. [14] performed a case-control study among 87,980 individuals (including 725 CAVS cases and 1413 controls free of cardiovascular disease) to test whether the risk of CAVS is mediated by the content of proinflammatory, procalcific phosphocoline-containing oxidized phospholipids (OxPL) carried by Lp(a), which has been shown to induce differentiation of calcifying vascular cells, suggesting that they might be involved in aortic valve calcification [15]. OxPL carried by apoB (apolipoprotein B-100; OxPL-apoB) or apolipoprotein(a) [OxPL-apo(a)] containing Lp(a) levels were measured. OxPL-apoB and OxPL-apo(a) levels correlated with Lp(a) levels among cases (P < 0.001) and controls (P < 0.001). OxPL-apoB and OxPL-apo(a) levels were associated with increased risk of CAVS.
Besides studying Lp(a), Després et al. [11•] also observed that patients with CAVS had 50% higher OxPL-apoB and 69.9% higher OxPL-apo(a) levels compared with individuals without CAVS (P < 0.0001).
Autotaxin Derived from Lp(a) and CAVS
Bouchareb et al. [16] described autotaxin (ATX) as an agent that transforms LPC into lysophosphatidic acid. They hypothesized that ATX-lysophosphatidic acid might promote inflammation/mineralization of the aortic valve and have documented the expression of ATX in control and mineralized aortic valves by using different approaches in a mouse model of calcific aortic valve disease. Enzyme specific ATX activity was elevated by 60% in mineralized aortic valves compared with control valves.
Bicuspid Aortic Valve, Atherosclerotic Calcification and CAVS: A Particular Threesome
Hemodynamic valvular impairment is a usual determinant of the natural history of bicuspid aortic valve (BAV). The role of elevated Lp(a) levels in influencing CAVS development in patients with tricuspid aortic valve was recognized. Sticchi et al. [17] investigated the association between Lp(a) the presence of CAVS in BAV patients. Sixty-nine patients were investigated. For each patient, clinical (ECG and echocardiography) and laboratory [Lp(a)] evaluation were performed. Patients were compared with 69 control subjects. Among BAV patients, significantly higher Lp(a) levels according to calcification degree were found. Furthermore, higher Lp(a) levels in patients with CAVS were also found. The authors concluded that their data suggest the potential role for Lp(a) as a possible risk marker useful to stratify, among BAV patients, those with a higher chance to develop CAVS.
Genetic Driving Forces of CAVS
The European Prospective Investigation into Cancer (EPIC)-Norfolk [8] study included around 18,000 patients to determine whether the rs10455872 genetic variant of LPA, which is strongly associated with Lp(a) levels, is associated with an increased risk of developing CAVS. Compared with rs10455872 AA homozygotes, carriers of 1 or 2 alleles were at increased risk of CAVS, suggesting that this association may be causal.
Data from the Copenhagen City Heart Study and the Copenhagen General Population Study were combined [7] with the purpose of determining whether LPA risk genotypes (rs10455872, rs3798220, kringle IV type 2 repeat polymorphism) prospectively associated with increased risk of CAVS. Lp(a) levels were elevated among carriers of rs10455872 and rs3798220 minor alleles, and of low number of KIV-2 repeats. Combining all genotypes, the analysis yielded a genetic relative risk for CAVS of 1.6 (95% CI: 1.2 to 2.1) for a 10-fold Lp(a) increase.
The role LPA Kringle IV type 2 (KIV-2) size polymorphism in influencing aortic valve calcification and stenosis development in patients with tricuspid aortic valve was recognized [7]. Sticchi et al. [17] investigated the association between LPA KIV-2 repeat number and the presence of calcification and stenosis in BAV patients. No significant association between Lp(a) circulating levels and LPA KIV-2 repeat number and BAV was evidenced, but lower LPA KIV-2 repeat numbers in subjects with more severe calcification degree were observed.
CAVS and coronary artery disease (CAD) have a significant genetic contribution and commonly co-exist. To compare and contrast genetic determinants of the two diseases, Trenkwalder et al. [18•] investigated associations of the LPA and 9p21 loci, i.e., the two strongest CAD risk loci, with risk of CAVS. The authors genotyped the CAD-associated variants at the LPA (rs10455872) in the GeneCAST (Genetics of Calcific Aortic STenosis) Consortium and confirmed the association of the LPA risk allele with risk of CAVS, again with a higher effect size in those without CAD.
The Genetic Epidemiology Research on Aging cohort [19••] replicated the association between LPA variants with CAVS and identify subgroups who are at higher risk of developing CAVS. Two single-nucleotide polymorphisms in the LPA locus, rs10455872 and rs3798220, are known to be associate with circulating plasma lipoprotein(a) levels and an LPA risk score. Both LPA variants were associated with CAVS, with a per risk allele odds ratio of 1.34 for rs10455872 and 1.31 for rs3798220 after adjusting for age and sex. The results remained significant after adjusting for risk factors. Individuals with 2 risk alleles had a 2-fold or greater odds of CAVS compared with individuals with no risk alleles. Each rs10455872 risk allele was also associated with CAVS.
To study the associations of LPA variants with CAVS in a cohort [6] of patients undergoing heart surgery and LPA with CAVS in patients with CAD vs those without CAD and to determine whether first-degree relatives of patients with CAVS and high lipoprotein(a) (Lp [a]) levels showed evidence of aortic valve microcalcification, a study included 1009 individuals undergoing cardiac surgery and 1017 control participants in the QUEBEC-CAVS cohort (Genome-Wide Association Study on Calcific Aortic Valve Stenosis in Quebec); 3258 individuals with CAVS and CAD; 41,100 controls with CAD; 2069 individuals with CAVS without CAD; and 380,075 control participants without CAD in the UK Biobank, EPIC-Norfolk (the European Prospective Investigation of Cancer) and GERA studies (Genetic Epidemiology Research on Aging) and 3 French cohorts combined. In the QUEBEC-CAVS study, each SD increase of the genetic risk score was associated with a higher risk of CAVS in patients with and without CAD (Table 1).
Abraityte et al. [20] showed for the first time a relationship between serum levels of the Notch ligand Delta-like (DLL)1 and symptomatic AS. Notch is a signaling pathway whose mutated receptors have been linked to valve defects and valve calcification, being its ligand known as Delta-like (DLL) shown to promote osteogenic differentiation and calcification. Their main findings were that circulating DLL1 levels were elevated in patients with symptomatic CAVS, and DLL1 was expressed in calcified aortic valves and correlated with systemic DLL1 concentrations.
Hadji et al. [21] identified in patients with CAVS that, in mineralized aortic valves, the dysregulated NOTCH1 gene expression led to the osteogenic transition of valve interstitial cells, inducing a faster progression of CAVS.
Irtyuga et al. [22] showed that mutation in NOTCH1 might play an important role in the formation and progression of aortic valve calcification due to modulation of the ligand-binding site in NOTCH1 by calcium affinity.
Limitations in the Current Literature—the Problem with Animal Models
In the study of CAVS, a large number of current animal research is carried out in mouse models, as mice are uniquely suited to mechanistic studies of aortic valve pathology. Mouse models of CAVS offer multiple advantages, including their small size, uncomplicated husbandry, and efficiency. Additionally, short generation time, less difficulty of genetic manipulations, and availability of clonal samples allow for the possibility of investigation of molecular mediators of CAVS [23,24,25]. Despite these advantages, mouse models are under the influence of several limitations. The anatomical structure of mouse aortic valves differs enormously from that of humans. Mice do not have the triple layer of aortic valve tissue characteristic of human valves; rather their leaflets usually have at the most a 10-cell thickness and do not exhibit separated layers [25, 26]. Furthermore, wild-type mice on standard diets do not develop spontaneous calcification [24, 25], and consequently the study of CAVS in mouse models needs dietary [25, 27] genetic [27,28,29,30] or other interventions [31, 32] to give rise to calcium burden on the valves. According to Miller et al. [33], perhaps the greatest challenge in using mice is examination of molecular mechanisms underlying CAVS. The small size of the valve cusps and base, and limited amount of tissue, makes isolation of pure tissue and examination of gene expression (by quantitative real-time reverse transcriptase-polymerase chain reaction) challenging.
Future Perspectives: Lipid-Lowering Strategies and Anti-Calcific Therapies
At the moment, the following trials are investigating either lipid-lowering strategies or anti-calcific therapies: EAVall (Early Aortic Valve Lipoprotein(a) Lowering; https://clinicaltrials.gov/ct2/show/NCT02109614), SALTIRE-II (Study Investigating the Effect of Drugs Used to Treat Osteoporosis on the Progression of Calcific Aortic Stenosis; https://clinicaltrials.gov/ct2/show/NCT02132026), PCSK9 Inhibitors in the Progression of Aortic Stenosis (https://clinicaltrials.gov/ct2/show/NCT03051360), BASIK2 (Bicuspid Aortic Valve Stenosis and the Effect of Vitamin K2 on Calcium Metabolism on 18F-NaF PET/MRI; https://clinicaltrials.gov/ct2/show/NCT02917525), CALCIFICA (Value of Oral Phytate [InsP6] in the Prevention of Progression of Cardiovascular Calcifications; https://clinicaltrials.gov/ct2/show/NCT01000233), and CAVS (A Study Evaluating the Effects of Ataciguat [HMR1766] on Aortic Valve Calcification; https://clinicaltrials.gov/ct2/show/NCT02481258). Just a word of caution: Since women have less calcification than men, it is possible that these therapeutic options will not be effective in this population, thus, results must be provided by sex in these studies and probably other studies targeting fibrosis instead of calcification would be interesting in women.
Conclusions
Cutting-edge research has shed some light upon the whole of this complex issue. As we deepen our understanding of the pathophysiology underlying CAVS, novel therapeutic approaches have been adopted and put under the microscope. Nevertheless, no medical therapy to date has proven effective in reducing the incidence or progression of CAVS. Although lipoproteins and calcium remain possible targets for therapeutic intervention in the scenario of CAVS, we are still waiting for the groundbreaking clinical trial to elevate these actors to greater clinical relevance. With positive results from such clinical trials, it might finally be time to add management of these factors to our daily practice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cho KI, Sakuma I, Sohn IS, Jo SH, Koh KK. Inflammatory and metabolic mechanisms underlying the calcific aortic valve disease. Atherosclerosis. 2018;277:60–5.
Rossebø AB, Pedersen TR, Boman K, Brudi P, Chambers JB, Egstrup K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med. 2008;359(13):1343–56.
Cowell SJ, Newby DE, Prescott RJ, Bloomfield P, Reid J, Northridge DB, et al. Scottish aortic stenosis and lipid lowering trial, impact on regression (SALTIRE) investigators. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. 2005;352(23):2389–97.
•• Capoulade R, Chan KL, Mathieu P, Bosse Y, Dumesnil JG, Tam JW, et al. Autoantibodies and immune complexes to oxidation-specific epitopes and progression of aortic stenosis: results from the ASTRONOMER trial. Atherosclerosis. 2017;260:1–7 This study failed to show that the reduction of LDL cholesterol can reduce the incidence of CAVS, and indirect markers of oxidation-specific epitopes are predictive of its progression.
Ferretti G, Bacchetti T, Johnston TP, Banach M, Pirro M, Sahebkar A. Lipoprotein(a): a missing culprit in the management of athero-thrombosis? J Cell Physiol. 2018;233:2966–81.
Perrot N, Thériault S, Dina C, Chen HU, Boekholdt SM, Rigade S, et al. Genetic variation in LPA, calcific aortic valve stenosis in patients undergoing cardiac surgery, and familial risk of aortic valve microcalcification. JAMA Cardiol. 2019. https://doi.org/10.1001/jamacardio.2019.1581.
Kamstrup PR, Tybjærg-Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol. 2014;63:470–7.
Arsenault BJ, Boekholdt SM, Dubé MP, Rhéaume E, Wareham NJ, Khaw KT, et al. Lipoprotein(a) levels, genotype, and incident aortic valve stenosis: a prospective Mendelian randomization study and replication in a case-control cohort. Circ Cardiovasc Genet. 2014;7(3):304–10.
Yu B, Hafiane A, Thanassoulis G, Ott L, Filwood N, Cerruti M, et al. Lipoprotein(a) induces human aortic valve interstitial cell calcification. J Am Coll Cardiol Basic Trans Science. 2017;2:358–71.
Yu B, Khan K, Hamid Q, Mardini A, Siddique A, Aguilar-Gonzalez LP, et al. Pathological significance of lipoprotein(a) in aortic valve stenosis. Atherosclerosis. 2018;272:168–74.
• Després AA, Perrot N, Poulin A, Tastet L, Shen M, Chen HY, et al. Lipoprotein(a), oxidized phospholipids, and aortic valve microcalcification assessed by 18F-sodium fluoride positron emission tomography and computed tomography. CJC Open. 2019;1(3):131–40 This study suggests that elevated Lp(a) and OxPL levels are associated with prevalent CAVS in a “real-world” setting, and showed that aortic valve microcalcification is present before the development of macroscopic and clinically manifested CAVS.
Mahmut A, Mahmut A, Husseini DE, Fournier D, Bouchareb R, Després JP, et al. Elevated expression of lipoprotein-associated phospholipase A2 in calcific aortic valve disease. Implications for valve mineralization. J Am CollCardiol. 2014;63:460–9.
Capoulade R, Mahmut A, Tastet L, Arsenault M, Bédard E, Dumesni JG, et al. Impact of plasma Lp-PLA2 activity on the progression of aortic stenosis the PROGRESSA study. J Am Coll Cardiol Img. 2015;8:26–33.
Kamstrup PR, Hung MY, Witztum JL, Tsimikas S, Nordestgaard BG. Oxidized phospholipids and risk of calcific aortic valve disease the Copenhagen General Population Study. Arterioscler Thromb Vasc Biol. 2017;37:1570–8.
Demer LL, Tintut Y. Inflammatory, metabolic, and genetic mechanisms of vascular calcification. Arterioscler Thromb Vasc Biol. 2014;34:715–23.
Bouchareb R, Mahmut A, Nsaibia MJ, Boulanger MC, Dahou A, Lépine JL, et al. Autotaxin derived from lipoprotein(a) and valve interstitial cells promotes inflammation and mineralization of the aortic valve. Circulation. 2015;132:677–90.
Sticchi E, Giusti B, Cordisco A, Gori AM, Sereni A, Sofi F, et al. Role of lipoprotein (a) and LPA KIV2 repeat polymorphism in bicuspid aortic valve stenosis and calcifcation: a proof of concept study. Intern Emerg Med. 2019;14:45.
• Trenkwalder T, Nelson CP, Musameh MD, Mordi IR, Kessler T, Pellegrini C, et al. Effects of the coronary artery disease associated LPA and 9p21 loci on risk of aortic valve stenosis. Int J Cardiol. 2019;276:212–7. https://doi.org/10.1016/j.ijcard.2018.11.094 This study confirmed the association of the LPA locus with risk of AS, with a higher effect in those without concomitant coronary disease.
•• Chen HU, Dufresne L, Burr H, Ambikkumar A, Yasui N, et al. Association of LPA variants with aortic stenosis a large-scale study using diagnostic and procedural codes from electronic health records. JAMA Cardiol. 2018;3(1):18–23. https://doi.org/10.1001/jamacardio.2017.4266 Large genetic study about AS including over 40,000 individuals, confirming the association between 2 LPA variants and AS.
Abraityte A, Gullestad L, Askevold ET, Nymo S, Dahl CP, Aakhus S, et al. The Notch ligand Delta-like 1 is elevated and associated with mortality in patients with symptomatic aortic stenosis. Int J Cardiol. 2015;180:18–20.
Hadji F, Boulanger MC, Guay SP, Gaudreault N, Amellah S, Mkannez G, et al. Altered DNA methylation of long noncoding RNA H19 in calcific aortic valve disease promotes mineralization by silencing NOTCH1. Circulation. 2016;134:1848–62.
Irtyuga O, Malashicheva A, Zhiduleva E, Freylikhman O, Rotar O, Bäck M, et al. NOTCH1 mutations in aortic stenosis: association with osteoprotegerin/RANK/RANKL. Biomed Res Int. 2017;2017:6917907.
Guerraty M, Mohler ER. Models of aortic valve calcification. J Investig Med. 2007;55(6):278–83.
Fazio S, Linton MF. Mouse models of hyperlipidemia and atherosclerosis. Front Biosci. 2001;6:D515–25.
Sider KL, Blaser MC, Simmons CA. Animal models of calcific aortic valve disease. Int J Inflam. 2011;2011:364310.
Hinton RB Jr, Alfieri CM, Witt SA, Glascock BJ, Khoury PR, Benson DW, et al. Mouse heart valve structure and function: echocardiographic and morphometric analyses from the fetus through the aged adult. Am J Physiol Heart Circ Physiol. 2008;294(6):H2480–8.
Drolet MC, Roussel E, Deshaies Y, Couet J, Arsenault M. A high fat/high carbohydrate diet induces aortic valve disease in C57BL/6J mice. J Am Coll Cardiol. 2006;47(4):850–5.
Weiss RM, Ohashi M, Miller JD, Young SG, Heistad DD. Calcific aortic valve stenosis in old hypercholesterolemic mice. Circulation. 2006;114(19):2065–9.
Aikawa E, Nahrendorf M, Figueiredo JL, Swirski FK, Shtatland T, Kohler RH, et al. Osteogenesis associates with inflammation in early-stage atherosclerosis evaluated by molecular imaging in vivo. Circulation. 2007;116(24):2841–50.
Aikawa E, Nahrendorf M, Sosnovik D, Lok VM, Jaffer FA, Aikawa M, et al. Multimodality molecular imaging identifies proteolytic and osteogenic activities in early aortic valve disease. Circulation. 2007;115(3):377–86.
Aikawa E, Aikawa M, Libby P, Figueiredo JL, Rusanescu G, Iwamoto Y, et al. Arterial and aortic valve calcification abolished by elastolytic cathepsin S deficiency in chronic renal disease. Circulation. 2009;119(13):1785–94.
Hjortnaes J, Butcher J, Figueiredo JL, Riccio M, Kohler RH, Kozloff KM, et al. Arterial and aortic valve calcification inversely correlates with osteoporotic bone remodelling: a role for inflammation. Eur Heart J. 2010;31(16):1975–84.
Miller JD, Weiss RM, Heistad DD. Calcific aortic valve stenosis: methods, models, and mechanisms. Circ Res. 2011;108(11):1392–412.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Evidence-Based Medicine, Clinical Trials and Their Interpretations
Rights and permissions
About this article
Cite this article
de Oliveira Sá, M.P.B., Cavalcanti, L.R.P., Perazzo, Á.M. et al. Calcific Aortic Valve Stenosis and Atherosclerotic Calcification. Curr Atheroscler Rep 22, 2 (2020). https://doi.org/10.1007/s11883-020-0821-7
Published:
DOI: https://doi.org/10.1007/s11883-020-0821-7