Abstract
Aspirin remains one of the most extensively studied cardiovascular medications in the history of medicine. However, despite multiple, well-designed, large randomized controlled trials evaluating the potential of aspirin to prevent cardiovascular events in individuals without known cardiovascular disease (CVD), the role of aspirin in primary prevention is currently unclear. The initial aspirin trials included largely low-risk individuals with primary outcomes mostly focused on myocardial infarction (MI) and stroke, and showed a significant reduction in these CVD outcomes, especially MI. The more recently conducted trials have focused on older, higher CVD risk populations with high rates of lipid-lowering and antihypertensive medications use. These studies have used broader CVD outcomes as their primary end points and have failed to show a significant benefit of aspirin therapy in primary prevention. The exact reasons for the lack of efficacy in these recent trials are unclear but may be related to low rate of atherothrombotic events relative to other CVD events in the populations studied. Four large randomized controlled trials are currently underway which should provide some clarity in determining the optimal use of aspirin in the primary prevention of CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platelet activation and subsequent arterial thrombosis, triggered by atherosclerotic plaque rupture, has long been understood to be directly responsible for a substantial portion of cardiovascular disease (CVD) events and deaths, including the majority of myocardial infarctions (MIs) [1–3]. In addition to analgesic, anti-inflammatory, and anti-pyretic effects, acetylsalicylic acid (aspirin) inhibits platelet cyclooxygenase, particularly the cyclooxygenase-1 isozyme whose major product induces platelet aggregation [4]. The role of aspirin as an anti-platelet agent in the treatment of acute cardiovascular events as well as for secondary prevention of future CVD events has been well established [5–9].
However, despite ten well-designed randomized controlled trials (RCTs) that focused patients without known CVD [10••, 11–14, 15•, 16–18, 19••], the role of aspirin for the primary prevention of CVD is currently unclear. Recently, the United States Prevention Service Task Force (USPSTF) made available for comment a draft recommendation statement on the use of aspirin for the prevention CVD and cancer [20]. The statement recommends that adults aged 50–59 who have an estimated 10-year CVD risk of ≥10 % should consider taking a low dose aspirin. They also suggest individuals age 60–69 at increased CVD risk discuss the risks and benefits of ASA with their doctor. These recommendations have raised controversy given that lack of consensus on this topic. The aim of this review is to summarize the evidence on aspirin for primary prevention, focusing on prior RCTs, review the most recent guidelines, and discuss potential future directions to determine the optimal use of aspirin for the primary prevention of CVD.
The First 6 RCTs: Clear Efficacy
From 1988–2005, six RCTs evaluated the potential of aspirin to reduce CVD events in individuals without known CVD (Table 1). The Physician’s Health Study (PHS) randomized 22,071 US physicians using a 2 × 2 factorial design with 325 mg of aspirin every-other-day, beta carotene, and placebos [10••]. In PHS, a substantial 44 % relative risk reduction (relative risk 0.56, 95 % confidence interval [CI] 0.45–0.70) was seen for fatal and non-fatal MI in those taking aspirin alone compared to placebo. There was no reduction in CVD mortality though mortality rates were substantially lower than what the trial was powered to evaluate. The British Doctor’s Trial randomized 5139 male physicians without known cardiovascular disease to either take 500 mg of aspirin daily or avoid aspirin in a 2:1 fashion and followed them over 6 years [11]. The study was not placebo controlled and ∼20 % of the intervention group stopped aspirin due to potential side effects. The study showed significant reductions in TIAs by half in the aspirin group but no significant difference in rates of MI. However, given the smaller sample size, the significant rate of aspirin discontinuation, and the fact that the observed event rate of MI was less than predicted, the study was underpowered to evaluate many of its primary outcome measures.
Four additional prospective trials followed over the next ∼15 years. The first two, the Thrombosis Prevention Trial (TPT) and Hypertension Optimal Treatment (HOT) Trial, targeted populations at greater risk of CVD. The 2 × 2 factorial design TPT trial examined the benefit of warfarin and aspirin in primary prevention on 5499 men aged 45–69 years who were at high risk for coronary heart disease, and found a 20 % relative risk reduction for all ischemic heart disease, mostly attributed to a 32 % relative risk reduction in non-fatal coronary events with aspirin [12]. The HOT trial examined the potential benefits of lowering blood pressure and use of aspirin in 18,790 hypertensive men and women. The trial demonstrated a relative risk reduction in major cardiovascular events by 15 %, with a significant 36 % risk reduction for MI [13]. Neither TPT or the HOT trial showed a significant difference in mortality, though again, the trials were not powered to adequately evaluate those outcomes. The Primary Prevention Project (PPP) examined the effect of vitamin E and aspirin in 4495 men and women with 1+ major cardiac risk factor, and showed a 44 % relative risk reduction in cardiovascular death and 33 % relative risk reduction in total cardiovascular events in the aspirin group [14]. Finally, the Women’s Health Study (WHS) randomized 39,876 female health professionals without known CVD or major illnesses to either 100 mg of aspirin or placebo every-other-day [15•]. No significant decrease in the rate of overall cardiovascular events or MI was noted in the intervention group. However, the study included women at very low risk for CVD events (the rate of the primary outcome of major CVD events—non-fatal MI, non-fatal stroke, or CVD death—was <3 % over 10 years). When stratified by age in WHS, women over 65 did have a significant reduction in major CVD events (hazard ratio [HR] 0.74 (95 % CI, 0.59–0.92)), including a reduction in non-fatal myocardial infarction (HR 0.66 [95 % CI, 0.44–0.97]). Unlike previous studies, a 17 % decrease in the risk of stroke was noted as well (HR 0.83 [95 % CI, 0.69–0.99]).
In 2006, a meta-analysis was performed using the first six RCTs, comparing benefits and risks by sex [21]. Pooled results showed a 12 % reduction in cardiovascular events and 17 % reduction in strokes among studied women. Men were shown to have a 14 % reduction in cardiovascular events and a 32 % reduction in MI. There was a significant increase in risk of bleeding in both women and men as well (odds ratio 1.68 [95 % CI, 1.13–2.52] in women, odds ratio 1.72 [96 % CI, 1.35–2.20] in men). Based on these data, in 2009, the USPSTF published tailored recommendations for men and women [22]. The guidelines assumed a 32 % reduction in CHD in men and a 17 % reduction in stroke in women as well as a varying risk in the rate of gastrointestinal bleeding with aspirin use according to age. Aspirin was encouraged for women 55 to 79 years old whose risk for stroke outweighed their risk for gastrointestinal bleeding. Men 45 to 79 years old whose risk for MI outweighed that of gastrointestinal bleeding were also encouraged to take aspirin. Guidelines from the American Heart Association (AHA) have followed a similar absolute risk-based approach to the use of aspirin. The 2002 guidelines for primary prevention of CVD and stroke recommended that men with a ≥10 % 10-year risk of CHD consider taking a daily aspirin [23]. A 2011 update to the AHA guidelines for CVD prevention for women recommended aspirin use for women with a ≥10 % 10-year CVD risk [24].
The Recent four RCTs: Efficacy Unclear
From 2008–2014, four additional RCTs have been published that evaluated aspirin for primary prevention in individuals presumed to be at high CVD risk (Table 2). The Prevention of Progression of Arterial Disease and Diabetes (POPADAD) trial included 1276 adults with diabetes and an abnormal ankle-brachial index suggestive of peripheral arterial disease [16]. Despite a study population of individuals at high CVD risk, there was no difference in the primary cardiovascular end points with the use of 100 mg aspirin daily over a mean follow-up of ∼6 years (HR 0.98; 95 % CI, 0.76 to 1.26). The Japanese Primary Prevention of Atherosclerosis with Aspirin for Diabetes (JPAD) trial also evaluated a high-risk population, including 2539 individuals with type II diabetes but without known CVD [17]. Over a median follow-up of 4.4 years, there was no difference in the primary end-point of total atherosclerotic events (HR 0.80; 95 % CI, 0.58–1.10). Both the POPADAD and JPAD trials suffered from difficulties in recruitment and lower than expected event rates and subsequently were underpowered to evaluate their primary end points.
In 2010, the Aspirin for Asymptomatic Atherosclerosis (AAA) trial screened individuals without known CVD for a low ankle-brachial index (ABI) as a proxy for atherosclerosis [18]. Over a mean follow-up of 8.2 (1.6) years, 3350 men and women were followed on either 100 mg of aspirin daily or placebo. The primary end point was a composite of fatal or non-fatal coronary event or stroke as well as revascularization. Despite the long duration of follow-up and adequate event rate, there was no difference in the primary end point (HR 1.03; 95 % CI, 0.84–1.27). Most recently, the Japanese Primary Prevention Project (JPPP) with aspirin evaluated the effect of 100 mg of aspirin daily on the composite end point of non-fatal MI or stroke or CVD death [19••]. Patients included in the study were age 60–85 and had to have at least one risk factor (hyperlipidemia, hypertension, or diabetes). In 14,464 men and women followed for ∼5 years, there was no difference in the primary end point (HR 0.94; 95 % CI, 0.77–1.15). There was a significant reduction in non-fatal MI (HR 0.53; 95 % CI, 0.31–0.091) but also a significant increase in the risk of serious extra-cranial hemorrhage (HR 1.85; 95 % CI, 1.22–2.81).
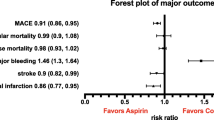
A meta-analysis encompassing the first nine aforementioned published RCTs demonstrated a small benefit in terms of CVD risk reduction, with a significant 10 % reduction in CVD events and a 20 % reduction in non-fatal MI with the use of aspirin but no significant CVD mortality benefit [25]. However, this benefit came at the cost of a virtually equivalent increase in the risk of bleeding, with a calculated number-needed-to-treat (NNT) to prevent a single CVD event of 120 versus a number-needed-to-harm (NNH) for a significant bleed of 73. Based on these data, the European Society of Cardiology updated guidelines on cardiovascular prevention in 2012 did not endorse the use of aspirin for primary prevention due to lack of clear efficacy and a significant increase in major bleeding [26]. Neither the AHA nor the USPSTF have officially updated their guidelines for aspirin use based on these recent studies, though the USPSTF did recently make available a draft recommendation statement on the use of aspirin for the prevention CVD and cancer [20]. The recent lifestyle and cholesterol guidelines from the American College of Cardiology (ACC) and the AHA did not address the use of aspirin for primary prevention of CVD [27, 28].
Applying the Data and Future Directions: Finding Clarity
How can the results of the first six RCTs be reconciled with the results of the four recent RCTs? There are several potential explanations. Differences in sample size, patient populations, study design, and aspirin dosage may all have played a role in producing variable results among the different trials. Potentially, a more important difference is that the initial trials focused on MI and stroke at a time when traditional CVD risk factors were less optimally controlled while the recent trials have focused on broader CVD outcomes in patients with high rates of use of preventive CVD medications.
From the standpoint of pathophysiology, aspirin should largely just be beneficial for those individuals destined to otherwise experience an event that involves arterial thrombosis. A number of factors may have led to a decrease over the past couple of decades in the number of atherothrombotic events relative to other cardiovascular events. The initial aspirin trials occurred at a time when cholesterol and blood pressure were not as well controlled as they were at the time of the most recent four aspirin trials [29, 30]. Utilization of statin therapy was infrequent during the first six trials, whereas given the high-risk nature of the individuals included in the recent four trials, statin therapy was present in the majority of patients in those trials. Both statin therapy as well as improved blood pressure control have been associated with a substantial reduction in MI [31, 32]. Having a patient population with well controlled CHD risk factors may have removed the “low-hanging fruit” that was present in previous aspirin trials. To support this concept, prior data has shown the rate of MI has declined significantly over the past two decades, largely due to a decline in STEMI [33], which is almost universally an atherothrombotic event. This decline in CHD has largely been attributed to better control of CHD risk factors [34]. Recent data from a large electronic health record database of ∼1.9 million adults showed that the majority (66 %) of all initial CVD events were not myocardial infarction or stroke [35]. Additionally, older individuals in that database were even less likely to suffer an MI or stroke as there initial event. Given that the four recent trials included older individuals compared to the first six trials, it may be that the populations studied were at high CVD risk, but not necessarily high risk for an atherothrombotic event.
As an example, in the JPPP aspirin trial, aspirin reduced the rate of non-fatal MI by 47 %, but this did not significantly influence the primary outcome as non-fatal MIs represented only a small portion of the total CVD events (207 total events in the placebo group, 56 fatal CVD events, and 38 [18 % of total CVD events] were non-fatal MI) [19••]. Conversely, in PHS, the sample size was 1.5 times higher compared to JPPP, but there were 5.6 times more non-fatal MIs (213 in the placebo group) over a similar follow-up duration of ∼5 years [10••]. It seems plausible that aspirin may have not lost its efficacy for preventing atherothrombotic events over time, but rather it has recently been studied in patient populations with low rates of the type of CVD events it is capable of preventing.
There is hope for clarity in regard to the risks and benefits of aspirin for primary CVD prevention in the modern era of medicine with four trials currently underway. The Aspirin to Reduce Risk of Initial Vascular Events (ARRIVE) trial has enrolled 12,000 patients with moderate CVD risk, a group not studied in previous trials [36]. The Aspirin in Reducing Events in the Elderly (ASPREE) trial has 15,000 patients over 70 years old without known CVD enrolled, a group also not included in previous studies [37]. To better determine what, if any benefit, aspirin plays in primary prevention of CVD in diabetic patients, the ongoing ASCEND trial (A Study of Cardiovascular Events in Diabetes) has enrolled over 15,000 patients with plans to complete the study within the next couple of years [38]. Additionally, ACCEPT-D (Aspirin and Simvastatin Combination for Cardiovascular Events Prevention Trial in Diabetes) has a planned enrollment of 5170 patients, evaluating the preventative benefit of aspirin + statin versus aspirin alone [39]. While none of these trials will address the benefit of aspirin in a mixed clinical population with no-to-few cardiovascular risk factors, they should help decide if these particular populations at-risk for CVD show sufficient benefit to warrant recommendation for aspirin despite the increased bleeding risk. It is important to note that any benefit or harm from aspirin therapy (even if small in magnitude) is important from a public health stand point as the population attributable benefit or risk could still be high given the large number of individuals currently using aspirin for primary CVD prevention.
An alternative approach that may be helpful in determining an individual’s benefit, or lack thereof, from aspirin therapy is personalizing risk assessment with a coronary artery calcium (CAC) score. A recent paper hypothesized that CAC scoring could be used to determine which individuals are most and least likely to benefit from aspirin therapy [40•]. Using data from the Multi-Ethnic Study of Atherosclerosis (MESA), the study estimated the risks and benefits of aspirin in participants stratified by CAC score at baseline of the study. The study showed that individuals with significant plaque in their arteries (coronary artery calcium score ≥100) were estimated to be two to four times more likely to prevent a heart attack with aspirin use than to have a major bleed secondary to aspirin. Conversely, MESA participants with no calcified plaque (coronary artery calcium score = 0) were estimated to be two to four times more likely to suffer a major bleed from aspirin use than to prevent a heart attack with aspirin. These findings were independent of qualification for aspirin by AHA guidelines (Fig. 1).
The risks and benefits of aspirin in 4229 MESA participants stratified by coronary artery calcium score and CHD risk [40•]
Conclusions
Despite a large amount of data, the role of aspirin in primary prevention is currently unclear. Similar to the patient-provider discussion recommended by the recent ACC/AHA cholesterol guidelines [28], a thorough patient-provider discussion concerning the risks and benefits of aspirin is warranted for individuals without known CVD. A more personalized risk assessment using CAC may be beneficial in determining the likelihood of benefit from aspirin but further research is needed before such an approach can be strongly recommended. Fortunately, the results of the four large RCTs that currently underway should be available in the next 2–3 years. Hopefully, they will provide clarity in determining the optimal use of aspirin in the primary prevention of CVD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Barnett HJ. Platelet and coagulation function in relation to thromboembolic stroke. Adv Neurol. 1977;16:45–70.
OLIVA PB. Pathophysiology of acute myocardial infarction, 1981. Ann Intern Med. 1981;94(2):236–50.
Moore S. Platelet aggregation secondary to coronary obstruction. Circulation. 1976;53(3 Suppl):I66–9.
Schrör K. Aspirin and platelets: the antiplatelet action of aspirin and its role in thrombosis treatment and prophylaxis. Semin Thromb Hemost. 1997;23(4):349–56.
Elwood PC, Cochrane AL, Burr ML, Sweetnam PM, Williams G, Welsby E, et al. A randomized controlled trial of acetyl salicylic acid in the secondary prevention of mortality from myocardial infarction. Br Med J. 1974;1(5905):436–40.
Elwood PC, Sweetnam PM. Aspirin and secondary mortality after myocardial infarction. Lancet. 1979;314(8156):1313–5.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86.
Berger JS, Brown DL, Becker RC. Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. Am J Med. 2008;121(1):43–9.
CAST: Randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (chinese acute stroke trial) collaborative group. Lancet 1997; 349(9066):1641-9.
Hennekens CH. Final report on the aspirin component of the ongoing physicians health study. New England J Med. 1989;321(3):129–35. A landmark trial that established aspirin as a potential treatment for the primary prevention of CHD. A 44% reduction in the risk of non-fatal and fatal MI was seen.
Peto R, Gray R, Collins R, Wheatley K, Hennekens C, Jamrozik K, et al. Randomised trial of prophylactic daily aspirin in british male doctors. Br Med J (Clin Res Ed). 1988;296(6618):313–6.
Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The medical research council’s general practice research framework. Lancet 1998; 351(9098):233-41.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial. HOT study group. Lancet. 1998;351(9118):1755–62.
de Gaetano G. Collaborative Group of the Primary Prevention Project. Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Collaborative group of the primary prevention project. Lancet. 2001;357(9250):89–95.
Ridker PM, Cook NR, Lee I-M, Gordon D, Gaziano JM, Manson JE, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. New England J Med. 2005;352(13):1293–304. The Women’s Health Study is the only aspirin trial to include only women. The primary outcome of the trial was negative but the event rate was quite low. A significant reduction in stroke was found as well as a reduction in MI for women age 65 or older.
Belch J, MacCuish A, Campbell I, Cobbe S, Taylor R, Prescott R, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840.
Ogawa H, Nakayama M, Morimoto T, Uemura S, Kanauchi M, Doi N, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134–41.
Fowkes FG, Price JF, Stewart MC, Butcher I, Leng GC, Pell AC, et al. Aspirin for Asymptomatic Atherosclerosis Trialists. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303(9):841–8.
Ikeda Y, Shimada K, Teramoto T, Uchiyama S, Yamazaki T, Oikawa S, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312(23):2510–20. The JPPP study is the most recent trial evaluating aspirin for primary prevention of CVD. The study found that aspirin did not reduce total CVD in a group of older Japanese patient with at least one major CVD risk factor.
U.S. Preventive Services Task Force. Aspirin to prevent cardiovascular disease (CVD) and cancer: consumer guide (draft recommendation). http://www.uspreventiveservicestaskforce.org/Home/GetFileByID/2292. Accessed on September 28, 2015.
Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295(3):306–13.
US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. preventive services task force recommendation statement. Ann Intern Med. 2009;150(6):396–404.
AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation 2002;106:388-91.
Effectiveness-based guidelines for the prevention of CVD in women—2011 update. A guideline from the American Heart Association. Circulation 2011;123:1243-62.
Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Erqou S, Sattar N, et al. Effect of aspirin on vascular and nonvascular outcomes: meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172(3):209–16.
Perk J, De Backer G, Gohlke H, European Association for Cardiovascular Prevention & Rehabilitation (EACPR); ESC Committee for Practice Guidelines (CPG), et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33(13):1635–701.
Eckel RH, Jakicic JM, Ard JD, Miller NH, Hubbard VS, Nonas CA, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. J Am Coll Cardiol. 2014;63:2960–84.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Cutler JA, Sorlie PD, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008;52:818–27.
Mann D, Reynolds K, Smith D, et al. Trends in statin use and low density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–15.
Brugts JJ, Yetgin T, Hoeks SE, Gotto AM, Shepherd J, Westendorp RG, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ. 2009;338:b2376.
Turnbull F. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527–35.
Yeh RW, Sidney S, Chandra M, et al. Population trends in incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–65.
Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356(23):2388–98.
George J, Rapsomaniki E, Pujades-Rodriguez M, Shah AD, Denaxas S, Herrett E, et al. How does cardiovascular disease first present in women and men? Incidence of 12 cardiovascular diseases in a contemporary cohort of 1,937,360 people. Circulation. 2015;CIRCULATIONAHA-114.
Bayer ARRIVE aspirin research study; Available from: http://www.arrive-study.com/EN/study.cfm. Accessed 18 August 2015.
ASPREE Investigator Group. Study design of aspirin in reducing events in the elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials. 2013;36(2):555–64.
ASCEND trial website; Available from: https://www.ctsu.ox.ac.uk/ascend/. Accessed 18 August 2015.
De Berardis G, Sacco M, Evangelista V, Filippi A, Giorda CB, Tognoni G, et al. Aspirin and simvastatin combination for cardiovascular events prevention trial in diabetes (ACCEPT-D): design of a randomized study of the efficacy of low-dose aspirin in the prevention of cardiovascular events in subjects with diabetes mellitus treated with statins. Trials. 2007;8:21.
Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7(3):453–60. This study provided estimates demonstrating that coronary artery calcium may provide patients with personalized risk information to help determine their risk/benefit profile from aspirin therapy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Michael D. Miedema, Joseph Huguelet, and Salim S. Virani declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Miedema, M.D., Huguelet, J. & Virani, S.S. Aspirin for the Primary Prevention of Cardiovascular Disease: In Need of Clarity. Curr Atheroscler Rep 18, 4 (2016). https://doi.org/10.1007/s11883-015-0555-0
Published:
DOI: https://doi.org/10.1007/s11883-015-0555-0