Abstract
Purpose of Review
The purpose of this review is to summarize the evidence from recently published original studies investigating how glutathione S-transferase (GST) gene polymorphisms modify the impact of air pollution on asthma, allergic diseases, and lung function.
Recent Findings
Current studies in epidemiological and controlled human experiments found evidence to suggest that GSTs modify the impact of air pollution exposure on respiratory diseases and allergies. Of the nine articles included in this review, all except one identified at least one significant interaction with at least one of glutathione S-transferase pi 1 (GSTP1), glutathione S-transferase mu 1 (GSTM1), or glutathione S-transferase theta 1 (GSTT1) genes and air pollution exposure. The findings of these studies, however, are markedly different. This difference can be partially explained by regional variation in the exposure levels and oxidative potential of different pollutants and by other interactions involving a number of unaccounted environment exposures and multiple genes.
Summary
Although there is evidence of an interaction between GST genes and air pollution exposure for the risk of respiratory disease and allergies, results are not concordant. Further investigations are needed to explore the reasons behind the discordancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A human adult inhales several thousand liters of air every day, and each breath of air carries a large number of compounds with oxidative potential, including pollens, gaseous pollutants like ozone (O3) and nitrogen dioxide (NO2), and particulate matter (PM). The particles larger than 10 μm diameter (PM10) in inhaled air can be efficiently trapped by the initial clearing processes in the nose and upper airways. However, gaseous pollutants and fine particles less than 2.5 μm diameter (PM2.5) can easily pass through smaller airways and reach the alveoli [1]. Components of traffic-related air pollution (TRAP), such as NO2 and PM2.5, are known to be strong oxidants [2, 3] and are able to generate reactive oxygen species (ROS) [4]. These pollutants promote increased airway oxidation and inflammation [5••]. Gaseous pollutants like O3 and NO2 cause lung damage through oxidative stress, direct oxidative injury, or indirectly by induction of airway inflammation [6].
Epidemiological studies investigating the direct effects of air pollution exposure on asthma, allergic diseases, and lung function have produced inconsistent results. Within a particular population, certain groups of people are more vulnerable to the effects of air pollution exposure than others. This inter-individual variation in measured health effects has been demonstrated even in controlled experimental studies of healthy human participants [5••, 7]. Many possible explanations for this individual variability have been investigated, such as atopy, sex, nutritional status, social stress, and genetic predisposition [8–10].
The oxidative stress metabolism pathway responds to endogenous and exogenous agents. One of the major oxidative response mechanisms is via the glutathione metabolism pathway. This pathway is controlled by genes [11, 12] including the glutathione S-transferases (GSTs). The human GST genes are part of a large gene superfamily located on seven chromosomes [13], and they encode soluble, dimeric enzymes critical for the detoxification of endogenous and exogenous agents via conjugation of reduced glutathione (GSH) [14]. Genetic polymorphisms of these genes directly affect their functional oxidative capacity in lungs and other vital organs. This may confer genetic susceptibility to oxidative stress and result in subsequent allergies, airway inflammation, or even asthma [15]. The enzymatic properties of these transferase enzymes and their unique role in oxidative stress and inflammatory pathways provided a logical hypothesis for studies to investigate interaction with air pollutants [14, 16].
GSTs have been studied as possible effect modifiers of the association between air pollution exposure and respiratory and allergic diseases [17]. Among the numerous GST polymorphisms, three isozymes, glutathione S-transferase theta 1 (GSTT1), glutathione S-transferase mu 1 (GSTM1), and glutathione S-transferase pi 1 (GSTP1), have gained special interest due to their involvement in biological pathways and their role in detoxification of endogenous agents, such as tobacco smoke and air pollution. The null variants of GSTT1 and GSTM1 and ile/val alleles of GSTP1 have been widely studied, and it has been shown that individuals with these variants have different susceptibility to environmental toxicants, including smoke and air pollution exposure [17, 18].
Identifying how genetic factors modify the relationship between TRAP exposure and respiratory diseases and allergies helps in understanding the underlying biological mechanisms, disease pathogenesis, and, most importantly, in identifying individuals at high risk of allergic and respiratory diseases. Identification of high-risk groups provides a better focus for new preventive and/or therapeutic approaches [17, 18]. The last review on this topic was published in 2011 [19••]. Since then, there have been a number of studies published with contradictory results. Hence, we aimed to build on and extend the previous review by examining the most recent evidence on the interaction between GSTs and air pollution exposure on the risk of asthma, allergies, and lower levels of lung function.
Data Syntheses
Influence of GSTP1 Polymorphisms on the Relationship Between TRAP Exposure and Asthma, Allergic Diseases, and Lung Function
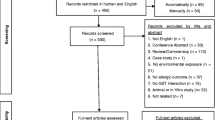
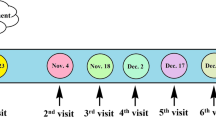
The most commonly studied GST polymorphism regarding TRAP exposure and respiratory and allergic diseases is GSTP1. A common functional polymorphism in the GSTP1 gene is Ile105Val, which occurs in high frequencies in humans. The most common form of GST found in the human lung lining fluid is GSTP1 [20]. In this manuscript, GSTP1 represents the GSTP1 rs1695 (Ile105 ➔ val105) variant unless otherwise specified. Epidemiological studies investigating interactions of GSTP1 for the associations of TRAP exposure and asthma, allergic diseases, allergic sensitization, and lung function are given in Table 1. There have been nine new articles published since the previous systematic review conducted by Minelli and colleagues in 2011 [19••]. The current review contains nine articles which utilized different study types. They are as follows: one long-term cohort study of adults [21••]; two articles which combined six birth cohorts in Europe and North America [22, 23••]; another two articles from the same cohort investigating different levels of air pollution [24, 25•]; one population-based cross-sectional analysis [26]; two cross-sectional studies with small sample sizes [27, 28]; and one cohort with family history of allergic diseases [29•].
There was considerable variation between these studies in terms of air pollution markers investigated, respiratory and allergic disease outcomes explored, and the age group of participants studied. In terms of the air pollution markers investigated, five studies looked at NO2 [24, 27, 28, 29•, 30], four at PM2.5 [22, 24, 27, 30], four at PM10 [21••, 25•, 27, 28], and two at CO [24, 27] exposure. Asthma was the main outcome investigated (five studies) [23••, 24, 25•, 26, 29•], followed by lung function measures (four studies) [21••, 26–28]. Of the nine studies, six were child [22, 23••, 24, 25•, 27, 28], one was adolescent [29•], and two were adult studies [21••, 26]. The majority of studies found some interactions with the GSTP1 polymorphism. Although significant interactions were evident for GSTP1, results were ambiguous.
Studies Finding Evidence of Interaction
A recent study combining six birth cohorts including 5115 children aged 7–8 years found that GSTP1 minor allele carriers (val/val or ile/val) had an increased risk of current or ever asthma when exposed to higher NO2 during the first year of life (OR 1.43 (95% CI 1.03, 1.98) and 1.36 (95% CI 1.08, 1.70) per 10 μg/m3 increase in NO2, respectively) compared to carriers of ile/ile. They also observed similar results with current and ever asthma for minor allele carries of GSTP1 rs1138272 [23••]. Similarly, findings from the Taiwan Children’s Health Study (TCHS) showed that carriers of at least one GSTP1 val allele had an elevated risk of asthma or wheeze when exposed to higher 3-year average community levels of PM2.5 or O3, compared to ile/ile carriers [24]. In another analysis of the TCHS study data using a different statistical approach, authors categorized children into low and high exposure based on ordered subset information gain (OSIG) analysis. They found that children living in low PM10 communities with a GSTP1 ile/ile genotype were more likely to suffer from asthma compared to children with the ile/val or val/val genotype. In contrast, children who lived in high PM10 communities and were carriers of ile/val or val/val genotype had a higher risk of childhood asthma [25•].
The Swiss Study on Air Pollution and Lung Diseases in Adults (SAPALDIA) found that decreased PM10 exposure over 11 years was associated with attenuated decline of FEF25–75% (26.5 ml 95% CI 11.4 to 43.2, per 10 μg m−3 decrease in PM10) in carriers of GSTP1 val/val. This study showed that in low PM10 environments, carriers of val/val had an additional advantage in decreased PM10 related to attenuated lung function decline in terms of FEF25–75% when compared with ile allele carriers [21••]. A study from South Africa (n = 129) reported that short-term PM10 exposure (defined as the 24-h average for the last 3 days) was associated with reduced FEV1 among ile/ile compared to carriers of val. They reported a significant interaction by genotype despite finding no direct association between ile/ile carriage and FEV1 for increasing PM10 levels (β −2.52 ml 95% CI −10.23, 5.20; per 29.4 μg m−3 increase in PM10) [28].
Studies Finding No Evidence of Interaction
In a pooled analysis of the same six birth cohorts as above investigating NO2, PM2.5, PM10, or O3 exposure in the first year of life and the risk of allergic rhinitis at the age of 7–8 years, there was no significant interaction found with GSTP1 polymorphisms [22]. Similar results were found in a recent article from our group investigating the effects of TRAP exposure during the first year of life on the risk of asthma, wheeze, and hay fever at 12 or 18 years [29]. Another study in adults from our group found no significant interactions with GSTP1 polymorphisms for the association between NO2 exposure or proximity to major roads and asthma, wheeze, allergic sensitization, or lower levels of lung function [26]. A recent study in Taiwanese children found no interactions with GSTP1 polymorphisms for the association between PM10 or PM2.5 exposure and lung function or nasal inflammation [27] (Table 1).
Influence of GSTM1 Polymorphisms on the Relationship Between TRAP Exposure and Asthma, Allergic Diseases, and Lung Function
The presence of GSTM1 enzymes in human lung tissues suggests that these enzymes may provide some protection against oxidative stress in the lung [31]. There have been seven new articles published since the last systematic review in 2011 addressing the potential interaction of GSTM1 polymorphisms on the association between air pollution exposures and respiratory or allergic outcomes. They have reported contradictory results. Table 2 describes the major characteristics of these seven studies [21••, 24, 25•, 26–28, 29•].
Studies Finding Evidence of Interaction
A recent study investigating PM2.5 exposure on nasal inflammation, as assessed through nasal lavage, showed that carriers of GSTM1 null had increased numbers of leukocytes (8.52% 95% CI 3.13, 13.92) and neutrophils (9.68% 95% CI 4.51, 14.85%) per 11.5 μg m−3 increase in PM2.5, indicating increased upper airway inflammation when compared with GSTM1 non-null carriers [27]. In a South African study in children, carriers of GSTM1 null had significantly decreased FEV1 compared to GSTM1 non-null carriers when exposed to increased SO2 [28]. Conversely, the same study [28] reported that carriers of GSTM1 non-null with elevated exposure to PM10 had reduced FEV1, while GSTM1 null carriers with elevated exposure to PM10 had no association with FEV1 levels. Similar results were demonstrated in a study from our group, with GSTM1 non-null carriers having an increased risk of asthma at 12 years of age with greater exposure to roads within a 100-m radius of the residential address during the first year of life, while GSTM1 null showed no association with the same exposure [29•].
Studies Finding No Evidence of Interaction
The SPALDIA cohort found no significant interaction between GSTM1 polymorphisms and reduction in PM10 over 10 years and attenuated lung function in adults [21••]. Two papers from the TCHS found no significant interaction between GSTM1 polymorphisms and air pollution exposure for the risk of asthma [24, 25•]. Similar results were found in one of our studies in Australian adults for the association of air pollution exposure and asthma, allergic sensitization, or lung function [26] (Table 2).
Influence of GSTT1 Polymorphisms on the Relationship Between TRAP Exposure and Asthma, Allergic Diseases, and Lung Function
The frequency of the GSTT1 null genotype is highly variable based on ethnicity, with higher null allele frequencies among Asians (50–60%) compared with Caucasians (10–20%) [32]. It has been shown that GSTT1 is involved in detoxification of polycyclic aromatic hydrocarbons (PAHs), which are known components of TRAP [33]. Table 3 describes the new studies (since Minelli 2011 [19••]) investigating the interaction between GSTT1 polymorphisms and TRAP exposure on the risk of asthma, allergic diseases, allergic sensitization, and lung function [8, 21••, 24, 25•, 26, 29•].
Studies Finding Evidence of Interaction
Two recent studies from our group found significant interactions between GSTT1 polymorphisms and air pollution for the risk of respiratory diseases and allergies [26, 29•]. The first study on children at a high risk of developing allergic diseases found a significant interaction between GSTT1 polymorphisms and TRAP exposure in the first year of life on the risk of asthma or wheeze at the age of 12 years, with GSTT1 null carriers having an increased risk [29•]. Our other study in middle-aged adults found that increased NO2 exposure was associated with increased risk of any house dust mite (HDM) or cat allergen sensitization in GSTT1 null carriers. In the same study using an alternative definition of TRAP exposure, living less than 200 m from a major road, we found a similar association between TRAP exposure and increased risk of sensitization and current asthma in GSTT1 null carriers [26].
Studies Finding No Evidence of Interaction
However, another four studies investigating air pollution exposure and asthma or lung function or nasal inflammation found no significant interaction with GSTT1 polymorphisms [21••, 24, 25•, 27] (Table 3).
Discussion
The 2011 review by Minelli et al. [19••] reported some evidence to support the presence of oxidative stress gene air pollution interactions and respiratory outcomes. However, evidence was limited for certain genes like GSTT1. Further, they suggested carrying out larger studies with accurate air pollution assessment. In the current review, we identified nine further studies to update this evidence. Of these, four addressed the criteria outlined by Minelli et al. for further investigation in this area. These four large studies used advanced air pollution assessment tools and comparatively large sample sizes [21••, 22, 23••, 26]. Tellingly, three of these high-quality studies showed significant GST polymorphism/air pollution interactions [21••, 23••, 26].
Publications since 2009 provide support for interactions between polymorphisms of GSTP1 and air pollution exposure, and there is some evidence that different alleles (ile or val) may respond to high and low air pollution levels in different ways. Two recent studies showed that GSTT1 null interacted significantly with TRAP exposures [26, 29•]. The findings associated with GSTM1 are not clear. One study identified GSTM1 null as a risk allele, while another found that GSTM1 non-null was associated with increased risk [27, 28]. Although there are some heterogeneous results, eight of the nine studies found at least one significant GST gene polymorphism interaction between air pollution exposure and lung health outcomes.
Evidence from Controlled Human Studies
Controlled human exposure studies exploring interactions by GST polymorphisms on the association between air pollution exposure and respiratory disease and allergies are concordant with and ratify the findings of observational studies. It is important to note that controlled human studies are often limited by ethical and practical concerns and usually have smaller sample sizes compared with observational studies. Recent studies of atopic individuals from Canada showed that controlled co-exposure to diesel exhaust and allergens is associated with augmented allergic inflammation, increased IL-5, and activation of cytotoxic CD69+ T cells in bronchoscopic lavage fluid, but only in individuals with the GSTT1 null genotype [5••]. Using the same participants, a further study showed that in atopic individuals, co-exposure to diesel exhaust and allergens caused a significant decrease in FEV1 2 h post exposure in GSTT1 null compared to GSTT1 non-null carriers [34]. Neither of these studies found significant interactions for polymorphisms of GSTM1. Interestingly, another recent study in healthy individuals found no association between controlled exposure to diesel exhaust and ozone (O3) and subsequent FEV1 in those with GSTM1 null genotype [35]. A 2004 study by Gilliland and colleagues showed that co-exposure to diesel exhaust and ragweed allergen in ragweed-sensitized individuals resulted in enhanced IgE and histamine level in those with GSTP1 ile/ile or GSTM1 null genotype, but not in GSTT1 null carriers [7].
Mechanistic Perspectives
Exposure to very high levels of air pollution, such as those experienced in the mega cities of China and developing countries, is associated with histologic changes in the nasal mucosa, direct irritant, and inflammatory effects on airway neuroreceptors and epithelium [36, 37]. However, these extreme levels of air pollution do not occur in Europe, North America, or Australia. Despite these regions having lower levels of exposure, evidence suggests these levels can still have an impact on asthma and allergies [26]. Hence, other mechanisms may have a vital role in the determination of airway diseases in countries with low air pollution levels. The biological mechanisms by which air pollution exposure at low levels has an impact may be related to inter-individual variation in the biological response to these pollutants. The UK’s committee on the medical effects of air pollutants proposed the following mechanisms for the effects of air pollution exposure on asthma and allergic diseases: oxidative stress and damage, airway remodeling, inflammatory pathways and immunological responses, and enhancement of respiratory sensitization to aeroallergens [38]. However, the exact mechanisms explaining the association of air pollution exposure and chronic airway diseases have not been fully elucidated [39].
In experimental studies, oxidative stress has been identified as one of the major pathways underlying the adverse health effects of air pollution, including allergies and chronic respiratory diseases [40]. Oxidative stress arises from an imbalance between prooxidant and antioxidant defenses [41]. Genetic susceptibility is likely to play an important role in the response to air pollution and the development of allergies and chronic respiratory diseases. The mechanism of air pollution exposure on the occurrence and persistence of respiratory diseases and allergies is best described by the oxidative stress hypothesis. Phase II enzymes of GSTs are involved in catalyzing the glutathione conjugation of a variety of electrophilic xenobiotics, ranging from environmental toxins and carcinogens to drugs used in the treatment of cancer [42].
ROS can be generated after exposure to triggers such as components of TRAP (NO2 or PM2.5). Exposure to these components can then lead to an influx of inflammatory cells, such as neutrophils, into the airways. Recruitment of these inflammatory cells capable of releasing large quantities of free radicals causes a second wave of oxidative stress. In the absence of any foreign invading agent to react with, these free radicals subsequently attack airway tissues and cause cell injury [43].
To regulate the oxidative stress generated by numerous oxidative agents encountered by the lungs, the pulmonary system has enzymatic (e.g., superoxide dismutase, catalase, and glutathione peroxidase) and non-enzymatic antioxidant systems [44]. These systems are capable of buffering a wide range of environmental oxidants and allow the lungs to function efficiently [45]. The glutathione peroxidase antioxidant system has been investigated in relation to air pollution exposure and asthma and allergic disease risk, because it helps to maintain intracellular glutathione levels. The intracellular glutathione (GSH), a tripeptide thiol, is critically important in maintaining intracellular oxidant balance [46]. After initiation of an oxidative reaction, ROS are reduced (and inactivated) through oxidation of GSH into glutathione disulfide or oxidized glutathione (GSSG) [45, 47]. A large number of epoxides derived from environmental toxicants are detoxified by GSTs. These include PAHs and styrene by the actions of cytochromes P450 in the liver and lung. The PAHs are common chemical components of cigarette smoke and traffic exhaust, and these compounds represent an ever present threat to health [42].
Why Heterogeneous Results in Studies?
Although both observational and controlled human studies show interactions between GST polymorphisms and air pollution exposure related to respiratory diseases and allergies, the results are highly heterogeneous. This can be attributed to a number of reasons: (1) The GST variants (GSTP1, GSTM1, and GSTT1) commonly used in studies explain only a small proportion of the complex regulation of the oxidative pathway which is regulated by many genes. These commonly investigated genetic variants may explain only a small portion of the genes involved in regulating oxidative stress and may be confounded by other interactions involving a number of environment exposures and multiple genes not accounted for in the current studies. (2) Accurate air pollution exposure assessment in population-based studies is challenging, and these issues have been discussed in detail in the literature previously [48]. The studies included in this review used different approaches to determine air pollution exposure, which ranged from simple proxies of air pollution exposure (e.g., proximity to roads) to more complex land use regression models. Each of these models has their own strengths and limitations. Polluted air, for example measured by traffic exhaust, is a complex mixture of pollutants such as gases, PAHs, and PM. However, most of the studies measured only a limited number of pollutants in this complex mixture. The diversity and complexity of the pollutants in different regions can be markedly different based on different emission sources. Additionally, the oxidative potential of some pollutants, like PM, has been reported to vary both between and within regions [49]. Most importantly, it is not clear how these specific antioxidant enzymes respond to a complex mixture of chemicals because studies have only investigated them individually. (3) Gene-environmental interaction studies require an adequate sample size in order to have sufficient power to detect associations. Generally, it is accepted that gene-environmental interaction studies require a sample size at least four times larger than that required for the detection of a main effect of a similar size [50]. Some of the studies are undoubtedly underpowered to detect interactions between GSTs and air pollution. Additionally, most of the observational studies investigating GST and air pollution exposure were not primarily designed to investigate such interactions. There is a need for studies specifically designed to investigate these interactions.
When considering GSTP1 polymorphisms, the results to date have been inconsistent in terms of the risk allele. Some studies showed an increased risk related to the val allele and others reported ile as the risk allele. A study by Su et al. in 2013 [25•] provides an explanation for these heterogeneous associations. They found that children carrying the homozygous ile variant living in low PM10 areas had a higher risk of asthma than those with ile/val or val/val variants. In contrast, children living in high PM10 areas with ile/val or val/val variants had a higher risk of asthma compared to the homozygous ile variant [25•]. This provides some evidence that alleles of GSTP1 depend on the level of exposure. It can be further hypothesized that genetic variants may respond to air pollution in different ways based on differential oxidative capacities of the air pollution mixture in different areas [49]. Even though they have not specifically investigated GST polymorphism-air pollution interactions, a recent Canadian study showed that city level differences in the oxidative potential of PM2.5 modified the association between PM2.5 exposure and acute respiratory illnesses, even at low PM2.5 concentrations [51]. This may further help to explain the inconsistent findings.
Conclusions
Recent observational and controlled human studies provide evidence for interactions between GST gene polymorphisms and air pollution in studies investigating the effects of air pollution exposure on respiratory diseases and allergies. There are, however, some conflicting findings which may be due to the complexity of and different oxidative potential of the air pollution mixture in different areas/regions or due to other currently unstudied genes which contribute to the detoxification of air pollutants in humans. Appreciation of the heterogeneous effects by pollutants may lead to further investigation of the pathophysiologic mechanisms behind these associations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Xing Y-F, Xu Y-H, Shi M-H, Lian Y-X. The impact of PM2.5 on the human respiratory system. J Thorac Dis. 2016;8(1):E69–74. doi:10.3978/j.issn.2072-1439.2016.01.19.
Last JA, Sun WM, Witschi H. Ozone, NO, and NO2: oxidant air pollutants and more. Environ Health Perspect. 1994;102 Suppl 10:179–84.
Nawrot TS, Kuenzli N, Sunyer J, Shi T, Moreno T, Viana M, et al. Oxidative properties of ambient PM2.5 and elemental composition: heterogeneous associations in 19 European cities. Atmos Environ. 2009;43(30):4595–602. doi:10.1016/j.atmosenv.2009.06.010.
Velsor LW, Postlethwait EM. NO2-induced generation of extracellular reactive oxygen is mediated by epithelial lining layer antioxidants. Am J Physiol. 1997;273(6 Pt 1):L1265–75.
•• Carlsten C, Blomberg A, Pui M, Sandstrom T, Wong SW, Alexis N, et al. Diesel exhaust augments allergen-induced lower airway inflammation in allergic individuals: a controlled human exposure study. Thorax. 2016;71(1):35–44. doi:10.1136/thoraxjnl-2015-207399. This controlled human exposure study demonstrated that exposure to diesel exhaust augments allergen-induced lower airway inflammation in allergic individuals with GSTT1 null polymorphism.
Olivieri D, Scoditti E. Impact of environmental factors on lung defences. Eur Respir Rev. 2005;14(95):51–6.
Gilliland FD, Li Y-F, Saxon A, Diaz-Sanchez D. Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet. 2004;363(9403):119–25. doi:10.1016/S0140-6736(03)15262-2.
Chen E, Schreier HM, Strunk RC, Brauer M. Chronic traffic-related air pollution and stress interact to predict biologic and clinical outcomes in asthma. Environ Health Perspect. 2008;116(7):970–5. doi:10.1289/ehp.11076.
Gordian ME, Haneuse S, Wakefield J. An investigation of the association between traffic exposure and the diagnosis of asthma in children. J Expo Sci Environ Epidemiol. 2006;16(1):49–55. doi:10.1038/sj.jea.7500436.
Sienra-Monge JJ, Ramirez-Aguilar M, Moreno-Macias H, Reyes-Ruiz NI, Del Rio-Navarro BE, Ruiz-Navarro MX, et al. Antioxidant supplementation and nasal inflammatory responses among young asthmatics exposed to high levels of ozone. Clin Exp Immunol. 2004;138(2):317–22. doi:10.1111/j.1365-2249.2004.02606.x.
Allen RG, Tresini M. Oxidative stress and gene regulation. Free Radic Biol Med. 2000;28(3):463–99. doi:10.1016/S0891-5849(99)00242-7.
Weiss ST. Lung function and airway diseases. Nat Genet. 2010;42(1):14–6.
Strange RC, Spiteri MA, Ramachandran S, Fryer AA. Glutathione-S-transferase family of enzymes. Mutat Res. 2001;482(1–2):21–6. doi:10.1016/S0027-5107(01)00206-8.
Hayes JD, Strange RC. Glutathione S-transferase polymorphisms and their biological consequences. Pharmacology. 2000;61(3):154–66. doi:10.1159/000028396.
Piacentini S, Polimanti R, Simonelli I, Donno S, Pasqualetti P, Manfellotto D, et al. Glutathione S-transferase polymorphisms, asthma susceptibility and confounding variables: a meta-analysis. Mol Biol Rep. 2013;40(4):3299–313. doi:10.1007/s11033-012-2405-2.
Romieu I, Moreno-Macias H, London SJ. Gene by environment interaction and ambient air pollution. Proc Am Thorac Soc. 2010;7(2):116–22. doi:10.1513/pats.200909-097RM.
Holloway JW, Savarimuthu Francis S, Fong KM, Yang IA. Genomics and the respiratory effects of air pollution exposure. Respirology. 2012;17(4):590–600. doi:10.1111/j.1440-1843.2012.02164.x.
Hosgood Iii HD, Berndt SI, Lan Q. GST genotypes and lung cancer susceptibility in Asian populations with indoor air pollution exposures: A meta-analysis. Mutat Res. 2007;636(1–3):134–43. doi:10.1016/j.mrrev.2007.02.002.
•• Minelli C, Wei I, Sagoo G, Jarvis D, Shaheen S, Burney P. Interactive effects of antioxidant genes and air pollution on respiratory function and airway disease: a HuGE review. Am J Epidemiol. 2011;173(6):603–20. doi:10.1093/aje/kwq403. Systematic review that synthesized evidence based on literature published until 2009 related to interactions of oxidative stress gene polymorphisms on air pollution exposure and airway diseases.
Kellen E, Hemelt M, Broberg K, Golka K, Kristensen VN, Hung RJ, et al. Pooled analysis and meta-analysis of the glutathione S-transferase P1 Ile 105Val polymorphism and bladder cancer: a HuGE-GSEC review. Am J Epidemiol. 2007;165(11):1221–30. doi:10.1093/aje/kwm003.
•• Curjuric I, Imboden M, Schindler C, Downs SH, Hersberger M, Liu SLJ, et al. HMOX1 and GST variants modify attenuation of FEF25-75% decline due to PM10 reduction. Eur Respir J. 2009;35(3):505–14. doi:10.1183/09031936.000443-2009. Using data from a longitudinal cohort, this study demonstrated the effects of reduced PM 10 over 11 years on lung function change in relation to GST polymorphisms.
Fuertes E, Brauer M, MacIntyre E, Bauer M, Bellander T, von Berg A, et al. Childhood allergic rhinitis, traffic-related air pollution, and variability in the GSTP1, TNF, TLR2, and TLR4 genes: results from the TAG Study. J Allergy Clin Immunol. 2013;132(2):342-52.e2. doi:10.1016/j.jaci.2013.03.007.
•• MacIntyre EA, Brauer M, Melen E, Bauer CP, Bauer M, Berdel D, et al. GSTP1 and TNF Gene variants and associations between air pollution and incident childhood asthma: the traffic, asthma and genetics (TAG) study. Environ Health Perspect. 2014;122(4):418–24. doi:10.1289/ehp.1307459. Combining six birth cohort studies and using advanced air pollution modeling, this study demonstrated how early life exposure to air pollutants is modified by GST polymorphisms.
Hwang B-F, Young L-H, Tsai C-H, Tung K-Y, Wang P-C, Su M-W, et al. Fine particle, ozone exposure, and asthma/wheezing: effect modification by glutathione S-transferase P1 polymorphisms. PLoS One. 2013;8(1):e52715. doi:10.1371/journal.pone.0052715.
• Su MW, Tsai CH, Tung KY, Hwang BF, Liang PH, Chiang BL, et al. GSTP1 is a hub gene for gene-air pollution interactions on childhood asthma. Allergy. 2013;68(12):1614–7. doi:10.1111/all.12298. This study reported the effects of differential exposure levels of PM 10 on childhood asthma in children with GSTP1 polymorphism.
Bowatte G, Lodge CJ, Knibbs LD, Lowe AJ, Erbas B, Dennekamp M, et al. Traffic-related air pollution exposure is associated with allergic sensitization, asthma, and poor lung function in middle age. J Allergy Clin Immunol. 2016. doi:10.1016/j.jaci.2016.05.008.
Chen B-Y, Chen C-H, Chuang Y-C, Kim H, Honda Y, Chiang H-C, et al. Schoolchildren’s antioxidation genotypes are susceptible factors for reduced lung function and airway inflammation caused by air pollution. Environ Res. 2016;149:145–50. doi:10.1016/j.envres.2016.05.007.
Reddy P, Naidoo RN, Robins TG, Mentz G, Li H, London SJ, et al. GSTM1 and GSTP1 gene variants and the effect of air pollutants on lung function measures in South African children. Am J Ind Med. 2012;55(12):1078–86. doi:10.1002/ajim.22012.
• Bowatte G, Lodge CJ, Lowe AJ, Erbas B, Dennekamp M, Marks GB, et al. Do variants in GSTs modify the association between traffic air pollution and asthma in adolescence? Int J Mol Sci. 2016;17(4):485. doi:10.3390/ijms17040485. First epidemiological study to report the significant effects of GSTT1 polymorphisms for the association of air pollution exposure and asthma/wheeze.
MacIntyre EA, Carlsten C, MacNutt M, Fuertes E, Melen E, Tiesler CMT, et al. Traffic, asthma and genetics: combining international birth cohort data to examine genetics as a mediator of traffic-related air pollution’s impact on childhood asthma. Eur J Epidemiol. 2013;28(7):597–606. doi:10.1007/s10654-013-9828-5.
Mainwaring GW, Williams SM, Foster JR, Tugwood J, Green T. The distribution of theta-class glutathione S-transferases in the liver and lung of mouse, rat and human. Biochem J. 1996;318(Pt 1):297–303.
Raimondi S, Paracchini V, Autrup H, Barros-Dios JM, Benhamou S, Boffetta P, et al. Meta- and pooled analysis of GSTT1 and lung cancer: a HuGE-GSEC review. Am J Epidemiol. 2006;164(11):1027–42. doi:10.1093/aje/kwj321.
Yang F, Xiong J, Jia X-E, Gu Z-H, Shi J-Y, Zhao Y, et al. GSTT1 deletion is related to polycyclic aromatic hydrocarbons-induced DNA damage and lymphoma progression. PLoS One. 2014;9(2):e89302. doi:10.1371/journal.pone.0089302.
Zhang X, Hirota JA, Yang C, Carlsten C. Effect of GST variants on lung function following diesel exhaust and allergen co-exposure in a controlled human crossover study. Free Radic Biol Med. 2016;96:385–91. doi:10.1016/j.freeradbiomed.2016.04.202.
Madden MC, Stevens T, Case M, Schmitt M, Diaz-Sanchez D, Bassett M, et al. Diesel exhaust modulates ozone-induced lung function decrements in healthy human volunteers. Part Fibre Toxicol. 2014;11(1):1–10. doi:10.1186/s12989-014-0037-5.
Calderón-Garcidueñas L, Rodríguez-Alcaraz A, Villarreal-Calderón A, Lyght O, Janszen D, Morgan KT. Nasal epithelium as a sentinel for airborne environmental pollution. Toxicol Sci. 1998;46(2):352–64. doi:10.1093/toxsci/46.2.352.
Shusterman D. The effects of air pollutants and irritants on the upper airway. Proc Am Thorac Soc. 2011;8(1):101–5. doi:10.1513/pats.201003-027RN.
Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, et al. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology. 2012;17(6):887–98. doi:10.1111/j.1440-1843.2012.02195.x.
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–92. doi:10.1016/s0140-6736(14)60617-6.
Huang SK, Zhang Q, Qiu Z, Chung KF. Mechanistic impact of outdoor air pollution on asthma and allergic diseases. J Thorac Dis. 2015;7(1):23–33. doi:10.3978/j.issn.2072-1439.2014.12.13.
Bowler RP, Crapo JD. Oxidative stress in allergic respiratory diseases. J Allergy Clin Immunol. 2002;110(3):349–56. doi:10.1067/mai.2002.126780.
Hayes JD, Flanagan JU, Jowsey IR. Glutathione transferases. Annu Rev Pharmacol Toxicol. 2005;45:51–88. doi:10.1146/annurev.pharmtox.45.120403.095857.
Kelly F. Oxidative stress: its role in air pollution and adverse health effects. Occup Environ Med. 2003;60(8):612–6.
Rahman K. Studies on free radicals, antioxidants, and co-factors. Clin Interv Aging. 2007;2(2):219–36.
Holguin F. Oxidative stress in airway diseases. Ann Am Thorac Soc. 2013;10(Suppl):S150–7. doi:10.1513/AnnalsATS.201305-116AW.
Rahman I, MacNee W. Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J. 2000;16(3):534–54.
Lodovici M, Bigagli E. Oxidative stress and air pollution exposure. J Toxicol. 2011;2011:487074. doi:10.1155/2011/487074.
Brauer M. How much, how long, what, and where: air pollution exposure assessment for epidemiologic studies of respiratory disease. Proc Am Thorac Soc. 2010;7(2):111–5.
Künzli N, Mudway IS, Götschi T, Shi T, Kelly FJ, Cook S, et al. Comparison of oxidative properties, light absorbance, and total and elemental mass concentration of ambient PM(2.5) collected at 20 European sites. Environ Health Perspect. 2006;114(5):684–90. doi:10.1289/ehp.8584.
Smith PG, Day NE. The design of case-control studies: the influence of confounding and interaction effects. Int J Epidemiol. 1984;13(3):356–65.
Weichenthal SA, Lavigne E, Evans GJ, Godri Pollitt KJ, Burnett RT. Fine particulate matter and emergency room visits for respiratory illness. Effect modification by oxidative potential. Am J Respir Crit Care Med. 2016;194(5):577–86. doi:10.1164/rccm.201512-2434OC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
The two studies that the authors are part of are approved by the Human Research Ethics Committee at the University of Melbourne (Human Research Ethics Committee No. 040375), Mercy Maternity Hospital Ethics Committee (HREC nos. R07/20 and R88/06), and Royal Children’s Ethics Committee (HREC: 28035). All the participants in these two studies provided written informed consent.
Additional information
Melanie C. Matheson, and Shyamali C. Dharmage are equal senior authors.
This article is part of the Topical Collection on Allergies and the Environment
Melanie C. Matheson and Shyamali C. Dharmage contributed equally to this work.
Rights and permissions
About this article
Cite this article
Bowatte, G., Lodge, C.J., Perret, J.L. et al. Interactions of GST Polymorphisms in Air Pollution Exposure and Respiratory Diseases and Allergies. Curr Allergy Asthma Rep 16, 85 (2016). https://doi.org/10.1007/s11882-016-0664-z
Published:
DOI: https://doi.org/10.1007/s11882-016-0664-z