Abstract
Proteomics encompasses a variety of approaches unraveling both the structural features, post-translational modifications, and abundance of proteins. As of today, proteomic studies have shed light on the primary structure of about 850 allergens, enabling the design of microarrays for improved molecular diagnosis. Proteomic methods including mass spectrometry allow as well to investigate protein-protein interactions, thus yielding precise information on critical epitopes on the surface of allergens. Mass spectrometry is now being applied to the unambiguous identification, characterization, and comprehensive quantification of allergens in a variety of matrices, as diverse as food samples and allergen immunotherapy drug products. As such, it represents a method of choice for quality testing of allergen immunotherapy products.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proteomics, defined as the in-depth analysis of protein repertoires within a given species, organ, or organelle, has considerably extended in the last few years our knowledge of an ever expanding number of proteins [1]. As a result, more than 550,000 proteins have now been described in the literature, from a total of more than 63 million protein sequence entries currently referenced in public databases [2]. Whereas proteomic methods are broadly applied to the deciphering of numerous physiological and pathophysiological mechanisms [3–7], we focus in the present review on their current concrete applications to the field of allergy [8••]. Food and respiratory allergies as of today represent a major public health burden, with an increasing prevalence [9–12, 13•]. In this context, proteomics is of great interest for the identification and structural characterization of allergens involved in such allergies. Also, immune epitopes derived from such allergens can be defined using technologies such as X-ray diffraction or hydrogen deuterium exchange (HDX) mass spectrometry (MS). Moreover, proteomics can provide semi-quantitative or quantitative information regarding those molecules, for example, within food or environmental samples, as well as pharmaceutical-grade natural extracts used for allergen-specific immunotherapy (AIT). Proteomic approaches are also useful for the in vitro diagnostic of allergen sensitization and further for searching biomarkers of efficacy for AIT. Herein, we review each of those applications of proteomics to allergen identification, characterization, quantification, and quality testing, as well as the discovery of biomarkers of AIT efficacy.
Proteomics Dedicated to Allergen Identification
Identification is critical for the detection of allergens not only in food and beverages but also within AIT products from the biopharmaceutical industry. Hundreds of known allergens are proteins or glycoproteins [14••]. Those allergens are commonly identified based on their IgE reactivity and subsequently classified as minor or major allergens on the basis of the prevalence of IgE sensitization to them [15]. In the early 1980s, the combination of modern biochemistry with molecular biology gave rise to the identification of an exponential number of new allergens that were further purified, sequenced, and expressed as recombinant proteins. Those allergens originating from either animal dander, foods, mites, pollens, whole insects, or derived venoms and yeasts were initially partially sequenced by Edman degradation to identify the first 10 to 30 amino acids, thus subsequently allowing to perform gene cloning and sequencing [16–19]. Within the last two decades, MS and most particularly tandem MS (MS/MS) have progressively and advantageously replaced Edman degradation in order to obtain entire allergen sequences [20–26]. MS also contributed to the elucidation and detection of a number of post-translational modifications such as N-glycosylation, among which some important cross-reactive carbohydrate determinants encompassing for instance the galactose-alpha-1,3-galactose motif [21, 27–34].
Immunological methods have been the gold standard for allergen identification or detection and are routinely used to this aim in many laboratories performing dot blots or western blots [35, 36]. The selectivity of the latter methods relies upon antibody specificity, associated with either a polyclonal or preferably a monoclonal antibody (mAb). However, the production of suitable mAbs is cumbersome and difficult since both the specificity and the stability of the obtained product are never guaranteed a priori. Moreover, matrix interference, cross-reactivity, and other molecules such as antibodies or lectins can interfere or abolish the detection of the allergen of interest [37]. Aptamers (i.e., oligonucleotides or peptides) selected for their ability to bind to a specific target molecule represent an attractive alternative to mAbs, but this technology is currently not widely available [38]. In this context, MS carries significant advantages by providing a virtually reagent-free allergen identification, based on the acquisition of MS/MS data from the allergen of interest prior to an in silico comparison with protein sequence databases. For instance, a single multiplexed MS method can specifically detect egg, milk, and soy allergens, with a level of detection ranging from 0.1 to 2 μg/g of food sample [39–41, 42•].
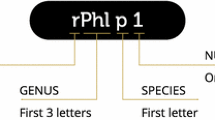
In the last few years, allergen identification has benefited from combined approaches associating proteomics with transcriptomics and IgE immunoblotting. Bi-dimensional polyacrylamide gel electrophoresis (2D-PAGE) combined with MS is a method of choice to discover new allergens, especially major allergens [43–45]. Briefly, the proteome from a biological sample (e.g., aqueous mite or pollen extract) is first subjected to isoelectric focusing (i.e., first dimension) to fractionate proteins based on their charge, with further separation according to molecular masses (i.e., second dimension). As a result, hundreds of proteins are usually resolved as small spots within the polyacrylamide gel, which can further be transferred to a membrane by western blotting. The membrane is then revealed by sera from allergic patients, highlighting IgE reactive spots subsequently characterized by MS/MS. When limited or no data are available in protein databases, the use of transcriptomic information (i.e., data from RNA sequencing) is highly valuable to identify new allergens of clinical importance. This combined approach based on omics technologies was successfully implemented by us and others to characterize allergen extracts obtained from either house dust mites or pollens from tropical grasses or ragweed [46–48]. Moreover, we applied MS as a release testing identification method to confirm that a drug product made of a mix of five grass pollens contains in a consistent manner grass pollen group 1 major allergens (namely, Ant o 1, Dac g 1, Lol p 1, Phl p 1, and Poa p 1) originating from each of the selected grass species [31].
Unraveling Allergen Epitopes Through Proteomics
Understanding the allergen/antibody binding interaction (as well as potential cross-reactivity) through the mapping of epitopes represents an essential component in the development of both immunoassays as well as AIT drug products [49–51]. To this aim, complex methodologies such as nuclear magnetic resonance spectroscopy (NMR) or X-ray diffraction were successfully implemented to characterize a small number of allergen epitopes [52–55]. Antibodies raised against allergen-derived peptides were also successfully used to compete with the patients’ IgEs in binding to the native allergen, thereby identifying immune epitopes [56]. Broader information can also be obtained through the simple production and testing of synthetic overlapping peptides that cover the entire allergen sequence [57–59]; however, this approach fails to identify most conformational epitopes [60].
HDX-MS can be used to locate linear and conformational epitopes in a manner that complements classical structural approaches [61–63]. HDX-MS probes the solvent accessibility of proteins in their native state based on the rate of exchange of backbone amide hydrogens (H) against deuterium (D). In this regard, the binding of a mAb to a target allergen reduces the solvent accessibility of the epitope leading to a mass reduction in the complex compared to the free allergen. The technology has been established several years ago and is now available on fully automated instruments in order for instance to develop and compare biologicals such as therapeutic mAbs [64].
In our hands, we have used HDX-MS to identify an epitope specifically recognized by a Der p 1-specific mAb (namely, 5H8 from Indoor Biotechnologies, Cardiff, UK). Briefly, Der p 1-5H8 complexes were obtained at 30 °C prior to labeling with a deuterated PBS buffer. Over the time course of the experiment (ranging from 1 min to 1 h), aliquots of the complex were recovered, quenched, and dissociated prior to MS analysis. Our HDX-MS data confirmed that the 5H8 mAb recognizes a conformational epitope located in the B domain of Der p 1 (Fig. 1a), composed of segments Thr48-Ala57, Tyr82-Tyr93, and the Ser102-Ile113 loop. An equivalent epitope was identified by X-ray crystallography (Fig. 1b), in agreement with the HDX-MS approach [65–67]. Such data demonstrate that conformational epitopes can be identified by measuring the change in deuterium uptake between the free and bound allergen. Compared to X-ray crystallography, HDX-MS results are of medium resolution (i.e., 8–10 residues) but the technology requires low quantities of biological material (i.e., 5–10 pmols per injection) and provides a rapid (1 to 2 days) and efficient way to map epitopes.
Comparison of the Der p 1 epitope targeted by Fab 5H8 as elucidated by a HDX-MS and b X-ray crystallography. The binding of Fab 5H8 reduces the solvent accessibility of three regions within the B domain of the Der p 1 allergen, covered by peptides Tyr48-Ala57 (red), Tyr82-Tyr93 (green), and Ser102-Ile113 (blue). Equivalent regions were identified by X-ray crystallography. The amino acid residues involved in hydrogen bonding upon complex formation are also displayed. An excellent agreement between the two epitope mapping strategies was observed
Proteomics for Allergy Diagnostic
Proteomic approaches can also be used to perform molecular allergy diagnostic. On a routine basis, the anamnesis combining symptom assessment and skin prick testing data is the main cornerstone of allergy diagnostic [68–70]. The latter relies as well upon specific IgE in vitro binding assays, making use of microarrays of purified allergens as part of a “component resolved diagnostic” in order to improve routine clinical care. As of today, microarrays carrying over 100 distinct allergens offer the opportunity to characterize patients’ IgE sensitization patterns to multiple allergens in a single analysis with small blood volumes and distinguish true sensitization from cross-reactivity [71, 72•, 73]. The clinical interest of such technologies, including point-of-care or near-patients diagnostics, is however currently limited by the availability of highly purified, well-characterized, and stable allergens. In the near future, proteomic-based miniaturized devices allowing a more accurate, faster, and simpler diagnostic of allergic sensitization will likely contribute to the emergence of personalized AIT tailored for individual allergic patients [74•].
In this context, new nanoscopic scale biosensors are being developed to assess patient’s circulating IgEs from as little as 50 μL of blood sample. For instance, the abioscope apparatus (Abionic SA, Lausanne, Switzerland) is a novel small footprint device that allows to quantify allergen-specific IgEs (e.g., directed to either Can f 1, Der p 1, Fel d 1, or Phl p 1) in 5 min, thanks to modern nanofluidic biosensors that enhance molecular interactions and reduce incubation time from hours to minutes. Results obtained with this technology compare to the ones generated using the Immunocap technology (Thermo Fischer Scientific, Uppsala, Sweden) [71].
Proteomics to Document Pharmaceutical Quality
AIT was shown to restore appropriate immunoregulatory responses in allergic patients, thereby alleviating clinical symptoms and reducing the uptake of symptomatic drugs [75–82]. As of today, AIT treatments rely upon standardized allergen extracts obtained from natural source materials (e.g., mites, pollens) produced and tested as per health authorities recommendations [83, 84]. The guideline on allergen products (CHMP/BWP/304831/2007) provides European manufacturers with recommendations in terms of quality for the production of allergen products intended for the diagnostic or treatment of allergic diseases [85]. Importantly, health authorities request a specific identity test for the allergenic source materials used for drug manufacturing. To address this topic, electrophoretic (PAGE) or immunological (western blotting, enzyme-linked immunosorbent assay (ELISA)) methods are frequently performed, even though the specificity of those approaches is not always fully documented. We and others have shown that a fast and simple MS acquisition can identify and distinguish several pollen source materials [86].
Biotyping based on matrix-assisted laser desorption/ionization time-of-flight (MALDI-ToF) MS has been originally applied for the reliable and swift identification of pathogenic microorganisms in clinical and veterinary microbiology [87–89]. Using this straightforward methodology, we could identify, in a reproducible manner, source materials from multiple species including insect venoms (i.e., Apis melifera, Poliste spp., Vespula spp.), molds (i.e., Alternaria alternata, Aspergillus fumigatus, Aspergillus niger, Cladosporium herbarum, Cladosporium IHEM, Penicillium notatum), grass and cereal pollens (i.e., Agrostis, Anthoxanthum odoratum, Avena fatua, Avena sativa, Bromus hordeaceus, Cynodon dactylon, Dactylis glomerata, Hordeum vulgare, Lolium perenne, Phleum pratense, Poa pratensis, Secale cereale, Triticum, Ventenata dubia, Zea mays), tree pollens (i.e., Chamaecyparis obtuse, Cryptomeria japonica, Juniperus ashei, Olea europaea) and house dust mites (i.e., Blomia tropicalis, Dermatophagoides farinae, and Dermatophagoides pteronyssinus). This technology, in addition to being user-friendly, requires only few milligrams of product to allow unambiguous source material identification. As illustrated in Fig. 2, even closely related species can be identified and distinguished on the basis on their unique molecular compositions, when assessed by MALDI-ToF MS proteomics. We thus believe that the latter method may be suitable for release testing of most allergenic source materials.
Composite correlation index matrix visualization (Biotyper, Bruker Daltonics) of 31 different allergenic extracts assessed by MALDI-ToF MS (AutoFlex Speed, Bruker Daltonics). Reddish (hot) colors mark closely related species. Bluish (cold) colors mark non-related species. Proteins from the allergenic extracts were resuspended in 70 % formic acid solution and sonicated. One microliter of sample was deposited on the MALDI target with 1 μL of α-cyano-4-hydroxycinnamic acid matrix solution and dried prior to MALDI-ToF acquisition
In the interest of allergic patients, the quality of AIT biologicals must be properly documented with respect to their composition, consistency, and stability using state-of-the-art and validated analytical methods. Specifically, proper and consistent allergen dosing is critical to guarantee AIT safety and efficacy. To this aim, allergenic extracts must be standardized based on their potency, which reflects their ability to bind IgEs from allergic patients. In addition, such biological drug products must contain consistent, defined, and clinically efficacious amounts of major allergens [90–92, 93•, 94]. Despite a sustained interest in purified recombinant allergens to perform AIT, natural standardized allergen extracts remain the only authorized therapeutic option, although documenting pharmaceutical quality of the latter is far more complex when compared with the former [95]. Immunological methods, especially ELISA, are routinely used to assess major allergen content of natural extracts [94]. The prerequisites for this method rely on the specificity of mAbs as well as the quality of the reference standard, and the concern arose that some allergen proteoforms (or isoallergens) might not be properly quantified by antibody-based assays [91, 93•].
In this context, MS-based allergen quantification methods were recently developed to circumvent potential specificity issues associated with ELISA [96–99, 100•, 101]. Currently, this methodology relies on the quantification of peptides derived from the allergen following enzymatic digestion. Briefly, the allergenic extract (or food or beverage sample) is reduced and alkylated to disrupt disulfide bonds within the allergens, thereby facilitating their proteolysis by trypsin. Resulting proteotypic peptides are subsequently separated by liquid chromatography and quantified by triple quadrupole MS/MS. As developed in the 1990s, the reference standard can be one (or more) synthetic isotopically labeled peptide with a sequence identical to the one from the protein to be quantified [102]. Because the latter analytical procedure assumes that 100 % of the allergen is digested during sample preparation, an alternative and preferred method is rather based on standard addition of non-labeled intact allergen as a reference standard. The main advantage of this latter technique is that it provides accurate and comprehensive allergen quantification, irrespective of the extent of target allergen digestion. As a result, based on this standard addition method, we found a 30-fold increase in absolute quantification of grass pollen group 1 allergen with MS when compared with results obtained using a dedicated ELISA, likely as a consequence of the variability of grass pollen allergens with some isoallergens poorly recognized by either one of the mAbs used in the ELISA [31, 103]. Overall, the most compelling reasons to recommend the implementation of allergen quantification by MS for release testing of AIT drug products are the unrivaled specificity and comprehensiveness of this method.
Identification of Biomarkers of AIT Efficacy
There is currently a growing interest in identifying biomarkers guiding the physician’s decision to initiate, continue, or terminate AIT [104–108]. A biomarker is defined as a molecule that is detected or quantified in the body fluids to differentiate a patient from a healthy individual or to document the impact of a treatment [109]. As of today, very few studies related to AIT have revealed candidate biomarker molecules correlating with clinical benefit at an individual patient level [110]. Such biomarkers would be most valuable for many actors, including but not limited to the physicians and patients as well as health authorities and payers. The search for such biomarkers now benefits from the combined use of omic technologies, as part of a “panoromic” approach [111•].
We have applied a combination of proteomic methods, namely, 2D differential gel electrophoresis (2D-DiGE) and label-free MS, in order to identify candidate biomarkers of clinical efficacy by comparing the proteomes of various subtypes of effector and regulatory human dendritic cells (DCs). Briefly, 2D-DiGE consists in labeling the proteins from the samples to be compared with different dyes and further subjecting the labeled proteins to 2D-PAGE. Following separation, gel images were acquired with a wavelength specific of each dye and statistically compared for protein abundance. Similarly, label-free MS consists in a statistical analysis of the amount of proteins within the compared sera and also allows quantifying hundreds of proteins. Those two orthogonal and semi-quantitative methods evidenced, among other molecules, complement component 1 (C1Q) and the receptor stabilin-1 molecules as candidate markers of the clinical tolerance induced by grass pollen AIT [112]. In combination with qPCR, an extensive label-free MS study revealed at least five proteins that are differentially expressed in DC2s and DCreg cells, thereby confirming that AIT modifies key components of the innate immune system within 2 months of treatment [113]. These semi-quantitative methods were further applied to compare sera from grass pollen allergic patients enrolled in a double-blind placebo-controlled study performed in an exposure challenge chamber [114]. As a result, we observed differences in post-translational modification of serum α-2-HS-glycoprotein (or fetuin A) when comparing sera from patients exhibiting clinical responses with weak AIT responders (manuscript in preparation).
Overall and despite the fact that the identification of biomarkers based on proteomics is still a lengthy, resource-demanding, and complex process, it remains a unique approach to identify proteins or protein isoforms (e.g., glycoforms) that represent candidate biomarkers of AIT efficacy. For this reason, proteomics is usually applied to a limited number of sera (up to 100) and more simple methods (e.g., ELISA, qPCR) are subsequently applied to a larger number of patients to validate those molecules.
Conclusions
Current allergy care can benefit from many applications of proteomics, whether through specific allergen detection in numerous matrices, in vitro diagnostic, or documentation of the quality and consistency of biological products intended for safe and efficacious AIT. In this context, we speculate that mass spectrometry and hyphenated techniques (including powerful biocomputing dedicated to data mining) will play an expanding role in the field of allergy. During the next decade, we believe that proteomics will keep paving the way for (i) improved understanding of the pathophysiology of allergic diseases, (ii) unambiguous identification and characterization of allergens, (iii) highly specific and comprehensive allergen quantification, and (iv) enhanced molecular diagnostic including the identification of efficacy biomarkers. Lastly, it is also through the use of state-of-the-art proteomics, likely in combination with genomics and next-generation sequencing, that second generation allergen immunotherapy drug products will be made available for allergic patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kenyon GL, DeMarini DM, Fuchs E, Galas DJ, Kirsch JF, Leyh TS, et al. Defining the mandate of proteomics in the post-genomics era: workshop report. Mol Cellular Proteomics. 2002;1(10):763–80.
The UniProt Consortium. UniProt: a hub for protein information. Nucleic Acids Res 2015;43:D204-212.
Szefler SJ, Wenzel S, Brown R, Erzurum SC, Fahy JV, Hamilton RG, et al. Asthma outcomes: biomarkers. J Allergy Clin Immunol. 2012;129(3 Suppl):S9–23.
Paczesny S. Discovery and validation of graft-versus-host disease biomarkers. Blood. 2013;121(4):585–94.
Yeat NC, Lin C, Sager M, Lin J. Cancer proteomics: developments in technology, clinical use and commercialization. Expert Rev Proteomics. 2015;12(4):391–405.
Mohan C, Assassi S. Biomarkers in rheumatic diseases: how can they facilitate diagnosis and assessment of disease activity? BMJ. 2015;351:5079.
Lindsey ML, Mayr M, Gomes AV, Delles C, Arrell DK, Murphy AM, et al. Transformative impact of proteomics on cardiovascular health and disease: a scientific statement from the American heart association. Circulation. 2015;132(9):852–72.
Bousquet J, Anto JM, Akdis M, Auffray C, Keil T, Momas I, et al. Paving the way of systems biology and precision medicine in allergic diseases: the MeDALL success story. Allergy 2016. doi:10.1111/all.12880. Combination of epigenetics, proteomics, transcriptomics and IgE micro-array to better manage allergic diseases.
Nathan RA, Meltzer EO, Derebery J, Campbell UB, Stang PE, Corrao MA, et al. The prevalence of nasal symptoms attributed to allergies in the United States: findings from the burden of rhinitis in an America survey. Allergy Asthma Proc. 2008;29(6):600–8.
Ait-Khaled N, Pearce N, Anderson HR, Ellwood P, Montefort S, Shah J. Global map of the prevalence of symptoms of rhinoconjunctivitis in children: the International Study of Asthma and Allergies in Childhood (ISAAC) phase three. Allergy. 2009;64(1):123–48.
Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):9–17.
Calderon MA, Demoly P, Gerth van Wijk R, Bousquet J, Sheikh A, Frew A, et al. EAACI: a European declaration on immunotherapy. Designing the future of allergen specific immunotherapy. Clin Transl Allergy. 2012;2(1):20.
Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133(2):291–307. Review on the epidemiology, pathogenesis, diagnosis, and treatment of food allergy.
Radauer C, Nandy A, Ferreira F, Goodman RE, Larsen JN, Lidholm J, et al. Update of the WHO/IUIS allergen nomenclature database based on analysis of allergen sequences. Allergy. 2014;69(4):413–9. Public database with official systematic nomenclature of allergenic proteins and links to proteomics resources.
Lowenstein H. Quantitative immunoelectrophoretic methods as a tool for the analysis and isolation of allergens. Prog Allergy. 1978;25:1–62.
Niall HD. Automated Edman degradation: the protein sequenator. Methods Enzymol. 1973;27:942–1010.
Simpson RJ, Nice EC, Moritz RL, Stewart GA. Structural studies on the allergen Der p 1 from the house dust mite Dermatophagoides pteronyssinus: similarity with cysteine proteinases. Protein Seq Data Anal. 1989;2(1):17–21.
Villalba M, Batanero E, Lopez-Otin C, Sanchez LM, Monsalve RI, de la Pena MA G, et al. The amino acid sequence of Ole e I, the major allergen from olive tree (Olea europaea) pollen. Eur J Biochem. 1993;216(3):863–9.
Kettner A, Hughes GJ, Frutiger S, Astori M, Roggero M, Spertini F, et al. Api m 6: a new bee venom allergen. J Allergy Clin Immunol. 2001;107(5):914–20.
Swoboda I, Jilek A, Ferreira F, Engel E, Hoffmann-Sommergruber K, Scheiner O, et al. Isoforms of Bet v 1, the major birch pollen allergen, analyzed by liquid chromatography, mass spectrometry, and cDNA cloning. J Biol Chem. 1995;270(6):2607–13.
Kristensen AK, Schou C, Roepstorff P. Determination of isoforms, N-linked glycan structure and disulfide bond linkages of the major cat allergen Fel d1 by a mass spectrometric approach. Biol Chem. 1997;378(8):899–908.
Helsper JP, Gilissen LJ, van Ree R, America AH, Cordewener JH, Bosch D. Quadrupole time-of-flight mass spectrometry: a method to study the actual expression of allergen isoforms identified by PCR cloning. J Allergy Clin Immunol. 2002;110(1):131–8.
Shefcheck KJ, Musser SM. Confirmation of the allergenic peanut protein, Ara h 1, in a model food matrix using liquid chromatography/tandem mass spectrometry (LC/MS/MS). Journal of Agric Food Chem. 2004;52(10):2785–90.
Natale M, Bisson C, Monti G, Peltran A, Garoffo LP, Valentini S, et al. Cow’s milk allergens identification by two-dimensional immunoblotting and mass spectrometry. Mol Nutr Food Res. 2004;48(5):363–9.
Abdel Rahman AM, Kamath SD, Lopata AL, Robinson JJ, Helleur RJ. Biomolecular characterization of allergenic proteins in snow crab (Chionoecetes opilio) and de novo sequencing of the second allergen arginine kinase using tandem mass spectrometry. J Proteomics. 2011;74(2):231–41.
Downs ML, Baumert JL, Taylor SL, Mills EN. Mass spectrometric analysis of allergens in roasted walnuts. J Proteomics. 2016;142:62–9.
Batanero E, Villalba M, Monsalve RI, Rodriguez R. Cross-reactivity between the major allergen from olive pollen and unrelated glycoproteins: evidence of an epitope in the glycan moiety of the allergen. J Allergy Clin Immunol. 1996;97(6):1264–71.
Aalberse RC. Clinical relevance of carbohydrate allergen epitopes. Allergy. 1998;53(45 Suppl):54–7.
Kolarich D, Altmann F. N-Glycan analysis by matrix-assisted laser desorption/ionization mass spectrometry of electrophoretically separated nonmammalian proteins: application to peanut allergen Ara h 1 and olive pollen allergen Ole e 1. Anal Biochem. 2000;285(1):64–75.
Dumez ME, Teller N, Mercier F, Tanaka T, Vandenberghe I, Vandenbranden M, et al. Activation mechanism of recombinant Der p 3 allergen zymogen: contribution of cysteine protease Der p 1 and effect of propeptide glycosylation. J Biol Chem. 2008;283(45):30606–17.
Fenaille F, Nony E, Chabre H, Lautrette A, Couret MN, Batard T, et al. Mass spectrometric investigation of molecular variability of grass pollen group 1 allergens. J Proteome Res. 2009;8(8):4014–27.
Almond RJ, Flanagan BF, Antonopoulos A, Haslam SM, Dell A, Kimber I, et al. Differential immunogenicity and allergenicity of native and recombinant human lactoferrins: role of glycosylation. Eur J Immunol. 2013;43(1):170–81.
Berg EA, Platts-Mills TA, Commins SP. Drug allergens and food—the cetuximab and galactose-alpha-1,3-galactose story. Ann Allergy Asthma Immunol. 2014;112(2):97–101.
Soh WT, Le Mignon M, Suratannon N, Satitsuksanoa P, Chatchatee P, Wongpiyaboron J, et al. The house dust mite major allergen Der p 23 displays O-glycan-independent IgE reactivities but no chitin-binding activity. Int Arch Allergy Immunol. 2015;168(3):150–60.
Chen JQ, Heldman MR, Herrmann MA, Kedei N, Woo W, Blumberg PM, et al. Absolute quantitation of endogenous proteins with precision and accuracy using a capillary Western system. Anal Biochem. 2013;442(1):97–103.
Hamm M, Ha S, Rustandi RR. Automated capillary Western dot blot method for the identity of a 15-valent pneumococcal conjugate vaccine. Anal Biochem. 2015;478:33–9.
Hoofnagle AN, Wener MH. The fundamental flaws of immunoassays and potential solutions using tandem mass spectrometry. J Immunol Methods. 2009;347(1-2):3–11.
Svobodova M, Mairal T, Nadal P, Bermudo MC, O’Sullivan CK. Ultrasensitive aptamer based detection of beta-conglutin food allergen. Food Chem. 2014;165:419–23.
Monaci L, Losito I, Palmisano F, Visconti A. Identification of allergenic milk proteins markers in fined white wines by capillary liquid chromatography-electrospray ionization-tandem mass spectrometry. J Chromatogr A. 2010;1217(26):4300–5.
Faeste CK, Ronning HT, Christians U, Granum PE. Liquid chromatography and mass spectrometry in food allergen detection. J Food Prot. 2011;74(2):316–45.
Monaci L, Pilolli R, De Angelis E, Godula M, Visconti A. Multi-allergen detection in food by micro high-performance liquid chromatography coupled to a dual cell linear ion trap mass spectrometry. J Chromatogr A. 2014;1358:136–44.
Gomaa A, Boye J. Simultaneous detection of multi-allergens in an incurred food matrix using ELISA, multiplex flow cytometry and liquid chromatography mass spectrometry (LC-MS). Food Chem. 2015;175:585–92. Comparability of ELISA, LC-MS and multiplex flow cytometry methods for the detection of multiple allergens.
Petersen A, Suck R, Lindner B, Georgieva D, Ernst M, Notbohm H, et al. Phl p 3: structural and immunological characterization of a major allergen of timothy grass pollen. Clin Exp Allergy. 2006;36(6):840–9.
Schmidt H, Krause S, Gelhaus C, Petersen A, Janssen O, Becker WM. Detection and structural characterization of natural Ara h 7, the third peanut allergen of the 2S albumin family. J Proteome Res. 2010;9(7):3701–9.
Bouley J, Groeme R, Le Mignon M, Jain K, Chabre H, Bordas-Le Floch V, et al. Identification of the cysteine protease Amb a 11 as a novel major allergen from short ragweed. J Allergy Clin Immunol. 2015;136(4):1055–64.
Schulten V, Greenbaum JA, Hauser M, McKinney DM, Sidney J, Kolla R, et al. Previously undescribed grass pollen antigens are the major inducers of T helper 2 cytokine-producing T cells in allergic individuals. Proc Natl Acad Sci U S A. 2013;110(9):3459–64.
Bordas-Le Floch V, Le Mignon M, Bouley J, Groeme R, Jain K, Baron-Bodo V, et al. Identification of novel short ragweed pollen allergens using combined transcriptomic and immunoproteomic approaches. PLoS One. 2015;10(8), e0136258.
Batard T, Baron-Bodo V, Martelet A, Le Mignon M, Lemoine P, Jain K, et al. Patterns of IgE sensitization in house dust mite-allergic patients: implications for allergen immunotherapy. Allergy. 2016;71(2):220–9.
Meno KH. Allergen structures and epitopes. Allergy. 2011;66 Suppl 95:19–21.
Westernberg L, Schulten V, Greenbaum JA, Natali S, Tripple V, McKinney DM, et al. T-cell epitope conservation across allergen species is a major determinant of immunogenicity. J Allergy Clin Immunol 2016;138(2):571–578.e7.
Klimek L, Pfaar O, Worm M. New opportunities for allergen immunotherapy using synthetic peptide immuno-regulatory epitopes (SPIREs). Expert Rev Clin Immunol. 2016.
Spangfort MD, Mirza O, Ipsen H, Van Neerven RJ, Gajhede M, Larsen JN. Dominating IgE-binding epitope of Bet v 1, the major allergen of birch pollen, characterized by X-ray crystallography and site-directed mutagenesis. J Immunol. 2003;171(6):3084–90.
Ichikawa S, Takai T, Inoue T, Yuuki T, Okumura Y, Ogura K, et al. NMR study on the major mite allergen Der f 2: its refined tertiary structure, epitopes for monoclonal antibodies and characteristics shared by ML protein group members. J Biochem. 2005;137(3):255–63.
Padavattan S, Flicker S, Schirmer T, Madritsch C, Randow S, Reese G, et al. High-affinity IgE recognition of a conformational epitope of the major respiratory allergen Phl p 2 as revealed by X-ray crystallography. J Immunol. 2009;182(4):2141–51.
Tan KW, Ong TC, Gao YF, Tiong YS, Wong KN, Chew FT, et al. NMR structure and IgE epitopes of Blo t 21, a major dust mite allergen from Blomia tropicalis. J Biol Chem. 2012;287(41):34776–85.
Gieras A, Cejka P, Blatt K, Focke-Tejkl M, Linhart B, Flicker S, et al. Mapping of conformational IgE epitopes with peptide-specific monoclonal antibodies reveals simultaneous binding of different IgE antibodies to a surface patch on the major birch pollen allergen, Bet v 1. J Immunol. 2011;186(9):5333–44.
Ebner C, Szepfalusi Z, Ferreira F, Jilek A, Valenta R, Parronchi P, et al. Identification of multiple T cell epitopes on Bet v I, the major birch pollen allergen, using specific T cell clones and overlapping peptides. J Immuno. 1993;150(3):1047–54.
van Milligen FJ, van ’t Hof W, van den Berg M, Aalberse RC. IgE epitopes on the cat (Felis domesticus) major allergen Fel d I: a study with overlapping synthetic peptides. J Allergy Clin Immunol. 1994;93(1):34–43.
Miyaji K, Yurimoto T, Saito A, Yasueda H, Takase Y, Shimakura H, et al. Analysis of conformational and sequential IgE epitopes on the major allergen Cry j 2 of Japanese cedar (Cryptomeria japonica) pollen in humans by using monoclonal antibodies for Cry j 2. J Clin Immunol. 2013;33(5):977–83.
Arnon R, Van Regenmortel MH. Structural basis of antigenic specificity and design of new vaccines. Faseb J. 1992;6(14):3265–74.
Coales SJ, Tuske SJ, Tomasso JC, Hamuro Y. Epitope mapping by amide hydrogen/deuterium exchange coupled with immobilization of antibody, on-line proteolysis, liquid chromatography and mass spectrometry. Rapid Commun Mass Spectrom. 2009;23(5):639–47.
Zhang Q, Willison LN, Tripathi P, Sathe SK, Roux KH, Emmett MR, et al. Epitope mapping of a 95 kDa antigen in complex with antibody by solution-phase amide backbone hydrogen/deuterium exchange monitored by Fourier transform ion cyclotron resonance mass spectrometry. Anal Chem. 2011;83(18):7129–36.
Malito E, Faleri A, Lo Surdo P, Veggi D, Maruggi G, Grassi E, et al. Defining a protective epitope on factor H binding protein, a key meningococcal virulence factor and vaccine antigen. Proc Natl Acad Sci U S A. 2013;110(9):3304–9.
Houde D, Engen JR. Conformational analysis of recombinant monoclonal antibodies with hydrogen/deuterium exchange mass spectrometry. Methods Mol Biol. 2013;988:269–89.
Chapman MD, Heymann PW, Platts-Mills TA. Epitope mapping of two major inhalant allergens, Der p I and Der f I, from mites of the genus Dermatophagoides. J Immunol. 1987;139(5):1479–84.
Chruszcz M, Chapman MD, Vailes LD, Stura EA, Saint-Remy JM, Minor W, et al. Crystal structures of mite allergens Der f 1 and Der p 1 reveal differences in surface-exposed residues that may influence antibody binding. J Mol Biol. 2009;386(2):520–30.
Chruszcz M, Pomes A, Glesner J, Vailes LD, Osinski T, Porebski PJ, et al. Molecular determinants for antibody binding on group 1 house dust mite allergens. J Biol Chem. 2012;287(10):7388–98.
Peters RL, Allen KJ, Dharmage SC, Tang ML, Koplin JJ, Ponsonby AL, et al. Skin prick test responses and allergen-specific IgE levels as predictors of peanut, egg, and sesame allergy in infants. J Allergy Clin Immunol. 2013;132(4):874–80.
Tversky JR, Chelladurai Y, McGready J, Hamilton RG. Performance and pain tolerability of current diagnostic allergy skin prick test devices. J Allergy Clin Immunol Pract. 2015;3(6):888–93.
Tanno LK, Calderon MA, Papadopoulos NG, Sanchez-Borges M, Moon HB, Sisul JC, et al. Surveying the new allergic and hypersensitivity conditions chapter of the international classification of diseases (ICD)-11. Allergy. 2016.
Ewan PW, Coote D. Evaluation of a capsulated hydrophilic carrier polymer (the ImmunoCAP) for measurement of specific IgE antibodies. Allergy. 1990;45(1):22–9.
Canonica GW, Ansotegui IJ, Pawankar R, Schmid-Grendelmeier P, van Hage M, Baena-Cagnani CE, et al. A WAO—ARIA—GA(2)LEN consensus document on molecular-based allergy diagnostics. World Allergy Organ J. 2013;6(1):17. A guide for the indications, determination, and interpretation of molecular-based allergy diagnostics for clinicians.
Lupinek C, Wollmann E, Baar A, Banerjee S, Breiteneder H, Broecker BM, et al. Advances in allergen-microarray technology for diagnosis and monitoring of allergy: the MeDALL allergen-chip. Methods. 2014;66(1):106–19.
Stringari G, Tripodi S, Caffarelli C, Dondi A, Asero R, Di Rienzo Businco A, et al. The effect of component-resolved diagnosis on specific immunotherapy prescription in children with hay fever. J Allergy Clin Immunol. 2014;134(1):75–81. The impact of component-resolved diagnosis on AIT prescription.
Khinchi MS, Poulsen LK, Carat F, Andre C, Hansen AB, Malling HJ. Clinical efficacy of sublingual and subcutaneous birch pollen allergen-specific immunotherapy: a randomized, placebo-controlled, double-blind, double-dummy study. Allergy. 2004;59(1):45–53.
Dahl R, Kapp A, Colombo G, de Monchy JG, Rak S, Emminger W, et al. Efficacy and safety of sublingual immunotherapy with grass allergen tablets for seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006;118(2):434–40.
Frew AJ, Powell RJ, Corrigan CJ, Durham SR. Efficacy and safety of specific immunotherapy with SQ allergen extract in treatment-resistant seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006;117(2):319–25.
Didier A, Malling HJ, Worm M, Horak F, Jager S, Montagut A, et al. Optimal dose, efficacy, and safety of once-daily sublingual immunotherapy with a 5-grass pollen tablet for seasonal allergic rhinitis. J Allergy Clin Immunol. 2007;120(6):1338–45.
Powell RJ, Frew AJ, Corrigan CJ, Durham SR. Effect of grass pollen immunotherapy with Alutard SQ on quality of life in seasonal allergic rhinoconjunctivitis. Allergy. 2007;62(11):1335–8.
Dahl R, Kapp A, Colombo G, de Monchy JG, Rak S, Emminger W, et al. Sublingual grass allergen tablet immunotherapy provides sustained clinical benefit with progressive immunologic changes over 2 years. J Allergy Clin Immunol. 2008;121(2):512–8.
Cox LS, Casale TB, Nayak AS, Bernstein DI, Creticos PS, Ambroisine L, et al. Clinical efficacy of 300IR 5-grass pollen sublingual tablet in a US study: the importance of allergen-specific serum IgE. J Allergy Clin Immunol. 2012;130(6):1327–34.
Worm M, Rak S, de Blay F, Malling HJ, Melac M, Cadic V, et al. Sustained efficacy and safety of a 300IR daily dose of a sublingual solution of birch pollen allergen extract in adults with allergic rhinoconjunctivitis: results of a double-blind, placebo-controlled study. Clin Transl Allergy. 2014;4(1):7.
Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol. 2011;127(1 Suppl):S1–55.
Esch RE, Plunkett GA. Immunotherapy preparation guidelines, rules, and regulation. Allergy Asthma Rep. 2013;13(4):406–13.
http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/ WC500003333.pdf.
Krause B, Seifert S, Panne U, Kneipp J, Weidner SM. Matrix-assisted laser desorption/ionization mass spectrometric investigation of pollen and their classification by multivariate statistics. Rapid Commun Mass Spectrom. 2012;26(9):1032–8.
Lay Jr JO, Holland RD. Rapid identification of bacteria based on spectral patterns using MALDI-TOFMS. Methods Mol Biol. 2000;146:461–87.
Machen A, Drake T, Wang YF. Same day identification and full panel antimicrobial susceptibility testing of bacteria from positive blood culture bottles made possible by a combined lysis-filtration method with MALDI-TOF VITEK mass spectrometry and the VITEK2 system. PLoS One. 2014;9(2):87870.
Altun O, Botero-Kleiven S, Carlsson S, Ullberg M, Ozenci V. Rapid identification of bacteria from positive blood culture bottles by MALDI-TOF MS following short-term incubation on solid media. J Med Microbiol. 2015;64(11):1346–52.
van Ree R. The CREATE project: EU support for the improvement of allergen standardization in Europe. Allergy. 2004;59(6):571–4.
Himly M, Nony E, Chabre H, Van Overtvelt L, Neubauer A, van Ree R, et al. Standardization of allergen products: 1. Detailed characterization of GMP-produced recombinant Bet v 1.0101 as biological reference preparation. Allergy. 2009;64(7):1038–45.
Lowenstein H. Characterization and standardization of allergen extracts. Chem Immunol Allergy. 2014;100:323–32.
Himly M, Nandy A, Kahlert H, Thilker M, Steiner M, Briza P, et al. Standardization of allergen products: 2. Detailed characterization of GMP-produced recombinant Phl p 5.0109 as European pharmacopoeia reference standard. Allergy. 2016;71(4):495–504. The importance of proteomics methods for the establishment of well-characterized allergen reference standards.
Kaul S, Zimmer J, Dehus O, Costanzo A, Daas A, Buchheit KH, et al. Standardization of allergen products: 3. validation of candidate european pharmacopoeia standard methods for quantification of major birch allergen bet v 1. Allergy 2016
Nony E, Bouley J, Le Mignon M, Lemoine P, Jain K, Horiot S, et al. Development and evaluation of a sublingual tablet based on recombinant Bet v 1 in birch pollen-allergic patients. Allergy. 2015;70(7):795–804.
Careri M, Costa A, Elviri L, Lagos JB, Mangia A, Terenghi M, et al. Use of specific peptide biomarkers for quantitative confirmation of hidden allergenic peanut proteins Ara h 2 and Ara h 3/4 for food control by liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem. 2007;389(6):1901–7.
Seppala U, Dauly C, Robinson S, Hornshaw M, Larsen JN, Ipsen H. Absolute quantification of allergens from complex mixtures: a new sensitive tool for standardization of allergen extracts for specific immunotherapy. J Proteome Res. 2011;10(4):2113–22.
Houston NL, Lee DG, Stevenson SE, Ladics GS, Bannon GA, McClain S, et al. Quantitation of soybean allergens using tandem mass spectrometry. J Proteome Res. 2011;10(2):763–73.
Kuppannan K, Albers DR, Schafer BW, Dielman D, Young SA. Quantification and characterization of maize lipid transfer protein, a food allergen, by liquid chromatography with ultraviolet and mass spectrometric detection. Anal Chem. 2011;83(2):516–24.
Koeberl M, Clarke D, Lopata AL. Next generation of food allergen quantification using mass spectrometric systems. J Proteome Res. 2014;13(8):3499–509. A review of state-of-the-art approaches to quantify food allergens.
Briza P. The potential of mass spectrometry as a novel tool in standardization of natural allergen extracts. Arbeiten Paul-Ehrlich-Institut. 2013;97:57–62.
Barr JR, Maggio VL, Patterson Jr DG, Cooper GR, Henderson LO, Turner WE, et al. Isotope dilution—mass spectrometric quantification of specific proteins: model application with apolipoprotein A-I. Clin Chem. 1996;42(10):1676–82.
Batard T, Nony E, Chabre H, Hrabina M, Bouley J, Lemignon M, et al. Molecular and functional characterization of natural allergen extracts. Arbeiten Paul-Ehrlich-Institut. 2013;97:54–6.
Trusheim MR, Berndt ER, Douglas FL. Stratified medicine: strategic and economic implications of combining drugs and clinical biomarkers. Nat Rev Drug Discov. 2007;6(4):287–93.
Senna G, Calderon M, Makatsori M, Ridolo E, Passalacqua G. An evidence-based appraisal of the surrogate markers of efficacy of allergen immunotherapy. Curr Opin Allergy Clin Immunol. 2011;11(4):375–80.
Moingeon P. Update on immune mechanisms associated with sublingual immunotherapy: practical implications for the clinician. J Allergy Clin Immunol Pract. 2013;1(3):228–41.
Shamji MH, Ljorring C, Wurtzen PA. Predictive biomarkers of clinical efficacy of allergen-specific immunotherapy: how to proceed. Immunotherapy. 2013;5(3):203–6.
Willis JC, Lord GM. Immune biomarkers: the promises and pitfalls of personalized medicine. Nature reviews. Immunology. 2015;15(5):323–9.
Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 2001;69(3):89-95. doi:10.1067/mcp.2001.113989.
Shamji MH, Ljorring C, Francis JN, Calderon MA, Larche M, Kimber I, et al. Functional rather than immunoreactive levels of IgG4 correlate closely with clinical response to grass pollen immunotherapy. Allergy. 2012;67(2):217–26.
Moingeon P. Biomarkers for allergen immunotherapy: a “Panoromic” view. Immunol Allergy Clin North Am. 2016;36(1):161–79. Up-to-date review on the combination of omics methods to identify novel putative BMKs of AIT.
Zimmer A, Bouley J, Le Mignon M, Pliquet E, Horiot S, Turfkruyer M, et al. A regulatory dendritic cell signature correlates with the clinical efficacy of allergen-specific sublingual immunotherapy. J Allergy Clin Immunol. 2012;129(4):1020–30.
Gueguen C, Bouley J, Moussu H, Luce S, Duchateau M, Chamot-Rooke J, et al. Changes in markers associated with dendritic cells driving the differentiation of either TH2 cells or regulatory T cells correlate with clinical benefit during allergen immunotherapy. J Allergy Clin Immunol. 2016;137(2):545–58.
Horak F, Zieglmayer P, Zieglmayer R, Lemell P, Devillier P, Montagut A, et al. Early onset of action of a 5-grass-pollen 300-IR sublingual immunotherapy tablet evaluated in an allergen challenge chamber. J Allergy Clin Immunol. 2009;124(3):471–7. 477 e471.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Moingeon reports funding from Stallergenes Greer and has a patent identity test by MS pending. Dr. Le Mignon reports personal fees from Stallergenes SAS. Dr. Nony has a patent method for Grass Species Identification issued to Stallergenes SAS, a patent sialylated fetuin A as a marker of immunotherapy efficacy pending to Stallergenes SAS, and a patent biomarker of immunotherapy efficacy pending to Stallergenes SAS. Dr. Martelet reports personal fees from Stallergenes SAS.
Human and Animal Rights and Informed Consent
This article does not contain any studies with animal subjects performed by the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Additional information
This article is part of the Topical Collection on Allergens
Rights and permissions
About this article
Cite this article
Nony, E., Le Mignon, M., Brier, S. et al. Proteomics for Allergy: from Proteins to the Patients. Curr Allergy Asthma Rep 16, 64 (2016). https://doi.org/10.1007/s11882-016-0642-5
Published:
DOI: https://doi.org/10.1007/s11882-016-0642-5