Opinion statement
The use of the cannabis plant by cancer patients has been rising significantly in the past few years worldwide, primarily driven by public demand. There is an obvious need for more reliable scientific data, pharmacology information, a better understanding of its mode of action, and available clinical evidence supporting its robust use. Physicians must complete a thorough medical assessment, screening for potential drugs, or treatment contraindications before allowing its consumption. In light of the growing popularity of cannabis usage, it is highly essential that, in the near future, the medical community will be able to provide practical recommendations and explicit guidelines, including doses, and that cannabinoid concentrations in the used products are defined regarding its prescription before any medical procedure involving its usage is authorized. Here, we review and describe the favorable outcomes demonstrating the benefits of cannabis as an adjunctive treatment to conventional medicines for chemotherapy-induced nausea, vomiting, and cancer-related pain (primarily refractory chronic or neuropathic pain). Although not yet substantial enough, the treatment of anorexia, insomnia, depression, and anxiety is also seemingly favorable. To date, reports regarding its anti-neoplastic effects or its potent immunosuppressive properties influencing response to immunotherapy are still very conflicting and controversial. Thus, with the current state of evidence, cannabis use is not advisable as initial treatment, as an adjunct or an advanced line of care. In the coming years, we expect that preclinical data and animal models will shift to the clinical arena, and more patients will be recruited for clinical trials, and their reports will advance the field. Thus, physicians should prescribe cannabis only if careful clarification and consideration is provided together with a follow-up response evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
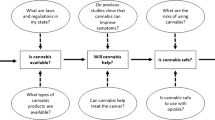
Cannabis has been used as a healing herb since ancient times and is currently approved in many countries for recreational and medicinal use. The cannabinoid receptor CB1 was characterized in 1991, the second receptor CB2 in 1993. The CB1 receptor is highly expressed primely in the central nervous system in areas like the amygdala, hippocampus, cortex, basal ganglia, and cerebellum, whereas CB2 presents primarily in the immune system [1] (Fig. 1a). CB1 receptor agonists were shown to affect the release of neurotransmitters from the synapses, while CB2 agonists are mostly related to the regulation of the immune system and inflammation [1].
Cannabinoid receptors expression and association with diseases and symptoms. a Scattering of cannabis receptors expression (CB1, CB2, TRVP1, TRVP2, GPR18, GPR55, and GPR119) in the body and their association with diseases and symptoms. b The endocannabinoids receptors CB1, CB2, TRPV1, TRPV2 channels and GPR-family receptors (GPR18, GPR55, and GPR119) are presented, in addition to PPARα nuclear receptors that play essential roles in the regulation of tumorigenesis and the FAAH mitochondrial receptor that comes to the endocannabinoid system. An increase in the endocannabinoid N-oleoyl glycine (OG) can elevate the expression of CB1 receptors, and palmitoylation enhances the hydrophobicity of the CB2 receptor. The PEA inhibitor of FAAH acts as a support compound in the spinal cord for the hypotensive effects of managed endocannabinoids
The endocannabinoid system is an endogenous lipid-based system of agonists that binds to cannabinoid receptors (CBRs). The most well-known and studied endocannabinoids are the N-arachidonoyl-ethanolamine (AEA; anandamide) and 2-arachidonoylglycerol (2-AG). Phytocannabinoids are cannabis-derived lipophilic molecules extracted from the plant. When consumed, phytocannabinoids can interact with our body’s receptors and produce numerous psychotropic and therapeutic effects. Currently, more than 140 different cannabinoids have been isolated from cannabis, exhibiting varied effects. The most notable phytocannabinoids are Δ9-tetrahydrocannabinol (Δ9-THC), Δ9-tetrahydrocannabivarin (Δ9-THCV), cannabinol (CBN), cannabidiol (CBD), cannabidivarin (CBDV), cannabigerol (CBG), and cannabichromene (CBC), which bind to CBRs (Fig. 1b) [2•, 3]. In addition, phytocannabinoids can also modulate a specific subset of transient receptor potential (TRP) (most potently at TRPV2, moderately modulate TRPV3, TRPV4) channels (Fig. 1b) [4]; these channels modulate ion entry and mediate a variety of neuronal signals that are responsible for the sensations of pressure, temperature, and smell. Furthermore, endocannabinoids (such as oleoylethanolamide (OEA) and palmitoylethanolamide (PEA)) activate as agonists the nuclear receptor peroxisome proliferator-activated receptors (PPARs) (Fig. 1b). These nuclear hormone receptors modulate the transcription of genes involved in the regulation of cell inflammation and differentiation, and metabolism [5]. Endocannabinoids, such as Aras, AraG, PEA, OEA, and 2-AG, also bind to other G protein–coupled receptors (GPCRs) like GPR18, GPR55, and GPR119 to regulate signals associated with cell proliferation and migration (Fig. 1b) [1, 3].
In light of the recently uncovered biological activity of eCB, reports of the medical use of cannabis or cannabis-based drugs and their efficacy in non-oncological illnesses, such as in alleviating resistant neurological pain in multiple sclerosis (MS) [6] and spinal injury pain, Tourette syndrome [7], Crohn’s disease [8], and intractable seizures [9], constantly emerge. Studies demonstrate benefit also in graft-versus-host disease after stem cell transplantation [10], fibromyalgia, arthritis, sleep problems, appetite and weight loss, anxiety, and others [11].
Cannabinoids are classified according to their source of production: phytocannabinoids occur naturally in the cannabis plant; endocannabinoids (eCBs) are produced endogenously by humans and other mammals, and synthetic cannabinoids have now been manufactured for use in research and medicine.
Natural phytocannabinoids may be extracted from plants and taken in an herbal form or manufactured synthetically. Oral cannabis formulations, including oils, capsules, edibles, or spray, can be mixed with food or tea, inhaled, smoked, or injected in tumors. Other types of administration are oromucosal sprays, rectal suppositories, salves, and topically delivered preparations. Novel devices had been developed to deliver a metered dose by inhalation, such as the Syqe Inhaler Exo (Syqe Medical Ltd., Tel Aviv, Israel) [12].
There are many medications based on natural or synthetic cannabinoids or cannabinoid analogs. Dronabinol (Marinol®, Mariette GA) is a ∆9-tetrahydrocannabinol (THC), used as an appetite stimulant, anti-emetic, and analgesic, approved in 2003 for improving anorexia and cachexia in AIDS patients and as a treatment against nausea and vomiting in cancer patients [13]. Another is Nabilone (Cesamet®, Aliso Viejo CA), a synthetic THC analog in oral form that is ten times more potent than natural THC, approved in 2006 for chemotherapy-induced nausea and vomiting and has been used off label for pain [14,15,16,17,18,19]. Nabiximols (the non-proprietary name for Sativex) is a mixture in an oromucosal spray form of THC and cannabidiol (CBD) directly isolated from Cannabis sativa L. The combination of these two components is intended to prevent some of the side effects attributed to THC when taken alone [20]. The spray is designed to mimic the quick absorption rate that occurs after smoking cannabis, compared to oral administration. It is approved for the treatment of neuropathic pain and symptoms of multiple sclerosis (MS).
Orally ingested cannabis has low (6–20%) and variable bioavailability. Peak plasma concentrations of ∆9-THC occur after 1–6 h and remain elevated with a terminal half-life of 20–30 h. Orally ingested ∆9-THC is initially metabolized in the liver to 11-OH-THC, a potent psychoactive metabolite [21]. Oral cannabis formulations are convenient, generally easy to dose, and have a long duration of action, but the onset of action is slow, and absorption may be reduced with food or enhanced with lipid or oil solvents [22••].
When inhaled, cannabinoids are rapidly absorbed into the bloodstream with a peak concentration of about 2–10 min, declining rapidly for 30 min and minimally generate the psychoactive 11-OH metabolite [23]. Smoking remains the most common and most rapid route of administration and is especially helpful for the treatment of acute symptoms. Vaporizers are safe and efficient devices that are temperature-controlled and electronically driven to decarboxylate inactive cannabinoids released as active cannabinoid compounds [24].
Here, we will thoroughly describe and summarize the most timely clinical therapeutic trends of cannabis usage in oncology. We will review its benefits and hazards and suggest that, before considering the use of medical cannabis in oncology, good clinical judgment should be determined if timing and indications for such treatment are appropriate.
Using cannabis in oncology for disease symptoms and treatment-related adverse effects
The effect of cannabis on various cancer-related symptoms relies on self-reporting for many variables, and often a control arm is missing in the majority of the published studies. A prospective observational study that included two interviews based on questionnaires that evaluated symptoms and side effects showed that many cancer-related symptoms improved significantly with cannabis consumption (p < 0.001) [25]. No significant side effects except for memory loss in patients with prolonged cannabis use (p = 0.002) were noted.
Another study on cannabis use in over 3000 cancer patients showed a significant improvement in the control of other common symptoms, including sleep problems (70.8%), fatigue (55.9%), anxiety and depression (74.1%), and nausea and vomiting (54.7%) [26]. Only 18.7% of patients reported good quality of life before treatment initiation, while 69.5% reported a good quality of life at 6 months. Furthermore, 36% of the patients stopped using opioids, and less than 20% discontinued their cannabis treatment. Of these, only 19.3% stopped due to side effects.
Cannabis is known to improve spasticity (including muscle cramps) in MS patients [27]. This effect was reported in a case study where cannabis use resulted in a significant reduction in the frequency of the muscle spasms and the level of pain in vismodegib-related muscle cramps in a patient with advanced basal cell carcinoma [28].
Cancer-related pain
CB1 receptors in the brain (hippocampus, associated cortical regions, cerebellum, and basal ganglia) are thought to modulate nociceptive processing in the brain, independently and in synergism with exogenous opioids and peripheral cannabinoid receptors that have been implicated in anti-nociception by activation of noradrenergic pathways [29]. THC binds as a partial agonist to the G protein–coupled cannabinoid receptors CB1 and CB2. It is thought to be responsible for most of the therapeutic effects attributed to cannabis, including mitigating pain, spasticity, nausea, insomnia, and appetite loss [30, 31].
Systematic reviews regarding the benefits of medicinal cannabis for the management of pain reveal mixed recommendations [11, 32, 33•, 34, 35, 36]. A study that aimed to assess the efficacy of medicinal cannabis for relieving pain in patients with malignant disease demonstrated a significant analgesic effect in 15 of 18 trials as compared to placebo [37•]. Nevertheless, a review from the College of Family Physicians of Canada (CFPC) recommended against the use of medicinal cannabis as a first- or second-line treatment to alleviate cancer pain (strong recommendation) [38•].
A randomized, placebo-controlled trial, which included 177 patients with cancer pain who experienced inadequate analgesia despite chronic opioid dosing, showed statistically significant pain reduction with THC/CBD compared with placebo, while the THC group showed a non-significant improvement. Twice as many patients taking THC/CBD showed a reduction of more than 30% from baseline pain numerical rating scale (NRS) score when compared with placebo. There was no change from baseline in median doses of opioid background medication, and the side effects were mild to medium only [39].
The long-term use of the THC/CBD spray is generally well-tolerated, with no evidence of a loss of effect for the relief of cancer-related pain with long-term use. According to a study including 43 patients evaluating the long-term safety and tolerability of THC/CBD and THC sprays, the effect of consumption was sustained for as long as 2 years without the need for elevations in opioid dosages [40]. THC/CBD spray (nabiximols) also showed efficacy in reducing the average daily pain from baseline and a reduction in sleep disruption according to a randomized, double-blind, placebo-controlled study in patients with advanced cancer and opioid-refractory pain [41]. This effect was mainly observed in the groups treated with low (1–4 sprays/day) and medium (6–10 sprays/day) doses. Adverse events were dose-dependent and significant only in the high-dose group (11–16 sprays/day). In two double-blind, randomized, placebo-controlled phase 3 studies, nabiximols (Sativex®) did not demonstrate superiority to placebo in reducing self-reported pain numerical rating scale (NRS) scores in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy [42].
The opioid-sparing effects of cannabis were observed in preclinical and early clinical studies [43]. Moreover, some evidence of potential synergistic relief of pain with concomitant use of opioids has been demonstrated without significantly altering plasma opioids levels [44]. For example, Bar-Sela et al. performed an observational study evaluating patient-reporting cancer-related symptoms using medical cannabis and found not only pain reduction but also reduction of opioid dose in near 50% of the subjects [25]. Cannabis cigarettes or vaporized cannabis was found to be effective in improving neuropathic pain according to two small randomized studies [45, 46].
Chemotherapy-induced nausea and vomiting
Medical cannabis is increasingly used in the management of chemotherapy-induced nausea and vomiting (CINV). As mentioned above, dronabinol and nabilone were approved by the FDA for refractory nausea and vomiting and were included in the recent national comprehensive cancer network (NCCN) guidelines for anti-emesis [47]. Since endocannabinoid receptors richly populate the neuronal tracts for emesis, they are chosen as designated targets for treating CINV. CB-1 receptors are found in the dorsal vagal complex, which contains vagal outputs in the gastrointestinal tract and regulates emesis. Activating these receptors by THC demonstrated anti-emetic effects [48]. Results from several preclinical studies suggest that CBD has anti-inflammatory, analgesic, anti-nausea, antiemetic, anti-psychotic, anti-ischemic, anxiolytic, and anti-epileptic impact [15]. Animal studies with delta-9-tetrahydrocannabinol and cannabidiol showed higher activity in suppressing anticipatory nausea than ondansetron (5-HT3 antagonist) [49].
In a small, controlled, randomized, “double-blind” experiment, oral tetrahydrocannabinol had anti-emetic properties and was significantly better than a placebo in reducing vomiting caused by chemotherapeutic agents [50]. A blinded, placebo-controlled trial comparing dronabinol, ondansetron, or a combination, for delayed CINV, showed non-inferiority for dronabinol versus ondansetron, without any synergism [51]. A small phase II study investigated nabiximols in 16 patients and found that 4.8 sprays daily was more effective than placebo in conjunction with standard anti-emetics [52].
A meta-analysis that included over 1100 patients from 30 randomized controlled studies found a statistically significant difference in favor of the cannabinoids over neuroleptic drugs in the treatment of CINV: RR=0.33 (CI=0.24–0.44; p < 0.00001) [53]. Two additional systematic reviews comparing THC to older anti-emetics in first-line therapy demonstrated greater effectiveness of cannabinoids, especially in medium-emetogenic chemotherapy regimens [54, 55]. A synergistic effect of dronabinol and prochlorperazine was shown in an RCT with a reduction in occurrence, duration, and severity of CINV [56]. However, a comprehensive meta-analysis found low-quality evidence for improvement in CINV [32].
Most of the anti-emetic research that was conducted compared medical cannabis treatment to placebo or various neuroleptic drugs. However, these studies did not compare cannabinoids with the anti-emetogenic new medicines, as the potential role of smoked marijuana in treating CINV. Thus, cannabis should be prescribed as an anti-emetic drug only when conventional anti-emetogenic treatment has failed.
Anorexia and cachexia
Cancer-related cachexia and anorexia syndrome (CACS) is a common phenomenon in patients with advanced cancer [57]. The effect of cannabis on appetite and weight gain is unclear as studies show mixed and conflicting results. In a survey that included less than 50 patients, improvement in taste, smell perception, appetite, and caloric intake in patients receiving chemotherapy in the dronabinol arm was demonstrated compared to placebo [58]. However, this study did not compare dronabinol to other effective drugs, such as megestrol acetate. In another study, which included 243 patients randomized to three arms—THC/CBD, THC alone, or a placebo—no significant differences between the groups could be observed regarding the improvement of appetite or weight gain [59]. It is worth noting that cannabinoid dosages in the study were low compared with other studies. A more extensive survey, including 469 advanced cancer patients suffering from a substantial weight loss, randomized patients to three treatment arms: dronabinol, megestrol acetate, or both together. A higher percentage of patients in the megestrol acetate arm reported appetite improvement compared with the dronabinol arm: 75% versus 49% (p = 0.0001) [60]. Combination therapy did not appear to confer additional benefit. In a further small, single-arm study aimed to evaluate the effect of dosage-controlled cannabis capsules on CACS in advanced cancer patients, a weight increase of ≥ 10% in 3/17 (17.6%) patients with a dose of 5mgX1 or 5mgX2 capsules daily, without significant side effects, was reported [57]. These results justify a more extensive study with dosage-controlled cannabis capsules in CACS. In summary, it seems that cannabis has a minor positive effect on CACS, but this effect did not prove superiority to other effective drugs, such as megestrol acetate.
Sleep disturbances, depression, and anxiety
No research yet has addressed the effect of sleep disturbances in oncology patients influenced directly by cannabis. In one study, no significant differences were found in the non-restorative sleep (NRS) quality with cannabis in cancer patients [39]. Another study showed an improvement from baseline of insomnia with THC/CBD base in the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-C30 [40].
A large meta-analysis by Whiting et al. found a positive association between cannabinoids and improved sleep quality, but the study cohort included not only oncology patients [32]. This meta-analysis found no trials evaluating depression fulfilled inclusion criteria. Positive results were found, however, in individuals with social anxiety disorder, as well as in anxiety outcomes in patients with chronic pain. A recent review found improved sleep latency and sleep continuity in insomnia patients and pain reduction and improved subjective sleep quality in patients with sleep disturbances secondary to chronic pain [61•]. Overall, it seems that cannabis has positive effects on sleep and anxiety, especially with patients suffering from cancer-related pain.
Cannabis and immunotherapy
CB2 receptor (CB2R) is widely expressed in immune cells when agonists that target this receptor have the potential to alter immune function. Studies show that cannabinoids interacting with the CB2 receptor, including ∆9-THC and CBD, have potent immunosuppressive effects [62]. Moreover, by activating CB2 receptors, ∆9-THC increases the production of IL-4, and IL-10 stimulates Th-2 and inhibits Th-1 responses, resulting in a pro-cancer effect [63]. Furthermore, in a brain tumor model, CB2 agonists caused downregulation of inflammatory pathways, reduced cytokine secretion by lymphocytes, and inhibited adhesion molecules and chemokines [64]. In breast carcinoma cell lines, ∆9-THC increased tumor growth by suppression of the anti-tumor immune response [65]. In a clinical observational study, cannabinoids significantly reduced response rate to immunotherapy treatment, without a difference in overall or progression-free survival, after considering confounders such as performance status and cannabis composition. The authors suggest a possible interaction between the two treatment modalities [66]. In a recent study by Bar-Sela et al., they enrolled 102 patients with advanced cancers initiating immunotherapy treatments. Cannabis users showed a significant decrease in time to treatment progression (TTP) and decreased overall survival (OS). Also, the use of cannabis reduced immune-related adverse events (iAE) [67••]. In conclusion, we recommend using cannabis with caution in oncology patients being treated with immunotherapy and suggest prescribing cannabis only when there are clear indications and expected benefits.
Cannabis as a potential anti-cancer treatment
Although cannabinoids are clinically used for palliative indications, recent studies open a promising possibility as anti-cancer agents. Several well-studied cell signaling pathways and biological processes are implicated in the connection between the endocannabinoids (eCBs) system and cancer [68•]. These pathways and processes include cyclic adenosine monophosphate (cAMP), mitogen-activated protein kinase (MAPK), protein kinase b (Akt), ceramide, reactive oxygen species (ROS) and id-1, epidermal growth factor (EGFR) family, and cancer stem cells (CSC). In line with this, preclinical evidence has shown that phytocannabinoids might have anti-cancer effects as well as anti-mitotic, anti-metastatic, anti-angiogenic, and pro-apoptotic effects in different in vitro cancer cells [69, 70].
For example, it was found that changes in the levels of eCBs metabolizing enzymes and cannabinoid receptors on pancreatic cancer cells may affect the prognosis and pain status of pancreatic cancer patients in a pivotal in vitro study [71]. Synthetic cannabinoid addition caused apoptosis in a significant portion of the cells in vitro [72, 73]. Two main cancer cell signaling pathways (the MAPK signaling pathway and the PI3K/Akt pathway) are involved in cannabinoid receptor reactions, and synthetic agonists of cannabinoid receptors increase the activity of these pathways, while antagonists block them [74]. Additional research has shown in vivo growth inhibition in murine models of lung carcinoma, glioma, thyroid epithelioma, lymphoma, and skin carcinoma [75]. Several in vitro studies suggested a potential synergism between cannabinoids with conventional chemotherapy [76,77,78,79,80] or radiation [81].
One clinical phase I trial was published on the intra-tumoral administration of ∆9-THC on nine patients with glioblastomas who had failed standard therapy [82]. THC administration was safe, and no significant side effects appeared on the nervous system or systemically. Two patients underwent another biopsy that showed reduced tumor cell proliferation and a decrease in tumor vascularization. Another small randomized placebo-controlled phase 2 study, including 21 patients, provided preliminary evidence that 1:1 CBD: THC offers some efficacy in patients with recurrent GBM when used as an adjunct to dose-intense temozolomide and confirmed the safety and feasibility of individualized dosing [83]. In 2011, two cases were reported of pilocytic astrocytomas having a complete response after a few years with residual disease directly correlated to cannabis inhalation [84]. In 2013, another article reported the case of a child with acute lymphoblastic leukemia for whom different cannabis preparations appeared to have a dose-dependent effect on the number of circulating blasts [85].
Despite extensive research, the anti-neoplastic effects of cannabis treatment in humans are still mostly anecdotal. Time-to-tumor progression (TTP) or overall survival (OS) has never been tested as secondary endpoints as part of the research hypothesis in many studies that examined the effects of cannabinoids in cancer patients. To date, there is no phase II or III clinical trials large enough to provide the necessary evidence to support the anti-cancer effects of medical cannabis.
Adverse effects and risks
Cannabinoids or synthetic drugs based on phytocannabinoids are considered medically safe [86]. The main reason for these drugs’ safety profile is the lack of cannabis receptors in the brain stem, thus preventing life-threatening side effects that exist, for example, in morphine-based medications [87]. Therefore, a cautious titration period with approved medical cannabis should be employed to determine the optimal dose and prevent and minimize some of the adverse events. Acute adverse effects include redness of the eyes, tachycardia, bronchodilation, and muscle relaxation. These adverse effects are due to the fact that cannabinoid receptors are present in other tissues throughout the body [39] (Fig. 1a). Another substantial acute adverse effect is the psychoactive effect of the plant, mostly depending on concentration and THC dosage. The psychoactive effect includes dizziness, euphoria, difficulty concentrating, disturbances in thinking, memory loss, and loss of coordination [88]. High tolerance to many of the psychoactive effects of cannabis has been documented in chronic heavy users, presumably due to CB1 receptor downregulation by THC [89]. It also appears that the subjective “high” or euphoric effect of THC usually occurs at higher doses than necessary for pain control [90]. CBD side effects at high doses (20 mg/kg) are diarrhea, vomiting, fatigue, pyrexia, somnolence, and abnormal results on liver-function tests [9, 91]. Sub-psychoactive doses as little as 2.5 mg of THC or less, with or without CBD, may offer many of the therapeutic benefits of cannabis while avoiding intoxication [92•]. CBD at lower doses may improve the tolerability and safety of THC by reducing many of the unwanted side effects (e.g., cognitive impairment, anxiety, paranoia, tachycardia) [16]. Therefore, it is advised to start with the lowest possible dose in cannabis-naïve patients and follow the general rule: “Start low, go up slow and stay low” [22••].
Long-term adverse effects of cannabis use, particularly at high intake levels, are associated with several undesirable psychosocial features, including lower educational achievement and, in some instances, psychiatric illness [93]. Nevertheless, the short time use of cannabis by cancer patients did not have a significant influence on cognitive skills [94]. Several studies indicate that the epidemiological link between cannabis use and schizophrenia probably represents a causal role of cannabis in precipitating the onset or relapse of schizophrenia [95]. A weaker but significant relationship between cannabis and depression has been found in various cohort studies, but the nature of the link is not yet explicit [96]. Persistent cannabis consumption was associated with neuropsychological decline broadly across domains of functioning, even after controlling for years of education. Impairment was concentrated among adolescent-onset cannabis users, with more persistent use associated with a more significant decline [97]. There is little evidence, however, that long-term cannabis use causes permanent cognitive impairment, nor is there are any apparent cause and effect relationship to explain the psychosocial associations according to another study [98]. Cannabis hyperemesis syndrome (CHS) is a rare side effect of unclear origin, a syndrome of cyclic vomiting associated with cannabis use, with no more than 80 reported cases, mostly in chronic cannabis users [99].
Dependence is another potential long-term adverse effect. Abrupt termination of cannabis use can cause withdrawal side effects like discomfort, lack of sleep, heat flashes, and nausea. Although these effects are reported to be mild, they are clinically significant since they can functionally impair normal daily activities and eventually cause a relapse of cannabis use [100]. It is worth noting the difficulty in diagnosing cannabis withdrawal syndrome (CWS) because symptoms do not occur immediately after cessation due to the accumulation of cannabinoids in the fat tissues of the body and their slow release into the plasma [101]. According to a recent review and meta-analysis, the overall pooled prevalence of CWS was 47% [102]. Although no specific study has been made with cannabis in patients with significant hepatic or renal impairment, it can be expected that effects would be more exaggerated or prolonged in these patients, taking into consideration that phytocannabinoids bind to plasma proteins and are unlikely to be removed by hemodialysis [103]. Furthermore, blood THC concentrations 2–5 ng/mL is associated with substantial driving impairment, particularly in occasional smokers, and higher accident culpability risk of drivers using cannabis [104].
Cannabis and risk for cancer
Whether cannabis smoking is a risk factor for cancer illnesses is unclear, and data from several studies are inconclusive. Cannabis smoking combustion products include tobacco carcinogens, such as nitrosamine and polycyclic aromatic hydrocarbons, products that are highly suspected of being associated with lung, head, and neck cancer (HNC) and bladder cancer [105]. Chronic inflammatory and precancerous changes in the airways have been demonstrated in cannabis smokers, and a case-control study shows an increased risk of lung cancer that is proportional to the amount of cannabis use [106]. Population studies conducted in North Africa show a direct connection between consumption of cannabis and nasopharyngeal carcinoma (NPC), independent of cigarette smoking [107], and a significant increase in lung cancer when cigarette smoking and cannabis smoking are combined, compared to smoking each separately [108]. A link between cannabis consumption and testicular cancer has been explored in several studies, the largest of which included 50,000 Swedish men and found higher incidence only in heavy cannabis users [109]. Conversely, other studies do not support the potential increased risk for cancer with cannabis smoking when pooled analysis data of the INHANCE consortium, including more than 4000 HNC patients and more than 5000 controls, showed no elevated risk for HNC among marijuana smoking [110]. Furthermore, smoking marijuana for 10–20 years was associated with a significantly reduced risk for HNC after adjusting for confounders in another case-control study [111].
Cannabis and anti-neoplastic drugs interactions
The metabolism of THC and CBD is not yet completely understood. It is carried out by the cytochrome P450 system, producing a considerable variance in pharmacokinetics between the oral and inhaled routes [112,113,114]. Interaction with potent CYP3A4 inhibitors, such as protease inhibitors, clarithromycin, ketoconazole, and sildenafil, has been mentioned in the literature but only as isolated case reports and does not seem to be clinically relevant [115, 116]. Cannabidiol’s inhibitory effect on CYP 2C9 could increase warfarin’s effect [117]. Evidence for potential interaction between pharmaceutical CBD formulations (5–50 mg/kg/day) and anti-neoplastic drugs in adults and children has also been reported [118]. This could also influence the therapeutic index on some anti-neoplastic drugs that have hepatic metabolism in the cytochrome P450 enzyme system. In one study, 24 cancer patients were treated with intravenous irinotecan (600 mg, n = 12) or docetaxel (180 mg, n = 12), followed 3 weeks later by the same drugs concomitant with medicinal cannabis taken in the form of 200-ml herbal tea, containing 18% THC and 0.8% CBD, for 15 consecutive days, starting 12 days before the second treatment. The administration of cannabis did not significantly influence exposure to and clearance of irinotecan or docetaxel, although the herbal tea route of administration may not reproduce the effects of inhalation or oral ingestion of fat-soluble cannabinoids [119].
Taken together, currently, there are little evidence-based data on how to manage the use of cannabis with other drugs; it has been suggested that frail patients using cannabis or those with polypharmacy issues should be advised that cannabis may result in drug interactions that may impact the efficacy and safety of their other medications [120]. Therefore, oncologists and other healthcare providers have an essential role in educating patients about the safety hazards and risks of its consumption [121].
Current barriers for cannabis use in cancer
The integration of cannabis in oncology faces many obstacles, including a lack of clinical research data, poor clinical knowledge on how to initiate and monitor cannabinoid treatments, and conflicting or confusing regulatory frameworks. Legislation barriers that accompany a drug regulated as illicit narcotics cause difficulty in undertaking clinical research. A survey published in 2017 of adult cancer patients at a major cancer center in Seattle, WA, found high rates of active cannabis use (24% in the last year) and also showed that cancer patients desire but are not receiving information about cannabis from oncology healthcare providers [122]. A survey of 237 US oncologists published in May 2018 showed that, while only 30% felt sufficiently informed to make recommendations regarding cannabis, 80% of oncologists conducted discussions about cannabis with their patients, and 46% recommend cannabis clinically. Additionally, 67% viewed it as a helpful adjunct to standard pain management strategies, and 65% thought cannabis was equal to or more effective than conventional treatments for anorexia and cachexia [123].
Similarly, a cross-sectional survey of Australian general practitioners showed that 61.5% had received at least one patient inquiry regarding cannabinoid-based treatments. Still, only 10% considered themselves as having sufficient knowledge of this class of medication [124]. Therefore, oncologists are challenged about how to knowledgeably address questions, provide professional recommendations, and confidently authorize medical cannabis. Educational programs for medical staff are warmly advised for medical staff who treat cancer patients.
Future directions
Cannabis will undoubtedly play a more significant role in oncology in the years to come, but there are still obstacles to overcome. Larger scale randomized control trials are challenging to conduct due to regulative issues. Exact doses of medical cannabis vary widely and depend upon individual patient needs and tolerance of side effects. The appropriate concentration of THC and CBD and the route of administration according to the patients’ indication of use is another major challenge in the field. The regularization of the medical cannabis field is a complex, unique, innovative, and original process, into which considerable efforts have been invested in its promotion, such as providing medical care according to a regulated medical method and practice, enterprise, and innovation to establish a wide array for the supply chain which operates according to adequate quality principles and the promotion of the knowledge and research in the field.
Moreover, defining clear clinical objectives with patients and their families is of great importance in palliative care. Individual responses to cannabis can vary considerably due to a different pharmacokinetic profile for different cannabinoid products in the market and various uncontrolled products, and subjects cause severe intra- and inter-patient inconsistency in terms of bioavailability of the drug.
To date, although cannabis holds many promises, patients and their families should be reminded of the realistically achievable outcome of medical cannabis treatments, especially when patients may choose to neglect critical anti-neoplastic therapy in an attempt to self-medicate with cannabis without medical monitoring. On the other hand, physicians should try to diminish prejudices related to the use of cannabis and minimize any stigma or lack of knowledge regarding its consumption as a palliative treatment.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zou S, Kumar U. Cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system. Int J Mol Sci. 2018;19. https://doi.org/10.3390/ijms19030833.
Shahbazi F, Grandi V, Banerjee A, Trant JF. Cannabinoids and cannabinoid receptors: the story so far. iScience. 2020. https://doi.org/10.1016/j.isci.2020.101301 In-depth review of the structural biology of the cannabinoids and their target receptrs.
Pacher P, Kogan NM, Mechoulam R. Beyond THC and endocannabinoids. Annu Rev Pharmacol Toxicol. 2020;60:637–59. https://doi.org/10.1146/annurev-pharmtox-010818-021441.
Muller C, Morales P, Reggio PH. Cannabinoid ligands targeting TRP channels. Front Mol Neurosci. 2019;11. https://doi.org/10.3389/fnmol.2018.00487.
O'Sullivan SE. An update on PPAR activation by cannabinoids. Br J Pharmacol. 2016;173:1899–910. https://doi.org/10.1111/bph.13497.
Novotna A, Mares J, Ratcliffe S, Novakova I, Vachova M, Zapletalova O, et al. A randomized, double-blind, placebo-controlled, parallel-group, enriched-design study of nabiximols* (Sativex®), as add-on therapy, in subjects with refractory spasticity caused by multiple sclerosis. Eur J Neurol. 2011;18:1122–31. https://doi.org/10.1111/j.1468-1331.2010.03328.x.
Artukoglu BB, Bloch MH. The potential of cannabinoid-based treatments in Tourette syndrome. CNS Drugs. 2019;33:417–30. https://doi.org/10.1007/s40263-019-00627-1.
Lee Y, Jo J, Chung HY, Pothoulakis C, Im E. Endocannabinoids in the gastrointestinal tract. Am J Physiol - Gastrointest Liver Physiol. 2016;311:G655–66. https://doi.org/10.1152/ajpgi.00294.2015.
Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, et al. Trial of cannabidiol for drug-resistant seizures in the dravet syndrome. N Engl J Med. 2017;376:2011–20. https://doi.org/10.1056/NEJMoa1611618.
Yeshurun M, Shpilberg O, Herscovici C, et al. Cannabidiol for the prevention of graft-versus-host-disease after allogeneic hematopoietic cell. Transplantation: Results of a Phase II Study. Biol Blood Marrow Transplant. 2015. https://doi.org/10.1016/j.bbmt.2015.05.018.
Groce E. The health effects of Cannabis and cannabinoids: the current state of evidence and recommendations for research. J Med Regul. 2018. https://doi.org/10.30770/2572-1852-104.4.32.
Vulfsons S, Ognitz M, Bar-Sela G, Raz-Pasteur A, Eisenberg E. Cannabis treatment in hospitalized patients using the SYQE inhaler: results of a pilot open-label study. Palliat Support Care. 2020;18:12–7. https://doi.org/10.1017/S147895151900021X.
Bar-Sela G, Avisar A, Batash R, Schaffer M. Is the clinical use of Cannabis by oncology patients advisable? Curr Med Chem. 2014;21:1923–30. https://doi.org/10.2174/0929867321666140304151323.
Engels FK, de Jong FA, Mathijssen RHJ, Erkens JA, Herings RM, Verweij J. Medicinal cannabis in oncology. Eur J Cancer. 2007;43:2638–44. https://doi.org/10.1016/j.ejca.2007.09.010.
Turgeman I, Bar-Sela G. Cannabis use in palliative oncology: a review of the evidence for popular indications. Isr Med Assoc J. 2017;19(2):85–8.
Murnion B. Medicinal cannabis. Aust Prescr. 2015. https://doi.org/10.18773/austprescr.2015.072.
Schrot RJ, Hubbard JR. Cannabinoids: medical implications. Ann Med. 2016;48:128–41. https://doi.org/10.3109/07853890.2016.1145794.
Abuhasira R, Shbiro L, Landschaft Y. Medical use of cannabis and cannabinoids containing products – regulations in Europe and North America. Eur J Intern Med. 2018;49:2–6. https://doi.org/10.1016/j.ejim.2018.01.001.
Hazekamp A, Ware MA, Muller-Vahl KR, Abrams D, Grotenhermen F. The medicinal use of Cannabis and cannabinoids-an international cross-sectional survey on administration forms. J Psychoactive Drugs. 2013;45:199–210. https://doi.org/10.1080/02791072.2013.805976.
Schoedel KA, Chen N, Hilliard A, White L, Stott C, Russo E, et al. A randomized, double-blind, placebo-controlled, crossover study to evaluate the subjective abuse potential and cognitive effects of nabiximols oromucosal spray in subjects with a history of recreational cannabis use. Hum Psychopharmacol. 2011. https://doi.org/10.1002/hup.1196.
Lee D, Vandrey R, Mendu DR, Anizan S, Milman G, Murray JA, et al. Oral fluid cannabinoids in chronic cannabis smokers during oral δ9-Tetrahydrocannabinol therapy and smoked cannabis challenge. Clin Chem. 2013;59:1770–9. https://doi.org/10.1373/clinchem.2013.207316.
MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med. 2018. https://doi.org/10.1016/j.ejim.2018.01.004 Authors provide a comprehensive, highly detailed, and helpful, practical guide for the administration of cannabinoid-based medicines in a wide range of patient populations.
Fabritius M, Chtioui H, Battistella G, Annoni JM, Dao K, Favrat B, et al. Comparison of cannabinoid concentrations in oral fluid and whole blood between occasional and regular cannabis smokers prior to and after smoking a cannabis joint. Anal Bioanal Chem. 2013;405:9791–803. https://doi.org/10.1007/s00216-013-7412-1.
Lanz C, Mattsson J, Soydaner U, Brenneisen R. Medicinal Cannabis: in vitro validation of vaporizers for the smoke-free inhalation of Cannabis. PLoS One. 2016;11:e0147286. https://doi.org/10.1371/journal.pone.0147286.
Bar-Sela G, Vorobeichik M, Drawsheh S, Omer A, Goldberg V, Muller E. The medical necessity for medicinal cannabis: prospective, observational study evaluating the treatment in cancer patients on supportive or palliative care. Evidence-based Complement Altern Med. 2013;2013:1–8. https://doi.org/10.1155/2013/510392.
Bar-Lev Schleider L, Mechoulam R, Lederman V, Hilou M, Lencovsky O, Betzalel O, et al. Prospective analysis of safety and efficacy of medical cannabis in large unselected population of patients with cancer. Eur J Intern Med. 2018;49:37–43. https://doi.org/10.1016/j.ejim.2018.01.023.
Notcutt W, Langford R, Davies P, Ratcliffe S, Potts R. A placebo-controlled, parallel-group, randomized withdrawal study of subjects with symptoms of spasticity due to multiple sclerosis who are receiving long-term Sativex (nabiximols). Mult Scler J. 2012;18:219–28. https://doi.org/10.1177/1352458511419700.
Kutiel TS, Vornicova O, Bar-Sela G. Cannabis for Vismodegib-related muscle cramps in a patient with advanced basal cell carcinoma. J Pain Symptom Manag. 2018;55:e1–2. https://doi.org/10.1016/j.jpainsymman.2018.02.004.
Fine PG, Rosenfeld MJ. The endocannabinoid system, cannabinoids, and pain. Rambam Maimonides Med J. 2013;4:e0022. https://doi.org/10.5041/rmmj.10129.
Jensen B, Chen J, Furnish T, Wallace M. Medical marijuana and chronic pain: a review of basic science and clinical evidence. Curr Pain Headache Rep. 2015;19:50. https://doi.org/10.1007/s11916-015-0524-x.
Abrams DI. Integrating cannabis into clinical cancer care. Curr Oncol. 2016;23:8. https://doi.org/10.3747/co.23.3099.
Whiting PF, Wolff RF, Deshpande S, di Nisio M, Duffy S, Hernandez AV, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA - J Am Med Assoc. 2015;313:2456–73. https://doi.org/10.1001/jama.2015.6358.
Allan GM, Finley CR, Ton J, Perry D, Ramji J, Crawford K, et al. Systematic review of systematic reviews for medical cannabinoids. Can. Fam. Physician. 2018; A systematic review of systematic reviews to determine the effects of medical cannabinoids on pain, spasticity, and nausea and vomiting, and to identify adverse events.
Mücke M, Phillips T, Radbruch L, Petzke F, Häuser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD012182.pub2.
Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA - J Am Med Assoc. 2015;313:2474–83. https://doi.org/10.1001/jama.2015.6199.
Nugent SM, Morasco BJ, O'Neil ME, Freeman M, Low A, Kondo K, et al. The effects of cannabis among adults with chronic painandan overview of general harms a systematic review. Ann Intern Med. 2017;167:319. https://doi.org/10.7326/M17-0155.
Darkovska-Serafimovska M, Serafimovska T, Arsova-Sarafinovska Z, Stefanoski S, Keskovski Z, Balkanov T. Pharmacotherapeutic considerations for use of cannabinoids to relieve pain in patients with malignant diseases. J Pain Res. 2018. https://doi.org/10.2147/JPR.S160556 An extensive systematic review of eighteen randomized controlled trials (RCTs) to assess the efficacy of cannabis for relieving pain in patients with malignant diseases.
• Allan GM, Ramji J, Perry D, et al. Simplified guideline for prescribing medical cannabinoids in primary care. Can. Fam. Physician. 2018;1:1 A simplified medical cannabinoid prescribing guideline that provides practical recommendations for the use of medical cannabinoids in primary care.
Johnson JR, Burnell-Nugent M, Lossignol D, Ganae-Motan ED, Potts R, Fallon MT. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manag. 2010;39:167–79. https://doi.org/10.1016/j.jpainsymman.2009.06.008.
Johnson JR, Lossignol D, Burnell-Nugent M, Fallon MT. An open-label extension study to investigate the long-term safety and tolerability of THC/CBD oromucosal spray and oromucosal THC spray in patients with terminal cancer-related pain refractory to strong opioid analgesics. J Pain Symptom Manag. 2013;46:207–18. https://doi.org/10.1016/j.jpainsymman.2012.07.014.
Portenoy RK, Ganae-Motan ED, Allende S, Yanagihara R, Shaiova L, Weinstein S, et al. Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded-dose trial. J Pain. 2012;13:438–49. https://doi.org/10.1016/j.jpain.2012.01.003.
Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, et al. Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain. 2017;11:119–33. https://doi.org/10.1177/2049463717710042.
Nielsen S, Sabioni P, Trigo JM, Ware MA, Betz-Stablein BD, Murnion B, et al. Opioid-sparing effect of cannabinoids: a systematic review and meta-analysis. Neuropsychopharmacology. 2017;42:1752–65. https://doi.org/10.1038/npp.2017.51.
Abrams DI, Couey P, Shade SB, Kelly ME, Benowitz NL. Cannabinoid-opioid interaction in chronic pain. Clin Pharmacol Ther. 2011;90:844–51. https://doi.org/10.1038/clpt.2011.188.
Wilsey B, Marcotte T, Deutsch R, Gouaux B, Sakai S, Donaghe H. Low-dose vaporized cannabis significantly improves neuropathic pain. J Pain. 2013;14:136–48. https://doi.org/10.1016/j.jpain.2012.10.009.
Wilsey B, Marcotte T, Tsodikov A, Millman J, Bentley H, Gouaux B, et al. A randomized, placebo-controlled, crossover trial of Cannabis cigarettes in neuropathic pain. J Pain. 2008;9:506–21. https://doi.org/10.1016/j.jpain.2007.12.010.
Ettinger DS, Berger MJ, Barbour S, et al. Antiemesis, Version 1.2020, NCCN clinical practice guidelines in oncology in: Journal of the National Comprehensive Cancer Network. JNCCN J Natl Compr Cancer Netw. 2020. https://doi.org/10.6004/jnccn.2017.0117.
Van Sickle MD, Oland LD, Ho W, Hillard CJ, Mackie K, Davison JS, et al. Cannabinoids inhibit emesis through CB1 receptors in the brainstem of the ferret. Gastroenterology. 2001;121:767–74. https://doi.org/10.1053/gast.2001.28466.
Parker LA, Kwiatkowska M, Mechoulam R. Delta-9-tetrahydrocannabinol and cannabidiol, but not ondansetron, interfere with conditioned retching reactions elicited by a lithium-paired context in Suncus murinus: an animal model of anticipatory nausea and vomiting. Physiol Behav. 2006;87:66–71. https://doi.org/10.1016/j.physbeh.2005.08.045.
Sallan SE, Zinberg NE, Frei E. Antiemetic effect of delta-9-tetrahydrocannabinol in patients receiving cancer chemotherapy. N Engl J Med. 1975;293:795–7. https://doi.org/10.1056/NEJM197510162931603.
Meiri E, Jhangiani H, Vredenburgh JJ, Barbato LM, Carter FJ, Yang HM, et al. Efficacy of dronabinol alone and in combination with ondansetron versus ondansetron alone for delayed chemotherapy-induced nausea and vomiting. Curr Med Res Opin. 2007;23:533–43. https://doi.org/10.1185/030079907X167525.
Duran M, Pérez E, Abanades S, Vidal X, Saura C, Majem M, et al. Preliminary efficacy and safety of an oromucosal standardized cannabis extract in chemotherapy-induced nausea and vomiting. Br J Clin Pharmacol. 2010;70:656–63. https://doi.org/10.1111/j.1365-2125.2010.03743.x.
Machado Rocha FC, Stéfano SC, De Cássia HR, Rosa Oliveira LMQ, Da Silveira DX. Therapeutic use of Cannabis sativa on chemotherapy-induced nausea and vomiting among cancer patients: systematic review and meta-analysis. Eur J Cancer Care (Engl). 2008;17:431–43. https://doi.org/10.1111/j.1365-2354.2008.00917.x.
Tramèr MR, Carroll D, Campbell FA, Reynolds DJM, Moore RA, McQuay HJ. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. Br Med J. 2001;323:16–21. https://doi.org/10.1136/bmj.323.7303.16.
Ben Amar M. Cannabinoids in medicine: a review of their therapeutic potential. J Ethnopharmacol. 2006;105:1–25. https://doi.org/10.1016/j.jep.2006.02.001.
Lane M, Vogel CL, Ferguson J, Krasnow S, Saiers JL, Hamm J, et al. Dronabinol and prochlorperazine in combination for treatment of cancer chemotherapy-induced nausea and vomiting. J Pain Symptom Manag. 1991;6:352–9. https://doi.org/10.1016/0885-3924(91)90026-Z.
Bar-Sela G, Zalman D, Semenysty V, Ballan E. The effects of dosage-controlled Cannabis capsules on cancer-related cachexia and anorexia syndrome in advanced cancer patients: pilot study. Integr Cancer Ther. 2019;18:153473541988149. https://doi.org/10.1177/1534735419881498.
Brisbois TD, de Kock IH, Watanabe SM, Mirhosseini M, Lamoureux DC, Chasen M, et al. Delta-9-tetrahydrocannabinol may palliate altered chemosensory perception in cancer patients: results of a randomized, double-blind, placebo-controlled pilot trial. Ann Oncol. 2011;22:2086–93. https://doi.org/10.1093/annonc/mdq727.
Strasser F, Luftner D, Possinger K, Ernst G, Ruhstaller T, Meissner W, et al. Comparison of orally administered cannabis extract and delta-9- tetrahydrocannabinol in treating patients with cancer-related anorexia-cachexia syndrome: a multicenter, phase III, randomized, double-blind, placebo-controlled clinical trial from the Cannab. J Clin Oncol. 2006;24:3394–400. https://doi.org/10.1200/JCO.2005.05.1847.
Jatoi A, Windschitl HE, Loprinzi CL, Sloan JA, Dakhil SR, Mailliard JA, et al. Dronabinol versus megestrol acetate versus combination therapy for cancer-associated anorexia: a north central cancer treatment group study. J Clin Oncol. 2002;20:567–73. https://doi.org/10.1200/JCO.20.2.567.
Choi S, Huang BC, Gamaldo CE. Therapeutic uses of Cannabis on sleep disorders and related conditions. J Clin Neurophysiol. 2020. https://doi.org/10.1097/WNP.0000000000000617 A review that provides the latest evidence regarding the medical risks and potential therapeutic benefits of cannabis in managing patients with sleep disorders or those with sleep disturbance as associated comorbidity.
Eisenstein TK, Meissler JJ. Effects of cannabinoids on T-cell function and resistance to infection. J NeuroImmune Pharmacol. 2015;10:204–16. https://doi.org/10.1007/s11481-015-9603-3.
Zhu LX, Sharma S, Stolina M, Gardner B, Roth MD, Tashkin DP, et al. Δ-9-Tetrahydrocannabinol inhibits antitumor immunity by a CB2 receptor-mediated. Cytokine-Dependent Pathway J Immunol. 2000;165:373–80. https://doi.org/10.4049/jimmunol.165.1.373.
Chakravarti B, Ravi J, Ganju RK. Cannabinoids as therapeutic agents in cancer: current status and future implications. Oncotarget. 2014. https://doi.org/10.18632/oncotarget.2233.
McKallip RJ, Nagarkatti M, Nagarkatti PS. Δ-9-Tetrahydrocannabinol enhances breast cancer growth and metastasis by suppression of the antitumor immune response. J Immunol. 2005;174:3281–9. https://doi.org/10.4049/jimmunol.174.6.3281.
Taha T, Meiri D, Talhamy S, Wollner M, Peer A, Bar-Sela G. Cannabis impacts tumor response rate to nivolumab in patients with advanced malignancies. Oncologist. 2019;24:549–54. https://doi.org/10.1634/theoncologist.2018-0383.
•• Bar-Sela G, Cohen I, Campisi-Pinto S, et al. Cannabis consumption used by cancer patients during immunotherapy correlates with poor clinical outcome. Cancers (Basel). 2020;12:2447 The first clinical report to show that cannabis consumption correlated with a significant decrease in time to tumor progression and overall survival.
Turgeman I, Bar-Sela G. Cannabis for cancer–illusion or the tip of an iceberg: a review of the evidence for the use of cannabis and synthetic cannabinoids in oncology. Expert Opin Investig Drugs. 2019. https://doi.org/10.1080/13543784.2019.1561859 A review that covered the use of cannabis in all aspects in oncology and addressed immunological and antineoplastic effects in preclinical and clinical trials.
Alexander A, Smith PF, Rosengren RJ. Cannabinoids in the treatment of cancer. Cancer Lett. 2009;285:6–12. https://doi.org/10.1016/j.canlet.2009.04.005.
Pisanti S, Malfitano AM, Grimaldi C, Santoro A, Gazzerro P, Laezza C, et al. Use of cannabinoid receptor agonists in cancer therapy as palliative and curative agents. Best Pract Res Clin Endocrinol Metab. 2009;23:117–31. https://doi.org/10.1016/j.beem.2009.02.001.
Michalski CW, Oti FE, Erkan M, Sauliunaite D, Bergmann F, Pacher P, et al. Cannabinoids in pancreatic cancer: correlation with survival and pain. Int J Cancer. 2008;122:742–50. https://doi.org/10.1002/ijc.23114.
Blázquez C, Salazar M, Carracedo A, Lorente M, Egia A, González-Feria L, et al. Cannabinoids inhibit glioma cell invasion by down-regulating matrix metalloproteinase-2 expression. Cancer Res. 2008;68:1945–52. https://doi.org/10.1158/0008-5472.CAN-07-5176.
De Jesús ML, Hostalot C, Garibi JM, Sallés J, Meana JJ, Callado LF. Opposite changes in cannabinoid CB1 and CB2 receptor expression in human gliomas. Neurochem Int. 2010;56:829–33. https://doi.org/10.1016/j.neuint.2010.03.007.
Gómez Del Pulgar T, Velasco G, Guzmán M. The CB1 cannabinoid receptor is coupled to the activation of protein kinase B/Akt. Biochem J. 2000;347:369–73. https://doi.org/10.1042/0264-6021:3470369.
Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389–462. https://doi.org/10.1124/pr.58.3.2.
Scott KA, Dalgleish AG, Liu WM. Anticancer effects of phytocannabinoids used with chemotherapy in leukaemia cells can be improved by altering the sequence of their administration. Int J Oncol. 2017;51:369–77. https://doi.org/10.3892/ijo.2017.4022.
Donadelli M, Dando I, Zaniboni T, Costanzo C, Dalla Pozza E, Scupoli MT, et al. Gemcitabine/cannabinoid combination triggers autophagy in pancreatic cancer cells through a ROS-mediated mechanism. Cell Death Dis. 2011;2:e152. https://doi.org/10.1038/cddis.2011.36.
Miyato H, Kitayama J, Yamashita H, Souma D, Asakage M, Yamada J, et al. Pharmacological synergism between cannabinoids and paclitaxel in gastric cancer cell lines. J Surg Res. 2009;155:40–7. https://doi.org/10.1016/j.jss.2008.06.045.
Holland ML, Allen JD, Arnold JC. Interaction of plant cannabinoids with the multidrug transporter ABCC1 (MRP1). Eur J Pharmacol. 2008;591:128–31. https://doi.org/10.1016/j.ejphar.2008.06.079.
Holland ML, Panetta JA, Hoskins JM, Bebawy M, Roufogalis BD, Allen JD, et al. The effects of cannabinoids on P-glycoprotein transport and expression in multidrug resistant cells. Biochem Pharmacol. 2006;71:1146–54. https://doi.org/10.1016/j.bcp.2005.12.033.
Scott KA, Dalgleish AG, Liu WM. The combination of cannabidiol and Δ9-tetrahydrocannabinol enhances the anticancer effects of radiation in an orthotopic murine glioma model. Mol Cancer Ther. 2014;13:2955–67. https://doi.org/10.1158/1535-7163.MCT-14-0402.
Guzmán M, Duarte MJ, Blázquez C, Ravina J, Rosa MC, Galve-Roperh I, et al. A pilot clinical study of Δ9-tetrahydrocannabinol in patients with recurrent glioblastoma multiforme. Br J Cancer. 2006;95:197–203. https://doi.org/10.1038/sj.bjc.6603236.
Twelves C, Short S, Wright S. A two-part safety and exploratory efficacy randomized double-blind, placebo-controlled study of a 1:1 ratio of the cannabinoids cannabidiol and delta-9-tetrahydrocannabinol (CBD: THC) plus dose-intense temozolomide in patients with recurrent glioblastoma m. J Clin Oncol. 2017;35:2046. https://doi.org/10.1200/jco.2017.35.15_suppl.2046.
Foroughi M, Hendson G, Sargent MA, Steinbok P. Spontaneous regression of septum pellucidum/forniceal pilocytic astrocytomas - possible role of Cannabis inhalation. Childs Nerv Syst. 2011;27:671–9. https://doi.org/10.1007/s00381-011-1410-4.
Singh Y, Bali C. Cannabis extract treatment for terminal acute lymphoblastic leukemia with a Philadelphia chromosome mutation. Case Rep Oncol. 2013;6:585–92. https://doi.org/10.1159/000356446.
Bonn-Miller MO, ElSohly MA, Loflin MJE, Chandra S, Vandrey R. Cannabis and cannabinoid drug development: evaluating botanical versus single molecule approaches. Int Rev Psychiatry. 2018;30:277–84. https://doi.org/10.1080/09540261.2018.1474730.
Thomas BF, Wei X, Martin BR. Characterization and autoradiographic localization of the cannabinoid binding site in rat brain using [3H]11-OH-Δ9-THC-DMH. J Pharmacol Exp Ther. 1992;263(3):1383–90.
Karila L, Roux P, Rolland B, Benyamina A, Reynaud M, Aubin H-J, et al. Acute and long-term effects of Cannabis use: a review. Curr Pharm Des. 2014;20:4112–8. https://doi.org/10.2174/13816128113199990620.
Babor TF, Mendelson JH, Greenberg I, Kuehnle JC. Marijuana consumption and tolerance to physiological and subjective effects. Arch Gen Psychiatry. 1975;32:1548–52. https://doi.org/10.1001/archpsyc.1975.01760300086007.
Ware MA, Wang T, Shapiro S, Robinson A, Ducruet T, Huynh T, et al. Smoked cannabis for chronic neuropathic pain: a randomized controlled trial. CMAJ. 2010;182:E694–701. https://doi.org/10.1503/cmaj.091414.
Machado Bergamaschi M, Helena Costa Queiroz R, Waldo Zuardi A, Alexandre S, Crippa J. Safety and side effects of Cannabidiol, a Cannabis sativa constituent. Curr Drug Saf. 2011;6:237–49. https://doi.org/10.2174/157488611798280924.
Cyr C, Arboleda MF, Aggarwal SK, Balneaves LG, Daeninck P, Néron A, et al. Cannabis in palliative care: current challenges and practical recommendations. Ann Palliat Med. 2018. https://doi.org/10.21037/apm.2018.06.04 The authors address the challenges that were delaying the appropriate integration of cannabis into clinical practice and provide practical recommendations regarding patient assessment for the use of cannabis.
Lagerberg TV, Kvitland LR, Aminoff SR, Aas M, Ringen PA, Andreassen OA, et al. Indications of a dose-response relationship between cannabis use and age at onset in bipolar disorder. Psychiatry Res. 2014;215:101–4. https://doi.org/10.1016/j.psychres.2013.10.029.
Bar-Sela G, Tauber D, Mitnik I, Sheinman-Yuffe H, Bishara-Frolova T, Aharon-Peretz J. Cannabis-related cognitive impairment: a prospective evaluation of possible influences on patients with cancer during chemotherapy treatment as a pilot study. Anti-Cancer Drugs. 2018;30:91–7. https://doi.org/10.1097/CAD.0000000000000685.
Chadwick B, Miller ML, Hurd YL. Cannabis use during adolescent development: susceptibility to psychiatric illness. Front Psychiatry. 2013;4. https://doi.org/10.3389/fpsyt.2013.00129.
Kalant H. Adverse effects of cannabis on health: an update of the literature since 1996. Prog Neuro-Psychopharmacology Biol Psychiatry. 2004;28:849–63. https://doi.org/10.1016/j.pnpbp.2004.05.027.
Meier MH, Caspi A, Ambler A, Harrington HL, Houts R, Keefe RSE, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109:E2657–64. https://doi.org/10.1073/pnas.1206820109.
Tamm L, Epstein JN, Lisdahl KM, Molina B, Tapert S, Hinshaw SP, et al. Impact of ADHD and cannabis use on executive functioning in young adults. Drug Alcohol Depend. 2013;133:607–14. https://doi.org/10.1016/j.drugalcdep.2013.08.001.
Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA. Cannabinoid hyperemesis syndrome: diagnosis, pathophysiology, and treatment—a systematic review. J Med Toxicol. 2017;13:71–87. https://doi.org/10.1007/s13181-016-0595-z.
Allsop DJ, Copeland J, Norberg MM, Fu S, Molnar A, Lewis J, et al. Quantifying the clinical significance of Cannabis withdrawal. PLoS One. 2012;7:e44864. https://doi.org/10.1371/journal.pone.0044864.
Hesse M, Thylstrup B. Time-course of the DSM-5 cannabis withdrawal symptoms in poly-substance abusers. BMC Psychiatry. 2013;13. https://doi.org/10.1186/1471-244X-13-258.
Bahji A, Stephenson C, Tyo R, Hawken ER, Seitz DP. Prevalence of Cannabis withdrawal symptoms among people with regular or dependent use of cannabinoids: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e202370. https://doi.org/10.1001/jamanetworkopen.2020.2370.
Aggarwal SK. Use of cannabinoids in cancer care: palliative care. Curr Oncol. 2016;23:33. https://doi.org/10.3747/co.23.2962.
Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59:478–92. https://doi.org/10.1373/clinchem.2012.194381.
Chacko JA, Heiner JG, Siu W, Macy M, Terris MK. Association between marijuana use and transitional cell carcinoma. Urology. 2006;67:100–4. https://doi.org/10.1016/j.urology.2005.07.005.
Callaghan RC, Allebeck P, Sidorchuk A. Marijuana use and risk of lung cancer: a 40-year cohort study. Cancer Causes Control. 2013;24:1811–20. https://doi.org/10.1007/s10552-013-0259-0.
Feng BJ, Khyatti M, Ben-Ayoub W, Dahmoul S, Ayad M, Maachi F, et al. Cannabis, tobacco, and domestic fumes intake are associated with nasopharyngeal carcinoma in North Africa. Br J Cancer. 2009;101:1207–12. https://doi.org/10.1038/sj.bjc.6605281.
Berthiller J, Straif K, Boniol M, Voirin N, Benhaïm-Luzon V, Ayoub WB, et al. Cannabis smoking and risk of lung cancer in men: a pooled analysis of three studies in Maghreb. J Thorac Oncol. 2008;3:1398–403. https://doi.org/10.1097/JTO.0b013e31818ddcde.
Callaghan RC, Allebeck P, Akre O, McGlynn KA, Sidorchuk A. Cannabis use and incidence of testicular cancer: a 42-year follow-up of Swedish men between 1970 and 2011. Cancer Epidemiol Biomark Prev. 2017;26:1644–52. https://doi.org/10.1158/1055-9965.EPI-17-0428.
Berthiller J, Lee YCA, Boffetta P, Wei Q, Sturgis EM, Greenland S, et al. Marijuana smoking and the risk of head and neck cancer: pooled analysis in the INHANCE consortium. Cancer Epidemiol Biomark Prev. 2009;18:1544–51. https://doi.org/10.1158/1055-9965.EPI-08-0845.
Liang C, McClean MD, Marsit C, Christensen B, Peters E, Nelson HH, et al. A population-based case-control study of marijuana use and head and neck squamous cell carcinoma. Cancer Prev Res. 2009;2:759–68. https://doi.org/10.1158/1940-6207.CAPR-09-0048.
Abrams DI, Guzman M. Cannabis in Cancer care. Clin Pharmacol Ther. 2015;97:575–86. https://doi.org/10.1002/cpt.108.
Borgelt LM, Franson KL, Nussbaum AM, Wang GS. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy. 2013;33:195–209. https://doi.org/10.1002/phar.1187.
Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60. https://doi.org/10.2165/00003088-200342040-00003.
Sachse-Seeboth C, Pfeil J, Sehrt D, Meineke I, Tzvetkov M, Bruns E, et al. Interindividual variation in the pharmacokinetics of Δ9- tetrahydrocannabinol as related to genetic polymorphisms in CYP2C9. Clin Pharmacol Ther. 2009;85:273–6. https://doi.org/10.1038/clpt.2008.213.
Lindsey WT, Stewart D, Childress D. Drug interactions between common illicit drugs and prescription therapies. Am J Drug Alcohol Abuse. 2012;38:334–43. https://doi.org/10.3109/00952990.2011.643997.
Grayson L, Vines B, Nichol K, Szaflarski JP. An interaction between warfarin and cannabidiol, a case report. Epilepsy Behav Case Reports. 2018;9:10–1. https://doi.org/10.1016/j.ebcr.2017.10.001.
Gaston TE, Bebin EM, Cutter GR, Liu Y, Szaflarski JP. Interactions between cannabidiol and commonly used anti-epileptic drugs. Epilepsia. 2017;58:1586–92. https://doi.org/10.1111/epi.13852.
Engels FK, de Jong FA, Sparreboom A, Mathot RAA, Loos WJ, Kitzen JJEM, et al. Medicinal Cannabis does not influence the clinical pharmacokinetics of irinotecan and docetaxel. Oncologist. 2007;12:291–300. https://doi.org/10.1634/theoncologist.12-3-291.
Cyr C, Arboleda MF, Aggarwal SK, Balneaves LG, Daeninck P, Néron A, et al. Erratum to cannabis in palliative care: current challenges and practical recommendations (Ann Palliat Med 2018, 7, 463-77). Ann Palliat Med. 2019. https://doi.org/10.21037/apm.2019.01.06.
Sznitman SR, Goldberg V, Sheinman-Yuffe H, Flechter E, Bar-Sela G. Storage and disposal of medical cannabis among patients with cancer: assessing the risk of diversion and unintentional digestion. Cancer. 2016;122:3363–70. https://doi.org/10.1002/cncr.30185.
Pergam SA, Woodfield MC, Lee CM, Cheng GS, Baker KK, Marquis SR, et al. Cannabis use among patients at a comprehensive cancer center in a state with legalized medicinal and recreational use. Cancer. 2017;123:4488–97. https://doi.org/10.1002/cncr.30879.
Braun IM, Wright A, Peteet J, Meyer FL, Yuppa DP, Bolcic-Jankovic D, et al. Medical oncologists’ beliefs, practices, and knowledge regarding marijuana used therapeutically: a nationally representative survey study. J Clin Oncol. 2018;36:1957–62. https://doi.org/10.1200/JCO.2017.76.1221.
Karanges EA, Suraev A, Elias N, Manocha R, McGregor IS. Knowledge and attitudes of Australian general practitioners towards medicinal cannabis: a cross-sectional survey. BMJ Open. 2018;8:e022101. https://doi.org/10.1136/bmjopen-2018-022101.
Funding
Dr. Idan Cohen is supported by the Israeli Cancer Association (ICA) (Grant number 20200021) and the Israel Ministry of Health, together with Prof. Gil Bar-Sela (Grant number 3000015198).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gil Bar-Sela declares no conflict of interest. Mahmoud Abu-Amna declares no conflict of interest. Talal Salti declares no conflict of interest. Mona Khoury declares no conflict of interest. Idan Cohen declares no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Palliative and Supportive Care
Rights and permissions
About this article
Cite this article
Abu-Amna, M., Salti, T., Khoury, M. et al. Medical Cannabis in Oncology: a Valuable Unappreciated Remedy or an Undesirable Risk?. Curr. Treat. Options in Oncol. 22, 16 (2021). https://doi.org/10.1007/s11864-020-00811-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-020-00811-2