Opinion statement
Treatment-related cardiotoxicity remains a significant concern for breast cancer patients undergoing cancer treatment and extends into the survivorship period, with adverse cardiovascular (CV) outcomes further compounded by the presence of pre-existing CV disease or traditional CV risk factors. Awareness of the cardiotoxicity profiles of contemporary breast cancer treatments and optimization of CV risk factors are crucial in mitigating cardiotoxicity risk. Assessment of patient- and treatment-specific risk with appropriate CV surveillance is another key component of care. Mismatch between baseline cardiotoxicity risk and intensity of cardiotoxicity surveillance can lead to unnecessary downstream testing, increased healthcare expenditure, and interruption or discontinuation of potentially life-saving treatment. Efforts to identify early imaging and/or circulating biomarkers of cardiotoxicity and develop effective management strategies are needed to optimize the CV and cancer outcomes of breast cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer diagnosis and cause of cancer death among females worldwide [1], but advances in breast cancer care have led to a growing population of survivors with an estimated ~ 3 million breast cancer survivors in the USA [2•]. Breast cancer and cardiovascular disease (CVD) share many common risk factors such as age, obesity, and tobacco use, and breast cancer outcomes can be affected by the presence of pre-existing CVD or other cardiovascular (CV) comorbidities [2•, 3, 4]. Furthermore, current breast cancer treatment options are associated with CV toxicities that can offset expected therapeutic benefits, disrupt the cancer treatment course, and adversely affect quality of life.
The goal of this review is to provide an update on the CV toxicities associated with contemporary breast cancer treatment.
Anthracyclines
Anthracyclines are one of the most widely used chemotherapeutic agents for the treatment of breast cancer [5]. Chronic progressive dose-dependent cardiomyopathy is the characteristic presentation of anthracycline-induced cardiotoxicity. Inhibition of topoisomerase-2β is a key mediator between interrelated pathways of injury that lead to oxidative stress, mitochondrial dysfunction, and cardiomyocyte apoptosis [6, 7]. An analysis of three studies comprised mostly of breast cancer patients showed a 5% incidence of symptomatic heart failure (HF) at a cumulative doxorubicin dose of 400 mg/m2, increasing to 48% at 700 mg/m2 [8]. A surveillance study on anthracycline-induced cardiotoxicity in 2625 patients (51% with breast cancer) demonstrated a median time to onset of 3.5 months after completion of anthracyclines, with almost all cases occurring within 1 year after treatment completion, at an estimated 9% increased risk per 50 mg/m2 increment of doxorubicin [9•].
Cumulative anthracycline dose is a well-recognized risk factor for development of cardiotoxicity. Based on a recent guideline from the American Society of Clinical Oncology (ASCO), “high dose” is regarded as a cumulative dose of doxorubicin ≥ 250 mg/m2 or epirubicin ≥ 600 mg/m2 [10••]. In the adjuvant setting, anthracycline doses are typically below this threshold, and a significant decline of left ventricular ejection fraction (LVEF) or HF can occur in ~ 9–10% and ~ 0.6–1.3% of patients, respectively [9•, 11, 12]. Other risk factors include older age, CV comorbidities (particularly hypertension), and exposure to chest radiation therapy (RT) or other sequential cardiotoxic therapies [8, 10••, 11, 13]. Strategies to mitigate anthracycline-induced cardiotoxicity including continuous versus bolus administration, liposomal formulation of doxorubicin, and cardioprotective agents such as dexrazoxane can reduce the risk of cardiotoxicity and should be considered in patients with metastatic breast cancer requiring high doses of anthracyclines [10••]. Dexrazoxane, which chelates iron and prevents free radical generation, afforded about a 65–80% lower risk of LV dysfunction among patients receiving high doses of anthracyclines with no clear effect on treatment efficacy [14, 15].
Targeted therapies
Anti-HER2 agents
It is estimated that ~ 20–25% of all breast cancers amplify or overexpress human epidermal growth factor 2 (HER2 or ErbB2), a transmembrane tyrosine kinase receptor, conferring a poor prognosis [13]. Anti-HER2 agents have significantly improved the course and survival of patients with early or advanced HER2-positive breast cancer and formed the cornerstone of therapy. Trastuzumab was the first anti-HER2 agent approved for use in this treatment setting, and several additional targeted therapies have since been developed.
Trastuzumab
Cardiotoxicity with trastuzumab was first recognized in patients with metastatic breast cancer undergoing concurrent treatment with anthracyclines [13]. Trastuzumab is a humanized monoclonal antibody that binds to the extracellular domain IV of HER2. The mechanism of cardiotoxicity is thought to be due to interference of the cardioprotective effects of neuregulin-1/HER downstream signaling, with increased susceptibility of cardiomyocytes especially after anthracycline exposure [16]. In randomized controlled trials where trastuzumab is administered sequentially after anthracyclines, corresponding rates of LVEF decline and HF range between 4.4–18.6% and 0.8–4.1%, respectively [11, 12, 17, 18]. Retrospective claims-based studies show significantly higher rates of cardiotoxicity, up to 32–42%, among patients receiving trastuzumab with or without anthracyclines [19, 20]. This discrepancy between clinical trials versus real-world data could stem from differences in patient characteristics and/or overestimation of CV endpoints with claims-based data. The incidence of asymptomatic LV dysfunction and HF with non-anthracycline trastuzumab-based regimens is lower (3.2–9.4% and 0.4–0.5%, respectively) [18, 21•].
Cardiac dysfunction most commonly occurs within 2 years of treatment initiation [11, 17], but increased long-term HF or cardiomyopathy risk and persistent subclinical changes have also been demonstrated [18, 20, 22, 23]. Banke et al. showed that compared with chemotherapy alone, the combination of chemotherapy with trastuzumab for adjuvant treatment was associated with a twofold increased risk of late-onset HF [23]. Importantly, treatment interruption occurs in 15–20% of patients due to cardiotoxicity [11, 24]. In contrast to anthracyclines, partial to complete LVEF recovery is common and can be seen in up to 80% of patients by 6–7 months with treatment interruption, spontaneously or with medical treatment [24,25,26], and some patients are able to tolerate rechallenge with trastuzumab [24]. In addition to anthracycline exposure, other risk factors include older age, concomitant CV risk factors and comorbidities, and lower baseline LVEF [11, 12, 27]. There have been efforts to develop risk prediction models for trastuzumab cardiotoxicity; however, additional studies are needed to validate these models in larger populations and to demonstrate that use of these prediction models can improve CV outcomes before they can be translated into clinical practice [11, 27].
Pertuzumab
Pertuzumab binds to the extracellular domain II of HER2 and complements the activity of trastuzumab by blocking HER2 dimerization, and it is used in the neoadjuvant, adjuvant, and metastatic settings [28,29,30,31]. Long-term follow-up studies demonstrate that addition of pertuzumab to trastuzumab does not increase the risk of cardiotoxicity beyond the risk associated with single-agent trastuzumab combined with standard chemotherapy [28,29,30,31].
Ado-trastuzumab emtansine
Ado-trastuzumab emtansine (T-DM1) is a conjugate of trastuzumab with a cytotoxic microtubule inhibitor that enables intracellular drug delivery to HER2-overexpressing cells, minimizing effects on normal tissue [32]. It is approved in the metastatic setting for patients who have progressed after prior treatment with trastuzumab and more recently has shown benefit in the early-stage setting among patients with residual disease after neoadjuvant therapy with a taxane and trastuzumab [32, 33]. In a phase III trial of T-DM1 for early breast cancer, only one (0.1%) cardiac event (severe HF or cardiac death) has been reported after a median follow-up of 40 months [33].
Anti-HER2 tyrosine kinase inhibitors
Lapatinib is an oral reversible small-molecule tyrosine kinase inhibitor (TKI) against epidermal growth factor receptor (EGFR), HER1, and HER2 and is approved for use in combination with capecitabine or letrozole in patients with progressive metastatic HER2-positive breast cancer [34]. A pooled analysis of phase I–III trials of 3689 patients showed an incidence of cardiac events of 1.6% (1.4% asymptomatic, 0.2% symptomatic) occurring at a mean of 13 weeks, with an average absolute LVEF decline of 18.8% from baseline, and partial or full recovery by 7.6 weeks in the majority of patients [35]. Trials in treatment-naïve [36, 37] and pre-treated [38,39,40] early and advanced breast cancer patients demonstrate a low incidence of cardiac events (< 5% overall, ~ 1% severe) and no intensification of cardiotoxicity when used in combination with other therapies [35]. Lapatinib has also been associated with rare arrhythmias and QTc prolongation to > 500 ms in about 6% of patients, although no cases of torsades de pointes have been reported [41].
Neratinib is an oral irreversible small-molecule TKI that binds to and inhibits HER1, HER2, and HER4 and that received FDA approval in 2017 for extended adjuvant therapy of HER2-positive early-stage breast cancer after 1 year of trastuzumab [42,43,44]. Two trials in early and advanced HER2-positive breast cancer did not show evidence of early neratinib-related cardiotoxicity, although these trials enrolled low-risk patients with no significant cardiac comorbidities [42, 43].
Cyclin-dependent kinase 4/6 inhibitors
Cyclin-dependent kinase (CDK) 4/6 inhibitors such as abemaciclib, palbociclib, and ribociclib are used in conjunction with endocrine therapy (aromatase inhibitors (AIs) or fulvestrant) in patients with hormone receptor–positive, HER2-negative advanced breast cancer. They inhibit tumor growth by regulating the retinoblastoma pathway, causing cell cycle arrest [45]. A meta-analysis of phase II and phase III studies demonstrated a 3.5-fold increased risk of venous thromboembolism when CDK 4/6 inhibitors were added to endocrine therapy [46]. In addition, a phase I study of ribociclib demonstrated dose-dependent QTc prolongation starting at 600 mg/day [45]. The product label for ribociclib recommends periodic QTc monitoring at baseline, at day 14, at the beginning of cycle 2 (day 28), and thereafter as clinically indicated, with dose reduction and/or interruption for QTc prolongation [47].
Endocrine therapy
Endocrine therapy with tamoxifen or third-generation AIs such as anastrozole, letrozole, and exemestane is recommended as long-term adjuvant therapy in early disease or as first-line therapy in advanced disease in women with hormone receptor–positive disease [48]. Tamoxifen is a selective estrogen receptor modulator that affects downstream estrogen signaling, while AIs interfere with endogenous estrogen production in adipose tissue. Although AIs have shown superior disease benefit over tamoxifen, there is concern that they carry a greater CV risk. A meta-analysis of RCTs estimates a 19% increased risk for CV events with AIs compared with tamoxifen, although AIs were not associated with an increased risk compared with placebo [49]. These findings suggest that the increased CV risk attributed to AIs is driven by the cardioprotective benefit of tamoxifen rather than harm associated with AIs [49]. Tamoxifen has been associated with favorable lipid changes, while AIs with unchanged or unfavorable lipid parameters [50, 51]. Incident hypertension of up to 13% [52] and evidence of significant vascular dysfunction [53] were more common with AIs. On the other hand, increased thrombogenicity has been demonstrated with tamoxifen—almost a twofold increased risk and up to 5% rate of venous thromboembolism [51, 52]. Questions regarding the clinical implications of these cardiometabolic changes remain, as CV deaths remain unchanged and an improved overall survival has been demonstrated with AIs over tamoxifen [51, 54].
Radiation-induced ischemic heart disease
Incidental radiation of cardiac structures during breast cancer therapy creates an inflammatory and profibrotic environment that can lead to endothelial dysfunction, accelerated atherosclerosis, and myocardial fibrosis, which can manifest clinically as coronary artery disease or cardiomyopathy [55]. Survivors have a 2 to 5.9 times increased risk of radiation-induced heart disease (RIHD), augmented by factors such as younger age at exposure and treatment with other cardiotoxic therapies, CVD, and CV risk factors [56]. Darby et al. [57] demonstrated a 7.4% increased risk of major coronary events per Gy of mean heart dose (MHD), beginning within the first few years after radiation exposure and continuing after 20 years. Patients receiving left-sided versus right-sided RT have a 29% and 22% increased risk for coronary heart disease and cardiac death, respectively [58]. The left ventricular apex and left anterior descending coronary artery segments are particularly vulnerable to higher doses of radiation exposure given their proximity to the anterior chest wall [59,60,61]; thus, parameters other than MHD such as left ventricular volumes receiving 5 Gy have been studied, though further validation is required [62].
Contemporary RT techniques aimed at minimizing cardiac exposure such as CT-based simulation, prone imaging, respiratory gating, heart blocks, intensity-modulated radiation therapy, and volumetric modulated arc therapy have substantially reduced the radiation dose to the heart [63]. Impact of further reduction in MHD remains unknown, given the long latency period between radiation exposure and clinical CV events. Proton therapy is an alternative radiation technique that further minimizes radiation dose to the heart beyond what is achievable with conventional photon-based radiation techniques. The RADCOMP trial (NCT02603341) is a randomized trial that will compare 10-year CV outcomes among patients undergoing proton versus photon RT.
Prevention, detection, and management of cardiotoxicity
Pre-treatment evaluation of CVD risk is recommended prior to initiation of cardiotoxic cancer treatment. This includes a comprehensive history, physical examination, and baseline LVEF assessment. Screening and active management of pre-existing CVD and/or CV risk factors according to society guidelines are recommended throughout the treatment duration [10••].
Primary prevention
Several studies have evaluated the efficacy of prophylactic renin-angiotensin system–blocking and beta-blocking agents to prevent LV systolic dysfunction associated with adjuvant anthracycline and/or trastuzumab therapy in patients with early breast cancer (Table 1). The PRADA trial [64] randomized patients receiving an epirubicin-based regimen to candesartan, metoprolol succinate, or placebo. Those on candesartan, but not metoprolol, had a small yet significant attenuation of LVEF decline as measured by cardiac magnetic resonance imaging (CMR). Of note, only 22% of patients in the PRADA trial were treated with a high-risk regimen of anthracyclines plus trastuzumab. The CECCY trial randomized a homogenous cohort of HER2-negative patients scheduled to start ACT (anthracycline, cyclophosphamide, and taxane; cumulative doxorubicin dose 240 mg/m2) to carvedilol or placebo [65]. There was no difference in LVEF reduction among those on carvedilol versus placebo, although fewer patients developed diastolic dysfunction and troponin (Tn) elevation. In the MANTICORE study, a modest but significant attenuation in LVEF decline was noted with bisoprolol versus perindopril or placebo among patients receiving trastuzumab, although there was no difference in the primary endpoint of cardiac remodeling between the treatment groups. Notably, treatment interruption due to cardiac dysfunction was more common in the placebo group [67]. Among patients treated with anthracyclines followed by trastuzumab, a study by Boekhout et al. [66] did not demonstrate any cardioprotective benefit with candesartan, although a limitation of this study was that candesartan was not initiated until after completion of the anthracycline course. However, recent findings by Guglin et al. show that lisinopril and carvedilol are effective for preventing LVEF decline in a subset of breast cancer patients treated with anthracyclines and trastuzumab [68•]. A common limitation of these trials was that they included mostly low-risk patients with few CV comorbidities or patients receiving low-risk treatment regimens, and this may account for the modest benefits seen with primary prevention strategies. A primary prevention strategy targeting a higher-risk patient population may yield a greater clinical benefit.
Statins have been proposed as a preventive medication for anthracycline cardiotoxicity given their multiple pleiotropic effects including both anti-inflammatory and antioxidant properties [69, 70]. In a retrospective cohort study, Seicean et al. demonstrated that statin use during anthracycline therapy was associated with a decreased risk of incident HF [71]. A prospective trial investigating the prophylactic value of atorvastatin in patients planned for adjuvant anthracycline treatment is ongoing (PREVENT, ClinicalTrials.gov Identifier: NCT01988571).
Early detection and management of treatment-related cardiotoxicity
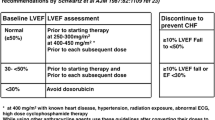
Current recommendations for surveillance of treatment-related cardiotoxicity entail routine LVEF assessments during and after anthracycline and anti-HER2 therapy [72, 73]. A schedule of LVEF assessments at baseline and every 3 months during trastuzumab treatment is most commonly cited [73]. Adherence to this cardiac monitoring schedule is generally poor (< 50%) irrespective of age or other CV comorbidities [74, 75•]. However, the value of frequent monitoring to improve outcomes among low-risk patients has been questioned, especially among patients with HER2-positive breast cancer receiving non-anthracycline-based regimens in which the risk of cardiotoxicity is low. Potential harms of treatment interruption or false-positive findings leading to unnecessary testing associated with frequent LVEF monitoring must be balanced with the CV risks associated with LVEF declines [76]. Data from several small studies suggest that patients with asymptomatic LVEF decline can safely continue anti-HER2 therapy with close cardiac monitoring and treatment with cardiac medications, although additional safety studies are warranted [77•, 78].
Recent efforts have focused on identifying early sensitive markers of cardiotoxicity prior to the overt impairment of LV systolic function. Global longitudinal strain (GLS) via speckle tracking echocardiography (STE) is a sensitive marker of LV systolic function and can detect early signs of cardiotoxicity [79]. The predictive value of GLS for subsequent cardiotoxicity among patients receiving trastuzumab with or without prior anthracyclines has also been demonstrated [80,81,82]. Negishi et al. showed that a change in GLS from baseline to 6 months of 11% (95% confidence interval 8.3–14.6%) was the strongest predictor of cardiotoxicity among trastuzumab-treated patients [80]. Based on American Society of Echocardiography (ASE) guidelines, a relative decrease in GLS of > 15% is likely to reflect a clinically significant change in LV systolic function that may warrant further intervention [72]. GLS has also been used to detect subclinical signs of radiation-induced cardiotoxicity, with declines in GLS that correspond to areas receiving the highest dose of radiation [60, 83]. However, a recent study showed no significant change in GLS after contemporary breast RT among patients treated with anthracyclines and trastuzumab, which may be explained by the low mean heart dose that is delivered with contemporary RT techniques [63].
The value of more sensitive markers of cardiotoxicity is dependent on whether CV outcomes can be improved with early detection and intervention. The ICOS-ONE study compared prophylactic versus Tn-triggered initiation of enalapril for the prevention of anthracycline-induced cardiotoxicity among patients receiving a median doxorubicin equivalent dose of 180 mg/m2. While enalapril did not decrease the risk of troponin elevation during treatment, the incidence of cardiotoxicity was lower in both groups (1.1%) compared with prior studies, suggesting the potential role of enalapril in preventing anthracycline-induced cardiotoxicity [84]. The SUCCOUR trial is a prospective trial that will compare a strategy of LVEF versus GLS-guided initiation of cardioprotective therapy for anthracycline-induced cardiotoxicity among high-risk patients (88% breast cancer) [85••].
CMR in patients receiving cardiotoxic cancer therapy can be used to provide superior image resolution for more accurate assessments of LV volumes and function and to characterize myocardial tissue [72, 86]. Detection of early stages of cardiac injury as evidenced by myocardial inflammation and edema has been demonstrated based on early gadolinium enhancement and T1/T2 mapping [86, 87]. Based on a recent study of serial multiparametric CMR assessments in the pig model, prolonged T2 relaxation time was found to be the earliest marker of anthracycline-induced cardiotoxicity, consistent with increased intracardiomyocyte edema on pathologic correlates [87]. This finding reflected a reversible stage of cardiotoxicity that—if confirmed with further studies—can have significant clinical implications in cardioprotective strategies and continued anthracycline therapy [87, 88]. CMR-based assessment of LV volumes may also help to identify the etiology of LVEF declines during cancer treatment. Cardiotoxicity as defined by reductions in LVEF is generally thought to be caused by impairment of LV contractility. However, LVEF declines in the setting of cardiotoxic cancer therapy can be attributed to isolated declines in LV preload, in which the appropriate treatment may be to provide volume repletion rather than to discontinue cancer therapy and/or initiate cardioprotective medications [89].
With regard to circulating biomarkers, several studies have demonstrated that post-anthracycline Tn elevations portend an increased risk of future cardiotoxicity [81, 84, 90]. Among patients receiving adjuvant anthracycline followed by paclitaxel and trastuzumab, Ky et al. showed that early increases in TnI and myeloperoxidase conferred up to a 46.5% increased risk of cardiotoxicity [90]. Cardinale et al. [91] showed that TnI elevations were associated with an increased risk of trastuzumab-induced cardiotoxicity and lower likelihood of LVEF recovery. The integration of circulating and imaging biomarkers, particularly among selected individuals at high cardiotoxicity risk (e.g., patients receiving sequential anthracyclines and trastuzumab), may provide the greatest predictive value of cardiotoxicity and prove to be most beneficial in clinical practice.
Despite the currently identified clinical factors that are associated with cardiotoxicity, there continues to be significant heterogeneity in the tolerance to cardiotoxic cancer therapy. This suggests that genetics may provide insight into an individual’s susceptibility to cardiotoxicity. Changes in gene expression in response to cardiotoxic cancer therapy [92] and single nucleotide polymorphisms (SNPs) in genes involved in anthracycline metabolism and oxidative stress such as ABCC2, CYBA, RAC2, ABCB1, and CBR3 have been proposed as markers that can identify patients at high risk for anthracycline-induced cardiotoxicity [93,94,95]. Candidate SNPs such as the HER2/neu Pro 1170 Ala polymorphism have also been identified as potential genetic markers of trastuzumab cardiotoxicity [66, 95,96,97]. Additional studies are needed to further explore the relationship between these genetic markers and cardiotoxicity events.
Exercise and fitness
Weight gain, decreased physical activity, and impaired exercise capacity are common changes among breast cancer patients after initial diagnosis and during treatment [98, 99]. Jones et al. showed that patients and survivors have on average 27% less exercise capacity than age-matched healthy sedentary controls [99]. Moreover, a strong inverse relationship between CVD and increasing physical activity has been demonstrated, with benefits that persisted long term [100]. The “multiple hit” model emphasizes that pre-existing CV risk factors combined with therapy-associated CV injury can lead to direct and indirect effects on the global CV system, eventually resulting in CVD [101]. Accordingly, the safety and potential CV benefits of exercise during and after treatment have previously been shown [98, 102,103,104]. The OptiTrain trial demonstrated that high-intensity interval training (HIIT) during treatment offered multiple benefits, including prevention of cardiorespiratory fitness decline and cancer-related fatigue and improvement in muscle strength [104]. Several prospective trials are ongoing to evaluate the effect of exercise interventions on cancer- and CV-related outcomes [105, 106].
Conclusion
As advances in cancer care continue to improve upon the cancer outcomes of breast cancer patients, more survivors will be at risk for developing late adverse CV effects from cancer treatment or overt CVD. Balancing the expected benefits of cancer treatment with treatment- and patient-specific CV risk and identifying strategies to prevent cardiotoxicity are needed to improve long-term outcomes and quality of life. Increased knowledge of imaging and circulating biomarkers has translated to earlier identification of subclinical cardiotoxicity and provides an opportunity for early intervention prior to the development of overt clinical CVD. Moreover, increasing awareness of insults to the CV system associated with cardiotoxic cancer treatment has created strides towards novel multidisciplinary approaches to the cardio-oncology care of breast cancer patients. Continued collaborative efforts within cardio-oncology will lead to better CV and cancer outcomes in cancer survivors.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
• Mehta LS, Watson KE, Barac A, Beckie TM, Bittner V, Cruz-Flores S, et al. Cardiovascular disease and breast cancer: where these entities intersect: a scientific statement from the American Heart Association. Circulation. 2018;137(8):e30–66. https://doi.org/10.1161/CIR.0000000000000556 This is the first American Heart Association scientific statement providing a comprehensive evidence-based discussion on the association between breast cancer and CVD.
Abdel-Qadir H, Austin PC, Lee DS, Amir E, Tu JV, Thavendiranathan P, et al. A population-based study of cardiovascular mortality following early-stage breast cancer. JAMA Cardiol. 2017;2(1):88–93. https://doi.org/10.1001/jamacardio.2016.3841.
Hershman DL, Till C, Shen S, Wright JD, Ramsey SD, Barlow WE, et al. Association of cardiovascular risk factors with cardiac events and survival outcomes among patients with breast cancer enrolled in SWOG Clinical Trials. J Clin Oncol. 2018;36(26):2710–7. https://doi.org/10.1200/JCO,10.1200/JCO.2017.
Blum JL, Flynn PJ, Yothers G, Asmar L, Geyer CE Jr, Jacobs SA, et al. Anthracyclines in early breast cancer: the ABC trials—USOR 06-090, NSABP B-46-I/USOR 07132, and NSABP B-49 (NRG Oncology). J Clin Oncol. 2017;35(23):2647–55. https://doi.org/10.1200/JCO,10.1200/JCO.2016.
Zhang S, Liu X, Bawa-Khalfe T, Lu LS, Lyu YL, Liu LF, et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med. 2012;18(11):1639–42. https://doi.org/10.1038/nm.2919.
Octavia Y, Tocchetti CG, Gabrielson KL, Janssens S, Crijns HJ, Moens AL. Doxorubicin-induced cardiomyopathy: from molecular mechanisms to therapeutic strategies. J Mol Cell Cardiol. 2012;52(6):1213–25. https://doi.org/10.1016/j.yjmcc.2012.03.006.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79. https://doi.org/10.1002/cncr.11407.
• Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131(22):1981–8. https://doi.org/10.1161/CIRCULATIONAHA.114.013777 This is a surveillance study among adult patients characterizing the incidence, timing, risk factors, and trend of anthracycline-induced cardiotoxicity over a median follow-up of 5.2 years. It also showed that partial or full LVEF recovery after prompt initiation of HF therapy occurred in the majority of those who developed cardiotoxicity.
•• Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2017;35(8):893–911. https://doi.org/10.1200/JCO.2016.70.5400 This contains guideline recommendations based on available evidence and expert consensus describing the approach to adult cancer survivors before, during, and after cancer treatment. It also identified evidence gaps and future directions particularly relevant in the field of cardio-oncology.
Romond EH, Jeong JH, Rastogi P, Swain SM, Geyer CE Jr, Ewer MS, et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2012;30(31):3792–9. https://doi.org/10.1200/JCO.2011.40.0010.
Advani PP, Ballman KV, Dockter TJ, Colon-Otero G, Perez EA. Long-term cardiac safety analysis of NCCTG N9831 (Alliance) adjuvant trastuzumab trial. J Clin Oncol. 2016;34(6):581–7. https://doi.org/10.1200/JCO.2015.61.8413.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
Marty M, Espie M, Llombart A, Monnier A, Rapoport BL, Stahalova V, et al. Multicenter randomized phase III study of the cardioprotective effect of dexrazoxane (Cardioxane) in advanced/metastatic breast cancer patients treated with anthracycline-based chemotherapy. Ann Oncol. 2006;17(4):614–22. https://doi.org/10.1093/annonc/mdj134.
Swain SM, Whaley FS, Gerber MC, Weisberg S, York M, Spicer D, et al. Cardioprotection with dexrazoxane for doxorubicin- containing therapy in advanced breast cancer. J Clin Oncol. 1997;15:1318–32.
Tocchetti CG, Ragone G, Coppola C, Rea D, Piscopo G, Scala S, et al. Detection, monitoring, and management of trastuzumab-induced left ventricular dysfunction: an actual challenge. Eur J Heart Fail. 2012;14(2):130–7. https://doi.org/10.1093/eurjhf/hfr165.
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 2017;389(10075):1195–205. https://doi.org/10.1016/s0140-6736(16)32616-2.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
Chen J, Long JB, Hurria A, Owusu C, Steingart RM, Gross CP. Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Coll Cardiol. 2012;60(24):2504–12. https://doi.org/10.1016/j.jacc.2012.07.068.
Bowles EJ, Wellman R, Feigelson HS, Onitilo AA, Freedman AN, Delate T, et al. Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. J Natl Cancer Inst. 2012;104(17):1293–305. https://doi.org/10.1093/jnci/djs317.
• Tolaney SM, Barry WT, Dang CT, Yardley DA, Moy B, Marcom PK, et al. Adjuvant paclitaxel and trastuzumab for node-negative, HER2-positive breast cancer. N Engl J Med. 2015;372(2):134–41. https://doi.org/10.1056/NEJMoa1406281 This is a trial demonstrating the efficacy and cardiac safety of a non-anthracycline adjuvant treatment with paclitaxel and trastuzumab in patients with stage 1 HER2-positive disease.
Tan TC, Bouras S, Sawaya H, Sebag IA, Cohen V, Picard MH, et al. Time trends of left ventricular ejection fraction and myocardial deformation indices in a cohort of women with breast cancer treated with anthracyclines, taxanes, and trastuzumab. J Am Soc Echocardiogr. 2015;28(5):509–14. https://doi.org/10.1016/j.echo.2015.02.001.
Banke A, Fosbol EL, Ewertz M, Videbaek L, Dahl JS, Poulsen MK, et al. Long-term risk of heart failure in breast cancer patients after adjuvant chemotherapy with or without trastuzumab. JACC Heart Fail. 2019;7(3):217–24. https://doi.org/10.1016/j.jchf.2018.09.001.
Yu AF, Yadav NU, Lung BY, Eaton AA, Thaler HT, Hudis CA, et al. Trastuzumab interruption and treatment-induced cardiotoxicity in early HER2-positive breast cancer. Breast Cancer Res Treat. 2015;149(2):489–95. https://doi.org/10.1007/s10549-014-3253-7.
Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002;20(5):1215–21.
de Azambuja E, Procter MJ, van Veldhuisen DJ, Agbor-Tarh D, Metzger-Filho O, Steinseifer J, et al. Trastuzumab-associated cardiac events at 8 years of median follow-up in the Herceptin Adjuvant trial (BIG 1-01). J Clin Oncol. 2014;32(20):2159–65. https://doi.org/10.1200/JCO.2013.53.9288.
Ezaz G, Long JB, Gross CP, Chen J. Risk prediction model for heart failure and cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Heart Assoc. 2014;3(1):e000472. https://doi.org/10.1161/JAHA.113.000472.
von Minckwitz G, Procter M, de Azambuja E, Zardavas D, Benyunes M, Viale G, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377(2):122–31. https://doi.org/10.1056/NEJMoa1703643.
Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372(8):724–34. https://doi.org/10.1056/NEJMoa1413513.
Gianni L, Pienkowski T, Im Y-H, Tseng L-M, Liu M-C, Lluch A, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17(6):791–800. https://doi.org/10.1016/s1470-2045(16)00163-7.
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Waldron-Lynch M, et al. Long-term efficacy analysis of the randomised, phase II TRYPHAENA cardiac safety study: evaluating pertuzumab and trastuzumab plus standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer. Eur J Cancer. 2018;89:27–35. https://doi.org/10.1016/j.ejca.2017.10.021.
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91. https://doi.org/10.1056/NEJMoa1209124.
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2018;380:617–28. https://doi.org/10.1056/NEJMoa1814017.
Tykerb (lapatinib) [package insert]. GlaxoSmithKline, Research Triangle Park, NC. 2007.
Perez EA, Koehler M, Byrne J, Preston AJ, Rappold E, Ewer MS. Cardiac safety of lapatinib: pooled analysis of 3689 patients enrolled in clinical trials. Mayo Clin Proc. 2008;83(6):679–86. https://doi.org/10.4065/83.6.679.
Johnston S, Pippen J Jr, Pivot X, Lichinitser M, Sadeghi S, Dieras V, et al. Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol. 2009;27(33):5538–46. https://doi.org/10.1200/JCO.2009.23.3734.
de Azambuja E, Holmes AP, Piccart-Gebhart M, Holmes E, Di Cosimo S, Swaby RF, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. The Lancet Oncology. 2014;15(10):1137–46. https://doi.org/10.1016/s1470-2045(14)70320-1.
Piccart-Gebhart M, Holmes E, Baselga J, de Azambuja E, Dueck AC, Viale G, et al. Adjuvant lapatinib and trastuzumab for early human epidermal growth factor receptor 2-positive breast cancer: results from the randomized phase III adjuvant lapatinib and/or trastuzumab treatment optimization trial. J Clin Oncol. 2016;34(10):1034–42. https://doi.org/10.1200/JCO.2015.62.1797.
Geyer CE, Forster J, LIndquist D, Chan S, Romieu CG, Pienkowski T, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355(26):2733–43.
Blackwell KL, Burstein HJ, Storniolo AM, Rugo HS, Sledge G, Aktan G, et al. Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 study. J Clin Oncol. 2012;30(21):2585–92. https://doi.org/10.1200/JCO.2011.35.6725.
Buza V, Rajagopalan B, Curtis AB. Cancer treatment-induced arrhythmias: focus on chemotherapy and targeted therapies. Circ Arrhythm Electrophysiol. 2017;10(8). https://doi.org/10.1161/CIRCEP.117.005443.
Martin M, Holmes FA, Ejlertsen B, Delaloge S, Moy B, Iwata H, et al. Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1688–700. https://doi.org/10.1016/S1470-2045(17)30717-9.
Burstein HJ, Sun Y, Dirix LY, Jiang Z, Paridaens R, Tan AR, et al. Neratinib, an irreversible ErbB receptor tyrosine kinase inhibitor, in patients with advanced ErbB2-positive breast cancer. J Clin Oncol. 2010;28(8):1301–7. https://doi.org/10.1200/JCO.2009.25.8707.
Nerlynx (neratinib) [package insert]. Puma Biotechnology, Los Angeles, CA. 2017.
Infante JR, Cassier PA, Gerecitano JF, Witteveen PO, Chugh R, Ribrag V, et al. A phase I study of the cyclin-dependent kinase 4/6 inhibitor ribociclib (LEE011) in patients with advanced solid tumors and lymphomas. Clin Cancer Res. 2016;22(23):5696–705. https://doi.org/10.1158/1078-0432.CCR-16-1248.
Thein KZ, Ball S, Zaw MH, Tun AM, Quirch M, Hardwicke F, et al. Updated meta-analysis of randomized controlled trials (RCTs) to determine the CDK 4/6 inhibitors associated venous thromboembolism (VTE) risk in hormone receptor-positive breast cancer (BC) patients. Ann Oncol. 2018;29(suppl_8):viii603-viii40. https://doi.org/10.1093/annonc/mdy300.
Kisqali (ribociclib) [package insert]. Novartis Pharmaceuticals Corporation, East Hanover, NJ. 2017.
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, et al. Adjuvant endocrine therapy for women with hormone receptor–positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2018;37(5):423–38. https://doi.org/10.1200/JCO.18.01160.
Khosrow-Khavar F, Filion KB, Al-Qurashi S, Torabi N, Bouganim N, Suissa S, et al. Cardiotoxicity of aromatase inhibitors and tamoxifen in postmenopausal women with breast cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Oncol. 2017;28(3):487–96. https://doi.org/10.1093/annonc/mdw673.
Esteva FJ, Hortobagyi GN. Comparative assessment of lipid effects of endocrine therapy for breast cancer: implications for cardiovascular disease prevention in postmenopausal women. Breast. 2006;15:301–12. https://doi.org/10.1016/j.breast.2005.08.033.
Amir E, Seruga B, Niraula S, Carlsson L, Ocana A. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2011;103(17):1299–309. https://doi.org/10.1093/jnci/djr242.
Arimidex T, Alone or in Combination Trialists’ Group, Buzdar A, Howell A, Cuzick J, Wale C, et al. Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol. 2006;7(8):633–43.
Blaes A, Beckwith H, Florea N, Hebbel R, Solovey A, Potter D, et al. Vascular function in breast cancer survivors on aromatase inhibitors: a pilot study. Breast Cancer Res Treat. 2017;166(2):541–7. https://doi.org/10.1007/s10549-017-4447-6.
van de Velde CJH, Rea D, Seynaeve C, Putter H, Hasenburg A, Vannetzel JM, et al. Adjuvant tamoxifen and exemestane in early breast cancer (TEAM): a randomised phase 3 trial. Lancet. 2011;377(9762):321–31.
Taunk NK, Haffty BG, Kostis JB, Goyal S. Radiation-induced heart disease: pathologic abnormalities and putative mechanisms. Front Oncol. 2015;5:39. https://doi.org/10.3389/fonc.2015.00039.
Lancellotti P, Nkomo VT, Badano LP, Bergler-Klein J, Bogaert J, Davin L, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14(8):721–40. https://doi.org/10.1093/ehjci/jet123.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–98. https://doi.org/10.1056/NEJMoa1209825.
Cheng YJ, Nie XY, Ji CC, Lin XX, Liu LJ, Chen XM, et al. Long-term cardiovascular risk after radiotherapy in women with breast cancer. J Am Heart Assoc. 2017;6(5). https://doi.org/10.1161/JAHA.117.005633.
Nilsson G, Holmberg L, Garmo H, Duvernoy O, Sjogren I, Lagerqvist B, et al. Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol. 2012;30(4):380–6. https://doi.org/10.1200/JCO.2011.34.5900.
Lo Q, Hee L, Batumalai V, Allman C, MacDonald P, Lonergan D, et al. Strain imaging detects dose-dependent segmental cardiac dysfunction in the acute phase after breast irradiation. Int J Radiat Oncol Biol Phys. 2017;99(1):182–90. https://doi.org/10.1016/j.ijrobp.2017.05.030.
Jacob S, Broggio D, Derreumaux S, Camilleri J, Lapeyre M, Bruguiere E, et al. Cardiac radiation exposure due to breast cancer radiotherapy: why mean heart dose is a limited parameter for cardiotoxicity studies? (BACCARAT study). Eur Heart J. 2018;39(suppl_1). https://doi.org/10.1093/eurheartj/ehy563.P3505.
van den Bogaard VA, Ta BD, van der Schaaf A, Bouma AB, Middag AM, Bantema-Joppe EJ, et al. Validation and modification of a prediction model for acute cardiac events in patients with breast cancer treated with radiotherapy based on three-dimensional dose distributions to cardiac substructures. J Clin Oncol. 2017;35(11):1171–8. https://doi.org/10.1200/JCO.2016.69.8480.
Yu AF, Ho AY, Braunstein LZ, Thor ME, Lee Chuy K, Eaton A et al. Assessment of early radiation-induced changes in LV function by myocardial strain imaging after breast radiation therapy. J Am Soc Echocardiogr. 2019;32(4)521–28. https://doi.org/10.1016/j.echo.2018.12.009.
Gulati G, Heck SL, Ree AH, Hoffmann P, Schulz-Menger J, Fagerland MW, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 x 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37(21):1671–80. https://doi.org/10.1093/eurheartj/ehw022.
Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR Jr, das Dores Cruz F, Goncalves Brandao SM, Rigaud VOC, et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. J Am Coll Cardiol. 2018;71(20):2281–90. https://doi.org/10.1016/j.jacc.2018.02.049.
Boekhout AH, Gietema JA, Milojkovic Kerklaan B, van Werkhoven ED, Altena R, Honkoop A, et al. Angiotensin II-receptor inhibition with candesartan to prevent trastuzumab-related cardiotoxic effects in patients with early breast cancer: a randomized clinical trial. JAMA Oncol. 2016;2(8):1030–7. https://doi.org/10.1001/jamaoncol.2016.1726.
Pituskin E, Mackey JR, Koshman S, Jassal D, Pitz M, Haykowsky MJ, et al. Multidisciplinary approach to novel therapies in cardio-oncology research (MANTICORE 101-breast): a randomized trial for the prevention of trastuzumab-associated cardiotoxicity. J Clin Oncol. 2017;35(8):870–7. https://doi.org/10.1200/JCO.2016.68.7830.
Guglin ME. Lisinopril or carvedilol for prevention of trastuzumab induced cardiotoxicity - lisinopril or carvedilol for cardiotoxicity. Presented at American College of Cardiology Annual Scientific Session (ACC 2018); March 11, 2018; Orlando, FL2018. This is a randomized, placebo-controlled primary prevention study assessing the value of lisinopril or carvedilol in preventing cardiomyopathy among patients treated with trastuzumab therapy, stratified according to anthracycline exposure. Results showed that lisinopril or carvedilol can mitigate LVEF decline in a subset of patients who received prior anthracycline.
Antonopoulos AS, Margaritis M, Lee R, Channon K, Antoniades C. Statins as anti-inflammatory agents in atherogenesis: molecular mechanisms and lessons from the recent clinical trials. Curr Pharm Des. 2012;18(11):1519–30.
Davignon J, Jacob RF, Mason RP. The antioxidant effects of statins. Coron Artery Dis. 2004;15(5):251–8.
Seicean S, Seicean A, Plana JC, Budd GT, Marwick TH. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012;60(23):2384–90. https://doi.org/10.1016/j.jacc.2012.07.067.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27(9):911–39. https://doi.org/10.1016/j.echo.2014.07.012.
Florido R, Smith KL, Cuomo KK, Russell SD. Cardiotoxicity From human epidermal growth factor receptor-2 (HER2) targeted therapies. J Am Heart Assoc. 2017;6(9). https://doi.org/10.1161/jaha.117.006915.
Chavez-MacGregor M, Niu J, Zhang N, Elting LS, Smith BD, Banchs J, et al. Cardiac monitoring during adjuvant trastuzumab-based chemotherapy among older patients with breast cancer. J Clin Oncol. 2015;33(19):2176–83. https://doi.org/10.1200/JCO.2014.58.9465.
• Henry ML, Niu J, Zhang N, Giordano SH, Chavez-MacGregor M. Cardiotoxicity and cardiac monitoring among chemotherapy-treated breast cancer patients. JACC Cardiovasc Imaging. 2018;11(8):1084–93. https://doi.org/10.1016/j.jcmg.2018.06.005 This study assessed adherence to recommended cardiac monitoring during breast cancer treatment among > 16,000 adult patients. Guideline-adherent monitoring during trastuzumab therapy was suboptimal, regardless of age or comorbidities. This highlights the importance of considering patient-specific CV risk factors in the cardiotoxicity surveillance of breast cancer patients.
Dang CT, Yu AF, Jones LW, Liu J, Steingart RM, Argolo DF, et al. Cardiac surveillance guidelines for trastuzumab-containing therapy in early-stage breast cancer: getting to the heart of the matter. J Clin Oncol. 2016;34(10):1030–3.
• Lynce F, Barac A, Geng X, Dang CT, Yu AF, Smith KL, et al. SAFE-HEaRt: a pilot study assessing the cardiac safety of HER2 targeted therapy in patients with HER2 positive breast cancer and reduced left ventricular function. J Clin Oncol. 2018;36(15_suppl):1038 This is the first prospective trial to evaluate the safety of anti-HER2 therapies among 30 breast cancer patients with asymptomatic mildly decreased LV function (40–49%), while receiving appropriate HF medications (beta blockers and ACEis) and regular cardiac surveillance.
Hussain Y, Drill E, Dang CT, Liu JE, Steingart RM, Yu AF. Cardiac outcomes of trastuzumab therapy in patients with HER2-positive breast cancer and reduced left ventricular ejection fraction. Breast Cancer Res Treat. 2019. https://doi.org/10.1007/s10549-019-05139-6.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63(25 Pt A):2751–68. https://doi.org/10.1016/j.jacc.2014.01.073.
Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr. 2013;26(5):493–8. https://doi.org/10.1016/j.echo.2013.02.008.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Tan TC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging. 2012;5(5):596–603. https://doi.org/10.1161/CIRCIMAGING.112.973321.
Fei HW, Ali MT, Tan TC, Cheng KH, Salama L, Hua L, et al. Left ventricular global longitudinal strain in HER-2 + breast cancer patients treated with anthracyclines and trastuzumab who develop cardiotoxicity is associated with subsequent recovery of left ventricular ejection fraction. Echocardiography. 2016;33(4):519–26. https://doi.org/10.1111/echo.13168.
Jacob S, Walker V, Fondard O, Chevelle C, Jimenez G, Bernier MO, et al. Use of myocardial strain imaging by echocardiography for the early detection of radiotherapy-induced cardiotoxicity in breast cancer patients (BACCARAT study). Arch Cardiovasc Dis Suppl. 2019;11(1):49–50. https://doi.org/10.1016/j.acvdsp.2018.10.107.
Cardinale D, Ciceri F, Latini R, Franzosi MG, Sandri MT, Civelli M, et al. Anthracycline-induced cardiotoxicity: a multicenter randomised trial comparing two strategies for guiding prevention with enalapril: the International CardioOncology Society-one trial. Eur J Cancer. 2018;94:126–37. https://doi.org/10.1016/j.ejca.2018.02.005.
•• Negishi T, Thavendiranathan P, Negishi K, Marwick TH, investigators S. Rationale and design of the strain surveillance of chemotherapy for improving cardiovascular outcomes: the SUCCOUR trial. JACC Cardiovasc Imaging. 2018;11(8):1098–105. https://doi.org/10.1016/j.jcmg.2018.03.019 This ongoing international multicenter randomized controlled trial is the first to compare conventional LVEF- versus GLS-guided surveillance and initiation of cardioprotective therapy among high-risk patients undergoing cardiotoxic chemotherapy over a 3-year follow-up period.
Thavendiranathan P, Wintersperger BJ, Flamm SD, Marwick TH. Cardiac MRI in the assessment of cardiac injury and toxicity from cancer chemotherapy: a systematic review. Circ Cardiovasc Imaging. 2013;6(6):1080–91. https://doi.org/10.1161/CIRCIMAGING.113.000899.
Galan-Arriola C, Lobo M, Vilchez-Tschischke JP, Lopez GJ, de Molina-Iracheta A, Perez-Martinez C, et al. Serial magnetic resonance imaging to identify early stages of anthracycline-induced cardiotoxicity. J Am Coll Cardiol. 2019;73(7):779–91. https://doi.org/10.1016/j.jacc.2018.11.046.
Yu AF, Chan AT, Steingart RM. Cardiac magnetic resonance and cardio-oncology: does T2 signal the end of anthracycline cardiotoxicity? J Am Coll Cardiol. 2019;73(7):792–4. https://doi.org/10.1016/j.jacc.2018.11.045.
Melendez GC, Sukpraphrute B, D’Agostino RB Jr, Jordan JH, Klepin HD, Ellis L, et al. Frequency of left ventricular end-diastolic volume-mediated declines in ejection fraction in patients receiving potentially cardiotoxic cancer treatment. Am J Cardiol. 2017;119(10):1637–42. https://doi.org/10.1016/j.amjcard.2017.02.008.
Ky B, Putt M, Sawaya H, French B, Januzzi JL Jr, Sebag IA, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol. 2014;63(8):809–16. https://doi.org/10.1016/j.jacc.2013.10.061.
Cardinale D, Colombo A, Torrisi R, Sandri MT, Civelli M, Salvatici M, et al. Trastuzumab-induced cardiotoxicity: clinical and prognostic implications of troponin I evaluation. J Clin Oncol. 2010;28(25):3910–6. https://doi.org/10.1200/JCO.2009.27.3615.
Todorova VK, Makhoul I, Siegel ER, Wei J, Stone A, Carter W, et al. Biomarkers for presymptomatic doxorubicin-induced cardiotoxicity in breast cancer patients. PLoS One. 2016;11(8):e0160224. https://doi.org/10.1371/journal.pone.0160224.
Leong SL, Chaiyakunapruk N, Lee SW. Candidate gene association studies of anthracycline-induced cardiotoxicity: a systematic review and meta-analysis. Sci Rep. 2017;7(1):39. https://doi.org/10.1038/s41598-017-00075-1.
Hertz DL, Caram MV, Kidwell KM, Thibert JN, Gersch C, Seewald NJ, et al. Evidence for association of SNPs in ABCB1 and CBR3, but not RAC2, NCF4, SLC28A3 or TOP2B, with chronic cardiotoxicity in a cohort of breast cancer patients treated with anthracyclines. Pharmacogenomics. 2016;17(3):231–40.
Serie DJ, Crook JE, Necela BM, Dockter TJ, Wang X, Asmann YW, et al. Genome-wide association study of cardiotoxicity in the NCCTG N9831 (Alliance) adjuvant trastuzumab trial. Pharmacogenet Genomics. 2017;27(10):378–85. https://doi.org/10.1097/FPC.0000000000000302.
Gomez Pena C, Davila-Fajardo CL, Martinez-Gonzalez LJ, Carmona-Saez P, Soto Pino MJ, Sanchez Ramos J, et al. Influence of the HER2 Ile655Val polymorphism on trastuzumab-induced cardiotoxicity in HER2-positive breast cancer patients: a meta-analysis. Pharmacogenet Genomics. 2015;25(8):388–93. https://doi.org/10.1097/FPC.0000000000000149.
Stanton SE, Ward MM, Christos P, Sanford R, Lam C, Cobham MV, et al. Pro1170 Ala polymorphism in HER2-neu is associated with risk of trastuzumab cardiotoxicity. BMC Cancer. 2015;15(1). https://doi.org/10.1186/s12885-015-1298-6.
Yu AF, Jones LW. Breast cancer treatment-associated cardiovascular toxicity and effects of exercise countermeasures. Cardiooncology. 2016;2. https://doi.org/10.1186/s40959-016-0011-5.
Jones LW, Courneya KS, Mackey JR, Muss HB, Pituskin EN, Scott JM, et al. Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J Clin Oncol. 2012;30(20):2530–7. https://doi.org/10.1200/JCO.2011.39.9014.
Jones LW, Habel LA, Weltzien E, Castillo A, Gupta D, Kroenke CH, et al. Exercise and risk of cardiovascular events in women with nonmetastatic breast cancer. J Clin Oncol. 2016;34(23):2743–9. https://doi.org/10.1200/JCO.2015.65.6603.
Jones LW, Haykowsky MJ, Swartz JJ, Douglas PS, Mackey JR. Early breast cancer therapy and cardiovascular injury. J Am Coll Cardiol. 2007;50(15):1435–41. https://doi.org/10.1016/j.jacc.2007.06.037.
Scott JM, Iyengar NM, Nilsen TS, Michalski M, Thomas SM, Herndon J 2nd, et al. Feasibility, safety, and efficacy of aerobic training in pretreated patients with metastatic breast cancer: a randomized controlled trial. Cancer. 2018;124(12):2552–60. https://doi.org/10.1002/cncr.31368.
Hornsby WE, Douglas PS, West MJ, Kenjale AA, Lane AR, Schwitzer ER, et al. Safety and efficacy of aerobic training in operable breast cancer patients receiving neoadjuvant chemotherapy: a phase II randomized trial. Acta Oncol. 2014;53(1):65–74. https://doi.org/10.3109/0284186X.2013.781673.
Mijwel S, Backman M, Bolam KA, Olofsson E, Norrbom J, Bergh J, et al. Highly favorable physiological responses to concurrent resistance and high-intensity interval training during chemotherapy: the OptiTrain breast cancer trial. Breast Cancer Res Treat. 2018;169(1):93–103. https://doi.org/10.1007/s10549-018-4663-8.
Pituskin E, Haykowsky M, McNeely M, Mackey J, Chua N, Paterson I. Rationale and design of the multidisciplinary team IntervenTion in cArdio-oNcology study (TITAN). BMC Cancer. 2016;16(1):733. https://doi.org/10.1186/s12885-016-2761-8.
Courneya KS, McNeely ML, Culos-Reed SN, Vallance JK, Bell GJ, Mackey JR, et al. The Alberta moving beyond breast cancer (AMBER) cohort study: recruitment, baseline assessment, and description of the first 500 participants. BMC Cancer. 2016;16:481. https://doi.org/10.1186/s12885-016-2534-4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Katherine Lee Chuy declares that she has no conflict of interest.
Anthony F. Yu has received compensation from Glenmark Pharmaceuticals, Takeda Oncology, Bristol-Myers Squibb, and Bayer for service as a consultant.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardio-oncology
Rights and permissions
About this article
Cite this article
Lee Chuy, K., Yu, A.F. Cardiotoxicity of Contemporary Breast Cancer Treatments. Curr. Treat. Options in Oncol. 20, 51 (2019). https://doi.org/10.1007/s11864-019-0646-1
Published:
DOI: https://doi.org/10.1007/s11864-019-0646-1