Abstract
Background and aims
International guidelines emphasise the importance of securing ruptured cerebral aneurysms within 48–72 h of ictus. We assessed the timing of treatment of patients with aneurysmal subarachnoid haemorrhage (aSAH) referred to a national neurosurgical centre.
Materials and methods
Analysis of a prospective database of patients with aSAH admitted between 1st of February 2016 and 29th of February 2020 was performed. The timing to treatment was expressed in days and analysed in three ways: ictus to treatment, ictus to referral and referral to treatment. ORs with 95% CI were calculated for aneurysm treatment within 24, 48 and 72 h for good grade (WFSN 1–3) and poor grade (WFNS 4–5) cohorts separately.
Results
Of a total of 538 patients with aSAH, the aneurysm was secured in 312 (58%) within 24 h and in 398 (74%) within 48 h of ictus. Securing the aneurysm within 48 h of ictus was achieved in 89% (395/444) of patients who were referred within 24 h of ictus, but in only 3.2% (3/94) who were referred > 24 h after ictus. Poor grade patients (WFNS 4–5) were more likely than good grade patients (WFNS 1–3) to be referred to neurosurgery within 48 h of ictus (OR 22.87, 95% CI 3.14–166.49, p = 0.0020) and for their aneurysm to be secured within 48 h (OR 1.78, 95% CI 1.06–2.98, p = 0.0297) of ictus. Ictus to referral delay was highest in WFNS grade 1 patients.
Conclusions
In centres with 7 day per week provision of interventional neuroradiology and vascular neurosurgery, the majority of patients with aSAH can be treated within the timeframes recommended by international guidelines and this applies to all grades of aSAH. However, delays still occur in a significant proportion of patients and this particularly applies to delays in presentation and diagnosis in good grade patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aneurysmal subarachnoid haemorrhage (aSAH) is a neurosurgical emergency [1] and despite reported declines in incidence, it still remains a significant source of morbidity and mortality [2,3,4]. Worldwide, approximately 10% of patients with aSAH die from the original bleed before reaching hospital. After the initial presentation, rebleed from the culprit aneurysm is the most frequent cause of death [5]. The risk of rebleeding is highest in the first 2 to 12 h, with nearly half of rebleeds occurring within 6 h of ictus [6,7,8]. Longer time to aneurysm treatment, worse neurological status on admission, larger aneurysm size and possibly systolic blood pressure > 160 mm Hg are some of the factors associated with aneurysm rebleeding [6].
The best time for securing a ruptured aneurysm is still debated and is often tailored to each patient’s specific situation, depending on factors such as World Federation of Neurosurgical Societies grade (WFNS grade), age and comorbidities. Early treatment, within 48–72 h of aSAH, is associated with favourable outcomes [3, 5, 6, 9,10,11,12,13,14,15,16,17]. Therefore, urgent evaluation, transfer to neurosurgery centres and subsequent treatment of patients with aSAH is recommended [6], in order to decrease the time to aneurysm repair and prevent rebleeding, as well as to decrease morbidity and mortality from aSAH [18].
Availability of resources such as neurosurgical intensive care unit beds, neurosurgical operating room, interventional neuroradiology suite and personnel including interventional neuroradiologists and neurovascular surgeons can also affect the timing of intervention [6, 19, 20]. There are a number of international guidelines which make recommendations regarding the timing of intervention for ruptured cerebral aneurysms. The guidelines of the American Heart Association recommend aneurysm treatment ‘as early as feasible’ to reduce the rate of rebleeding but do not provide any specific timelines [6]. The European Stroke Organisation guidelines recommend that the aneurysm should be ‘treated as early as logistically and technically possible to reduce the risk of rebleeding’ and ‘if possible, it should be aimed to intervene at least within 72 h after onset of first symptoms and that this decision should not depend on grading’ [3]. In the UK, both the Society of British Neurological Surgeons and the national clinical guidelines for stroke published by The Royal College of Physicians recommend that ‘treatment to secure the aneurysm should be undertaken within 48 h of ictus for good grade patients (WFNS grades 1–3), or within a maximum of 48 h of diagnosis if presentation was delayed’ [5]. As a result of these guidelines, many neurosurgical centres aim to treat aSAH within 2 days (48 h) of ictus [21]. The aim of this study was to assess whether patients with aSAH referred to a national neurosurgical centre (where interventional neuroradiology and neurovascular surgery are available on a 7-day-per-week basis) have their aneurysm secured within a timely fashion and in accordance with international guidelines. In addition we assessed time intervals from ictus to neurosurgical referral and from referral to aneurysm securement in good and poor grade aSAH patients.
Methods
Details of all patients with aSAH referred to Beaumont hospital, national neurosurgical centre, have been entered in a prospective database since 1st of February 2016. This is one of two centres providing neurosurgical care in the Republic of Ireland and has a catchment population of approximately 3.5 million people. Endovascular and microsurgical procedures for aneurysms are carried out by 5 interventional neuroradiologists and 3 neurovascular surgeons on a 7-day-per-week basis. Most aneurysms are secured during day time hours on the next available operating list. Emergency procedures such as haematoma evacuation or CSF diversion are carried out on a 24/7 basis. The vast majority of patients present to their local hospital where they undergo initial investigations such as computed tomography (CT) and CT angiography (CTA). Once the diagnosis of SAH is established, they are referred to the neurosurgical centre on a 24/7 basis. Imaging such as CT or CTA performed in the 25 referring hospitals can be reviewed immediately by the neurosurgical team on the National Integrated Medical Imaging System (NIMIS).
Institutional approval for data collection for this study was obtained. Prospectively collected data included patient demographics, WFNS grade, Fisher grade, aneurysm treatment received (endovascular, surgical or none) and dates of ictus, referral, admission to neurosurgical centre and definitive aneurysm treatment.
The time interval between ictus and aneurysm treatment was measured in days. Day of ictus was defined as day 0. Aneurysm treatment on days 0 and 1 was categorised as treatment within 24 h of ictus. Treatment on days 2 and 3 was classified as treatment within 48 and 72 h of ictus, respectively. We also analysed the data to assess the time intervals between ictus and referral to neurosurgery and between referral to neurosurgery and definitive aneurysm treatment. In the rest of this article, ‘referral’ indicates referral to the neurosurgery department. Definitive aneurysm treatment included endovascular treatment or surgical clipping. Patients who did not undergo definitive aneurysm treatment were excluded from the study. Patients included in the study were dichotomised based on their WFNS grades. WFNS grades 1–3 were defined as good grade and WFNS grades 4 and 5 as poor grade. We analysed the data to elucidate the number of patients treated within 24, 48 and 72 h of ictus. This analysis was performed for the entire cohort of patients and also for the subgroups of good and poor grade aSAH.
Statistical Analysis
We analysed whether there was a relationship between timing of aneurysm treatment and WFNS grades using chi-square tests. Odds ratios (ORs) with 95% confidence intervals (CI) were calculated for the different categories of timing of treatment, with good grade and poor grade aSAH as the reference groups. Statistical significance was defined as p < 0.05.
Results
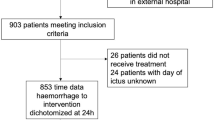
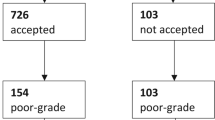
Between the 1st of February 2016 and the 29th of February 2020, 704 patients were admitted to Beaumont Hospital with spontaneous SAH. Of these 704 patients, 166 patients were excluded as they received no treatment for one of the following reasons: patients with angiogram negative SAH (n = 134) and patients in extremely poor clinical condition (e.g. non-survivable haemorrhage with fixed dilated pupils, N = 32). The remaining 538 patients underwent either endovascular treatment (N = 465, 86.43%) or surgical clipping of the aneurysm (N = 73, 13.57%) (Fig. 1). Of these 538 patients, the diagnosis of SAH was made on CT scan in 507 patients. In 31 patients, the CT scan was negative, and SAH was diagnosed by the presence of xanthochromia on examination of cerebrospinal fluid (CSF). A total of 497/538 (92.4%) of the patients in this study initially presented to another hospital and required transfer to the neurosurgical centre.
The mean age of the patients at admission (± standard error of mean (SEM)) was 55.57 ± 0.53 years, and median age was 56 (range 12–91). A total of 364 patients were female (67.66%). Of the 538 patients, 273 were WFNS 1 (50.74%), 125 were WFNS 2 (23.23%), 24 were WFNS 3 (4.46%), 74 were WFNS 4 (13.75%) and 42 were WFNS 5 (7.81%). Baseline characteristics of patients are listed in Table 1.
Ictus to treatment
The mean number of days from ictus to treatment for the entire cohort was 2.87 (standard deviation (SD) 3.89, interquartile range (IQR) 2) and the median was 1 day (range 0–46 days). Out of the total 538 patients, 312 (57.99%) were treated within 24 h, 398 (73.98%) within 48 h and 434 (80.67%) within 72 h of ictus. Table 2 outlines the ictus to treatment times for the entire cohort and for the good and poor grade subgroups.
There was a statistically significant relationship between WFNS grading and timing of ictus to treatment for 24 h and 48 h groups. Patients with poor grade (WFNS 4–5) aSAH were more likely to be treated within the 24 h (OR 2.12, 95% CI 1.36–3.31, p = 0.0010) and 48 h (OR 1.78, 95% CI 1.06–2.98, p = 0.0297) of ictus when compared with patients with good grade (WFNS 1–3) aSAH.
Ictus to referral
The mean number of days from ictus to referral was 1 (SD 2, IQR 1), and the median was 0 days (range 0–20 days). Of the 538 patients, 444 (82.53%) were referred within 24 h and 467 (86.80%) within 48 h of ictus. Table 3 demonstrates the ictus to referral times for the entire cohort and for the good and poor grade subgroups.
There was a statistically significant relationship between WFNS grading and timing of ictus to referral for 24 h and 48 h groups (Tables 3 and 4). Patients with poor grade aSAH were more likely to be referred within 24 h (OR 10.36, 95% CI 3.21–33.36, p = 0.0001) and 48 h (OR 22.87, 95% CI 3.14–166.49, p = 0.0020) of ictus when compared with patients with good grade aSAH. The percentage of patients referred to neurosurgery within 24 h of ictus was lowest in WFNS grade 1 patients (74%) and highest in WFNS grade 5 patients (97.6%) (Table 4). Of 444 patients referred within 24 h of ictus, 395 (88.96%) had their aneurysm secured within 48 h of ictus. Of 94 patients referred more than 24 h after ictus, 3 (3.19%) had their aneurysm secured within 48 h of ictus (Table 5). The difference between these 2 groups was highly significant (OR 86.55, 95% CI 26.99–277.56, p < 0.0001).
Referral to treatment
The mean number of days from referral to treatment was 1.61 (SD 3.01, IQR 0), and the median was 1 day (range 0–45 days). Of the total 538 patients, 434 (80.67%) were treated within 24 h and 482 (89.59%) within 48 h of referral. Table 6 outlines the referral to treatment times for the entire cohort and for the good and poor grade subgroups.
Discussion
Our data demonstrates that the majority of patients with aSAH admitted to our centre had their aneurysm secured within the internationally recommended timeframes of 48–72 h of ictus. The ruptured aneurysm was secured within 24, 48 and 72 h of ictus, in 58%, 74% and 80% of patients, respectively. Furthermore, once the diagnosis of aSAH was made and the patient was referred to neurosurgery, the vast majority of patients were transferred and treated rapidly. The ruptured aneurysm was secured within 24 and 48 h of referral to neurosurgery, in 81% and 90% of patients, respectively. It must be noted that 497/538 (92.4%) of the patients in this study initially presented to another hospital and required transfer to the neurosurgical centre. These results have been possible to achieve by the provision of a 7-day service for both interventional neuroradiology and vascular neurosurgery. We strive to secure ruptured aneurysms as early as feasible usually on the next available operating list. For those with space occupying haematomas or hydrocephalus, emergency neurosurgery is performed on a 24/7 basis. Treatment in high volume centres with availability of interventional neuroradiology, vascular neurosurgery and neurosurgical intensive care allows for multidisciplinary management of patients, on a 7-day basis and likely results in improved outcomes [6, 19, 20]. This is especially critical for the management of patients with poor grade aSAH [6].
In our cohort of patients, the time from ictus to treatment was significantly shorter in patients who were in poorer clinical grades (WFNS 4–5). In these patients, the ruptured aneurysm was secured within 24 and 48 h of ictus, in 72% and 82% respectively. One explanation for this could be that poor grade patients are more likely to seek urgent medical attention and are more likely to be referred due to the urgency of the clinical situation. However, it also reflects a shift in neurosurgical management of these patients, which is at least partly due to the significant shift towards endovascular treatment of ruptured aneurysms. Traditionally, many neurosurgical centres delayed surgery in poor grade aSAH patients until clinical improvement occurred (often 10–14 days after ictus). Our results show that the majority of poor grade aSAH patients transferred to our centre are now undergoing intervention to secure their aneurysm within the first 24–48 h after ictus. This seems appropriate, given that several studies have previously shown that patients with WFNS grades 4–5 are at a higher risk of early rebleeding from the ruptured aneurysm compared with those with WFNS grades 1–3 [13,14,15,16,17].
In this study, delay between ictus and referral to neurosurgery was a significant contributor to the overall time from ictus to treatment. Of the 538 patients, 17.5% were referred to neurosurgery more than 24 h after ictus and 13% more than 48 h after ictus. Securing the ruptured aneurysm within 48 h of ictus was achieved in 89% of patients referred within 24 h of ictus, but only in 3.2% of those referred more than 24 h after ictus. From the time of ictus to neurosurgical referral, several stages exist in the patient pathway, and a delay in any of these steps can be responsible for the overall delay in securing the aneurysm. These include time from ictus to the patient presenting for medical assessment (either to GP or local A&E department), time from A&E attendance to CT scan and time from CT scan to neurosurgical referral. Further studies are required to establish how these steps can be made more efficient.
International guidelines for aSAH often focus on patients in good clinical grades (WFNS grades 1–3) because these patients have the best chance of a good functional outcome [22]. In our 422 patients with good-grade aSAH, the aneurysm was secured within 48 h of ictus in 72% and within 24 and 48 h of referral to neurosurgery in 81% and 91%, respectively. However, the delay between ictus and referral to neurosurgery was most pronounced in patients with WFNS grade 1 aSAH (Table 4). These patients present in the best clinical condition. Therefore, the patient may present late, not realising the significance of a sudden severe headache. In addition, the normal conscious level and the lack of neurological deficit may instil a degree of false reassurance to the initial examining physician and lead to a delay in obtaining a CT scan. Increasing public awareness and education of healthcare professionals should be an important part of any strategy aiming to improve timing to treatment of aSAH [4, 5, 19, 23].
In conclusion, with the provision of 7-day interventional neuroradiology and neurovascular surgery services, the majority of patients with aSAH can be treated within the time frames specified by international guidelines, and this applies to all WFNS grades. However, delays in the overall diagnosis and treatment pathway still occur in a significant proportion of patients, particularly in those with good grade aSAH. Further studies are needed in order to identify factors which result in such delays, both before and after neurosurgical referral.
Strengths and limitations of this study
The strengths of this study are the relatively large number of patients included and that the data was collected prospectively. The weakness of the study is that aneurysm treatment was expressed in days rather than hours after aSAH, as we did not have the exact times of ictus in all patients.
Conclusions
In centres with 7-day-per-week provision of interventional neuroradiology and vascular neurosurgery, majority of patients with aSAH can be treated within the timeframes recommended by international guidelines, and this applies to all grades of aSAH. However, delays still occur in a significant proportion of patients, and this particularly applies to delays in presentation and diagnosis in good grade patients.
Change history
08 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11845-021-02591-6
References
Sweeney K, Silver N, Javadpour M (2016) Subarachnoid haemorrhage (spontaneous aneurysmal). BMJ Clin Evid 2016:1–13
Nicholson P, Ohare A, Power S et al (2019) Decreasing incidence of subarachnoid hemorrhage. J Neurointerv Surg 11:320–322. https://doi.org/10.1136/neurintsurg-2018-014038
Steiner T, Juvela S, Unterberg A et al (2013) European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis 35:93–112. https://doi.org/10.1159/000346087
R. Germans M, Hoogmoed J, Van Straaten HAS et al (2014) Time intervals from aneurysmal subarachnoid hemorrhage to treatment and factors contributing to delay. J Neurol 261:473–479. https://doi.org/10.1007/s00415-013-7218-2
Intercollegiate Stroke Working Party (2008) National clinical guideline for stroke - 3rd edition
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 43:1711–1737. https://doi.org/10.1161/STR.0b013e3182587839
Naidech AM, Janjua N, Kreiter KT et al (2005) Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. Arch Neurol 62:410–416. https://doi.org/10.1001/archneur.62.3.410
Ohkuma H, Tsurutani H, Suzuki S (2001) Incidence and significance of early aneurysmal rebleeding before neurosurgical or neurological management. Stroke 32:1176–1180. https://doi.org/10.1161/01.STR.32.5.1176
Siddiq F, Chaudhry SA, Tummala RP et al (2012) Factors and outcomes associated with early and delayed aneurysm treatment in subarachnoid hemorrhage patients in the United States. Neurosurgery 71:670–677. https://doi.org/10.1227/NEU.0b013e318261749b
Tykocki T, Czyż M, Machaj M et al (2017) Comparison of the timing of intervention and treatment modality of poor-grade aneurysmal subarachnoid hemorrhage. Br J Neurosurg 31:430–433. https://doi.org/10.1080/02688697.2017.1319906
Wong GKC, Boet R, Ng SCP et al (2012) Ultra-early (within 24 hours) aneurysm treatment after subarachnoid hemorrhage. World Neurosurg 77:311–315. https://doi.org/10.1016/j.wneu.2011.09.025
Dorhout Mees SM, Molyneux AJ, Kerr RS et al (2012) Timing of aneurysm treatment after subarachnoid hemorrhage: relationship with delayed cerebral ischemia and poor outcome. Stroke 43:2126–2129. https://doi.org/10.1161/STROKEAHA.111.639690
De Gans K, Nieuwkamp DJ, Rinkel GJE, Algra A (2002) Timing of aneurysm surgery in subarachnoid hemorrhage: a systematic review of the literature. Neurosurgery 50:336–340. https://doi.org/10.1097/00006123-200202000-00018
Nieuwkamp DJ, De Gans K, Algra A et al (2005) Timing of aneurysm surgery in subarachnoid haemorrhage - an observational study in the Netherlands. Acta Neurochir (Wien) 147:815–820. https://doi.org/10.1007/s00701-005-0536-0
Mahaney KB, Todd MM, Torner JC (2011) Variation of patient characteristics, management, and outcome with timing of surgery for aneurysmal subarachnoid hemorrhage: Clinical article. J Neurosurg 114:1045–1053. https://doi.org/10.3171/2010.11.JNS10795
van Donkelaar CE, Bakker NA, Veeger NJGM et al (2015) Predictive factors for rebleeding after aneurysmal subarachnoid hemorrhage: rebleeding aneurysmal subarachnoid hemorrhage study. Stroke 46:2100–2106. https://doi.org/10.1161/STROKEAHA.115.010037
Gaberel T, Emery E (2015) Timing of surgical aneurysmal exclusion in SAH. J Neurosurg 122:1248. https://doi.org/10.3171/2011.2.JNS11277
Sorteberg A, Bredmose PP, Hansen AE, Sorteberg W (2019) The path from ictus to Neurosurgery: chronology and transport logistics of patients with aneurysmal subarachnoid haemorrhage in the South-Eastern Norway Health Region. Acta Neurochir (Wien) 161:1497–1506. https://doi.org/10.1007/s00701-019-03971-9
Dick R (2005) Managing the flow Cut Tool Eng 57:19–21. https://doi.org/10.1007/3-211-38158-9_1
Lamb JN, Crocker M, Tait MJ et al (2011) Delays in treating patients with good grade subarachnoid haemorrhage in London. Br J Neurosurg 25:243–248. https://doi.org/10.3109/02688697.2010.544787
Oudshoorn SC, Rinkel GJE, Molyneux AJ et al (2014) Aneurysm treatment <24 versus 24–72 h after subarachnoid hemorrhage. Neurocrit Care 21:4–13. https://doi.org/10.1007/s12028-014-9969-8
Teo M, Teo M, Turner C et al (2017) What Factors determine treatment outcome in aneurysmal subarachnoid hemorrhage in the modern ERA? A post hoc STASH analysis. World Neurosurg 105:270–281. https://doi.org/10.1016/j.wneu.2017.05.005
Inagawa T (2011) Delayed diagnosis of aneurysmal subarachnoid hemorrhage in patients: a community-based study - Clinical article. J Neurosurg 115:707–714. https://doi.org/10.3171/2011.5.JNS102157
Funding
This study was part funded by Friends of A, a charitable organisation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Beaumont Hospital Ethics Committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
The original online version of this article was revised: The original article contains an error. In Table 5, ‘h’ was missing and should be corrected to “<48 h”.
Rights and permissions
About this article
Cite this article
Choudhry, A., Murray, D., Corr, P. et al. Timing of treatment of aneurysmal subarachnoid haemorrhage: are the goals set in international guidelines achievable?. Ir J Med Sci 191, 401–406 (2022). https://doi.org/10.1007/s11845-021-02542-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02542-1