Abstract
Background and aims
In this study, we compared duration for reaching desired Ramsay Sedation Score (RSS) and postoperative recovery according to Modified Aldrete Score (MAS) of propofol and propofol-ketamine combination in a group of colonoscopy patients. Rates of cardiovascular, respiratory, laryngospasm, visual and nausea/vomiting complications were also compared as secondary outcomes.
Methods
This is a double-blinded prospective randomized controlled trial. 95 patients were included and blocked randomized to either propofol (GroupP, n: 47) or propofol-ketamine (GroupPK, n: 48). GroupP patients received 0.5 mg/kg propofol and GroupPK received 0.5 mg/kg ketamine-propofol. Subjects were monitorized noninvasively preoperatively and every 5 min during procedure. RSS was recorded for every minute before starting procedure and for every 5 min during procedure. Recovery after colonoscopy was evaluated according to MAS. Same observer checked for MAS just after procedure in postoperative 1 min and for every 3 min during follow-up. Postoperative respiratory depression was defined as rate <10/min, hypercapnia/hypercarbia—arterial CO2 tension >50 mmHg or SO2 <90 while hypotension was defined as a decrease of 20 % in mean blood pressure compared to initial values.
Results
GroupPK patients needed shorter duration for achieving RSS ≥ 4 (p: 0.038) but longer duration for achieving MAS ≥ 9 (p: 0.005). GroupP’s intraoperative blood pressures and heart rates were significantly lower compared to initial values. We observed that respiratory depression (19.1 vs 0 %, p: 0.001), hypotension (29.8 vs 10.4 %, p: 0.018), and nausea/vomiting (17 vs 4.2 %, p: 0.041) were significantly more common in GroupP.
Conclusion
Propofol-ketamine combination is an advantageous choice in means of achieving sedation in a shorter period of time, a better hemodynamic stability, less nausea and vomiting and respiratory complication rates. Yet it seems that this choice might be related with longer recovery duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colonoscopy is a highly accurate diagnostic technique which also provides an opportunity for therapeutic approach. However, it could be painful for patient and it is advised to be performed under procedural sedation.
Propofol is a commonly used agent for daily anesthesia procedures as it has early-onset effect with single dose and a short half-life [1]. Yet it has some serious side effects like hypotension, bradycardia, and respiratory depression [2]. Ketamine is an amnestic and analgesic agent that binds to N-methyl d-Aspartate (NMDA) receptors. Due to low cardiovascular side effect profile, ketamine is widely used as a combination agent in anesthetic procedures. However, it might delay postoperative recovery [3–6]. Depending on these previous literature, we hypothesized that using ketamine-propofol combination for colonoscopy procedures might result in shorter sedation achievement duration, lower hemodynamic and respiratory complication rates and less side effects. For this purpose, we performed this study to query if ketamine-propofol combination is superior to propofol alone in means of shorter durations for reaching required sedation levels and recovery with lower complication rates.
Methods
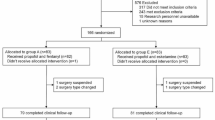
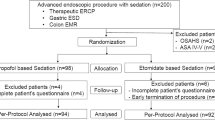
Study was approved by local ethical committee (Keciören Research Hospital Ethical Committee—14.4.2013) and all subjects signed informed consent. Study was planned and performed as a double-blinded prospective randomized controlled trial. Patients were block randomized to either propofol (GroupP) or propofol-ketamine (GroupPK) during preprocedural evaluation 24 h before colonoscopy when both inclusion and medication group decisions were made by same anesthesiologist. 425 patients who had colonoscopy with procedural sedation between 01.05.2013 and 01.01.2014 were screened and 98 patients were included. Exclusion criteria were as follows; preoperative American Society of Anesthesiologists (ASA) physical status classification 3–4, <18 or >70 years old, previous coronary heart disease, hypertension, arterial aneurysm, epilepsia, intracranial mass of benign or malign nature, respiratory–hepatic or renal impairment, and propofol or ketamine allergy history. Two patients in GroupP and 1 patient in GroupPK were excluded from study due to premature termination of colonoscopy procedure because of insufficient colon cleansing. After excluding these patients study groups were as follows; Group P, n: 47 and Group PK, n:48.
Duration for reaching desired Ramsay Sedation Score (RSS ≥ 4) was compared as the primary outcome. Postoperative recovery duration according to Modified Aldrete Scores (MAS ≥ 9), rates of cardiovascular (hypertension, hypotension, bradycardia), respiratory depression, laryngospasm, visual side effects, nausea/vomiting complications were also compared between groups as secondary outcomes.
Medications were prepared by same anesthesiology specialist and were applied by another specialist in each subject. This second specialist was blinded for the content of applied medication and followed every subject during procedure till recovery and also recorded all observed side effects. All patients were monitorized noninvasively for systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MBP), heart rate and rhythm, peripheral O2 saturation (SO2) preoperatively and every five minutes during procedure. All patients received 4 ml/kg h % 0.9 NaCl infusion and 2 lt min−1 nasal O2 during procedure. RSS was recorded for every minute before starting procedure and for every 5 min during procedure by the second specialist who was blinded for the content of applied medication. All patients received 0.03 mg/kg midazolam iv as premedication. GroupP patients received 0.5 mg/kg propofol iv in a period of 30–45 s. If patients could not achieve a RSS ≥ 4 after 2 min follow-up, we applied another dose of 0.25 mg/kg propofol for every 2 min and started colonoscopy procedure when RSS is ≥4. Predefined maximum dose for propofol was 2 mg/kg. For GroupPK a 1:1 ketamine-propofol combination (5 mg/ml propofol and 5 mg/ml ketamine) was prepared and applied as 0.5 mg/kg iv in 30–45 s. If patients could not achieve a RSS ≥ 4 we applied additional propofol as defined previously in this paragraph. Predefined maximum dose for ketamine-propofol was 2 mg/kg. Total procedure duration was defined as the duration between the initiation of sedation and patient being taken to recovery room. Recovery after colonoscopy was evaluated according to MAS and patients were discharged from post-procedure care unit when they achieved a MAS ≥ 9. Same blinded observer checked for MAS just after procedure in postoperative 1 min and for every 3 min during follow-up.
Respiratory depression (rate <10/min or SO2 <90), hypotension (a decrease of 20 % in MBP compared to initial values), hypertension (an increase of 20 % in MBP compared to initial values), bradycardia (<45/min), nausea, vomiting, partial or complete laryngospasm (decrease or deficiency of lung sounds accompanied by observed glottic muscle spasm), visual problems during procedure and emergence reactions like dream like states, vivid imaginary, hallucinations, delirium, excitement, irrational behaviors etc. were recorded as side effects. Side effect profile data were collected by second anesthesiologist who applied medications and followed up patients during procedure and he/she was blinded to the content of medication.
Statistical methodology
Statistical Package for Social Sciences (SPSS for Windows, Chicago, IL, USA) version of 14.0 was used for statistical analysis. Data were submitted to a frequency distribution analysis by Kolmogorov–Smirnov’s test. Values displaying normal distribution were expressed as the mean ± SD and values with skew distribution were expressed as median (interquartile range). Differences between numeric variables were tested with independent samples t or Mann–Whitney U tests where appropriate. Categorical data were compared by Chi-square test. The value of confidence interval was accepted as 95 % and statistical significance was accepted as: “p < 0.05”.
Results
Study groups were similar in means of gender—ASA distributions, age, body weight, and body mass indices. Preoperative SBP, DBP, MBP, heart rates, and SO2 values and total colonoscopy durations were also similar (9 vs 8 min).
GroupPK patients needed shorter duration for achieving RSS ≥ 4 (3.3 ± 4.2 vs 2.4 ± 1.6 min, p: 0.038). GroupP patients’ requirement for and additional dose of propofol for achieving adequate sedation was significantly higher compared to GroupPK (66 vs 33.3 %, p: 0.001). None of the patients in either group required a third dose of propofol.
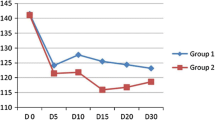
GroupPK patients had longer recovery duration (MAS ≥ 9, 1 vs 5 min, p: 0.005). Hemodynamic findings during procedure were as follows; GroupP’s intraoperative SBP, DBP, and MBP were significantly lower compared to preoperative values (Table 1). We also observed a significant drop in mean heart rates of patients in GroupP (p: 0.0001, Table 1). There was no significant change in GroupPK in means of pre- and intraoperative SBP, DBP, MBP, and heart rates. When groups were compared with each other, we observed that intraoperative SBP (p: 0.013), MBP (p: 0.018), and heart rates (p: 0.037) were significantly lower in GroupP (Table 1). These patients also had a tendency for lower intraoperative DBP but this difference was not statistically significant (75.9 ± 8.9 vs 79.7 ± 10.4 mmHg, p: 0.06). GroupP patients had significantly lower intraoperative SO2 values compared to Group PK (p: 0.003).
In means of sedation-related complications, we observed that respiratory depression (19 vs 0 %, p: 0.001), hypotension (29.8 vs 10.4 %, p: 0.018), and nausea or vomiting were significantly more common in GroupP (17 vs 4.2 %, p: 0.041, Table 2). While hypertension incidences were similar we did not observe any cases of bradycardia, laryngospasm or visual problems in any groups. No emergence reactions were observed in any of patients.
Discussion
In this study, we compared a group of 95 colonoscopy patients who received procedural sedation with either propofol or propofol-ketamine combination in means of duration for reaching desired RSS. We also compared postoperative recovery durations according to MAS, hemodynamic/respiratory complications, and side effect profiles. We observed that patients receiving propofol alone required longer duration to reach desired RSS but had shorter recovery duration compared to propofol-ketamine used patients. These patients also had a tendency to experience some predefined side-effects like respiratory depression, hypotension, bradycardia, and nausea and/or vomiting.
Appropriate analgesia and sedation are essential not only for patients’ comfort but also for clinicians’ comfort during colonoscopy. Used agent should not suppress spontaneous respiration, cause hemodynamical instability and also should not have any other serious side effects [7]. Personal characteristics of patients might affect duration and dose requirements for achieving and stabilizing patient at desired sedation level [8].
A group of sedative agents could be used alone or as combination for endoscopic procedures. Most commonly used agents are propofol, ketamine and midazolam [9–11]. Using propofol-ketamine combination is a preferred method for achieving a better sedation with less side effects [12]. There are 10 mg/ml ketamine—10 mg/ml propofol containing ketamine-propofol solutions for practical use in many countries [13].
Ketamine is a N-methyl-d-aspartate receptor antagonist that is primarily used for analgesia and has minimal respiratory side effects. It also has a protective sympathomimetic activity that preserves heart rate and blood pressure [14]. However in increased doses, it might cause hallucination, visual problems, nausea, vomiting and laryngospasm [15, 16]. Propofol is a widely preferred sedative agent in daily practice because of its amnestic, anxiolytic, antiemetic properties, and short half-life. On the other hand respiratory depression, hypotension due to decreased cardiac output, and peripheral vascular resistance are side effects that might limit its usage [14, 17].
Fast sedation and early recovery are important parameters in daily procedures like endoscopic evaluations that require sedation. In our study, we compared Ramsay and Alderte scoring systems to evaluate initiation of and recovery from sedation respectively. We observed that propofol alone has an advantage of early recovery on the other hand has a disadvantage of requiring longer duration for achieving desired sedation level compared to propofol-ketanine combination (Table 1). It is also an important finding that propofol alone used patients required higher additional doses for adequate sedation yet they recovered faster that ketamine-propofol combination group (median 1 vs 5 min). We believe that this might be a result of high metabolism rate and short half life of propofol. Contradicting our findings Ghadami et al. reported longer recovery duration with propofol in a group of 60 pediatric patients [18]. Khajavi et al. reported similar recovery durations for ketamine-propofol and fentanyl-propofol in colonoscopy patients [19]. We believe that these differences might be secondary to study population characteristics.
In our study we observed respiratory depression in 9 patients in propofol group. Respiratory depression incidence was 19.1 % in this group; on the other hand in combination group there was no respiratory problem. Previously Celik et al. reported higher rates of respiratory depression in a group of geriatric patients who underwent endoscopic procedure by propofol-fentanyl combination compared to patients who received ketamine-midazolam. They reported that 45 % of patients in propofol-fenatnyl group experienced respiratory depression while this rate was only 17.5 % in ketamine-midazolam group [20]. In an other study that analyzed effects of ketamine-propofol combination in healthy volunteers it has also been reported that this mixture does not cause any fall in bood O2 saturation [21]. Similarly Cok et al. also reported a fall in O2 saturation in only 2 out of 102 patients who received propofol-ketamine combination and underwent endoscopic retrograde cholangiography. They concluded that this is a really low incidence compared to previous studies [8]. Kayhan et al. compared ketamine-propofol and thiopental and reported no respiratory depression in either group [12].
We also observed significantly lower intraoperative blood pressure and heart rate in propofol group compared to propofol-ketamine receiving patients. These patients also experienced significant falls in these parameters compared to their initial findings (Table 1). Hypotension incidence was also significantly higher in propofol receiving patients (Table 2). It is well known that propofol decreases systemic vascular resistance, cardiac contractility, and preload which all cause a decrease in arterial blood pressure. Propofol also inhibits arterial baroreflex and hypotension induced tachycardia [1]. There are some previous studies that reported propofol-ketamine combination is safe in means of hemodynamic stability in groups of pediatric, emergency room, and regional analgesia patients [13, 20, 22]. Smischney et al. compared ketamine-propofol (0.75 mg/kg) and propofol (1,5 mg/kg) in general anesthesia induction and reported lower myocardial depression and vasodilation in ketamine-propofol group [23]. Cok et al. also reported better hemodynamic and respiratory stability in ketamine-propofol combination [8].
We observed higher nausea vomiting rates in propofol receiving patients (Table 1). In fact propofol is an efficient anti-emetic; however, we believe that higher hypotension rates in this group might be related with increased nausea vomiting incidence [14, 17].
As a conclusion, propofol-ketamine combination is an advantageous choice compared to propofol alone in colonoscopy patients in means of achieving desired sedation level in a shorter period of time with lower dose requirements. Propofol-ketamine also provides a better hemodynamic stability, less nausea and vomiting, and respiratory complication rates. Yet it seems that this choice might be related with longer recovery duration. We believe that choosing propofol-ketamine combination option in patients who require faster sedation induction and with increased cardiovascular complication risks would be the appropriate approach.
References
Morgan, G. Edward, Maged S, Murray MJ (2008) Lange Clinical Anesthesiology. Lange Medical Books/McGraw Hill Medical Pub, New York, pp 179–203
Arora S (2008) Combining Ketamine and propofol (“Ketofol”) for emergency department procedural sedation and analgesia: a review. WestJEM 9(1):20–23
Badrinath S, Avramov MN, Shadrick M et al (2000) The use of a ketamine-propofol combination during monitored anesthesia care. Anesth Analg 90(4):858–862
Tanaka M, Sato M, Saito A et al (2000) Reevaluation of rectal ketamine premedication in children: comparison with rectal midazolam. Anesthesiology 93(5):1217–1224
Erdogan MA, Begec Z, Aydogan MS (2013) Comparison of effects of propofol and ketamine-propofol mixture (ketofol) on laryngeal mask airway insertion conditions and hemodynamics in elderly patients: a randomized, prospective, double-blind trial. J Anesth. 27(1):12–17
Ozgul U, Begec Z, Karahan K et al (2013) Comparison of propofol and ketamine-propofol mixture (Ketofol) on laryngeal tube-suction ii conditions and hemodynamics: a randomized, prospective, double-blind trial. Curr Ther Res Clin Exp. 75:39–43
McQuaid KR, Laine L (2008) A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc 67(6):910–923
Cok OY, Eker HE, Izmirli H et al (2009) Sedation during endoscopic retrograde cholangiopancreatography: The comparison of propofol - ketamine mixture infusion with bolus administrations. J Anesth 17(1):49–54
Chen WX, Lin HJ, Zhang WF et al (2005) Sedation and safety of propofol for therapeutic endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int 4(3):437–440
Kongkam P, Rerknimitr R, Punyathavorn S et al (2008) Propofol infusion versus intermittent meperidine and midazolam injection for conscious sedation in ERCP. J Gastrointestin Liver Dis 17(3):291–297
Varadarajulu S, Eloubeidi MA, Tamhane A et al (2007) Prospective randomized trial evaluating ketamine for advanced endoscopic procedures in difficult to sedate patients. Aliment Pharmacol Ther 25(8):987–997
Kayhan GE, Toprak HI, Aslan A et al (2013) Anaesthesia Induction with Ketamine: Propofol Combination (Ketofol) in Caesarean Delivery. Turk J Anaesth Reanim 41:131–136
Willman EV, Aldolfatto G (2007) A prospective evaluation of “Ketofol” (Ketamin/propofol combination) for procedural sedation and analgesia in the emergency department. Ann Emerg Med 49(1):23–30
Miller RD (2010) Intravenous anaesthetics. In: ‘Miller Anesthesia’ Translation Editor: Aydin D, 6th edition. Gunes Publishing House, Izmir, Turkey, pp 317–378
Robins K, Lyons G (2009) Intraoperative awereness during general anesthesia for cesarean delivery. Anesth Analg 109(3):886–890
Vallejo MC, Romeo RC, Davis DJ et al (2002) Propofol-ketamine versus propofol-fentanyl for outpatient laparoscopy: comparison of postoperative nausea, emesis, analgesia, and recovery. J Clin Anesth 4(6):426–431
Gottschling S, Meyer S, Krenn T et al (2005) Propofol versus midazolam/ketamine for procedural sedation in pediatric oncology. J Pediatr Hematol Oncol 27(9):471–476
Ghadami Yazdi A, Ayatollahi V, Hashemi A et al (2013) Effect of two Different Concentrations of Propofol and Ketamine Combinations (Ketofol) in Pediatric Patients under Lumbar Puncture or Bone Marrow Aspiration. Iran J Ped Hematol Oncol 3(1):187–192
Khajavi M, Emami A, Etezadi F et al (2013) Conscious Sedation and Analgesia in Colonoscopy: Ketamine/Propofol Combination has Superior Patient Satisfaction Versus Fentanyl/Propofol. Anesth Pain Med 3(1):208–213
Celik JB, Topal A, Erdem TB et al (2012) A comparison of two different sedation techniques in geriatric patients for endoscopic urological surgery. Turkish J Geriat 15(1):55–60
Rapeport DA, Martyr JW, Wang LP (2009) The use of “ketofol” (ketamine-propofol admixture) infusion in conjunction with regional anaesthesia. Anaesth Intens Care 37(1):121–123
Weatherall A, Venclovas R (2010) Experience with a propofol-ketamine mixture for sedation during pediatric orthopedic surgery. Paediatr Anaesth 20(11):1009–1016
Smischney NJ, Beach ML, Loftus RW et al (2012) Ketofol is associated with improved hemodynamics as an induction agent: a randomized, controlled trial. J Trauma Acute Care Surg 73(1):94–101
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baykal Tutal, Z., Gulec, H., Derelı, N. et al. Propofol-ketamine combination: a choice with less complications and better hemodynamic stability compared to propofol? On a prospective study in a group of colonoscopy patients. Ir J Med Sci 185, 699–704 (2016). https://doi.org/10.1007/s11845-015-1348-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1348-8