Abstract
Background
Adenoid cystic carcinoma is a malignant tumour of major and minor salivary glands. Distant metastasis and poor survival are persistent in the literature, with recent publications aimed at understanding molecular pathogenesis and development of pharmaceutical therapeutic options.
Aim
Provide an update of recent studies in the management of adenoid cystic carcinoma of the head and neck.
Methods
Literature search using Medline, Scopus, Google Scholar, the Cochrane Database of Systematic Reviews and the Cochrane central register of controlled trials for articles on adenoid cystic carcinoma from January 2005 to January 2015.
Conclusion
Adenoid cystic carcinoma is characterized by a slow growing mass, with distant metastasis independent of local or regional control. Primary tumour resection remains the preferred option with radiotherapy having an adjuvant role. Recent advances have been made with novel targeted therapies however, limited to clinical trials and advanced disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adenoid cystic carcinoma (ACC) is a rare malignant tumour of the secretory gland of both major and minor salivary glands [1]. It is characterized by slow growth, perineural invasion and distant metastases, independent of local or regional control. With persistently poor long-term survivals being reported, recent studies have sought to improve our understanding of the pathogenesis of the diseases and expand the scope of therapeutic options currently available. The aim of this article is to provide an update of recent studies in the management of adenoid cystic carcinoma of the head and neck (ACCHN).
Methods
A search was performed using Medline, Scopus, Google Scholar, the Cochrane Database of Systematic Reviews and the Cochrane central register of controlled trials for articles on ACC from January 2005 to January 2015. Article types included clinical trials, cohort studies, meta-analysis and systematic reviews. The search was limited to articles in English. MeSH terms included adenoid cystic carcinoma, head and neck, demographics, biomarkers, molecular therapy, radiology, perineural invasion and neck dissection. Relevant articles were selected following critical evaluation. We excluded studies on ACC from sites outside the Head and Neck.
Demographics
The United State’s National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program has recently been analyzed for cases of ACCHN between 1973 and 2007 [2]. Ellington et al. analyzed a total of 3026 patients and found a mean age at diagnosis of 57.4 years with a range of 11–99. There were 41 % males and 59 % females. These findings compare to earlier publications on ACC that describe diagnosis during the 5th or 6th decade of life with a marginal female prevalence. Race distribution was divided to 81.66 % white, 9.45 % black, 7.77 % Asian and 1 % others. The authors also comment that the overall incidence of ACCHN has steadily declined between 1973 and 2007, and that this was most notably in early stage disease.
Primary site
Whilst the study by Ellington et al. [2] comments that salivary gland primary tumours were the majority (57.98 %), followed by oral cavity tumours (36.91 %), and the oropharynx and nasopharynx accounted for 4.56 %, Li et al. [3] used the SEER database from a similar time period to examine the primary site in greater detail. Of 4008 tumours from various sub-sites of the head and neck, the most common locations were the parotid (22.6 %), gum and other oral cavity (including hard palate) (19.7 %), and submandibular glands (19.5 %). The major salivary glands account for 46.2 % of the total number, whilst the oral cavity minor salivary glands account for 30.2 % in total. This differs somewhat from the historic literature [4, 5], and some recent institutional studies [6], where ACC was more frequently seen within minor salivary glands compared to major salivary glands. The nose and middle ear were grouped together in the study, and account for 525 (13.1 %) of the total number. One and ninety-two (4.8 %) tracheal and laryngeal ACC were also found.
Histopathology and immunochemistry advances
Adenoid cystic carcinoma (ACC) is defined as “a basaloid tumour consisting of epithelial and myoepithelial cells in variable morphologic configurations, including tubular, cribriform and solid patterns” [7]. The ICD O-3 code for ACC as defined by the World Health Organisation is 8200/3 [8]. Gross pathology of an adenoid cystic tumour has been described as a hard unencapsulated mass [9]. A sagittal slice of the tumour would reveal a grey white coloured mass, with haemorrhage and necrosis indicative of high-grade transformation [10]. The cell cytoplasm is often clear with a hyperchromic and angulated nucleus [11].
Immunohistochemical staining with α-smooth muscle actin (αSMA) and S-100 protein may be used to observe myoepithelial cells surrounding pseudocysts, however, these are non-specific, and often weak or patchy [7]. Other non-specific stains include p63 [12] and CD117 (c-KIT), which may also be seen in polymorphous low-grade adenocarcinoma (PLGA) and monomorphic adenomas [13]. PLGA bears a superficial histological and immunophenotypic resemblance to ACC, but the tumours can be distinguished by much higher levels of Ki-67 (MIB1 antibody) in PLGA [6, 14].
Research into the molecular pathogenesis of ACC has demonstrated a recurrent translocation t(6;9)(q22-23;p23-24) in at least 80–90 % of cases of AdCC, which consistently results in a fusion of the MYB oncogene to the transcription factor gene NFIB [15]. This MYB–NFIB fusion gene has not been found in other salivary gland carcinomas and can be detected by RT-PCR, FISH analysis or by immunohistochemical staining of MYB-proteins [7, 16]. In addition to being diagnostically useful biomarker for adenoid cystic carcinoma, MYB and its downstream effectors are also novel potential therapeutic targets [17].
Tumour grade
Histopathological growth pattern are often mixed within an ACC tumour and are an important prognostic factor [5, 18, 19]. Poor survival rates have been found in patients with a predominant solid variant tumour, whilst the tubular variant is associated with a more favourable outcome [20, 21]. A number of grading systems have been suggested to correlate the biological course and prognostic influence of histopathological growth pattern subtype [5, 18, 19]. The current WHO classification refers to tumours by predominant pattern rather than actually assigning a numeric grade [22].
A new grading system has been proposed [23], which suggests that pathologist grade ACCHN tumours as either solid positive or negative. The study compared 81 surgically treated ACCHN tumours to be graded by both existing grading systems and the new proposed system. Limiting the grading system to solid positive (s+) or negative (s−) showed lower observer variability compared to existing grading systems, and an equal predictive power when comparing grade to survival.
Genetic mapping in adenoid cystic carcinoma
Genetic mapping of malignant tumours is a key step in developing novel targeted therapies. A recent publication by Allen et al. [24] sheds insight into the genetic landscape of ACC. The authors sequenced 55 exomes and five genomes from 60 ACC tumour samples to identify 710 nonsynonymous mutations across 643 genes (1–36 per tumour). Further methods were employed to distinguish between driver and passenger mutations. Analysis of driver genes identified such as; PIK3A, TP53 (5 %), PTEN, SMARCA2 (2 %), KDM6A and CREBBP revealing enhancement of chromatin remodelling (35 %), DNA damage, MYB, protein kinase A signalling and PI3K signalling.
Chromatin remodelling gene mutation is known to have oncogenic implications [25]. In the study by Allen et al. [24], the incidence was 35 %. Multiple aberrations were also noted in the actin dependent regulator of chromatin (SMARC) family [24], that are known to have a role in development of malignant disease [26, 27]. The study also observed mutations in NTNG1, SEMA3G, SEMA5A [24]. These domains are responsible for neural axon guidance cues [28], possibly explaining the propensity of perineural invasion by ACC tumours. The MYB–NFIB fusion oncogene was observed in 57 % of samples [24]. This study also highlights specific mutations in both MYB and NFIB genes suggesting a combined and individual role in oncogenesis between the two genes [24].
The variations in genetic mutations observed lead authors to conclude that ACC genetic mutation is characterized by MYB pathway alterations and functional biological mutations [24].
A study by Stephen et al. [29] elaborates on the exomal sequencing of ACC. The study conducted involved 23 ACC specimens and one regional lymph node metastatic specimen to reveal 312 somatic mutations (13 mutations per exome). Somatic mutations were observed in known oncogenic genes such as, CDKN2A, NOTCH1, NOTCH2, histone modification and chromatin remodelling pathways. Spen homolog transcription factor (SPEN) was observed following six mutations in five specimens of known solid histological subtype of ACC. SPEN is a regulator of the NOTCH signalling pathway [30]. Somatic mutations were also observed in NOTCH1 and NOTCH2 in three cases. The identification of these mutations may suggest an avenue for targeted therapy research.
Perineural invasion and distant metastasis
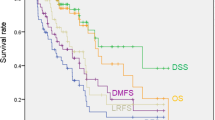
ACCHN often presents as a firm mass, with symptoms dependent on tumour location. Features of pain or regional nerve dysfunction are clinically indicative of the propensity of ACC to invade and metastasise via nerves. The role of perineural invasion as a prognostic indicator remains controversial, as a review found that there was a ‘plethora of conflicting data’, which suggests the answer may be in the affirmative, particularly if the nerve involved is above a certain diameter [31]. Perineural invasion may be defined as malignant cells in any of the three layers of the nerve sheath (epineurium, perineurium and endoneurium) or >33 % neural invasion [32]. A classification system has been proposed, with true perineural invasion, defined as onion bulb formation, circular cell formation or endoneural invasion, being classified as P1. Tumours adjacent to nerves without the characteristics above are classified as P2 [33]. In a small cohort of patients (n = 49), a higher recurrence rate was demonstrated in patients with P1 neural invasion [33]. Further to this, a recent international collaboration compared the clinical relevance of perineural invasion and intraneural invasion (defined as perineural invasion with tumour cells invading the axon) [34]. Although patients with perineural invasion were shown to have a poorer 5-year disease specific survival (DSS) compared to patients with no nerve involvement (77 vs 82 %, p = 0.04), there was no significant difference in overall survival (OS) between the two groups (74 % vs 77 %, p = 0.11).
However, survival analysis demonstrated that intraneural invasion was one of only two (the other being tumour site) independent predictors of DSS (p = 0.02) and OS (p = 0.03) [34].
Another clinical feature associated with ACC is the occurrence of distant metastases, independent of locoregional control. In one study, 82 of 111 (74 %) had distant metastases without failure at the primary site [35]. The lungs are the most common location for disease proliferation, accounting for approximately 75 % of 145 patients with distant metastases in a recent article. Bone (6.9 %), liver (3.4 %) and brain (2.1 %) were the next most common sites [36]. In 13.1 % of the patients, multiple metastases were found. Factors that influence the development of distant metastasis include age, primary tumour site (submandibular gland, paranasal sinuses palate and tongue), size (>4 cm), positive margins and solid tumours [35, 36]. Positive margins may indeed have the most significant impact on the development of distant metastasis. Shingaki et al. [37] reported a 89 % rate of developing distant metastasis with positive margins compared to 29 % in those patients whose tumours were fully resected (p = 0.012).
Surgery, radiotherapy and chemotherapy
The primary treatment modality for ACCHN remains wide surgical resection with clear margins.
Adjuvant radiotherapy (RT) has been shown to improve locoregional control for patients with ACC [38, 39], and many authors would consider this the standard of care [40]. However, controversy still exists, and a large review of 2286 patients with ACCHN in the National Cancer Institute’s Surveillance, Epidemiology, and End Results database showed no evidence of increased overall or cause-specific survival in patients receiving adjuvant RT [41].
Therefore, with ongoing clinical equipoise, reducing effects of radiotoxicity, which have significant impact on the patient’s quality of life, is of great importance. Mizoe et al. [42] reported on the use of carbon ions (CI) for the management of head and cancer in a phase II clinical trial. The cohort included 69 patients with ACC treated with CI RT alone. The authors report a 5-year local control rate of 73 % and an overall survival rate of 68 % for ACCHN [43]. There were no significant reports of radiotoxicity related events. A recent study also reports on the role of proton or carbon ion radiotherapy to manage unresectable or T4 tumours. The study involved 80 patients divided equally into two groups undergoing either proton or carbon ion radiotherapy. There were no significant differences between the two groups with the 5-year overall local control reported at 66 and 68 % for protons and CI, respectively. The lack of high grade toxicities has also been reported by other author’s [44] but the technology has yet to become widely used [45]. The use of adjuvant radiotherapy is yet to demonstrate a survival benefit [46, 47]. Radiotherapy, however, has a role in the management of painful metastasis, and metastatic ACC tumours are not as radioresistant as previously considered [48].
There are no currently recognized chemotherapy regimes for the management of ACCHN, either for primary treatment or the management of disease recurrence. There is some evidence that concurrent chemoradiotherapy, especially with platinum based chemotherapy seems to be effective in improving locoregional control [49]. In one study, 13 of 16 patients with unresectable disease were still alive with a median follow-up of 25 months [50]. The rationale for the addition of chemotherapy to radiotherapy may be that it provides a benefit to overcome the radioresistence of most salivary gland cancers [51].
A 2010 systematic review measuring anti-tumour activity with the use of chemotherapy by Laurie et al. reports no benefit of cytotoxic drugs outside clinical trial scenario, but highlights a palliative role in managing advanced ACC of salivary glands. Five trials involving 101 patients, treated with single cytotoxic agent were reviewed. Disease stabilization was the most commonly observed outcome (response duration 5–20 months) with mitoxantrone, vinorelbine and gemcitabine showing superior benefits. Cisplatin based combination regimes in 14 studies (n = 118) reported a response rate of 25 % with the benefit of disease stabilisation and symptom improvement [52].
The current consensus is that chemotherapy is avoided in the primary treatment of ACC, outside the clinical trial setting. Current publications highlighting the palliative role of chemotherapy in the management of advanced ACC only involves small cohort retrospective studies and is yet to be verified in a clinical trial setting.
Elective neck dissection
Cervical lymph node status is an important prognostic indicator in ACCHN [41, 53, 54]. Recent and past studies are consistent in reporting a lower survival in patients with node positive disease at time of primary therapy (5 year survival 44–48 % with node positive vs 73–77 % node negative) [5, 53, 55, 56]. Therapeutic neck dissection (TND) is indicated in the management of cervical node positive (N+) disease, but the role of elective neck dissection remains undefined largely due to the varying incidence of nodal spread in ACCHN reported at 4–29 % [40, 41, 53]. A multicentre retrospective study (n = 495) reported the clinical outcomes following neck dissection (ND) in managing ACCHN [53], with 275 patients having a neck dissection, 226 of these being carried out in clinically and radiologically N0 necks. Forty-seven (17 %) patients out of the 226 patients had node positive disease. The highest incidence rates of occult nodal metastases were in patients with oral cavity tumours (22 %; 25 of 116), and those with cancer of the paranasal sinuses (16 %; 4/24). The 5-year overall survival was reported at 44 % in the TND group, 65 % in the END group with occult nodes and 73 % without occult metastases (p = 0.017). Distant metastasis was higher in N+ patients (40 vs 27 % p = 0.029). In another paper on the same cohort of patients, the authors showed no statistical survival advantage for those that underwent END compared to those who did not [53]. Another study (n = 61) reported similar findings of lower survival rates with N+ patients at 5 years (56.8 % N+ vs 85 % N−) and 10 years (28.4 % N+ vs 81 % N−) p = 0.025 [54]. However, as there were only four patients with occult positive nodes, the paper failed to show a statistical difference between patients who underwent END compared to those who did not. Whilst some authors still advocate END in all cases [57], others suggest a more selective approach depending on the patient and tumour’s risk factors [53].
Novel and targeted therapy
Current research development in clinical trials aimed at establishing treatments for ACC is based on expanding our knowledge of the molecular framework that drives malignant cell characteristics (Table 1). At the time of writing, there are 24 registered clinical trials on ACC at ClinicalTrials.gov, the vast majority on novel or targeted therapies [58].
The proto-oncogene c-KIT was observed to be overexpressed in 89 % of ACC tumours [59], and therefore a number of phase II trials were initiated to investigate to role of Imatinib (c-KIT inhibitor) in the management of locally advanced and metastatic ACCHN, not amenable to surgical resection [60, 61]. The trials were stopped early for a number of reasons, including no objective tumour response being noted, disease progression in 40–80 % of patients and associated toxicity in 20–50 % of patients. The trials concluded that overexpression of c-KIT likely does not contribute ACC biological profile. Ghosal et al. [62] reported the benefit on imatinib/cisplatin drug combination in a cohort of 28 patients with a profile of advanced disease and c-KIT overexpression on histology. Three patients had partial response on imaging (CT/MRI) and five showed reduced uptake of FDG on PET imaging. Stable disease was reported in 19 cases with an average of 15 months to disease progression and overall median survival of 35 months (range 1–75). The drug combination was well tolerated and may provide disease stabilisation benefit in advanced cases of ACCHN.
Epidermal growth factor receptor (EGFR) has a role in the downstream signalling pathways that enhance tumour proliferation, invasion and metastasis [63]. A phase II clinical trial assessing the role gefitinib (EGFR inhibitor) in managing 37 advanced salivary gland tumours (18 ACC cases) reported no objective tumour response [64]. Secondary observations were a median overall survival of 25.9 months in cases of ACC, but clinical benefits of gefitinib were not observed. Another clinical trial using cetuximab (EGFR inhibitor) again showed no clinical responses or benefits [65], however, a study using combination regimes is promising [66]. For nine patients with locally advanced tumour, cetuximab and radiotherapy (65 Gy) was administered. Twelve patients with metastatic disease were treated with cetuximab, cisplation and 5-fluorouracil. In both groups, the objective response was over 40 %. The locally advanced arm had a median progression free survival of 64 months and a 100 % 2 years overall survival. Patients with distant metastases had a median progression free survival and overall survival of 13 and 24 months, respectively. Another clinical trial using lapatinib (dual EGFR and erb B2 tyrosine kinase inhibitor) again showed no objective response in 19 advanced ACC cases, but disease stabilisation was reported at 47 %, with 24 % for over 6 months [67]. Further evaluation may show lapatinib to provide clinical benefits with combination regimes.
Vascular endothelial growth factor receptors (VEGFR) play an important role in tumour angiogenesis, proliferation and migration in ACC. Chau et al. [68] reported a phase II clinical trial study with sunitinib (VEGFR inhibitor), treating 14 patients with progressive and recurrent/metastatic ACCHN. Sunitinib enhanced disease stabilisation in 11 patients and for >6 months in eight patients. Median overall survival was 18.7 months but again, no objective responses are reported.
Other pathways have been shown to be activated in ACC, such as the TrkC/NTRK3 signalling pathway [69], suggesting that Trk kinase inhibition may be a potential therapeutic option in ACC. (PI3)/AKT/mammalian target of rapamycin (mTOR) pathway in ACC is promising, with ACC cell lines exhibited increased phosphorylated Akt activity [70]. A phase II study in Korea using everolimus, an mTOR inhibitor, showed promising efficacy and good tolerability in 34 patients with progressive unresectable ACC [71]. A subset of ACC was shown to have mutations in RAS pathway genes, including BRAF, suggesting that the BRAF inhibitor, vemurafenib, may be effective in patients with activating BRAF kinase mutations [72, 73].
The MYB–NFIB fusion gene may be the most promising target for novel treatments. MYB and its target genes are a key oncogenic event in the pathogenesis of ACC [15]. The MYB–NFIB fusion gene is a consequence of 3′ loss in the region of MYB on chromosome 6, leading to a recurrent t(6;9)(q22-23;p23-24) translocation [15] following fusion with NFIB gene on chromosome 9 [15]. This in turn leads to activation of MYB target genes that have a pertinent role in oncogenesis such as cell cycle control, apoptosis and angiogenesis [15, 74]. Known downstream targets of MYB gene are cyclooxygenase-2(COX-2), Bcl-2 and c-kit [75]. As yet, there are no specific clinical trials involving novel therapies targeting MYB gene or subsequent downstream targets. Research instead is examining known and new downstream targets of MYB [76].
Conclusion
The management of ACCHN is an oncological challenge. Often presenting as a hard mass, common primary sites include major salivary glands, oral cavity hard palate subsite, paranasal sinuses and trachea. Recent reports highlight a new grading system and clinical implications of intraneural invasion. Surgical resection remains the primary method of management with radiotherapy having an unverified role in adjuvant treatment. Cervical lymph node status is an important prognostic indicator, hence the indications for TND are defined but the role of END remains in question. Promising advances have been in the development of novel therapies targeting molecular tumour biomarkers, however, the use of these drugs are limited to the clinical trial setting and in the management of advanced or recurrent disease.
References
Foote FW Jr, Frazell EL (1953) Tumors of the major salivary glands. Cancer 6(6):1065–1133
Ellington CL, Goodman M, Kono SA, Grist W, Wadsworth T, Chen AY et al (2012) Adenoid cystic carcinoma of the head and neck: incidence and survival trends based on 1973–2007 surveillance, epidemiology, and end results data. Cancer 118(18):4444–4451
Li N, Xu L, Zhao H, El-Naggar AK, Sturgis EM (2012) A comparison of the demographics, clinical features, and survival of patients with adenoid cystic carcinoma of major and minor salivary glands versus less common sites within the surveillance, epidemiology, and end results registry. Cancer 118(16):3945–3953
Matsuba HM, Thawley SE, Simpson JR, Levine LA, Mauney M (1984) Adenoid cystic carcinoma of major and minor salivary gland origin. Laryngoscope 94(10):1316–1318
Spiro RH, Huvos AG, Strong EW (1974) Adenoid cystic carcinoma of salivary origin. A clinicopathologic study of 242 cases. Am J Surg 128(4):512–520
Saghravanian N, Mohtasham N, Jafarzadeh H (2009) Comparison of immunohistochemical markers between adenoid cystic carcinoma and polymorphous low-grade adenocarcinoma. J Oral Sci 51(4):509–514
Simpson RH, Skalova A, Di Palma S, Leivo I (2014) Recent advances in the diagnostic pathology of salivary carcinomas. Virchows Archiv Int J Pathol 465(4):371–384
IARC (2015) International classification of diseases for oncology, ICD-O-3, 8200/3 adenoid cystic carcinoma. WHO. http://codes.iarc.fr/code/282. Accessed 6 Jan 2015
Jaso J, Malhotra R (2011) Adenoid cystic carcinoma. Arch Pathol Lab Med 135(4):511–515
Seethala RR, Hunt JL, Baloch ZW, Livolsi VA, Leon Barnes E (2007) Adenoid cystic carcinoma with high-grade transformation: a report of 11 cases and a review of the literature. Am J Surg Pathol 31(11):1683–1694
Ellis GL, Auclair PL (2008) Tumors of the salivary glands. Atlas of tumor pathology; 4th series, Fascicle 9. ARP Press, Silver Spring (MD), pp 225–259
Edwards PC, Bhuiya T, Kelsch RD (2004) Assessment of p63 expression in the salivary gland neoplasms adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and basal cell and canalicular adenomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97(5):613–619
Edwards PC, Bhuiya T, Kelsch RD (2003) C-kit expression in the salivary gland neoplasms adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and monomorphic adenoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95(5):586–593
Skalova A, Simpson RH, Lehtonen H, Leivo I (1997) Assessment of proliferative activity using the MIB1 antibody help to distinguish polymorphous low grade adenocarcinoma from adenoid cystic carcinoma of salivary glands. Pathol Res Pract 193(10):695–703
Persson M, Andren Y, Mark J, Horlings HM, Persson F, Stenman G (2009) Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck. Proc Natl Acad Sci USA 106(44):18740–18744
Stenman G (2013) Fusion oncogenes in salivary gland tumors: molecular and clinical consequences. Head Neck Pathol 7(Suppl 1):S12–S19
Brill LB 2nd, Kanner WA, Fehr A, Andren Y, Moskaluk CA, Loning T et al (2011) Analysis of MYB expression and MYB–NFIB gene fusions in adenoid cystic carcinoma and other salivary neoplasms. Modern Pathol Off J US Can Acad Pathol 24(9):1169–1176
Szanto PA, Luna MA, Tortoledo ME, White RA (1984) Histologic grading of adenoid cystic carcinoma of the salivary glands. Cancer 54(6):1062–1069
Perzin KH, Gullane P, Clairmont AC (1978) Adenoid cystic carcinomas arising in salivary glands: a correlation of histologic features and clinical course. Cancer 42(1):265–282
Patey DH, Thackray AC, Keeling DH (1965) Malignant disease of the parotid. Br J Cancer 19(4):712–737
Thackray AC, Lucas RB (1960) The histology of cylindroma of mucous gland origin. Br J Cancer 14:612–620
Seethala RR (2009) An update on grading of salivary gland carcinomas. Head Neck Pathol 3(1):69–77
van Weert S, van der Waal I, Witte BI, Leemans CR, Bloemena E (2015) Histopathological grading of adenoid cystic carcinoma of the head and neck: analysis of currently used grading systems and proposal for a simplified grading scheme. Oral Oncol 51(1):71–76
Ho AS, Kannan K, Roy DM, Morris LG, Ganly I, Katabi N et al (2013) The mutational landscape of adenoid cystic carcinoma. Nat Genet 45(7):791–798
Wolffe AP (2001) Chromatin remodeling: why it is important in cancer. Oncogene 20(24):2988–2990
Dalgliesh GL, Furge K, Greenman C, Chen L, Bignell G, Butler A et al (2010) Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature 463(7279):360–363
Tsurusaki Y, Okamoto N, Ohashi H, Kosho T, Imai Y, Hibi-Ko Y et al (2012) Mutations affecting components of the SWI/SNF complex cause Coffin–Siris syndrome. Nat Genet 44(4):376–378
Binmadi NO, Yang YH, Zhou H, Proia P, Lin YL, De Paula AM et al (2012) Plexin-B1 and semaphorin 4D cooperate to promote perineural invasion in a RhoA/ROK-dependent manner. Am J Pathol 180(3):1232–1242
Stephens PJ, Davies HR, Mitani Y, Van Loo P, Shlien A, Tarpey PS et al (2013) Whole exome sequencing of adenoid cystic carcinoma. J Clin Investig 123(7):2965–2968
Oswald F, Kostezka U, Astrahantseff K, Bourteele S, Dillinger K, Zechner U et al (2002) SHARP is a novel component of the Notch/RBP-Jkappa signalling pathway. EMBO J 21(20):5417–5426
Barrett AW, Speight PM (2009) Perineural invasion in adenoid cystic carcinoma of the salivary glands: a valid prognostic indicator? Oral Oncol 45(11):936–940
Liebig C, Ayala G, Wilks JA, Berger DH, Albo D (2009) Perineural invasion in cancer: a review of the literature. Cancer 115(15):3379–3391
Teymoortash A, Zieger L, Hoch S, Pagenstecher A, Hofer MJ (2014) Distinct microscopic features of perineural invasion in adenoid cystic carcinoma of the head and neck. Histopathology 64(7):1037–1039
Amit M, Binenbaum Y, Trejo-Leider L, Sharma K, Ramer N, Ramer I et al (2014) International collaborative validation of intraneural invasion as a prognostic marker in adenoid cystic carcinoma of the head and neck. Head Neck 2014:7. doi:10.1002/hed.23710
Amit M, Binenbaum Y, Sharma K, Ramer N, Ramer I, Agbetoba A et al (2014) Analysis of failure in patients with adenoid cystic carcinoma of the head and neck. An international collaborative study. Head Neck 36(7):998–1004
Gao M, Hao Y, Huang MX, Ma DQ, Luo HY, Gao Y et al (2013) Clinicopathological study of distant metastases of salivary adenoid cystic carcinoma. Int J Oral Maxillofac Surg 42(8):923–928
Shingaki S, Kanemaru S, Oda Y, Niimi K, Mikami T, Funayama A et al (2014) Distant metastasis and survival of adenoid cystic carcinoma after definitive treatment. J Oral Maxillofac Surg Med Pathol 26(3):312–316
Chen AM, Bucci MK, Weinberg V, Garcia J, Quivey JM, Schechter NR et al (2006) Adenoid cystic carcinoma of the head and neck treated by surgery with or without postoperative radiation therapy: prognostic features of recurrence. Int J Radiat Oncol Biol Phys 66(1):152–159
Shen C, Xu T, Huang C, Hu C, He S (2012) Treatment outcomes and prognostic features in adenoid cystic carcinoma originated from the head and neck. Oral Oncol 48(5):445–449
Bhayani MK, Yener M, El-Naggar A, Garden A, Hanna EY, Weber RS et al (2012) Prognosis and risk factors for early-stage adenoid cystic carcinoma of the major salivary glands. Cancer 118(11):2872–2878
Lloyd S, Yu JB, Wilson LD, Decker RH (2011) Determinants and patterns of survival in adenoid cystic carcinoma of the head and neck, including an analysis of adjuvant radiation therapy. Am J Clin Oncol 34(1):76–81
Mizoe JE, Hasegawa A, Jingu K, Takagi R, Bessyo H, Morikawa T et al (2012) Results of carbon ion radiotherapy for head and neck cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol 103(1):32–37
Takagi M, Demizu Y, Hashimoto N, Mima M, Terashima K, Fujii O et al (2014) Treatment outcomes of particle radiotherapy using protons or carbon ions as a single-modality therapy for adenoid cystic carcinoma of the head and neck. Radiother Oncol J Eur Soc Ther Radiol Oncol 113(3):364–370
Tsujii H, Kamada T (2012) A review of update clinical results of carbon ion radiotherapy. Jpn J Clin Oncol 42(8):670–685
Schlaff CD, Krauze A, Belard A, O’Connell JJ, Camphausen KA (2014) Bringing the heavy: carbon ion therapy in the radiobiological and clinical context. Radiat Oncol 9(1):88
Spiro RH (1997) Distant metastasis in adenoid cystic carcinoma of salivary origin. Am J Surg 174(5):495–498
Vander Poorten V, Hunt J, Bradley PJ, Haigentz M Jr, Rinaldo A, Mendenhall WM et al (2014) Recent trends in the management of minor salivary gland carcinoma. Head Neck 36(3):444–455
Sung MW, Kim KH, Kim JW, Min YG, Seong WJ, Roh JL et al (2003) Clinicopathologic predictors and impact of distant metastasis from adenoid cystic carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 129(11):1193–1197
Maruya S, Namba A, Matsubara A, Kakehata S, Takeda I, Shirasaki T et al (2006) Salivary gland carcinoma treated with concomitant chemoradiation with intraarterial cisplatin and docetaxel. Int J Clin Oncol 11(5):403–406
Samant S, van den Brekel MW, Kies MS, Wan J, Robbins KT, Rosenthal DI et al (2012) Concurrent chemoradiation for adenoid cystic carcinoma of the head and neck. Head Neck 34(9):1263–1268
Cerda T, Sun XS, Vignot S, Marcy PY, Baujat B, Baglin AC et al (2014) A rationale for chemoradiation (vs radiotherapy) in salivary gland cancers? On behalf of the REFCOR (French rare head and neck cancer network). Crit Rev Oncol Hematol 91(2):142–158
Laurie SAAL, Matthew GF, Sherman E, Pfister DG (2010) Systematic therapy in the management of metastatic or locally recurrent adenoid cystic carcinoma of the salivary gland; a systematic review. Lancet Oncol 12(8):815–824
Amit M, Binenbaum Y, Sharma K, Ramer N, Ramer I, Agbetoba A et al (2014) Incidence of cervical lymph node metastasis and its association with outcomes in patients with adenoid cystic carcinoma. An international collaborative study. Head Neck
Lee SY, Kim BH, Choi EC (2014) Nineteen-year oncologic outcomes and the benefit of elective neck dissection in salivary gland adenoid cystic carcinoma. Head Neck 36(12):1796–1801
Min R, Siyi L, Wenjun Y, Ow A, Lizheng W, Minjun D et al (2012) Salivary gland adenoid cystic carcinoma with cervical lymph node metastasis: a preliminary study of 62 cases. Int J Oral Maxillofac Surg 41(8):952–957
Fordice J, Kershaw C, El-Naggar A, Goepfert H (1999) Adenoid cystic carcinoma of the head and neck: predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg 125(2):149–152
Nobis CP, Rohleder NH, Wolff KD, Wagenpfeil S, Scherer EQ, Kesting MR (2014) Head and neck salivary gland carcinomas—elective neck dissection, yes or no? J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 72(1):205–210
US National Institutes of Health (2015) ClinicalTrials.gov. https://clinicaltrials.gov/ct2/results?term=Adenoid+cystic+carcinoma&pg=5. Accessed 11 Jan 2015
Tang Y, Liang X, Zheng M, Zhu Z, Zhu G, Yang J et al (2010) Expression of c-kit and slug correlates with invasion and metastasis of salivary adenoid cystic carcinoma. Oral Oncol 46(4):311–316
Pfeffer MR, Talmi Y, Catane R, Symon Z, Yosepovitch A, Levitt M (2007) A phase II study of imatinib for advanced adenoid cystic carcinoma of head and neck salivary glands. Oral Oncol 43(1):33–36
Hotte SJ, Winquist EW, Lamont E, MacKenzie M, Vokes E, Chen EX et al (2005) Imatinib mesylate in patients with adenoid cystic cancers of the salivary glands expressing c-kit: a Princess Margaret Hospital phase II consortium study. J Clin Oncol Off J Am Soc Clin Oncol 23(3):585–590
Ghosal N, Mais K, Shenjere P, Julyan P, Hastings D, Ward T et al (2011) Phase II study of cisplatin and imatinib in advanced salivary adenoid cystic carcinoma. Br J Oral Maxillofac Surg 49(7):510–515
Huang Y, Yu T, Fu X, Chen J, Liu Y, Li C et al (2013) EGFR inhibition prevents in vitro tumor growth of salivary adenoid cystic carcinoma. BMC Cell Biol 14:13
Jakob JA, Kies MS, Glisson BS, Kupferman ME, Liu DD, Lee JJ et al (2014) Phase II study of gefitinib in patients with advanced salivary gland cancers. Head Neck. doi:10.1002/hed.23647
Locati LD, Bossi P, Perrone F, Potepan P, Crippa F, Mariani L et al (2009) Cetuximab in recurrent and/or metastatic salivary gland carcinomas: a phase II study. Oral Oncol 45(7):574–578
Hitre E, Budai B, Takacsi-Nagy Z, Rubovszky G, Toth E, Remenar E et al (2013) Cetuximab and platinum-based chemoradio- or chemotherapy of patients with epidermal growth factor receptor expressing adenoid cystic carcinoma: a phase II trial. Br J Cancer 109(5):1117–1122
Agulnik M, Cohen EW, Cohen RB, Chen EX, Vokes EE, Hotte SJ et al (2007) Phase II study of lapatinib in recurrent or metastatic epidermal growth factor receptor and/or erbB2 expressing adenoid cystic carcinoma and non adenoid cystic carcinoma malignant tumors of the salivary glands. J Clin Oncol Off J Am Soc Clin Oncol 25(25):3978–3984
Chau NG, Hotte SJ, Chen EX, Chin SF, Turner S, Wang L et al (2012) A phase II study of sunitinib in recurrent and/or metastatic adenoid cystic carcinoma (ACC) of the salivary glands: current progress and challenges in evaluating molecularly targeted agents in ACC. Ann Oncol 23(6):1562–1570
Ivanov SV, Panaccione A, Brown B, Guo Y, Moskaluk CA, Wick MJ et al (2013) TrkC signaling is activated in adenoid cystic carcinoma and requires NT-3 to stimulate invasive behavior. Oncogene 32(32):3698–3710
Younes MN, Park YW, Yazici YD, Gu M, Santillan AA, Nong X et al (2006) Concomitant inhibition of epidermal growth factor and vascular endothelial growth factor receptor tyrosine kinases reduces growth and metastasis of human salivary adenoid cystic carcinoma in an orthotopic nude mouse model. Mol Cancer Ther 5(11):2696–2705
Kim DW, Oh DY, Shin SH, Kang JH, Cho BC, Chung JS et al (2014) A multicenter phase II study of everolimus in patients with progressive unresectable adenoid cystic carcinoma. BMC Cancer 14:795
Wetterskog D, Wilkerson PM, Rodrigues DN, Lambros MB, Fritchie K, Andersson MK et al (2013) Mutation profiling of adenoid cystic carcinomas from multiple anatomical sites identifies mutations in the RAS pathway, but no KIT mutations. Histopathology 62(4):543–550
Carlson J, Licitra L, Locati L, Raben D, Persson F, Stenman G (2013) Salivary gland cancer: an update on present and emerging therapies. Am Soc of Clin Oncol Educ Book 2013:257–263
Ramsay RG, Gonda TJ (2008) MYB function in normal and cancer cells. Nat Rev Cancer 8(7):523–534
Bell D, Roberts D, Karpowicz M, Hanna EY, Weber RS, El-Naggar AK (2011) Clinical significance of Myb protein and downstream target genes in salivary adenoid cystic carcinoma. Cancer Biol Ther 12(7):569–573
Adenoid Cystic Carcinoma Reseach Foundation (2015) Therapeutic targets. http://www.accrf.org/research/therapeutic-targets. Accessed 11 Jan 2015
Conflict of interest
We declare no conflict of interest and obtained no funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Subramaniam, T., Lennon, P. & O’Neill, J.P. Ongoing challenges in the treatment of adenoid cystic carcinoma of the head and neck. Ir J Med Sci 184, 583–590 (2015). https://doi.org/10.1007/s11845-015-1298-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1298-1