Abstract
Purpose
Chemotherapy-induced peripheral neuropathy (CIPN) is a major side effect of neurotoxic cancer treatment, often impacting treatment tolerability and patient functioning. Factors predicting an individual’s vulnerability for developing CIPN remain ill-defined. However, patient characteristics may contribute to CIPN risk, with obesity being a prevalent patient comorbidity. This study was aimed at evaluate if being overweight (BMI ≥ 25 kg/m2) was associated with worse symptomatic, clinical, and functional CIPN following neurotoxic cancer treatment.
Methods
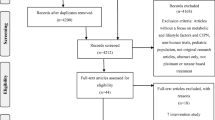
Three hundred seventy-nine cancer survivors were assessed 5 (IQR 3–5) months post oxaliplatin or paclitaxel treatment via comprehensive patient-reported, clinical, and functional CIPN measures. Patients classified as overweight (BMI ≥ 25 kg/m2) were compared to those within the normal BMI range (< 25 kg/m2). Multilinear regression was conducted to evaluate the association between patient clinical factors and CIPN severity.
Results
Most patients reported CIPN symptoms (78%), with deficits evident on clinical examination. Overweight patients (n = 242, 63.8%) had significantly worse CIPN across symptomatic, objective clinical, and functional outcomes compared to those with a normal BMI (p < .05). In multivariate linear regression, older age (B = .088, 95%CI = .053–.122, p < .001), larger waist circumference (B = .030, 95%CI = .001–.059, p < .05), and larger BSA (B = 2.41, 95%CI = .34–04.48, p < .05) were associated with CIPN. Diabetes and BMI were significant on univariate analysis but not in the final models.
Conclusions
Overweight patients represent a large proportion of cancer survivors who may be particularly impacted by CIPN, requiring closer monitoring and referral to supportive services. Accessible data such as a patient’s general and abdominal obesity status may aid in formulating personalized treatment.
Implications for Cancer Survivors
Identifying routinely measured patient characteristics which may contribute to an individual’s CIPN risk profile could assist with informing treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) is a dose-limiting side effect of neurotoxic cancer treatments including oxaliplatin and paclitaxel which are routinely used to treat common cancers [1]. CIPN can be irreversible, causing functional impairment and detriment to long-term quality of life [2]. Despite the prevalence and persistent impact of CIPN, there is a paucity of effective prevention and treatment [3]. Dose modification is currently the only recommended strategy available to clinicians to mitigate CIPN [4]. However, dose modification may reduce treatment efficacy [5, 6] and the impact of dose modification on long-term CIPN outcomes remains poorly characterized. Additionally, a spectrum of CIPN onset and severity can occur amongst homogenously treated cohorts, suggesting a role for individual risk factors [7]. However, risk factors which contribute to an individual’s vulnerability to develop CIPN remain ill-defined, in part due to the lack of a comprehensive quantitative CIPN assessment to validate putative risk factors [8]. Regardless, patient characteristics, comorbidities, and lifestyles have been increasingly indicated as potential risk factors. In particular, conditions associated with metabolic syndrome have emerged as probable candidates, due to their association with type 2 diabetes mellitus, a known etiology of peripheral neuropathy [9].
Of the conditions associated with metabolic syndrome, obesity is the most prevalent, reaching pandemic levels [10] with 39% of adults being overweight or obese worldwide [11]. Although obesity is a frequent comorbidity of type 2 diabetes [10], evidence from animal models and patient studies has suggested that obesity may induce peripheral nerve dysfunction in normoglycemic conditions[12, 13]. Further, centralized fat distribution has been specifically identified as contributing to greater neuropathy risk in non-oncological populations [12,13,14], possibly indicating neurotoxic effects associated with obesity.
A recent systematic review evaluating CIPN risk factors in taxane- and oxaliplatin-treated patients highlighted the discord around the role of obesity, mostly defined using body mass index (BMI), in the development of CIPN [15]. Though some studies demonstrated an association between obesity and greater CIPN prevalence and severity [16,17,18], other investigations failed to find any association [19,20,21,22]. These discrepancies likely reflect heterogeneity in patient populations, timing of assessment, and definitions of CIPN. Moreover, though no standard CIPN measure was utilized across all studies, patients were commonly assessed using clinician grading scales [16,17,18] which display poor sensitivity and lack of concurrence with patient reports and objective CIPN measures [23, 24].
Further, though CIPN can result in functional impairment, investigations into the additional impact obesity may have on patient function are lacking. As such, the association between obesity and CIPN outcomes remains ill-defined.
Given the prevalence of obesity, it is important to clarify the impact being overweight may have on CIPN outcomes. Therefore, this study was aimed at evaluating if being overweight was associated with worse symptomatic, clinical, and functional CIPN outcomes following treatment with two of the most commonly utilized neurotoxic chemotherapies, oxaliplatin and paclitaxel.
Methods
Patients and study design
Patients who received oxaliplatin or paclitaxel treatment were referred from July 2015 to February 2020 for comprehensive cross-sectional clinical and functional assessments 3–12 months post completion of neurotoxic treatment. Patients were eligible for inclusion if they were still receiving non-neurotoxic cancer treatment such as trastuzumab or 5-fluorouracil at the time of assessment. Written informed consent was obtained in accordance with the Declaration of Helsinki, with studies approved by the Sydney Local Health District and South Eastern Sydney Local Health District Human Research Ethics Committees.
Neuropathy assessment
Patients reported symptomatic CIPN burden via the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group-Neurotoxicity (FACT-GOG-Ntx, range 0–52) [25, 26], with lower scores indicating greater burden. Items 1 “I have numbness or tingling in my hands” and 2 “I have numbness or tingling in my feet” were used to describe specific patient-reported symptoms and severity (Supplementary methods) [27].
CIPN was clinically assessed via the Total Neuropathy Score clinical version (TNSc © Johns Hopkins University), a composite grading score of patient symptom report and clinical neurological examination, which addresses some of the limitations of unimodal CIPN assessment [1, 28, 29] (Supplementary methods), with greater CIPN severity indicated by higher scores (range 0–24) [28, 29]. von Frey monofilaments and two-point discrimination were preformed to assess distal sensation in the upper and lower limbs respectively (Supplementary methods). Similarly, functional assessments were undertaken using the grooved pegboard test as a measure of upper limb manual dexterity [30]. Lower limb functioning, indicated by standing balance was assessed via postural sway using a Swaymeter (Neuroscience Research Australia, Sydney) [31, 32]. Balance conditions were combined into a summed postural sway path length, with longer length indicating greater deficits [33] (Supplementary methods).
Clinical information and body composition measurements
Clinical and treatment information was retrieved from medical records in addition to pre-treatment height (m) and weight (kg). Body mass index (BMI) was calculated using weight (kg) divided by height (m) squared. Patients were classified as having normal weight (BMI < 25 kg/m2) or overweight (BMI ≥ 25 kg/m2) [11]. Normal body surface area (BSA) was classified as ≤1.9 m2 for males and ≤ 1.6 m2 for females calculated via the Mosteller equation [34]. Chemotherapy dose was prescribed based on uncapped BSA. Dosing information was used to calculate relative dose intensity (RDI, %) by dividing the total dose of administered chemotherapy treatment by planned total dose originally [35]. Metastatic cases were managed according to Australian government cancer treatment protocol guidelines, supplemented by clinician notes [36].
During CIPN assessments, additional anthropometric measurements were taken in a subset of patients (n = 149). Hip measurements (cm) were taken from the largest part of the buttocks, with waist measurements (cm) taken in line with the navel [12]. Abdominal obesity was defined as elevated waist circumference (males ≥ 94 cm, females ≥ 80 cm) based on published consensus guidelines [37]. Further measures for abdominal obesity were defined by the waist-to-hip ratio (WHR), calculated as waist circumference divided by hip circumference (males ≥ 0.95, females ≥ 0.80) [38].
Data analysis
Chi-square or independent samples t tests were used to compare categorical or continuous clinical factors and CIPN outcomes between oxaliplatin- and paclitaxel-treated patients. Additionally, CIPN outcomes were compared between patients classified as having normal weight or overweight based on BMI. Overweight patients (BMI between 25 and 29 kg/m2) and obese patients (BMI ≥ 30 kg/m2) were combined and compared to patients within the normal BMI range. Bootstrapping was performed based on 1000 bootstrap samples. Results are presented as the mean with standard deviation or median with interquartile range (IQR) as appropriate.
Linear regression was utilized to assess the association between measurements of obesity (BMI, BSA (uncapped), waist circumference, and waist-to-hip ratio) and clinical factors (age, sex, diabetic status, time since treatment, cumulative dose, relative dose intensity) with CIPN severity based on the TNSc. Missing data was handled using listwise deletion with results indicating complete case analysis. Variables identified as significant (p < .05) in univariate analysis were included in multivariate models. Factors not contributing to the model (p > .1) were eliminated during backward stepwise regression, with the remaining significant variables retained in the final multivariable model being reported. To avoid violating collinearity, two models were constructed substituting generalized measures of obesity (BSA and BMI) [14]. Q-Q residual plots were used to check normality and variance of the data. All analyses were performed using SPSS (Version 25, IBM) with significance indicated as p < .05.
Results
Patient characteristics
The cohort consisted of 379 patients (age 57.9 ± 12.5 years, female 77.8%, n = 295) who had completed neurotoxic cancer treatment 5 (IQR 3–8) months previously (Table 1). The most common cancer types were breast (40.6%), colorectal (27.7%), and ovarian (12.9%). Paclitaxel- (n = 245) and oxaliplatin-treated participants (n = 134) were comparable in age and diabetic status, but differed significantly in time since treatment completion, relative dose intensity, and sex, with more paclitaxel-treated patients being female, receiving a higher dose intensity, and assessed at a longer time since treatment completion (p < .05; Supplementary Table 1).
Of the total cohort, 63.8% (n = 242) were overweight (BMI ≥ 25 kg/m2), with 45.5% (n = 110) of these overweight patients having a BMI ≥ 30 kg/m2. Based on sex-specific values, 79.3% (n = 298) had abnormal BSA. Of those with measures of central obesity (n = 149), 85.2% (n = 127) had abnormal waist circumference and waist-to-hip ratio (WHR) (Table 2). There was no difference in the proportion of patients with abnormal waist circumference, BMI, or BSA between oxaliplatin- and paclitaxel-treated groups (N.S., Supplementary Table 1), with the proportion of oxaliplatin- and paclitaxel-treated patients being comparable in the overweight (BMI ≥ 25 kg/m2) and normal weight groups.
Symptomatic, clinical, and functional CIPN severity
Clinical, functional, and patient-reported neurological assessment outcomes for the whole cohort are presented in Table 3. Oxaliplatin-treated patients demonstrated greater CIPN severity compared to paclitaxel-treated patients, across patient-reported, clinical, and functional outcomes, suggesting greater symptomatic and objective CIPN in this cohort (Supplementary Table 2).
In total, CIPN symptoms were reported by the majority of the total cohort (78.5%, n = 296), with mild to moderate severity on patient-reported and clinical outcome measures (Table 3) in line with previous reports [39, 40]. More patients reported persistent numbness and tingling in the feet (74.5%; n = 281) compared to the hands (66%; n = 250).
During clinical examination, reduced deep tendon reflexes (64.8%, n = 239) and deficits in pinprick sensibility (61.5%, n = 227) were most frequently observed, with vibration sensibility being reduced in 34.1% of patients (n = 126). Manual muscle testing was normal for most patients (91.6%, n = 338), consistent with a sensory predominant neuropathy.
CIPN outcomes for patients classified as overweight
Overweight patients (BMI ≥ 25 kg/m2) had greater overall patient-reported symptom burden compared to patients classified as having normal weight (FACT-GOG-Ntx; normal:43.80 ± 8.35, overweight 40.20 ± 8.93, p < .01, Table 3) Specifically, overweight patients were more likely to report symptoms of numbness and tingling in the hands (X2(1, N = 375) = 14.33, p < .001) and feet (X2(1, N = 375) = 16.60, p < .001, Fig. 1), with a significantly larger proportion also reporting greater severity of CIPN symptoms in the feet compared to patients with normal weight (X2(1, N = 375) = 5.04, p < .05, Fig. 1).
Compared to those with normal weight, overweight individuals (BMI ≥ 25 kg/m2) demonstrated significantly worse deficits on clinical examination (TNS; normal weight 3.71 ± 2.85, overweight 4.85 ± 2.86, p < .05). Moreover, though they did not differ in specific tests of distal sensation, consistent with patient report, overweight individuals were more likely to demonstrate functional deficits in the upper limbs (pegboard; normal weight 72.75 ± 24.43 s, overweight 80.93 ± 25.72 s, p < .05) as well as significantly greater balance deficits (postural sway; normal 723.48 ± 235.79 mm, overweight 824.26 ± 281.88 mm, p < .01; Table 3).
Association between clinical factors, generalized and centralized obesity measures, and CIPN
Linear regression was conducted to evaluate the association between patient and clinical variables, including measures of general and central obesity, with CIPN severity (TNSc).
Univariate obesity measures and clinical variables associated with CIPN are presented in Table 4. WHR, cumulative dose, relative dose intensity, and months post treatment were non-significant factors in univariate analysis and not included in multivariate models (N.S.).
Two multivariable models were constructed based on each measurement of generalized obesity (model 1: BMI, model 2: BSA). In the first multivariate model (F(2,134) = 15.91, p < .001, r2 = .19), older age (B = .088, 95%CI = .053–.122, p < .001), and larger waist circumference (B = .030, 95%CI = .001–.059, p < .05) were significantly associated with worse CIPN severity. However, BMI, sex, chemotherapy type, and diabetic status did not contribute to the final model and were excluded during backwards regression.
In the second model (F(2,134) = 16.66, p < .0001, r2 = 0.20), older age (B = .096, 95%CI = .061–.130, p < .001) was also associated with worse CIPN severity, as was larger BSA (B = 2.409, 95%CI = .340–4.478, p < .05). Waist circumference, chemotherapy type, diabetes, and sex were non-significant factors in the final model (N.S.).
Discussion
This study was aimed at evaluating if being overweight (BMI ≥ 25 kg/m2) was associated with worse symptomatic, clinical, and functional CIPN following neurotoxic cancer treatment. Most of the cohort reported residual CIPN symptoms, with deficits also evident on clinical examination. Patients who were classified as overweight had significantly worse CIPN across symptomatic, objective clinical, and functional outcomes compared to those with a normal BMI. In multivariate linear regression, older age, larger waist circumference, and BSA were the main factors associated with CIPN. Diabetic status and BMI were significant on univariate analysis but failed to contribute to the final models.
Across western populations, obesity is highly prevalent with 71% of American and 67% of Australian adults having a BMI ≥ 25 kg/m2 [41]. In the current Australian cohort, 63.8% of cancer survivors were overweight, with 29% having a BMI ≥ 30 kg/m2. Previously, 22–55% of paclitaxel- and oxaliplatin-treated patients have been classified as obese (BMI ≥ 30 kg/m2) [9, 16, 42] likely reflecting heterogeneity in obesity rates between international populations [11]. Though BMI is used widely to report obesity, waist circumference has been highlighted as a more reliable estimator of adiposity and predictor of chronic diseases such type 2 diabetes [11, 43]. In the USA, more than 70% of women over the age of 50 exceed the waist circumference threshold (≥80 cm) for abdominal obesity, with the rate increasing with age [44, 45]. Similarly, 83% of Australian women over the age of 65 years were classified as having abdominal obesity [41], comparable to the rates of elevated waist circumference in the current female predominant study (85.2%).
Symptomatic, clinical, and functional CIPN outcomes for overweight cancer survivors
Comparable with other studies utilizing patient report [9, 21], the majority of the cohort (78.5%) described some level of residual CIPN symptoms, with most patients expressing greater severity of symptoms in the feet. Correspondingly, a large proportion of patients demonstrated deficits in clinical examination suggestive of sensory predominant neuropathy, consistent with previous reports [39, 40]. Overweight patients (BMI ≥ 25 kg/m2) were more likely to report CIPN symptoms and describe greater lower limb severity and worse overall symptom burden. Consistent with these observations, obesity has been identified as a predictor of patient-reported CIPN symptom burden in a large prospective study of breast cancer patients [9]. Similarly, patients reporting lower limb CIPN following platinum or taxane treatment were more likely to be obese [46]. However, patient report alone may be confounded by the increased mechanical force exerted on weight-bearing extremities in overweight individuals, potentially influencing patient perception of CIPN symptoms [42]. Consequently, additional CIPN assessment may mitigate the limitations of unimodal patient report. While two small studies have previously utilized clinical examination to quantify CIPN in paclitaxel-treated breast cancer patients, BMI was not found to be an independent risk factor for CIPN incidence [5, 47]. Further, there was no evidence of worsened vibration, cold perception, or light touch in objective examination of sensation in overweight cancer survivors with CIPN [42]. Similarly, this study did not identify measurable differences in sensory function in the upper or lower limbs. However, significant differences in a validated clinical assessment tool (TNSc) for CIPN were identified, suggestive of objective neurological deficits.
Importantly, this study assessed functional impairment associated with obesity and CIPN utilizing objective assessment including quantifying balance impairments. In the present cohort, overweight patients demonstrated increased postural sway, an objective indicator of balance deficits [32]. Consistent with these findings, overweight survivors with CIPN have previously reported significantly greater balance deficits compared to patients with CIPN and a normal BMI, with obese survivors also demonstrating worse balance scores on functional scales [42]. Similarly, in the present cohort, functional impairment in the hands were reflected in increased pegboard times, indicating reduced manual dexterity for overweight patients. In addition to greater functional burden associated with increased CIPN severity, being overweight may exacerbate functional deficits, with balance impairment reported to occur in overweight individuals without cancer [48]. Moreover, there is growing evidence supporting exercise as a strategy to ameliorate CIPN symptoms and related balance deficits [31, 49, 50]. Though physical activity levels were not recorded in this study, overweight individuals are less likely to meet recommended guidelines for physical activity, potentially forgoing some benefits for CIPN [51]. Given that cancer survivors with CIPN are nearly twice as likely to experience falls [33, 46], overweight individuals experiencing symptoms may be at particular risk and may benefit from supportive services such as referrals to occupational therapists and physiotherapists.
Factors associated with CIPN severity
In the present study, older age, larger waist circumference, and BSA were the main factors associated with CIPN. Diabetic status and BMI were significant on univariate analysis but failed to contribute to the final models. Multiple previous studies have demonstrated more severe patient-reported, clinician-graded, and objective CIPN with older age [5, 16, 52]. Similarly, large population studies have identified obesity based on BMI as an independent risk factor for CIPN [9, 16, 53], though these findings are not universal [19, 20]. Variability may be partly attributed to many earlier studies utilizing unimodal CIPN assessment such as a 4-point clinical-grading scale, with most analyses being conducted retrospectively. Interestingly, in the present study, waist circumference and BSA, not BMI, were associated with greater CIPN severity based on a validated clinical assessment tool (TNSc).
Waist circumference is a reliable measure of adiposity and indicator of poor body composition, which may influence the pharmacokinetics of neurotoxic treatment [11, 54]. Accordingly, when BSA was included in the model, waist circumference was no longer a significant predictor. BSA is used to calculate chemotherapy dose as it mitigates variability in adiposity distribution to a greater degree than BMI [55]. However, body composition may impact the pharmacokinetics of cancer treatment. Specifically, individuals with greater adiposity may be exposed to neurotoxic agents for a longer period [18] as lipophilic agents, including paclitaxel and oxaliplatin, accumulate in adipose tissue and have the potential to be re-released [56, 57]. Moreover, as anti-cancer drugs are generally metabolized within lean metabolic tissues, patients with larger BSA and lower lean body mass may essentially receive higher doses of neurotoxic cancer treatment and consequently experience greater dose-limiting toxicities such as neuropathy [58]. While CIPN prevalence and severity are broadly associated with cumulative dose [59], surprisingly, relative dose intensity was not a significant predictor in either model, suggesting that individual characteristics may be playing a more significant role than crude measures of dose. As such, more accurate evaluation of body composition and subsequent normalizing of dosing could assist in reducing toxicity [58]. Though imaging methods such as computed tomography scans provide an accurate estimation of body composition [18], waist circumference may offer an alternative estimation of centralized adiposity and body composition which can be easily implemented in routine clinical practice.
In this study, diabetic status was not associated with CIPN severity in the final models. Though some investigations have identified diabetes as a risk factor for CIPN [7, 17, 60], others have failed to find an association [5, 22, 46, 61]. However, diabetes is a common exclusion criterion for many CIPN trials and may be underrepresented as a risk factor. Moreover, the presence of diabetic neuropathy, time of diagnosis, or extent of diabetic control may better characterize the contribution of diabetes to CIPN vulnerability and need to be addressed in future trials.
Though the contribution of glycemic status to CIPN risk needs to be further elucidated, there is a growing body of evidence for obesity-related neuropathy amongst normoglycemic obese individuals without cancer [12, 14, 62]. Specifically, larger waist circumference has been associated with neuropathy risk in normoglycemic obese individuals independent from BMI [14], with inflammatory processes suggested as the primary pathophysiological mechanism [63, 64]. It is also possible that systemic metabolic and inflammatory processes linked to centralized obesity mediate the association with neuropathy risk [14]; however, these mechanistic relationships require further investigation in neurotoxic-treated cancer population.
Given the prevalence of obesity, overweight patients represent a large proportion of cancer survivors who may be particularly affected by CIPN and benefit most from supportive services, such as referrals to exercise physiologist, and occupational and physiotherapists. The factors identified in this study should be verified in large-scale trials, conducted longitudinally with baseline neuropathy assessment to confirm whether obese patients are impacted more severely by CIPN. Nevertheless, this study highlights the potential utility of routinely measured patient characteristics which may contribute to an individual’s CIPN risk profile and may assist with informing treatment decisions. Specifically, easily accessible data regarding general and central obesity status may aid in formulating a personalized approach to treatment through more nuanced dosing and by identifying patients warranting closer neurological monitoring to detect developing impairment and alter regimen prior to irreversible long term clinical disability.
^Cumulative dose based on uncapped BSA
^BSA not capped at 2 m2
Normal body mass index (BMI; n = 377) < 25 kg/m2; overweight ≥ 25 kg/m2; *p < .05, comparison between normal and overweight patients. Bootstrapping was conducted based on 1000 bootstrapped samples
Data availability
All data generated or analyzed during this study are included in this published article.
References
Argyriou AA, Park SB, Islam B, Tamburin S, Velasco R, Alberti P, et al. Neurophysiological, nerve imaging and other techniques to assess chemotherapy-induced peripheral neurotoxicity in the clinical and research settings. J Neurol Neurosurg Psychiatry. 2019. https://doi.org/10.1136/jnnp-2019-320969.
Swain SM, Arezzo JC. Neuropathy associated with microtubule inhibitors: diagnosis, incidence, and management. Clin Adv Hematol Oncol. 2008;6(6):455–67.
Hershman DL, Lacchetti C, Dworkin RH, Lavoie Smith EM, Bleeker J, Cavaletti G, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32(18):1941–67. https://doi.org/10.1200/jco.2013.54.0914.
Loprinzi CL, Lacchetti C, Bleeker J, Cavaletti G, Chauhan C, Hertz DL, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: ASCO guideline update. J Clin Oncol. 2020;0(0):JCO.20.01399. https://doi.org/10.1200/jco.20.01399.
Robertson J, Raizer J, Hodges JS, Gradishar W, Allen JA. Risk factors for the development of paclitaxel-induced neuropathy in breast cancer patients. J Peripher Nerv Syst. 2018;23(2):129–33. https://doi.org/10.1111/jns.12271.
Veitch Z, Khan OF, Tilley D, Tang PA, Ribnikar D, Stewart DA, et al. Impact of cumulative chemotherapy dose on survival with adjuvant FEC-D chemotherapy for breast cancer. J Natl Compr Cancer Netw. 2019;17(8):957–67. https://doi.org/10.6004/jnccn.2019.7286.
Hershman DL, Till C, Wright JD, Awad D, Ramsey SD, Barlow WE, et al. Comorbidities and risk of chemotherapy-induced peripheral neuropathy among participants 65 years or older in Southwest Oncology Group clinical trials. J Clin Oncol. 2016;34(25):3014–22. https://doi.org/10.1200/JCO.2015.66.2346.
Rivera DR, Ganz PA, Weyrich MS, Bandos H, Melnikow J. Chemotherapy-associated peripheral neuropathy in patients with early-stage breast cancer: a systematic review. J Natl Cancer Inst. 2017;110(2). https://doi.org/10.1093/jnci/djx140.
Greenlee H, Hershman DL, Shi Z, Kwan ML, Ergas IJ, Roh JM, et al. BMI, lifestyle factors and taxane-induced neuropathy in breast cancer patients: the pathways study. J Natl Cancer Inst. 2017;109(2). https://doi.org/10.1093/jnci/djw206.
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288–98. https://doi.org/10.1038/s41574-019-0176-8.
WHO. Obesity and overweight. World Health Organization. 2020. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. 2020.
Callaghan BC, Xia R, Reynolds E, Banerjee M, Rothberg AE, Burant CF, et al. Association between metabolic syndrome components and polyneuropathy in an obese population. JAMA Neurol. 2016;73(12):1468–76. https://doi.org/10.1001/jamaneurol.2016.3745.
Davidson EP, Coppey LJ, Calcutt NA, Oltman CL, Yorek MA. Diet-induced obesity in Sprague–Dawley rats causes microvascular and neural dysfunction. Diabetes Metab Res Rev. 2010;26(4):306–18. https://doi.org/10.1002/dmrr.1088.
Callaghan BC, Reynolds E, Banerjee M, Chant E, Villegas-Umana E, Feldman EL. Central obesity is associated with neuropathy in the severely obese. Mayo Clin Proc. 2020;95(7):1342–53. https://doi.org/10.1016/j.mayocp.2020.03.025.
Timmins HC, Mizrahi D, Li T, Kiernan MC, Goldstein D, Park SB. Metabolic and lifestyle risk factors for chemotherapy-induced peripheral neuropathy in taxane and platinum-treated patients: a systematic review. J Cancer Surviv. 2021. https://doi.org/10.1007/s11764-021-00988-x.
Barginear M, Dueck AC, Allred JB, Bunnell C, Cohen HJ, Freedman RA, et al. Age and the risk of paclitaxel-induced neuropathy in women with early-stage breast cancer (Alliance A151411): results from 1,881 patients from Cancer and Leukemia Group B (CALGB) 40101. Oncologist. 2019;24(5):617–23. https://doi.org/10.1634/theoncologist.2018-0298.
Ottaiano A, Nappi A, Tafuto S, Nasti G, De Divitiis C, Romano C, et al. Diabetes and body mass index are associated with neuropathy and prognosis in colon cancer patients treated with capecitabine and oxaliplatin adjuvant chemotherapy. Oncology. 2016;90(1):36–42. https://doi.org/10.1159/000442527.
Dijksterhuis WPM, Pruijt MJ, Woude SO, Klaassen R, Kurk SA, Oijen MGH, et al. Association between body composition, survival, and toxicity in advanced esophagogastric cancer patients receiving palliative chemotherapy. J Cachexia Sarcopenia Muscle. 2019;10(1):199–206. https://doi.org/10.1002/jcsm.12371.
Furlanetto J, Eiermann W, Marmé F, Reimer T, Reinisch M, Schmatloch S, et al. Higher rate of severe toxicities in obese patients receiving dose-dense (dd) chemotherapy according to unadjusted body surface area: results of the prospectively randomized GAIN study. Ann Oncol. 2016;27(11):2053–9. https://doi.org/10.1093/annonc/mdw315.
Schneider BP, Zhao F, Wang M, Stearns V, Martino S, Jones V, et al. Neuropathy is not associated with clinical outcomes in patients receiving adjuvant taxane-containing therapy for operable breast cancer. J Clin Oncol. 2012;30(25):3051–7. https://doi.org/10.1200/jco.2011.39.8446.
Hershman DL, Unger JM, Crew KD, Till C, Greenlee H, Minasian LM, et al. Two-year trends of taxane-induced neuropathy in women enrolled in a randomized trial of acetyl-L-carnitine (SWOG S0715). J Natl Cancer Inst. 2018;110(6):669–76. https://doi.org/10.1093/jnci/djx259.
Simon N, Danso M, Alberico T, Basch E, Bennett A. The prevalence and pattern of chemotherapy-induced peripheral neuropathy among women with breast cancer receiving care in a large community oncology practice. Qual Life Res. 2017;26(10):2763–72. https://doi.org/10.1007/s11136-017-1635-0.
Postma TJ, Aaronson NK, Heimans JJ, Muller MJ, Hildebrand JG, Delattre JY, et al. The development of an EORTC quality of life questionnaire to assess chemotherapy-induced peripheral neuropathy: The QLQ-CIPN20. Eur J Cancer. 2005;41(8):1135–9. https://doi.org/10.1016/j.ejca.2005.02.012.
Basch E, Iasonos A, McDonough T, Barz A, Culkin A, Kris MG, et al. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol. 2006;7(11):903–9. https://doi.org/10.1016/s1470-2045(06)70910-x.
Calhoun EA, Welshman EE, Chang CH, Lurain JR, Fishman DA, Hunt TL, et al. Psychometric evaluation of the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group-Neurotoxicity (Fact/GOG-Ntx) questionnaire for patients receiving systemic chemotherapy. Int J Gynecol Cancer. 2003;13(6):741–8.
Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. https://doi.org/10.1186/1477-7525-1-79.
Timmins HC, Li T, Huynh W, Kiernan MC, Baron-Hay S, Boyle F, et al. Electrophysiological and phenotypic profiles of taxane-induced neuropathy. Clin Neurophysiol. 2020;131:1979–85. https://doi.org/10.1016/j.clinph.2020.02.028.
Cavaletti G, Jann S, Pace A, Plasmati R, Siciliano G, Briani C, et al. Multi-center assessment of the Total Neuropathy Score for chemotherapy-induced peripheral neurotoxicity. J Peripher Nerv Syst. 2006;11(2):135–41. https://doi.org/10.1111/j.1085-9489.2006.00078.x.
Cornblath DR, Chaudhry V, Carter K, Lee D, Seysedadr M, Miernicki M, et al. Total neuropathy score: validation and reliability study. Neurology. 1999;53(8):1660–4. https://doi.org/10.1212/wnl.53.8.1660.
Schmidt SL, Oliveira RM, Rocha FR, Abreu-Villaca Y. Influences of handedness and gender on the Grooved Pegboard Test. Brain Cogn. 2000;44(3):445–54. https://doi.org/10.1006/brcg.1999.1204.
McCrary JM, Goldstein D, Sandler CX, Barry BK, Marthick M, Timmins HC, et al. Exercise-based rehabilitation for cancer survivors with chemotherapy-induced peripheral neuropathy. Support Care Cancer. 2019;27:3849–57. https://doi.org/10.1007/s00520-019-04680-w.
Sturnieks DL, Arnold R, Lord SR. Validity and reliability of the Swaymeter device for measuring postural sway.(Technical advance)(Report). BMC Geriatr. 2011;11:63.
McCrary JM, Goldstein D, Trinh T, Timmins HC, Li T, Menant J, et al. Balance deficits and functional disability in cancer survivors exposed to neurotoxic cancer treatments. J Natl Compr Cancer Netw. 2019;17(8):949–55. https://doi.org/10.6004/jnccn.2019.7290.
Simplified calculation of body-surface area. N Engl J Med. 1987;317(17):1098.
Wildiers H, Reiser M. Relative dose intensity of chemotherapy and its impact on outcomes in patients with early breast cancer or aggressive lymphoma. Crit Rev Oncol Hematol. 2011;77(3):221–40. https://doi.org/10.1016/j.critrevonc.2010.02.002.
Cancer Institute NSW C. eviQ cancer treatments. Australian Government 2020. https://www.eviq.org.au/. Accessed October 2020 2020.
Alberti K, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–5.
WHO WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 2000;894:i-xii, 1-253.
Park SB, Lin CSY, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC. Long-term neuropathy after oxaliplatin treatment: challenging the dictum of reversibility. Oncologist. 2011;16(5):708–16. https://doi.org/10.1634/theoncologist.2010-0248.
Timmins HC, Li T, Kiernan MC, Baron-Hay S, Marx G, Boyle F, et al. Taxane-induced peripheral neuropathy: differences in patient report and objective assessment. Support Care Cancer. 2020;28:4459–66. https://doi.org/10.1007/s00520-020-05299-y.
Statistics ABo. National Health Survey: first results, 2017-18., Canberra:. 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by Subject/4364.0.55.001~2017-18~Main Features~Overweight and obesity~90. Accessed 23/10/2020 2020.
Petrovchich I, Kober KM, Wagner L, Paul SM, Abrams G, Chesney MA, et al. Deleterious effects of higher body mass index on subjective and objective measures of chemotherapy-induced peripheral neuropathy in cancer survivors. J Pain Symptom Manag. 2019;58(2):252–63. https://doi.org/10.1016/j.jpainsymman.2019.04.029.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177–89. https://doi.org/10.1038/s41574-019-0310-7.
Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring). 2007;15(1):216–24. https://doi.org/10.1038/oby.2007.505.
Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL. Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999-2000 Through 2015-2016. Natl Health Stat Report. 2018;(122):1–16.
Winters-Stone KM, Horak F, Jacobs PG, Trubowitz P, Dieckmann NF, Stoyles S, et al. Falls, functioning, and disability among women with persistent symptoms of chemotherapy-induced peripheral neuropathy. J Clin Oncol. 2017;35(23):2604–12. https://doi.org/10.1200/jco.2016.71.3552.
Ghoreishi Z, Keshavarz S, Jafarabadi MA, Fathifar Z, Goodman KA, Esfahani A. Risk factors for paclitaxel-induced peripheral neuropathy in patients with breast cancer. BMC Cancer. 2018;18(1):958.
Frames CW, Soangra R, Lockhart TE, Lach J, Ha DS, Roberto KA, et al. Dynamical properties of postural control in obese community-dwelling older adults (†). Sensors (Basel). 2018;18(6):1692. https://doi.org/10.3390/s18061692.
Zimmer P, Trebing S, Timmers-Trebing U, Schenk A, Paust R, Bloch W, et al. Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: a randomized controlled trial. Support Care Cancer. 2018;26(2):615–24. https://doi.org/10.1007/s00520-017-3875-5.
Kleckner I, Kamen C, Gewandter J, Mohile N, Heckler C, Culakova E, et al. Effects of exercise during chemotherapy on chemotherapy-induced peripheral neuropathy: a multicenter, randomized controlled trial. Support Care Cancer. 2018;26(4):1019–28. https://doi.org/10.1007/s00520-017-4013-0.
Statistics AABo. Overweight and obesity in adults in Australia: a snapshot, 2007–08 2008. https://www.abs.gov.au/ausstats/abs@.nsf/Products/C789DF7995470E97CA25789C0023DBAA?opendocument. Accessed 6/11/2020.
Park SB, Kwok JB, Asher R, Lee CK, Beale P, Selle F, et al. Clinical and genetic predictors of paclitaxel neurotoxicity based on patient- versus clinician-reported incidence and severity of neurotoxicity in the ICON7 trial. Ann Oncol. 2017;28(11):2733–40. https://doi.org/10.1093/annonc/mdx491.
Song S, Min J, Suh S, Jung S, Hahn H, Im S-A, et al. Incidence of taxane-induced peripheral neuropathy receiving treatment and prescription patterns in patients with breast cancer. Support Care Cancer. 2017;25(7):2241–8. https://doi.org/10.1007/s00520-017-3631-x.
Rankinen T, Kim SY, Pérusse L, Després JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes. 1999;23(8):801–9. https://doi.org/10.1038/sj.ijo.0800929.
Bray GA, Perreault L. Obesity in adults: prevalence, screening, and evaluation. UpToDate; 2014.
Gérard S, Bréchemier D, Lefort A, Lozano S, Abellan Van Kan G, Filleron T, et al. Body composition and anti-neoplastic treatment in adult and older subjects - a systematic review. J Nutr Health Aging. 2016;20(8):878–88. https://doi.org/10.1007/s12603-015-0653-2.
Li J, Tang J, Li Y, Yu J, Zhang B, Yu C. Pharmacokinetic profile of paclitaxel in the plasma, lung, and diaphragm following intravenous or intrapleural administration in rats. Thorac Cancer. 2015;6(1):43–8. https://doi.org/10.1111/1759-7714.12139.
Ali R, Baracos VE, Sawyer MB, Bianchi L, Roberts S, Assenat E, et al. Lean body mass as an independent determinant of dose-limiting toxicity and neuropathy in patients with colon cancer treated with FOLFOX regimens. Cancer Med. 2016;5(4):607–16. https://doi.org/10.1002/cam4.621.
Park SB, Goldstein D, Krishnan AV, Lin CS, Friedlander ML, Cassidy J, et al. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J Clin. 2013;63(6):419–37. https://doi.org/10.3322/caac.21204.
Kus T, Aktas G, Kalender ME, Sevinc A, Kul S, Suner A, et al. Taxane-induced peripheral sensorial neuropathy in cancer patients is associated with duration of diabetes mellitus: a single-center retrospective study. Support Care Cancer. 2016;24(3):1175–9. https://doi.org/10.1007/s00520-015-2898-z.
Brown JC, Zhang S, Ou F-S, Venook AP, Niedzwiecki D, Lenz H-J, et al. Diabetes and clinical outcome in patients with metastatic colorectal cancer: CALGB 80405 (Alliance). JNCI Cancer Spectr. 2019;4(1). https://doi.org/10.1093/jncics/pkz078.
Callaghan BC, Xia R, Banerjee M, Rekeneire N, Harris TB, Newman AB, et al. Metabolic syndrome components are associated with symptomatic polyneuropathy independent of glycemic status.(Report). Diabetes Care. 2016;39(5):801. https://doi.org/10.2337/dc16-0081.
Klöting N, Blüher M. Adipocyte dysfunction, inflammation and metabolic syndrome. Rev Endocr Metab Disord. 2014;15(4):277–87. https://doi.org/10.1007/s11154-014-9301-0.
O'Brien PD, Hinder LM, Callaghan BC, Feldman EL. Neurological consequences of obesity. Lancet Neurol. 2017;16(6):465–77. https://doi.org/10.1016/S1474-4422(17)30084-4.
Funding
This study was supported by a Cancer Institute NSW Program Grant (14/TPG/1-05) and a National Health and Medical Research Council of Australia (NHMRC) Project Grant (#1080521). SBP is supported by a NHMRC Career Development Fellowship (#1148595). MCK is supported by a NHMRC Practitioner Fellowship (1156093) and by ForeFront, a large collaborative research group dedicated to the study of neurodegenerative diseases and funded by the National Health and Medical Research Council of Australia Program Grant (#1132524).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent and ethical approval
All studies included in this review complied with ethical standards and were conducted with informed consent.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 32 kb).
Rights and permissions
About this article
Cite this article
Timmins, H.C., Li, T., Goldstein, D. et al. The impact of obesity on neuropathy outcomes for paclitaxel- and oxaliplatin-treated cancer survivors. J Cancer Surviv 16, 223–232 (2022). https://doi.org/10.1007/s11764-021-01012-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-021-01012-y