Abstract
Objectives
This study aims to reduce mortality and morbidity by analyzing the factors associated with blunt chest trauma.
Methods
In this study, 1020 patients with blunt thoracic trauma were analyzed retrospectively. Major surgeries, complications, admission to intensive care unit, intubation, mortality, prolonged hospital stay were considered poor clinical outcomes. Independent variables were compared with clinical outcomes and analyzed.
Results
The mean age was 52.7 ± 19.1. Complications (p = 0.028) and mortality (p < 0.001) were higher in patients aged 65 years and older than those aged 65 years and younger. Severe chest wall injuries, hemopneumothorax, and pulmonary contusions were associated with poor clinical outcomes (OR = 2474, p = 0.001, OR = 2229, p < 0.001 and OR = 2229, p < 0.001, respectively). The variable most related to poor clinical outcomes was New Injury Severity Score (p < 0.001, OR = 8.37).
Conclusions
The most associated factor with poor clinical outcomes was injury severity. Prompt treatment of blunt chest trauma with timely chest tube thoracostomy or surgical treatment when necessary, optimal pain control, and chest physiotherapy will reduce mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumas have been a health problem since ancient times. However, they have become a growing public health issue with increasing motor vehicles and industrialization. The annual number of trauma-related deaths has recently reached 5.8 million worldwide [1]. Fifty percent of trauma patients have chest injuries, with a mortality rate of 25% [2].
Factors affecting prognosis and clinical outcomes of blunt thoracic trauma cases vary among studies. There is no definite consensus on the treatment of blunt thoracic trauma, and the treatment of such traumas is controversial.
This study aims to determine independent variables of morbidity and mortality, evaluate the role of surgical treatment, and improve clinical outcomes of patients with blunt chest injuries.
Materials and methods
The approval for this study was obtained from the Clinical Research Ethics Committee of Kahramanmaras Sutcu Imam University Faculty of Medicine with the decision number of 26.08.2020/21.
The study was conducted in three hospitals with level I trauma center qualifications: Adiyaman Training and Research Hospital, Kahramanmaras Necip Fazil City Hospital, and Kahramanmaras Sutcu Imam University Health Practices and Research Hospital. A detailed informed consent form was obtained from all patients included in the study.
The files of 1275 thoracic trauma patients admitted to thoracic surgery clinics October 2006–December 2019 were scanned. Penetrating thoracic traumas were excluded from the study. The data of 1020 patients were retrospectively evaluated. The data of patients were obtained from the hospital records. The diagnosis was based on chest computed tomography examinations reported by a radiologist.
The accident-related findings and demographic and personal characteristics of patients were considered independent variables. Patients were grouped as under 65 years old and 65 years old and over based on the World Health Organization classification [3]. The physical performance status of the patients was classified according to the American Society of Anesthesiologists (ASA) score [4].
Injury mechanisms were grouped as follows: motor vehicle accidents (1), falls (2), falls from height (3), and others (4). Chest wall injuries were grouped as follows: no chest wall injury (1), 1–4 rib fractures (2), and severe chest wall injuries (5 or more rib fractures/flail chest/sternal fractures) (3). Hemothorax, pneumothorax, and hemopneumothorax were defined as pleural injuries. Pulmonary contusion was defined by chest computed tomography. Pulmonary contusions were classified as follows: no pulmonary contusion (1), segmental (2), lobar (3), and multilobar contusions (4).
Each lesion was scored using the Abbreviated Injury Scale (AIS) [5]. The New Injury Severity Score (NISS), based on the sum of the squares of the AIS scores estimated for the three most severe injuries regardless of the body region, was calculated for each patient to determine the severity of trauma [6]. NISS was classified as 1–15 (1), 16–24 (2), and over 25 (3).
First-line treatment was a conservative treatment. A chest tube was inserted in pleural complications, affecting respiratory functions. Major surgery (thoracotomy, video-assisted thoracic surgery (VATS), surgical stabilization of the ribs or sternum) was performed in cases where conservative treatment or chest tube was insufficient.
Complications, Intensive Care Unit (ICU) admission, intubation requirement, and mortality were determined. In addition, the length of hospital stay was categorized as 6 days and shorter, and 7 days and longer based on the median value.
Patients meeting at least one of the following criteria were considered those with poor prognosis: major surgery, complications, intensive care admission, intubation, mortality, and prolonged length of hospital stay.
Statistical analysis
Statistical analyses were performed using SPSS version 22.0 for Windows (SPSS, Inc.; Chicago, USA) software package. In descriptive statistics, numerical variables are presented as mean ± standard deviation, median, and minimum–maximum values, while categorical variables are presented as number (n) and percentage (%). The Chi-square test or Fisher’s exact test compared categorical variables. Post hoc tests were performed when necessary. The correlation of independent variables obtained by pairwise comparisons with poor prognosis criteria was evaluated by logistic regression analysis. ‘The enter method’ was used for logistic regression analysis. The Hosmer–Lemeshow test was used for goodness of fit for logistic regression models. The level of statistical significance was set at a p value less than 0.05 (p < 0.05), with a confidence interval of 95%.
Results
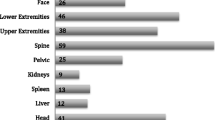
This study included 1020 patients with blunt thoracic trauma, of 770 (75.5%) males and 250 (24.5%) of whom were female. Table 1 shows the relationship between poor clinical outcomes and patient characteristics and injury types. The patients were between 12 and 103 years of age, with a mean age of 52.7 ± 19.1 years. ASA score (p < 0.001) and comorbidities (p < 0.001) were significantly higher at 65 years and above. The most common comorbidity was hypertension (n = 105, 10.3%), and the most common mechanism of injury was motor vehicle accidents. Motor vehicle accidents were more common in patients younger than 65 years, and falls were more frequent in patients 65 years and older (p < 0.001). Associated organ injuries (p = 0.004) and pulmonary contusion (p < 0.001) were common injuries in patients under 65 years, whereas rib fractures (p < 0.001) were more common in older patients. The NISS values of patients ranged from 1 to 66, with a mean NISS value of 14.84 ± 11.64. The most prevalent associated other organ injuries were upper extremity injuries (n = 100, 9.8%).
While medical treatment was sufficient in 706 (69.2%) patients, 278 (27.3%) patients required chest tube insertion, and 36 (3.5%) patients required major surgery. Figure 1 shows the patient flowchart. Major surgery included VATS in 15 (1.5%) patients, surgical chest wall stabilization in 12 (1.2%) patients, thoracotomy in 9 (0.9%) patients, and sternotomy in 3 (0.3%) patients. Hemopneumothorax (p = 0.023), severe chest wall injuries (p = 0.002), associated other organ injuries (p = 0.010), and NISS 25 or above (p < 0.001) were related to the need for major surgery. Emergency operation was performed in six (0.6%) patients. Five patients were operated on for massive hemothorax and one for cardiac injury. One patient with a major vessel injury died from massive hemothorax.
Of the 846 rib fracture patients, 274 (32.4%) had isolated rib fractures. Conservative treatment was sufficient in 267 (97.4%) patients with isolated rib fractures. Poor clinical outcomes were significantly higher in patients with additional injuries to rib fractures than in patients with isolated rib fractures (p < 0.001). Ten (0.98%) patients had a flail chest. While medical treatment was sufficient for two patients with flail chest, eight patients required chest tube insertion, seven (70%) were admitted to the intensive care unit (p = 0.002), and four (40%) were intubated (p < 0.001). One of the flail chest patients died, with a mortality rate of 10%. This patient also had a severe intracranial injury. Flail chest was not associated with mortality. Hemopneumothorax (p = 0.024), pulmonary contusion (p = 0.003), associated organ injury (p < 0.001), and prolonged hospital stay (p = 0.001) were more common in flail chest.
One hundred five (10.3%) patients required admission to the intensive care unit, and 26 (2.6%) patients were intubated. Fourteen patients, 13 males (92.8%), were emergency intubated. The most common reason for emergency intubation was cranial injuries in six patients (42.8%). Six of these patients (42.8%) died. ICU admission and intubation were significantly related to severe chest wall injuries (p < 0.001), hemopneumothorax (p < 0.001), pulmonary contusions involving multiple lobes (p < 0.001), and bilateral injuries (p < 0.001).
One hundred and thirteen (11.1%) patients developed complications. Most common complications were atelectasis (n = 46, 4.5%), and pneumonia (n = 18, 1.8%). Advanced ages (p = 0.028), bilateral injuries (p < 0.001), high ASA values (p < 0.001), comorbidities (p < 0.001), severe chest wall injuries (p < 0.001), hemopneumothorax (p < 0.001), pulmonary contusions involving multiple lobes (p < 0.001), associated injuries (p < 0.001), and high NISS values (p < 0.001) were associated with high complication rates.
Seventeen (1.66%) patients died. The most common cause of death was cranial injuries in eight (47%) patients. Comorbidities (p < 0.001), 65 years and above (p < 0.001), bilateral injuries (p < 0.001), severe chest wall injuries (p < 0.001), hemopneumothorax (p = 0.001), pulmonary contusions involving multiple lobes (p = 0.010), high ASA scores (p = 0.005), associated injuries (p = 0.002), and high NISS values (p < 0.001) were associated with mortality.
The length of hospital stay ranged from 1 to 29 days, with a mean value of 7.04 days (± 4.57) and a median value of 6 days. Motor vehicle accidents (p < 0.001), high ASA scores (p < 0.001), comorbidities (p = 0.040), bilateral injuries (p < 0.001), severe chest wall injuries (p < 0.001), hemopneumothorax (p < 0.001), pulmonary contusions involving multiple lobes (p = 0.005), associated injuries (p < 0.001), and high NISS values (p < 0.001) were related to mortality.
Logistic regression analysis showed that the independent variables related to poor prognosis were NISS, hemopneumothorax, associated organ injuries, severe chest wall injuries, ASA score, and pulmonary contusions (see Table 2).
Discussion
Due to the increase in the number of motor vehicles, blunt thoracic traumas have also increased [7]. As in previous studies, the most common trauma mechanism was motor vehicle accidents [8, 9].
As a result of this study, the factor most related to poor clinical outcomes was trauma severity, similar to some previous studies [10, 11]. Osler described NISS in 1997 based on the sum of the three most severe injuries regardless of the body area [6]. Even if the injuries are in a single body region, the higher the injury score, the higher the probability of mortality. [10]. Since most of the injuries in our patients were in the chest area, NISS could best represent the severity of injuries.
Conservative treatment is the most common method in blunt thoracic trauma [12, 13]. Observation is sufficient for patients with small hemothorax or pneumothorax (≤ 2 cm) without underlying respiratory disease or not requiring positive pressure ventilation [13]. Conservative treatment should include adequate analgesia, appropriate fluid therapy, chest physiotherapy, clearing of bronchial secretions, and antibiotic therapy if necessary. Hemopneumothorax is associated with a poor prognosis. A chest tube should be placed in a hemothorax or pneumothorax, causing respiratory distress [12]. According to previous studies, conservative treatment with chest tube placement, if necessary, is sufficient in the majority of patients with blunt chest trauma, and less than 5% of patients require major surgery. [2, 8]. In our study, the rate of major surgery was 3.5%, which is consistent with these rates. An emergency thoracotomy may be necessary to treat massive hemothorax or tension pneumothorax [9, 14]. Our emergency thoracotomy rate was 0.6%. VATS, a minimally invasive technique, can be used in patients with stable hemodynamic conditions for clotted hemothorax, persistent air leak, diaphragmatic rupture, and empyema [15].
The most common injury type in many studies was rib fracture [8, 16]. Some authors reported that the prognosis worsens as the number of broken ribs increases [9, 17, 18]. On the other hand, some authors reported that not rib fractures but accompanying pleural or parenchymal injuries cause poor prognosis [19, 20]. Our results also support this view.
The classical treatment of rib fractures and flail chest were conservative methods. However, in recent years, the treatment of rib fractures has become controversial with the publications of results on surgical fixation of fractured ribs. Athanassaidi et al. argued that hypoxia is caused not by rib fractures but by contusion, hematoma, alveolar collapse, and inadequate tissue oxygen delivery; therefore, surgical stabilization of the ribs would not be beneficial. Moreover, operative stabilization has disadvantages such as the risk of general anesthesia in severely traumatized patients, the difficulty and time of stabilization techniques, tissue damage due to surgical dissection, and increased infections by implanted foreign bodies [11]. Tanaka, Granetzny, and Marasco reported that surgical fixation of the chest wall in patients with flail chest improved respiratory functions, shortened the duration of mechanical ventilation, and length of stay in the ICU [21,22,23]. In 2016, Farquhar found that conservatively managed patients had significantly lower ICU and hospital stays and a lower pneumonia rate than patients who underwent surgical stabilization. He also found ICU and hospital stay days and pneumonia rates lower than Marasko’s results and concluded that surgical fixation had no benefit in flail chest patients [24]. Sirmali and Liman suggested that surgical fixation is not required for all patients but should be performed for fractured ribs in patients who underwent surgery for other reasons [14, 17]. More studies have been published on the benefits of surgical fixation in recent years [25, 26]. However, Granetzny reported postoperative complications in 35%, Wijffels in 30%; and Wijffels used invasive techniques to treat some complications [22, 25]. In a practice management guideline from the Eastern Association for the Surgery of Trauma, 2017 update, in adult patients with flail chest, rib operative reduction and internal rib fixation have been conditionally recommended to reduce mortality, reduce the incidence of pneumonia, reduce the need for tracheostomy, shorten the duration of mechanical ventilation, shorten the length of stay in the ICU, and shorten the length of stay in the hospital [27]. Currently, there is no consensus on the treatment of rib fractures and flail chests. According to our results, we do not recommend surgical stabilization in isolated rib fractures since the prognosis of isolated rib fractures is good. However, we think that surgical stabilization may be beneficial in patients with flail chest and severe chest wall injuries complicated by accompanying injuries such as massive hemopneumothorax or causing respiratory dysfunction that cannot be corrected with conservative treatment.
Pulmonary contusion is defined as lung parenchymal injury resulting in edema and interstitial hemorrhage. Its rate in blunt thoracic traumas is 17–75% [28]. Our rate is also between these limits (24.4%). Severe pulmonary contusion is an independent variable associated with poor clinical outcomes, which can cause respiratory complications such as pneumonia, acute respiratory distress syndrome (ARDS), and prolonged intubation. In addition, it is an independent predictive factor for mortality [20, 28]. However, since the injury was at the alveolar level, pulmonary contusions were not associated with the need for major surgery [26].
Patients with chest trauma often present with injuries to multiple body regions requiring more than one medical department [29]. The most crucial additional organ injuries are craniocervical injuries. Craniocervical injuries are associated with increased mortality and morbidity in blunt thoracic trauma [7, 29]. It is claimed that blunt thoracic traumas decrease venous return and increase cerebral venous congestion and the severity of the intracranial injury [16]. Also, in our study, the most common cause of death was head trauma. Injuries that prevent mobility such as vertebral, pelvic, or lower extremity injuries were associated with complications such as atelectasis and pneumonia.
Mortality rates vary between 1 and 22% in the literature [16, 17]. This high range may be due to different inclusion criteria. The factors most associated with mortality are injury severity, associated organ injuries, and pleural and pulmonary parenchymal injuries leading to respiratory failure [1, 11].
There is no consensus on the effects of advanced age on mortality and morbidity in patients with blunt thoracic trauma. While some authors reported that advanced age increases mortality and morbidity [7, 14], some authors reported that age does not affect mortality [18, 20]. In our series, age was not associated with poor clinical outcomes according to logistic regression analysis. However, complications and mortality were high in advanced ages in pairwise comparisons. Elderly patients suffer more minor injuries such as falls or home accidents. On the other hand, in elderly patients, ribs may be fractured with less force due to muscle wasting and osteoporosis. In addition, mild respiratory problems cause worse clinical outcomes due to comorbidities [13, 18].
Limitations
The limitations of this study are the probability of data loss due to its retrospective nature and the inclusion of hospitalized patients. Its strengths are that it compasses three different centers and an extensive series.
Conclusion
High NISS values are a good indicator of trauma severity and prognosis. Early and accurate scoring of blunt thoracic trauma is essential for identifying patients at risk, deciding on treatment modalities, determining priorities, and predicting complications.
References
Beshay M, Mertzlufft F, Kottkamp HW, Reymond M, Schmid RA, Branscheid D, et al. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: a mono-centre study. World J Emerg Surg. 2020;15:45.
Perna V, Morera R. Prognostic factors in chest traumas: a prospective study of 500 patients. Cirugía Española (English Edition). 2010;87(3):165–70.
World Health Organization. Men, ageing and health: achieving health across the life span (No. WHO/NMH/NPH/01.2). World Health Organization; 2001.
ASA House of Delegates. ASA physical status classification system. 2014. https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system
Gennarelli TA. Abbreviated ınjury scale 1985 revision. American Association for Automotive Medicine; 1985.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma Acute Care Surg. 1997;43(6):922–6.
Küçük MP, Küçük AO, Aksoy İ, Aydın D, Ülger F. Prognostic evaluation of cases with thoracic trauma admitted to the intensive care unit: 10-year clinical outcomes. Ulus Travma Acil Cerrahi Derg. 2019;25(1):46–54.
Gupta AK, Sharma AK, Suthar NK, Girija HR, Verma V, Jindal SP. Epidemiological pattern of blunt trauma chest in Western India. Apollo Med. 2020;17(2):66.
Demirhan R, Onan B, Oz K, Halezeroglu S. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg. 2009;9(3):450–3.
Rapsang AG, Shyam DC. Scoring systems of severity in patients with multiple trauma. Cir Esp. 2015;93(4):213–21.
Athanassiadi K, Theakos N, Kalantzi N, Gerazounis M. Prognostic factors in flail-chest patients. Eur J Cardiothorac Surg. 2010;38(4):466–71.
Kostov K. Diagnosis and treatment of thoracic injuries and traumatic hemopneumothorax. J IMAB. 2021;27(1):3611–4.
Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients—still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25:42.
Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici U, Kaya S, Taştepe I. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24(1):133–8.
Ludwig C, Koryllos A. Management of chest trauma. J Thorac Dis. 2017;9(Suppl 3):172.
Emircan S, Ozgüç H, Akköse Aydın S, Ozdemir F, Köksal O, Bulut M. Factors affecting mortality in patients with thorax trauma. Ulus Travma Acil Cerrahi Derg. 2011;17(4):329–33.
Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003;23(3):374–8.
Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43(1):8–17.
Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49(3):496–504.
Huber S, Biberthaler P, Delhey P, Trentzsch H, Winter H, van Griensven M, Trauma Register DGU, et al. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU®). Scand J Trauma Resusc Emerg Med. 2014;3(22):52.
Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727–32.
Granetzny A, El-Aal MA, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4(6):583–7.
Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, Lee G, Bailey M, Fitzgerald M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924–32.
Farquhar J, Almahrabi Y, Slobogean G, Slobogean B, Garraway N, Simons RK, et al. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg. 2016;59(5):299.
Wijffels MME, Hagenaars T, Latifi D, Van Lieshout EMM, Verhofstad MHJ. Early results after operatively versus non-operatively treated flail chest: a retrospective study focusing on outcome and complications. Eur J Trauma Emerg Surg. 2020;46(3):539–47.
Fokin AA, Wycech J, Weisz R, Puente I. Outcome analysis of surgical stabilization of rib fractures in trauma patients. J Orthop Trauma. 2019;33(1):3–8.
Kasotakis G, Hasenboehler EA, Streib EW, Patel N, Patel MB, Alarcon L, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82(3):618–26.
Bader A, Rahman U, Morris M, McCormack JE, Huang EC, Zawin M, et al. Pulmonary contusions in the elderly after blunt trauma: incidence and outcomes. J Surg Res. 2018;230:110–6.
Lin FC, Tsai SC, Li RY, Chen HC, Tung YW, Chou MC. Factors associated with intensive care unit admission in patients with traumatic thoracic injury. J Int Med Res. 2013;41(4):1310–7.
Funding
There is no financial or material supporter for this study.
Author information
Authors and Affiliations
Contributions
There is no other contributor other than the author on the list.
Corresponding author
Ethics declarations
Conflict of interest
The author (Mehmet Degirmenci) has no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Degirmenci, M. Factors related to clinical outcomes in blunt thoracic injuries. Gen Thorac Cardiovasc Surg 70, 804–811 (2022). https://doi.org/10.1007/s11748-022-01796-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01796-5