Abstract
Purpose
Our understanding of the growing geriatric population’s risk factors for outcomes after traumatic injury remains incomplete. This study aims to compare outcomes of severe isolated blunt chest trauma between young and geriatric patients and assess predictors of mortality.
Methods
The ACS-TQIP 2017–2020 database was used to identify patients with severe isolated blunt chest trauma. Patients having extra-thoracic injuries, no signs of life upon presentation to the emergency department (ED), prehospital cardiac arrest, or who were transferred to or from other hospitals were excluded. The primary outcome was in-hospital mortality. Univariate and multivariable regression analyses were performed to assess independent predictors of mortality.
Results
A total of 189,660 patients were included in the study, with a median age of 58 years; 37.5% were aged 65 or older, and 1.9% died by discharge. Patients aged 65 and older had significantly higher mortality (3.4% vs. 1.0%, p < 0.001) and overall complications (7.0% vs. 4.7%, p < 0.001) compared to younger patients. Age ≥ 65 was independently associated with mortality (OR: 5.45, 95%CI: 4.96–5.98, p < 0.001), prolonged hospitalization, and complications. In the geriatric group, age > 75 was an independent predictor of mortality compared to ages 65–75 (OR: 2.62, 95%CI: 2.37–2.89, p < 0.001). Geriatric patients with an MVC, presenting with a GCS ≤ 8, and having an SBP < 90 had the highest mortality of 56.9%.
Conclusion
The geriatric trauma patient with isolated severe blunt chest injury has significantly higher mortality and morbidity compared to younger patients and warrants special consideration of multiple factors that affect outcomes. Individual predictors of mortality carry a greater impact on mortality in geriatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The United States is amid unprecedented demographic shifts fueled by a large growth among the older adult population [1]. The geriatric population accounts for 43% of hospital care days and over a third of hospital discharges [2]. Blunt chest trauma represents more than 10% of all trauma presentations to the emergency department [3], and in patients over the age of 60, chest trauma is the second most injured anatomical region, with head injuries being the most common [4].
Blunt chest trauma carries significant morbidity and mortality, with overall mortality ranging from 4 to 20% [3, 5, 6]. In patients above the age of 65, mortality rates double after blunt chest trauma compared to younger patients [6, 7]. Furthermore, older adults with blunt chest trauma who initially present with non-immediate life-threatening injuries are at a much higher risk of delayed deterioration [8, 9].
Prior reviews of the literature have studied predictors of poor outcomes in older adults with blunt chest trauma [7, 10, 11]. However, most studies focus on rib fractures after blunt chest trauma and no studies utilize nationwide trauma databases to assess predictors of poor outcomes. In geriatric patients, early identification of risk factors for deterioration, prolonged hospitalization, and overall mortality is essential to guide and escalate patient care early on, improve patient and family communication, and plan discharge disposition.
The aim of this study is to assess predictors of poor outcomes, mainly mortality, hospital length of stay, and complications, after isolated severe blunt chest trauma in geriatric patients, and compare them to the younger cohort.
Methods
Patient selection
The American College of Surgeons (ACS) Trauma Quality Improvement Program (TQIP) 2017–2020 database was used to identify patients who had severe isolated blunt chest trauma. Severe chest trauma was defined as an abbreviated injury severity (AIS) score ≥ 3 and ≤ 5. Patients with concomitant extra-thoracic injuries with an AIS score > 2, injury severity score (ISS) > 33 or < 9, no signs of life (SOL) upon presentation to the emergency department (ED), prehospital cardiac arrest, or who were transferred to or from other hospitals were excluded. Furthermore, patients with missing data on sex, race, comorbidities, interhospital transfer status, and hospital data were excluded. International Classification of Diseases 10th Revision procedure codes were used to identify patients who underwent rib fixation (Supplementary Table 1).
Outcomes
The primary outcome of this study was in-hospital mortality. Secondary outcomes were total hospital length of stay (LOS), intensive care unit (ICU) LOS, and in-hospital complications. A composite outcome of in-hospital complications was defined as the presence of any of the complications. Prolonged hospital LOS, ICU LOS, and ventilator days were categorized into a binary outcome using the median duration of each as the cutoff. Multiple rib fractures were defined as ≥ 3 ribs fractured.
Statistical analysis
For categorical variables, results were reported as n (%), and the Chi-Square test was performed for hypothesis testing. For continuous variables, results were reported as median (IQR), and the Mann-Whitney U test was performed. Univariate analyses were performed to assess significant differences in demographics and injury characteristics between those who survived and those who did not. Variables that showed absolute values of standardized differences greater than 0.10, in addition to those that were clinically relevant, were included in the multilevel mixed-effects logistic regression analysis to assess significant predictors of mortality. Clustering by hospital was adjusted for in the model. P < 0.05 was set as significant.
All statistical analyses were performed using STATA version 17.0. The study was exempted from institutional review board approval as the database used has no patient identifiers.
Results
Patient characteristics
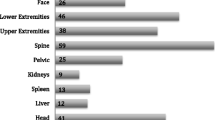
A total of 189,660 patients were included in the study, of whom 3,576 (1.9%) died by discharge. The median age of the study sample was 58 years, 37.5% were above or equal to the age of 65, 33.3% were females, and 31.7% had a BMI ≥ 30. Furthermore, 8.3% of the patients had COPD, 9.6% were on anticoagulant therapy, and 6.9% were functionally dependent prior to their injury (Table 1). As for injury characteristics, 40.3% of patients had a fall, and 32.3% had a motor vehicle crash (MVC). The majority of patients, more than 80%, had multiple rib fractures, and 14.4% had pulmonary contusion. Only a minor percentage of the patient sample had a pulmonary laceration and a flail chest (0.8% and 5.4%, respectively). Vitals measured by emergency medical services (EMS) showed an SBP < 90 mmHg in 3.1% of patients and a GCS ≤ 8 in 1.7%. Upon arrival to the ED, 2.1% of patients had an SBP < 90 mmHg, 1.3% had a GCS ≤ 8, and the median ISS was 15. The primary injury mechanism in patients aged 65 and older was falls, accounting for 64.2% of cases, followed by MVCs at 32.3%. Conversely, in patients younger than 65, MVCs were the leading cause of injury at 63.3%, with falls being the second most common at 26.0% (p < 0.001) (Table 2).
Outcomes
The overall mortality of the study sample was 1.9%. Compared to younger patients, those older than 65 years had a 3-fold increase in in-hospital mortality (3.4% vs. 1.0%, p < 0.001) and significantly higher in-hospital complications (7.0% vs. 4.7%, p < 0.001). As for the individual complications, patients above the age of 65 years had higher percentages of AKI (0.9% vs. 0.4%, p < 0.001), cardiac arrest requiring cardiopulmonary resuscitation (1.0% vs. 0.6%, p < 0.001), myocardial infarction (0.3% vs. 0.1%, p < 0.001), stroke/CVA (0.3% vs. 0.1%, p < 0.001), unplanned intubation (2.3% vs. 1.4%, p < 0.001), and unplanned admission to the ICU (3.2% vs. 1.9%, p < 0.001), compared to their younger counterparts (Table 3).
When adjusted for confounding variables, age ≥65 years was independently associated with mortality (OR: 5.45, 95% CI: 4.96–5.98, p < 0.001), prolonged hospitalization ≥4 days (OR: 1.62, 95% CI: 1.58–1.66, p < 0.001), prolonged ICU LOS ≥3 days (OR 1.22, 95% CI: 1.17–1.27 p < 0.001), prolonged ventilation days ≥3 days (OR: 1.29, 95% CI: 1.18–1.40, p < 0.001), and composite outcome in-hospital complications (OR: 1.79, 95% CI: 1.70–1.88, p < 0.001). For specific complications, age ≥65 years was independently associated with AKI, cardiac arrest requiring CPR, sepsis, catheter-associated urinary tract infection, central line-associated bloodstream infection, ventilator-associated pneumonia, pressure ulcer, deep vein thrombosis (DVT), pulmonary embolism, stroke/cerebrovascular accident (CVA), myocardial infarction, unplanned intubation, and unplanned admission to the ICU (Table 4).
As for injury characteristics, patients who experienced an MVC had a twofold increase in the mortality rate compared to those who sustained injuries from a fall (4.7% vs. 2.7%, p < 0.001). Furthermore, mortality was significantly higher in patients with pulmonary laceration (13.2% vs. 3.3%, p < 0.001), flail chest (8.2% vs. 3.1%, p < 0.001), and pulmonary contusion (6.1% vs. 3.0%, p < 0.001) compared to their counterparts. As for vitals upon presentation to the ED, mortality was significantly higher in those with SBP < 90 mmHg (20.2% vs. 3.0%, p < 0.001), with 41.4% of patients with a GCS upon presentation ≤ 8 not surviving till discharge (Supplementary Table 2).
Independent predictors of mortality
Multilevel mixed-effects logistic regression analyses were used to identify independent predictors of mortality in patients < 65 and ≥ 65 years old. In both patient cohorts, male sex, COPD, CKD, and anticoagulant therapy were characteristics independently associated with mortality. Furthermore, ED GCS ≤ 8, ED SBP < 90, pulmonary laceration, flail chest, and ISS ≥ 25 were also independent predictors of mortality. In the ≥ 65 years old cohort, age > 75 was independently associated with mortality compared to those between the ages of 65 and 75 (OR: 2.62, 95% CI: 2.37–2.89, p < 0.001). Interestingly, in the younger cohort below the age of 65, MVC as a mechanism of injury was protective against mortality compared to fall as a reference (OR: 0.85, 95% CI: 0.72–0.99, p = 0.034). This is in contrast to patients ≥ 65 years old where MVC was predictive of mortality compared to falls (OR: 1.39, 95% CI: 1.26–1.54, p < 0.001). This is mainly attributed to the ground-level falls seen in the elderly compared to high-energy falls in younger cohorts from an increased height. In both young and older cohorts, rib fixation was protective against mortality (OR 0.53, 95% CI: 0.36–0.79, p = 0.002) and (OR: 0.48, 95% CI: 0.34–0.67, p < 0.001), respectively [Table 5 (A) and (B)].
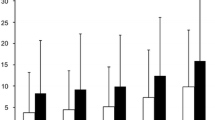
Figures 1 and 2 describe mortality rates based on the mechanism of injury, GCS, and SBP upon presentation to the ED in patients ≥ 65 and < 65 years old, respectively. In summary, geriatric patients had significantly higher mortality overall and in each stratification category compared to the younger cohort. In the geriatric group, patients who presented with a fall, with GCS > 8, and SBP ≥ 90 mmHg had the lowest mortality rate of 2.3%. In contrast, those who presented with MVC, GCS ≤ 8 and SBP < 90 mmHg had a mortality rate of 56.9%. In patients < 65 years, those who presented with a fall, with GCS > 8, and SBP ≥ 90 mmHg had a mortality of 0.6%, compared to a 33.7% mortality in MVC, GCS ≤ 8 and SBP < 90 mmHg group.
Supplementary Fig. 1 stratifies the geriatric cohort based on age 65–75 and > 75, in addition to vitals upon arrival. Patients aged 65–75 with GCS > 8 upon arrival and SBP ≥ 90 mmHg had a mortality rate of 1.8%. Those who were > 75 years old with GCS < 8 upon arrival and SBP < 90 mmHg had a 68.1% mortality rate.
Discussion
In this study, we have utilized a nationwide trauma database to assess independent predictors of mortality in geriatric patients with isolated severe blunt chest trauma.
A meta-analysis found age ≥ 65, presence of pre-existing comorbidities, pneumonia, and number of rib fractures as independent predictors of mortality in patients with blunt chest trauma [6]. In geriatric blunt chest trauma patients, a higher ISS and mechanical ventilation have been shown as additional risk factors for mortality [12]. There is a debate in the literature on the effect of the number of rib fractures on mortality. Some studies show that the number of rib fractures is directly associated with a higher risk of pulmonary complications [10, 11], ICU admission, mortality, and hospital length of stay [7, 13,14,15]. However, many other studies have found no association [16,17,18,19]. These variabilities have been attributed to the high variability among these studies [6]. Interestingly, our study did not show an association between multiple rib fractures and mortality in the multivariable regression model. This might be due to the colinearity between rib fractures and other chest injuries like pulmonary contusion. Additionally, the highest number of rib fractures in the database that is recorded is as a category of ≥ 3 fractures, with no further granularity in higher numbers.
In our study, we identified additional patient characteristics, comorbidities, and vital signs upon presentation to the ED as significant risk factors for poor outcomes in geriatric patients with blunt chest trauma. Patients above the age of 75, COPD patients, and those who have CKD have more than twice the odds of mortality compared to those between the ages of 65 and 75, and patients without these comorbidities. Furthermore, injury characteristics, including MVC, flail chest, pulmonary laceration, and contusion, independently increase the odds of mortality.
A recent expert practice review reported that guidelines focusing on blunt chest trauma in older adults are based on limited evidence. Furthermore, practice patterns vary among centers with a lack of consensus guidelines on how to manage geriatric trauma patients with blunt injuries to the chest [20]. While the predictors of poor outcomes we described are not modifiable, they are potentially useful in the early identification of high-risk patients to guide and escalate care early on, improve patient and family communication, and plan discharge disposition.
While it was surprising that the presence of multiple rib fractures was not a significant predictor of mortality in our regression model, we expect some degree of collinearity between multiple rib fractures and the other injury characteristics in the model, which could have made this variable insignificant. Nevertheless, we kept it in the model as a clinically relevant variable to adjust for when predicting mortality. Furthermore, due to the lack of clinical granularity in the ACS-TQIP database, we cannot determine the exact number of fractured ribs beyond “3 or more” or “unspecified multiple rib fractures.” As a result, it is possible that the mortality rates for patients with a higher number of rib fractures, such as six or more, which are significantly associated with higher mortality, might be obscured by the outcomes of those with three to four rib fractures, which are associated with less severe outcomes.
Our study has limitations. The use of a retrospective database from the United States creates a potential selection bias, where our results might be different in healthcare systems in other countries. The ACS-TQIP database does not record long-term outcomes, limiting our study to outcomes until discharge. We are unable to control for errors in data entry or coding within the database, the presence of which may introduce unknown bias into our study. Likewise, we are unable to control for regional or other systems-based differences in care that may skew our results. Furthermore, the ACS-TQIP database does not have frailty scores, which limits our analyses given the growing literature that suggests age is an inadequate measure of frailty alone. Lastly, the database lacks information on the type of anesthesia used, which limits our regression models as we are unable to adjust for this well-known risk factor.
Conclusions
Geriatric patients with isolated severe blunt chest trauma carry significantly higher mortality and morbidity compared to their younger counterparts. Individual predictors of mortality independently carry a higher impact on mortality in geriatric patients compared to younger ones. Furthermore, geriatric blunt chest trauma patients above the age of 65 should not be viewed as a single homogeneous group, as age over 75 is an independent predictor of mortality compared to those aged 65 to 75 years.
Data availability
No datasets were generated or analysed during the current study.
References
Halaweish I, Alam HB. Changing demographics of the American population. Surg Clin North Am. 2015;95(1):1–10.
Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Rep. 2010;29:1–20. 4.
Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37(6):975.
Network TTAaR. Major Trauma in Older People. 2017.
Quaday KA. Morbidity and mortality of rib fracture. J Trauma. 1995;39(3):617.
Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43(1):8–17.
Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–6. discussion 6–7.
Alexander JQ, Gutierrez CJ, Mariano MC, Vander Laan T, Gaspard DJ, Carpenter CL, Stain SC. Blunt chest trauma in the elderly patient: how cardiopulmonary disease affects outcome. Am Surg. 2000;66(9):855–7.
Shorr RM, Rodriguez A, Indeck MC, Crittenden MD, Hartunian S, Cowley RA. Blunt chest trauma in the elderly. J Trauma. 1989;29(2):234–7.
Vana PG, Mayberry J, Luchette FA. Management and complications of Rib fractures in older adults. Curr Geriatr Rep. 2016;5(1):25–30.
Aschkenasy MT, Rothenhaus TC. Trauma and falls in the elderly. Emerg Med Clin North Am. 2006;24(2):413–32. vii.
Sawa J, Green RS, Thoma B, Erdogan M, Davis PJ. Risk factors for adverse outcomes in older adults with blunt chest trauma: a systematic review. Cjem. 2018;20(4):614–22.
Shulzhenko NO, Zens TJ, Beems MV, Jung HS, O’Rourke AP, Liepert AE, et al. Number of rib fractures thresholds independently predict worse outcomes in older patients with blunt trauma. Surgery. 2017;161(4):1083–9.
Stawicki SP, Grossman MD, Hoey BA, Miller DL, Reed JF 3. Rib fractures in the elderly: a marker of injury severity. J Am Geriatr Soc. 2004;52(5):805–8.
Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, Gamelli RL. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138(4):717–23. discussion 23– 5.
Whitson BA, McGonigal MD, Anderson CP, Dries DJ. Increasing numbers of rib fractures do not worsen outcome: an analysis of the national trauma data bank. Am Surg. 2013;79(2):140–50.
Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196(4):549–55.
Testerman GM. Adverse outcomes in younger rib fracture patients. South Med J. 2006;99(4):335.
Elmistekawy EM, Hammad AA. Isolated rib fractures in geriatric patients. Ann Thorac Med. 2007;2(4):166–8.
Birse F, Williams H, Shipway D, Carlton E. Blunt chest trauma in the elderly: an expert practice review. Emerg Med J. 2020;37(2):73–8.
Acknowledgements
Not applicable.
Funding
This work was not funded or financially supported.
Author information
Authors and Affiliations
Contributions
V.S.P., J.O.H, H.M.K., M.P.D., I.C.N., M.A., W.R., and E.L. designed the study. V.S.P., E.L., W.R., M.A., I.C.N., S.A., A.H.H., K.A.G., and J.O.H. analyzed and interpreted the data. V.S.P. and J.O.H. wrote the manuscript. All the authors read, reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented at the 19th Annual Academic Surgical Congress, Washington, DC February 6-8, 2024.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Panossian, V.S., Lagazzi, E., Rafaqat, W. et al. Outcomes of severe isolated blunt chest trauma in young and geriatric patients. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02611-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02611-x