Abstract
Granulocyte colony stimulating factor (G-CSF)-producing lung cancer occasionally induces severe inflammation with an abnormally high white blood cell count. Herein, we report a 49-year-old man who suffered from resectable G-CSF-producing non-small cell lung cancer with continuous fever and severe anemia. Red blood cell transfusion was necessary for the anemia of inflammation. The patient underwent complete surgical tumor resection. The histopathological diagnosis was a pleomorphic carcinoma at pathological stage IIB. This is apparently the first successful case of surgical resection of G-CSF-producing lung cancer in a patient with severe anemia and uncontrollable fever.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancers with severe leukocytosis without any infection are occasionally encountered. One of these cancers is granulocyte colony stimulating factor (G-CSF)-producing lung cancer [1]. Patients with G-CSF-producing lung cancer occasionally have severe inflammation and continuous fever. However, there have been no reports of patients who suffer from severe anemia of inflammation and who are receiving red blood cell transfusion.
Case
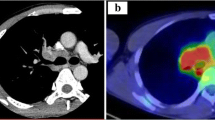
A 49-year-old man presented with fever and a small amount of bloody sputum for 2 months. Chest computed tomography (CT) showed a 79 × 55 mm tumor in the right upper lobe, which was suspected to invade the chest wall (Fig. 1a). Fluorodeoxyglucose positron emission tomography/CT demonstrated uptake of the tumor, subcarinal lymph node, and right hilar lymph node. There was no evidence of distant metastasis even on brain magnetic resonance imaging. Transbronchial lung biopsy indicated non-small cell lung carcinoma without epidermal growth factor receptor mutation or echinoderm microtubule-associated protein-like 4-anaplastic lymphoma kinase fusion gene rearrangement. The tumor was staged as clinical T3N2M0 stage IIIA (TNM classification 7th edition).
a Chest computed tomography showed a tumor in the right upper lobe having a maximum size of 79 mm, with suspected chest wall invasion. b Hematoxylin-eosin staining demonstrated pleomorphic tumor cells, including giant cells that were arranged randomly with massive necrosis (low power magnification). c Immunohistochemical staining demonstrated a few G-CSF-positive tumor cells (high-power magnification). d Immunohistochemical staining demonstrated IL-6-positive tumor cells (high-power magnification)
On admission to our hospital, the patient’s body temperature was 39.1 °C. His laboratory data showed the following: hemoglobin, 6.1 g/dl; serum iron, 16 µg/dl; serum total iron-binding capacity (TIBC), 183 µg/dl; ferritin, 2123 ng/dl. From these data, anemia of inflammation was suspected (Table 1). The white blood cell (WBC) count was 42,400/µl (neutrophils, 68.1%), the C-reactive protein (CRP) level was 19.38 mg/dl, and the procalcitonin level was 0.19 ng/ml, thus there was no evidence of infection. The serum G-CSF and serum interleukin-6 (IL-6) levels were 531 and 245 pg/ml, respectively. The patient had taken non-steroidal anti-inflammatory drugs for the persistent fever and has received red blood cell (RBC) transfusion (total amount, 2240 ml) for anemia of inflammation (Fig. 2). However, as these treatments were insufficient to control his fever and anemia, surgical resection of the tumor was scheduled.
The patient underwent right upper lobectomy with combined resection of the second to the fourth ribs and mediastinal lymph node dissection. His postoperative course was uneventful, and both persistent fever and anemia disappeared immediately postoperatively. The WBC count and CRP level improved to within the normal range, and the serum G-CSF level decreased to 19.5 pg/ml on postoperative day 14, when he was discharged.
Macroscopically, the tumor was 75 × 70 × 50 mm in diameter with massive necrosis. Histologically, the tumor was composed of numerous giant cells with significant nuclear pleomorphism (Fig. 1b). Immunohistochemically, the tumor was found to be positive for both G-CSF and IL-6 (Fig. 1c, d). There was no evidence of lymph node metastasis. The pathological diagnosis was T3cN0M0 stage IIB pleomorphic carcinoma, which produced G-CSF.
The patient received adjuvant platinum-based chemotherapy. He has remained healthy without any recurrence 3 years and 4 months after the lung resection.
Discussion
G-CSF-producing lung cancer was first described by Asano et al. in 1977 [2]. Although there are currently no established diagnostic criteria for G-CSF-producing lung cancers, the following criteria proposed by Asano et al. may be useful for diagnosis: (a) marked increase in WBC count (particularly in mature neutrophils) without any infection or other diseases, (b) elevation of serum G-CSF level, (c) decrease in WBC count and a normal serum G-CSF level after tumor resection, and (d) demonstration of G-CSF activity in the tumor specimens or tumor cell culture. The present case met all the above-mentioned criteria. Patients with G-CSF-producing tumors often have fever or a high serum CRP level, as well as a high WBC count [3, 4]. These phenomena are considered to induce the production of other inflammatory cytokines, because G-CSF alone does not induce inflammation. Kasuga et al. demonstrated that patients with G-CSF-producing tumors showed an increase in the serum IL-6 level and/or were positive for IL-6 on immunohistochemical staining [1]. Moreover, Castleman disease could be excluded as a diagnosis of the present case because the radiological findings showed no mediastinal mass or swollen mediastinal lymph nodes. There were also no pathological findings suspected of Castleman disease in the dissected lymph nodes. In the present case, G-CSF and IL-6 production by the tumor was assumed to induce the symptoms.
To the best of our knowledge, approximately 80–90 cases with G-CSF-producing lung cancer have been reported in English articles thus far, but there have been no reports showing that G-CSF-producing lung cancer induces severe anemia that requires RBC transfusion, except for anemia caused by gastrointestinal bleeding from gastrointestinal metastases. Most anemias of chronic disease/inflammation do not become severe with frequent RBC transfusions, but are mild or moderate. In the present case, despite the needed frequent RBC transfusions, the patient did not show shock or any unstable vital signs. The primary diagnosis was definitively anemia of inflammation due to the continuous fever and tumor. It was difficult to diagnose the condition as hemorrhagic anemia because the patient had a very small amount of bloody sputum and no gastrointestinal bleeding. The laboratory data showed normocytic anemia (MCV, 86.9 fl) with the number of reticulocytes slightly above the upper normal level (i.e., 1.68%; normal range 0.5–1.5%, data not shown in Table 1) and no evidence of hemolytic anemia. Moreover, the data demonstrated low levels of serum iron and TIBC, and high levels of serum ferritin and CRP. For these reasons, the G-CSF-producing lung cancer in the present case induced continuous severe inflammation and required the patient to have sequential transfusion for his anemia.
The performance status and general condition of the patient were expected to deteriorate because of the continuous inflammation. Furthermore, it was necessary to control his severe anemia immediately. We confirmed that the patient had paraneoplastic syndrome and decided to perform surgical resection so that both the syndrome and the lung cancer would be resolved. G-CSF-producing lung cancer occasionally shows a rapid progression or a worse survival rate than other lung cancers [1, 5]. It is, therefore, crucial to definitively diagnose G-CSF-producing tumors and make an immediate decision regarding their appropriate treatment. Herein, we report the apparent first successful case of surgical resection of G-CSF-producing lung cancer in a patient with severe anemia and uncontrollable fever.
References
Kasuga I, Makino S, Kiyokawa H, Katoh H, Ebihara Y, Ohyashiki K. Tumor-related leukocytosis is linked with poor prognosis in patients with lung carcinoma. Cancer. 2001;92(9):2399–405.
Asano S, Urabe A, Okabe T, Sato N, Kondo Y. Demonstration of granulopoietic factor(s) in the plasma of nude mice transplanted with a human lung cancer and in the tumor tissue. Blood. 1977;49(5):845–52.
Wada H, Yoshida S, Ishibashi F, Mizobuchi T, Moriya Y, Hoshino H, et al. Pleomorphic carcinoma of the lung producing granulocyte colony-stimulating factor: report of a case. Surg Today. 2011;41(8):1161–5.
Yamamoto M, Manabe S, Moriyama Y, Ishii H, Tanaka S, Takahashi R, et al. Long-term remission achieved via combined chemotherapy and radiotherapy in a non-resectable granulocyte colony-stimulating factor producing pleomorphic carcinoma of the lung. Intern Med. 2013;52(19):2259–63.
Matsumoto M, Nakayama T, Inoue D, Takamatsu K, Itotani R, Ishitoko M, et al. A pleomorphic carcinoma of the lung producing multiple cytokines and forming a rapidly progressive mass-like opacity. BMC Cancer. 2014;14:588.
Acknowledgements
The authors are indebted to Dr. Edward Barroga (http://orcid.org/0000-0002-8920-2607), Associate Professor and Senior Medical Editor from the Department of International Medical Communications of Tokyo Medical University for editing and reviewing the English manuscript. The authors also thank Hitomi Yokota for her skillful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this study.
Rights and permissions
About this article
Cite this article
Murakami, K., Kudo, Y., Kakihana, M. et al. Granulocyte colony stimulating factor-producing lung cancer with severe anemia of inflammation. Gen Thorac Cardiovasc Surg 66, 415–418 (2018). https://doi.org/10.1007/s11748-018-0914-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-018-0914-1