Abstract
Introduction
Intraoperative alveolar air leaks remain a significant problem in thoracoscopic surgery (TS) cases. We examined the usefulness of covering damaged lung tissue with a subcutaneous fat pad for preventing postoperative air leakage in patients with non-small cell lung cancer (NSCLC).
Methods
Patients with NSCLC underwent a thoracoscopic lobectomy or segmentectomy. When alveolar air leakage from the superficial pulmonary parenchyma was found, fibrin glue in combination with an absorbable mesh sheet was applied (S group; n = 100). When leakage originated from deep within the pulmonary parenchyma, a subcutaneous fat pad about 2 × 2 cm in size was harvested from the utility incision and placed on the damaged lung tissue with fibrin glue and sutures (F group; n = 66). Patient characteristics, air leak duration, and chest-tube removal time were analyzed.
Results
The homogeneity of each group was consistent, with no statistical differences for age, respiratory function, surgical procedures, pathologic stage, and histological type. The air leak duration was significantly shorter (p = 0.015), and the chest tube was removed significantly earlier (p = 0.002) in patients in the F group.
Conclusion
Use of a free subcutaneous fat pad during pulmonary resection for TS patients with NSCLC reduced the duration of air leakage and chest tube drainage. The present method is easy, safe, and effective for repairing an air leak from remaining lung tissues in such cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intraoperative alveolar air leaks can occur following a pulmonary resection procedure [1, 2], which, despite routine use of sutures and stapling devices, remain a significant problem in thoracoscopic surgery (TS) cases. Air leakage that persists for more than 7 days after surgery has traditionally been defined as a prolonged air leak and often results in increased complications, such as longer drainage time, infection, empyema, and increased length of hospitalization [3]. In fact, one of the most frequent complications encountered after TS is a prolonged air leak [4]. Although reinforcement of the visceral pleura around the staple line and injured pulmonary parenchyma is a reasonable method to prevent postoperative air leakage, such sutures may be difficult to employ in TS cases. We have recently reported that reinforcement of damaged lung tissues by use of subcutaneous free fat pads is a safe procedure in patients who underwent a pulmonary resection using a thoracoscopic surgical procedure [5]. In the present study, we examined the effectiveness of subcutaneous fat pads used for covering damaged lung tissue as prevention of postoperative air leaks in TS patients with non-small cell lung cancer (NSCLC).
Patients
We performed a retrospective review of prospectively collected chart data for 219 patients with NSCLC who underwent a lobectomy or segmentectomy using a thoracoscopic surgical procedure at Osaka University Hospital from January 2010 to March 2014.
Operative procedures
All patients underwent general anesthesia procedures and were intubated with a double-lumen endotracheal tube to allow selective contralateral ventilation, then placed in the lateral decubitus position. The initial thoracoscope incision was performed in the 7th intercostal space along the midaxillary line, and a 2-cm incision was then made in the 7th intercostal space in the auscultatory triangle. An access thoracotomy was also located in the 4th intercostal space along the anterior axillary line (3–5 cm) in all patients for all types of pulmonary resection performed. After resection, hilar and mediastinal lymph node dissection was performed as in an open thoracotomy procedure, followed by an air leak test under pressure loading of 25 cm H2O.
As no leakage was detected in 44 patients, no coverage of the margin of the dissected or stapled lung tissue was performed, while small air leaks in other patients were managed by suturing. In five patients, air leakage was controlled using a Tachosil® absorbable fibrin patch; thus, those were excluded from analysis. When alveolar air leakage occurred from the superficial pulmonary parenchyma, it was managed with fibrin glue in combination with an absorbable mesh sheet [Neoveil® absorbable polyglycolic acid (PGA) felt, Gunze, Osaka, Japan] (S group). In cases with alveolar air leakage occurring from a location deep in the pulmonary parenchyma, subcutaneous fat pads about 2 × 2 cm in size were harvested from the access thoracotomy (Fig. 1) and placed on the damaged lung tissue with fibrin glue in combination with 2 or 3 mattress sutures as shown in Fig. 2 (F group). The number of fat pad pieces employed was dependent on the number of air leaks repaired. When air leaks were noted from both superficial and deep pulmonary parenchyma locations, we used both PGA felts and subcutaneous fat pads with fibrin glue. Four patients were excluded from analysis because of postoperative complications such as chylothorax and cerebrovascular disease. Thus, the S and F groups consisted of 100 and 66 patients, respectively.
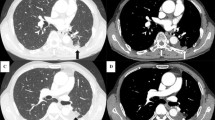
A Thoracoscopic view showing air leakage from lung parenchyma. B Thoracoscopic view showing an injured pulmonary parenchyma beside the intralobular pulmonary artery. C Thoracoscopic view showing management of an injured pulmonary parenchyma. D Thoracoscopic view showing harvested subcutaneous fat pads attached to damaged lung tissue with two mattress sutures
Comparisons
All of the patients received a 19- or 24-F chest tube at the end of the operation, and suction at −10 cm H2O was applied during the postoperative period. The chest tube was removed when pleural drainage decreased to less than 200 cc/day, and no air leakage was detected. The primary objective of this study was to determine the efficacy of fat pad use for avoiding prolonged postoperative air leakage by comparing the duration of chest-tube drainage between the groups.
Statistical analyses
Results are expressed as the mean ± standard deviation, median, and range values. Quantitative values were compared between the groups using a Student’s t test and a χ 2 test.
Results
The demographics and clinical characteristics of the patients are shown in Table 1. The homogeneity of each group was consistent, with no statistical differences for age, respiratory function, surgical procedures, pathologic stage, and histologic type. There were also no significant differences regarding the occurrence of postoperative complications other than postoperative prolonged air leak between the groups.
A prolonged air leak (>7 days) occurred in 15 patients (15 %) in the S group and 4 (7 %) in F (p = 0.15). Two patients in the S group underwent a re-operation for repair of air leakage and none in the F group. The air leak duration was significantly shorter, and the chest tube was removed significantly earlier in patients in the F group (Fig. 3).
Discussion
Use of fat pads harvested from the patient during a surgical procedure has advantages including no cost or adverse effects as compared to commercially available non-autologous materials. A previous report noted that autologous tissues including the pleura, pericardium, and fat pad can be used as biological pledgets and are particularly useful when the quality of the lung tissue is emphysematous and unlikely to support simple suturing [6]. In addition, Ueda et al. reported that a combination of PGA mesh and glue was superior to glue alone for reducing the duration of chest tube drainage and postoperative cardiopulmonary complications [7]. When alveolar air leakage occurs from the superficial pulmonary parenchyma, we use fibrin glue in combination with a PGA sheet for management. However, when that occurs from deep within or in a large area of pulmonary parenchyma, a subcutaneous-free fat pad is placed onto the damaged lung tissue with fibrin glue in combination with 2 or 3 mattress sutures. The present results showed that use of a free fat pad in addition to glue with or without a PGA sheet reduced the duration of chest tube drainage, indicating that this method is useful for air leakage repair. In addition, we previously reported the continuing existence of fixed free fat pads up to several months after surgery [5].
Postoperative air leaks frequently occur after closure of the chest wall despite water seal test findings showing no such leakage. During TS, it is difficult to find the exact location of an air leak, because the procedure is performed in a closed space and the infiltrated lung obstructs the thoracoscopic view. Another mechanism of air leakage recurrence may be over-inflation of the residual lung after closure of the chest wall, which stretches the dissected lung parenchyma, thereby reopening the alveolar fistula [7]. With our method, free subcutaneous fat pads applied to damaged fragile lung tissues are fixed by mattress sutures such as a pledgeted type to protect the parenchyma along the suture lines. However, it is difficult to perform continuous sutures at the point of air leakage during a TS procedure; thus, we consider that free subcutaneous fat pads are advantageous, as they can be easily collected and fixed. The operation time in the F group was similar to that in the S group, likely because it is easier to prepare the free fat pad from the working port during TS as compared to harvesting intrathoracic pleura or pericardial fat pad samples.
Limitations of this study include the small number of patients and lack of a prospective randomized procedure. The procedure to control air leakage was chosen by the attending surgeon during the operation. Thus, further investigation is required to prove the efficacy of our method. Furthermore, we analyzed the duration of chest tube drainage instead of air leak duration, though chest tube drainage time is considered to reliably reflect the duration of air leakage.
In conclusion, the use of free subcutaneous fat pads during TS for patients with NSCLC reduced the duration of chest tube drainage. Although not previously documented, this method was found to be safe and effective for repair of air leakage from remaining lung tissues.
References
Brunelli A, Varela G, Refai M, Jimenez MF, Pompili C, Sabbatini A, Aranda JL (2010) A scoring system to predict the risk of prolonged air leak after lobectomy. Ann Thorac Surg 90(1):204–209. doi:10.1016/j.athoracsur.2010.02.054
Filosso PL, Ruffini E, Sandri A, Lausi PO, Giobbe R, Oliaro A (2013) Efficacy and safety of human fibrinogen-thrombin patch (TachoSil(R)) in the treatment of postoperative air leakage in patients submitted to redo surgery for lung malignancies: a randomized trial. Interact Cardiovasc Thorac Surg 16(5):661–666. doi:10.1093/icvts/ivs571
Anegg U, Rychlik R, Smolle-Juttner F (2008) Do the benefits of shorter hospital stay associated with the use of fleece-bound sealing outweigh the cost of the materials? Interactive cardiovascular and thoracic surgery 7(2):292–296. doi:10.1510/icvts.2007.162677 discussion 226
Yamamoto K, Ohsumi A, Kojima F, Imanishi N, Matsuoka K, Ueda M, Miyamoto Y (2010) Long-term survival after video-assisted thoracic surgery lobectomy for primary lung cancer. Ann Thorac Surg 89(2):353–359. doi:10.1016/j.athoracsur.2009.10.034
Shintani Y, Inoue M, Nakagiri T, Okumura M (2014) Use of free subcutaneous fat pad for reduction of intraoperative air leak in thoracoscopic pulmonary resection cases with lung cancer. Eur J Cardiothorac Surg. doi:10.1093/ejcts/ezt608
Shrager JB, DeCamp MM, Murthy SC (2009) Intraoperative and postoperative management of air leaks in patients with emphysema. Thorac Surg Clin 19(2):223–231. doi:10.1016/j.thorsurg.2009.02.004 ix
Ueda K, Tanaka T, Li TS, Tanaka N, Hamano K (2010) Sutureless pneumostasis using bioabsorbable mesh and glue during major lung resection for cancer: who are the best candidates? J Thorac Cardiovasc Surg 139(3):600–605. doi:10.1016/j.jtcvs.2009.06.021
Disclosures
Yasushi Shintani, Masayoshi Inoue, Soichiro Funaki, Tomohiro Kawamura, Masato Minami, and Meinoshin Okumura have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shintani, Y., Inoue, M., Funaki, S. et al. Clinical usefulness of free subcutaneous fat pad for reduction of intraoperative air leakage during thoracoscopic pulmonary resection in lung cancer cases. Surg Endosc 29, 2910–2913 (2015). https://doi.org/10.1007/s00464-014-4019-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-4019-3