Abstract
To investigate the prognostic role of procalcitonin (PCT) assessment and blood culture (BC) acquisition in the emergency department (ED) in patients with urinary tract infection (UTI) or urosepsis. We enrolled patients admitted for UTI to our ED over a 10-year period. Mortality and in hospital length of stay (LOS) were compared between patients with UTI or urosepsis who had sampling for PCT levels and BC taken in the ED (ePCT group–eBC group) and those who had not (no-ePCT group–no-eBC group). 1029 patients were analyzed, 52.7% of which were female. Median age was 77 [65–83]; 139 patients (13.5%) had complicated UTI. Median LOS was 10 [7–17] days. In the ePCT group, LOS was 10 [7–16] days, vs. 10 [7–17] (p = 0.428) in the no-ePCT group. In the eBC group, LOS was 10 [6–16] days vs. 10 [7–17] days (p = 0.369) in the no-eBC group. The overall mortality rate was 6.6%. The mortality rate was not affected by early PCT determination (6% in the ePCT group vs. 6.9% in the no-ePCT group, p = 0.584). Similarly, the mortality rate was not different in the eBC group as compared to the no-eBC group (5.4% vs. 6.9%, p = 0.415). Performance of ePCT or eBC testing made no significant difference in terms of improvement of mortality rates in septic patients (11.4% vs. 7.2%; p = 0.397 and 8.8% vs. 9.8%; p = 0.845, respectively). The prognostic relevance of early evaluation of PCT and BC in the ED of patients with febrile UTI appears limited. In complicated UTI patients, PCT and BC testing may be more appropriate in the context of improving antibiotic stewardship, or as an integral component of PCT-guided standardized protocols.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is one of the most common pathologies presenting to the Emergency Department ED [1]. Acute pyelonephritis and cystitis are the most typical presentations of febrile UTI. These conditions may evolve into a clinical picture of urosepsis, which represents a life-threatening condition caused by dysregulated host responses to UTI [2, 3]. The overall mortality rate for urosepsis varies from 7.5 to 30% [4,5,6]. The diagnosis of febrile UTI is clinical and supported by urinalysis and urine culture findings, while the gold standard for confirming urosepsis is a positive blood culture (BC) [7, 8]. Nevertheless, most patients presenting to the ED with UTI will not develop urosepsis, and obtaining BC in the ED is time-consuming and expensive. Furthermore, the emergency physician clinical decision-making often takes place before BC results become available, at least 24–72 h after samples are sent. Although not yet present in established diagnostic algorithms, procalcitonin (PCT), a peptide precursor of the hormone calcitonin, has been proposed as an early biomarker of sepsis and is now widely used in this specific clinical scenario [9, 10]. However, some doubt remains as to early assessment of PCT is correlated to better outcomes in UTI patients accessing ED.
The aim of this work is to evaluate, in a retrospective series of patients admitted to the hospital from the ED over the last 10 years for febrile UTI, whether early assessment of PCT and/or BC was correlated to improved outcomes, defined as a reduction in mortality and in length of hospital stay (LOS).
Materials and methods
We conducted a retrospective analysis of all patients evaluated for UTI in the ED of a tertiary university hospital and then admitted to internal medicine or infectious disease units, from January 2009 to December 2018. Our ED has an annual attendance of about 75,000 patients, 87% of them adults. The inclusion criteria were age > 18 years, fever (T > 38 °C) or chills within 24 h of presentation, at least one symptom typical of UTI (flank pain or perineal pain, dysuria, frequency, urgency), leucocyturia or positive urine culture. Exclusion criteria were age < 18 years, pregnancy, history of kidney transplantation, hemodialyisis or peritoneal dialysis, patients suffering from acute lymphoma, leukemia or HIV+ .
In all cases, the quick-SOFA score (qSOFA) and Charlson comorbidity index were assessed [11, 12].
We classified enrolled patients as having either uncomplicated UTI or complicated UTI according to diagnosis at hospital discharge.
Patients were defined as having complicated UTI if the diagnosis at discharge included pyelonephritis, renal abscess or catheter-associated UTI, or if they developed urosepsis defined according to the current guidelines [13, 14]. The remaining patients were classified as uncomplicated UTI.
Blood samples
The emergency physician decided whether to request blood cultures or PCT at the time of ED admission based on clinical judgment.
Blood cultures were obtained in the ED using antiseptic technique. Two 10 ml blood samples were drawn into standard culture bottles. The cutoff value of PCT serum level predictive of sepsis was set at 1 ng/ml. A PCT value between 0.5 and 1 ng/ml was considered borderline. Testing was available 24 h a day in our ED.
Study outcome
Intra-hospital mortality and in hospital length of stay (LOS) were compared between patients who had undergone PCT sampling in the emergency department and patients who had not, and between patients who had BCs taken in the ED compared with patients who had not.
Statistical analysis and sample size
Categorical variables are presented as numbers and percentages, and continuous variables are presented as median [lower quartile, upper quartile]. Categorical variables evaluated in the study were statistically compared by univariate analysis with the χ² test. Since our continuous variables were not normally distributed, statistical comparison was performed using the Mann–Whitney U test.
We analyzed mortality rate and LOS in patients who underwent early PTC/BC testing in the ED compared to patients who did not. To reduce confounding bias introduced by differences in infection severity, we stratified our analysis in separate subgroups including uncomplicated UTI and complicated UTI or urosepsis.
Considering the overall mortality in this population of 6% assuming a beta error of 0.2 and an alpha error of 0.05, our sample size was adequate to evaluate a difference in overall mortality of 5% between the two study groups.
To further assess the relevance of early BC and PCT, we performed a sub-analysis of our data including only those patients who had these tests in the ED. Specifically, mortality rate and LOS were compared between patients with negative (< 1 ng/ml) early PCT results vs. positive (≥ 1 ng/ml) results, and we also compared death and LOS in patients who had a negative blood culture vs. patients with positive BC.
All data were analyzed by SPSS v25® (IBM, IL, USA).
Results
In the study period, 8172 patients received a diagnosis of UTI or urosepsis in our ED, of which 1110 were admitted to internal medicine or infectious disease units (13.6%). Among them, 81 were excluded from the study as they did not meet inclusion criteria. Thus, a final retrospective cohort of 1029 patients admitted to the hospital from the ED for febrile UTI or urosepsis was available for analysis in the present study.
There were 542 females (52.7%) with a median age of 78 [61–85] years and 487 males (47.3%), with a median age of 75 [64–82] years. On access to the ED 204 patients (19.8%) had a qSOFA > 0. When stratified according to the Charlson comorbidity index, 238 patients (23.1%) had a score of ≥ 2.
According to the discharge diagnosis, 139 (13.5%) patients were affected by complicated UTI, and 890 (86.5%) by uncomplicated UTI. Early PCT dosage (obtained during ED evaluation) was performed in 318 (30.9%) patients (ePCT group) and BC determination was performed in 222 (21.6%) (eBC group). Demographic and clinical data of the study patients are shown in Table 1.
Median LOS for the entire population was 10 [7–17] days. LOS was not significantly different between ePCT and no-ePCT groups (LOS was 10 [7–16] days in ePCT patients, and 10 [7–17] in no-ePCT group; p = 0.846) (Table 2).
In the subgroup analysis, LOS in patients with uncomplicated UTI was not found to be statistically different if PCT was assessed in the ED (ePCT group LOS 9 [6–14] days vs. no-ePCT group 10 [6–16] days; p = 0.081). Similarly, no statistically significant difference was found in the median LOS of complicated UTI patients between the ePCT and no-ePCT group (14, 5 [9–26] days vs. 13 [8.5–21] days, p = 0.163) (Table 2).
Length of stay was not significantly different between patients who had BCs taken in the ED compared to patients who were admitted to the ward without BC sampling (LOS was 10 [6–16] days eBC group vs. 10 [7–17] days in no-eBC group; p = 0.391). Similarly, BC determination in the ED did not affect LOS in complicated UTI patients (eBC LOS was 14 [9–26] days vs. 13 [9–21] days in no-eBC; p = 0.327). Interestingly, patients with uncomplicated UTI had a slight, but significant reduction in LOS if blood cultures were taken in the ED (eBC LOS 9 [5.5–13] days vs. no-eBC group 10 [7–16] days, p = 0.010) (Table 2).
Sixty-nine patients died, with an overall mortality rate of 6.6%. No statistically significant difference was found between the ePCt and the no-ePCT groups (19 patients (6%) vs. 49 patients (6.9%); p = 0.584) as well as between the eBC and the no-eBC groups (12 patients (5.4%), vs. 56 patients (6.9%); p = 0.415) (Table 3).
When considering uncomplicated UTI cases, no statistically significant difference in mortality was found between ePCT and no-ePCT groups (11 pts (6.2%) vs. 44 pts (6.9%); p = 0.179 (Table 3), with analogous findings when comparing the eBC and no-eBC groups (7 pts [4.2%] vs. 48 pts [6.6%]; p = 0.252).
Similarly, in complicated UTI patients, the mortality rate was comparable in both the ePCT and no-ePCT groups (8 pts (11.4%) vs. 5 pts (7.2%), p = 0.397). Again, the mortality rate did not differ significantly between the eBC and no-eBC groups (5 pts (8.8%) vs. 8 pts (9.8%), p = 0.845).
When taking into consideration solely, the 318 patients who underwent early PCT testing, we found that in 222 (69.8%), the PCT value was < 1 ng/ml, while in 96 (30.2%), it was > 1 ng/ml. No differences were found between positive and negative PCT patients in terms of age, Charlson comorbidity index or qSOFA score. As expected, the number of complicated UTIs was significantly higher in the PCT > 1 ng/ml group (Table 4A). Furthermore, we found that the median LOS was significantly higher in patients with high PCT (13[7.5–22] vs. 9 [7–15]; p = 0.024). Finally, we observed a higher mortality rate in patients with high PCT in the ED, but the difference did not reach statistical significance (Table 4A).
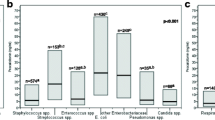
Among the 222 patients who had BCs performed in the ED, 158 patients (71.2%) had negative BCs and 64 (28.8%) were positive. We found that patients with positive BCs were significantly older (76 [64–83] years vs. negative BCs 69.5 [52–79] years; p = 0.002). As expected, diagnosis of complicated UTI was significantly more frequent with positive vs. negative BCs (89.1 vs. 6.3%, p < 0.001). Positive BC patients had a significantly longer LOS (14.5 [10–26] days vs. 8 [5–13] days, p < 0.001), and a higher mortality rate (9.4% vs 3.8%, p = 0.096). However, as for high PCT, this latter difference did not reach statistical significance (Table 4B).
Discussion
More than 1000,000 people in the United States are admitted annually to the ED for pyelonephritis or UTI [5]. Complications requiring hospital admission occur in approximately 10% of these patients [15], of which an estimated 41% develop sepsis [16]. Mortality rate for urosepsis varies from 7.5 to 30% of cases [4,5,6]. Unfortunately, determining which UTI may progress to a more serious clinical picture and which are simple uncomplicated UTI is a difficult task in the ED, particularly when the patient lacks the cognitive or physical ability to communicate symptoms [16, 17]. Indeed, despite convincing data that treatment of asymptomatic bacteriuria lacks benefit, these patients are overly exposed to broad-spectrum antibiotic therapy initiated in the ED or upon hospital admission [18, 19].
Recognition of bacterial infection and sepsis can be achieved by methods that are aimed at directly identifying bacteria in the bloodstream (blood culture), or indirectly by the evaluation of inflammatory response proteins [16]. Many inflammatory response proteins have been tested as early markers of poor prognosis in patients with febrile UTI, both in the ED as well as in Intensive Care Units (ICU). The utility of PCT in the management of patients with sepsis has been largely endorsed by the Sepsis Survival Campaign [20].
Many trials have reliably demonstrated the reliable performance of PCT in decision-support algorithms for antibiotic initiation or cessation, with consequent potential benefit in term of LOS and even survival. However, this benefit was not confirmed in the ED setting for lower respiratory tract infections [21], and in unselected ED patients with fever [22]. However, it has been argued that such a result was more due to the clinicians’ fear of untreated infection rather than a weakness of the test itself, given that broad-spectrum antibiotic therapy was often administered regardless of PCT values.
A recent meta-analysis investigating the role of PCT in diagnosis, prognosis, monitoring and escalation/de-escalation of antibiotic therapy in septic patients concluded that serum PCT concentrations do not correlate with the severity of sepsis or mortality [23]. Nevertheless, all but 1 of 17 studies considered [24] concerned patients admitted to intensive care units. To the best of our knowledge, only three studies addressed the correlation of early assessment of PCT in the ED and prognosis in patients affected by febrile UTI [25,26,27]. Lemiale et al. [25] found no correlation between PCT serum levels and adverse medical outcome among a group of 58 patients with pyelonephritis evaluated in the ED. Park et al. [26] showed that PCT had no role in predicting mortality among 240 female patients evaluated in the ED for acute pyelonephritis. On the other hand, Ko et al. [27] in a cohort of 49 patients affected by acute pyelonephritis subsequent to a ureteral stone, found a statistically significant correlation between PCT serum level and progression to septic shock.
The results of our study are in line with those reported by Lemiale et al. and Park et al. [25, 26]. We found no statistically significant difference both in terms of mortality and of LOS regardless of early PCT assessment in ED, both in uncomplicated febrile UTI and in complicated UTI.
However, while these findings were expected for patients with uncomplicated UTI, it is remarkable that the same results were found in patients with serious infections. A partial explanation of this latter finding could be that PCT levels vary with time [28], and it appears that the severity of infection is better predicted by the peak during the first 3 days of the septic state [29, 30]. Nevertheless, the most likely explanation for our data is that most of our patients received early broad-spectrum antibiotic therapy, as widely recommended [20], and that no specific PCT-guided antibiotic protocol was established in our ED.
Moreover, as previously noted, the most important role of PCT assessment is neither predictive nor prognostic, but is in guiding de-escalation of antibiotic therapy [31, 32]. Thus, the positive impact on clinical outcomes can only be expected when PCT is used by an antibiotic stewardship team to optimize antibiotic therapy during hospitalization. An antibiotic stewardship team has only recently been introduced to our hospital, and a strategy of early de-escalation based on results of PCT or BC has been not yet fully implemented.
As regards to BC sampling in our UTI cohort, our data confirm that in the 222 patients that had BCs in the ED, LOS and mortality rate were not statistically different compared with patients who did not have BCs taken. The literature supports this finding, as reports have shown limited usefulness of BCs in the ED particularly in immunocompetent patients with common illnesses, such as urinary tract infections [33,34,35]. Furthermore, a large 2007 study showed that of 2210 blood cultures taken in ED, only 132 yielded positive growth, with as low as 4 (0.18%) resulting in modification of the patient’s management [36]. Interestingly, we found that patients with uncomplicated UTI who had BC sampling in ED had a slightly lower LOS compared to patients who not received BC (Table 2), still having a similar mortality rate. These latter findings may be explained by the fact that BC results, typically negative in these patients, were more quickly available for clinical decision-making as they had been taken earlier, that is, in the ED. However, the slight difference in LOS in this group of patients should be confirmed in larger series, as should the real cost-effectiveness of indiscriminate BC acquisition in the ED for any febrile UTI patients.
Our data suggest that even in complicated UTI, BCs in the ED do not provide a clear benefit in terms of patient outcome. It is well known that bacteremia is present in 15–40% of patients with complicated urinary tract infections, with some guidelines recommending blood cultures [37, 38]. However, the available data suggest that in adult patients with simple pyelonephritis, BCs do not alter management, and in most cases, BC results concur with urine cultures [39, 40]. However, since most of the patients considered received early treatment with broad-spectrum antibiotic therapy, and only 64 patients had positive BCs, this study may be underpowered to accurately ascertain the effect of BC sampling on clinical outcome.
Study limitations
Although conducted on a large cohort of patients, our study had several limitations: first of all, its retrospective nature; in addition, we did not measure the number of PCT assessments and BCs taken during hospitalization. Finally, no established rule was defined to determine PCT and BC assessment in ED, nor was a specific management protocol based on PCT results put in place.
Conclusions
Our data suggest that in the ED, early PCT and BC assessment does not change the clinical course of patients admitted for febrile UTI. Furthermore, current evidence supporting the prognostic relevance of these tests in the ED is poor, especially in the absence of active involvement of an antibiotic stewardship team, or the presence of PCT- and BC-based protocols. Thus, when dealing with patients with uncomplicated UTI, a simple urinalysis followed by empiric antibiotic treatment is probably the most appropriate management approach, avoiding unnecessary procedures and related costs.
In complicated UTI, the determination of certified scores of severity of illness, such as APACHE II [41], SOFA [42] or qSOFA [11], appears to still be the most reliable method of identifying UTI patients with poor prognosis [7]. In these cases, PCT and BC sampling in the ED may be justified, but the utility of these tests is increased by the involvement of an antibiotic stewardship unit to optimize antibiotic therapy.
References
Long B, Koyfman A (2018) The emergency department diagnosis and management of urinary tract infection. Emerg Med Clin N Am 36:685–710
Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, Jinenez Cruz F, Selvaggi FP (2006) Urinary Tract Infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU) EAU guidelines on the management of urinary tract and male genital tract infections (UTI). Working group of the Health Care Office (HCO) of the European Association of Urology (EAU). Eur Urol 40:576–588
Wagenlehner FME, Pilatz A, Weidner W, Naber KG (2015) Urosepsis: overview of the diagnostic and treatment challenges. Microbiol Spectr 3(5):1–18
Brown P, Ki M, Foxman B (2005) Acute pyelonephritis among adults: cost of illness and considerations for the economic evaluation and therapy. Pharmacoeconomics 23:1123–1142
Foxman B, Klemstine KL, Brown PD (1997) Acute pyelonephritis in US hospital in hospitalization and in-hospital mortality. Am Epidemiol 13:144–150
Ackerman RI, Monroe PW (1996) Bacteremic urinary tract infection in older people. J Am Geriatr Soc 44:927–933
Papagiannopoulos D, Whelan P, Ahmad W, Rybak J, Hota B, Deane L, Nehra A (2016) Procalcitonin is a strong predictor, of urine culture results in patients with obstructing ureteral stones: a prospective, pilot study. Urol Ann 8:277–279
Lee A, Mirrett S, Reller LB, Weinstein MP (2007) Detection of bloodstream infections in adults: how many blood cultures are needed? J Clin Microbiol 45:3546–3548
van Nieuwkoop C, Bonten TN, van’t Wout JW, Kuijper EJ, Groeneveld GH, Becker MJ, Koster T, Wattel-Louis GH, Delfos NM, Ablij HC, Leyten EM, van Dissel JT (2010) Procalcitonin reflects bacteremia and bacterial load in urosepsis syndrome: a prospective observational study. Crit Care 14R206:2–9
Sugimoto K, Adomi S, Koike H, Esa A (2013) Procalcitonin as an indicator of urosepsis. Res Rep Urol 3:77–80
Antonelli M, DeBacker D, Dorman T. Surviving Sepsis campaign responds to Sepsis-3. http://www.survivingsepsis.org/SiteCollectionDocuments/SSC-Statements-Sepsis-Definitions-3-2016. Accessed 11 May 2019
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB (2011) Urinary tract infection: clinical practice guideline for diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128:595–610
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Best J, Kitlowski AD, Ou D, Bedolla J (2014) Diagnosis and management of urinary tract infections in the emergency department. Emerg Med Pract 16(7):1–23
Pescatore R, Niforatos JD, Rezaie S, Swaminathan A (2019) Evidence-informed practice: diagnostic questions in the urinary tract infections in the elderly. West J Emerg Med 20:573–577
Covino M, Petruzziello C, Onder G, Migneco A, Simeoni B, Franceschi F, Ojetti V (2019) A 12-year retrospective analysis of differences between elderly and oldest old patients referred to the emergency department of a large tertiary hospital. Maturitas 120:7–11
Gandhi T, Flanders SA, Markovitz E, Saint S, Kaul DR (2009) Importance of urinary tract infection to antibiotic use among hospitalized patients. Infect Control Hosp Epidemiol 30(2):193–195
Khawcharoenporn T, Vasoo S, Ward E, Singh K (2011) Abnormal urinalysis finding triggered antibiotic prescription for asymptomatic bacteriuria in the ED. Am J Emerg Med 29(7):828–830
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Huang DT, Yealy DM, Filbin, Brown AM, Chang CH, Doi Y, Donnino MW, Fine J, Fine MJ, Fischer MA, Holst JM, Hou PC, Kellum JA, Khan F, Kurz MC, Lotfipour S, LoVecchio F, Peck-Palmer OM, Pike F, Prunty H, Sherwin RL, Southerland L, Terndrup T, Weissfeld LA, Yabes J, Angus DC, ProACT Investigators (2018) Procalcitonin-guided use of antibiotics for lower respiratory tract infection. N Engl J Med 379(3):236–249
van der Does Y, Limper M, Jie KE, Schuit SCE, Jansen H, Pernot N, van Rosmalen J, Poley MJ, Ramakers C, Patka P, van Gorp ECM, Rood PPM (2018) Procalcitonin-guided antibiotic therapy in patients with fever in a general emergency department population: a multicentre non-inferiority randomized clinical trial (HiTEMP study). Clin Microbiol Infect 24(12):1282–1289
Sridharan P, Chamberlain RS (2013) The efficacy of procalcitonin as a biomarker in the management of sepsis: slaying dragons or tilting at windmills? Surg Infect 14:489–511
Hausfater P, Garric S, Ayed SB, Rosenheim M, Bernard M, Riou B (2002) Usefulness of procalcitonin as a marker of systemic infection in emergency department patients: a prospective study. Clin Infect Dis 34:895–901
Lemiale V, Renaud B, Moutereau S, N’Gako A, Salloum M, Calmettes MJ, Hervé J, Boraud C, Santin A, Grégo JC, Braconnier F, Roupie E (2007) A single procalcitonin level does not predict adverse outcomes of women with pyelonephritis. Eur Urol 51:1394–1401
Park JH, Wee JH, Choi SP, Park KN (2013) Serum procalcitonin level for the prediction of severity in women with acute pyelonephritis in the ED: value of procalcitonin in acute pyelonephritis. Am J Emerg Med 31:1092–1097
Ko YH, Ji YS, Park SY, Kim SJ, Song PH (2016) Procalcitonin determined at emergency department as an early indicator of progression to septic shock in patients with sepsis associated with ureteral calculi. Int Braz J urol 42:270–276
Meisner M, Tschaikowsky K, Palmaers T, Schmidt J (1999) Comparison of procalcitonin (PCT) and C- reactive protein (CRP) plasma concentration at different SOFA scores during the course of sepsis and MODS. Crit Care 3:45–50
Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W (2000) Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med 28:950–957
Luyt CE, Guérin V, Combes A, Trouillet JL, Ayed SB, Bernard M, Gibert C, Chastre J (2005) Procalcitonin kinetics as a prognostic marker of ventilator-associated pneumonia. Care Med 171:48–53
Yunus I, Fasih A, Wang Y (2018) The use of procalcitonin in the determination of severity of sepsis, patient outcomes and infection characteristics. PLoS One 13(11):e0206527
Gluck E, Nguyen HB, Yalamanchili K, McCusker M, Madala J, Corvino FA, Zhu X, Balk R (2018) Real-world use of procalcitonin and other biomarkers among sepsis hospitalizations in the United States: a retrospective, observational study. PLoS One 13(10):e0205924
Long B, Koyfman A (2016) Best clinical practice: blood culture utility in the emergency department. J Emerg Med 51:529–539
Mountain D, Bailey PM, O’Brien D, Jelinek GA (2006) Blood Cultures ordered in the adult emergency department are rarely useful. Eur J Emerg Med 13:76–79
Hsu CY, Fang HC, Chou KJ, Chen CL, Lee PT, Chung HM (2006) The clinical impact of bacteriemia in complicated acute pyelonephritis. Am J Med Sci 332:175–180
Howie N, Gerstenmaier JF, Munro PT (2007) Do peripheral blood cultures taken in the emergency department influence clinical management? Emerg Med J 24:213–214
Coburn B, Morris AM, Tomlinson G, Detsky AS (2012) Does this adult patient with suspected bacteremia require blood cultures? JAMA 308:502–511
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE (2011) Infectious Diseases Society of America; European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 52:e103–e120
Velasco M, Martínez JA, Moreno-Martínez A, Horcajada JP, Ruiz J, Barranco M, Almela M, Vila J, Mensa J (2003) Blood cultures for women with uncomplicated acute pyelonephritis: are they necessary? Clin Infect Dis 37:1127–1130
Smith WR, McClish DK, Poses RM, Pinson AG, Miller ST, Bobo-Moseley L, Morrison RE, Lancaster DJ (1997) Bacteremia in young urban women admitted with pyelonephritis. Am J Med Sci 313:50–57
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: on behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Being a retrospective study performed on a database of anonymized patients, approval of local ethic committee was substituted by formal communication made on May 11 2019.
Statements of human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Covino, M., Manno, A., Merra, G. et al. Reduced utility of early procalcitonin and blood culture determination in patients with febrile urinary tract infections in the emergency department. Intern Emerg Med 15, 119–125 (2020). https://doi.org/10.1007/s11739-019-02212-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02212-2