Abstract
It is not uncommon to incidentally discover prostate cancer during the transurethral resection of the prostate (TURP) for the treatment of benign prostatic hyperplasia and necessitate a subsequent robotic-assisted radical prostatectomy (RARP). The study aims to evaluate whether TURP have negative influence on subsequent RARP. Through a literature search using MEDLINE, EMBASE and the Cochrane Library, 10 studies with 683 patients who underwent RARP after previous TURP and 4039 patients who underwent RARP only were identified for the purposes of the meta-analysis. Compared to standard RARP, RARP after TURP was related to longer operative time (WMD: 29.1 min, 95% CI: 13.3–44.8, P < 0.001), more blood loss (WMD: 49.3 ml, 95% CI: 8.8–89.7, P = 0.02), longer time to catheter removal (WMD: 0.93 days, 95% CI: 0.41–1.44, P < 0.001), higher rates of overall (RR: 1.45, 95% CI: 1.08–1.95, P = 0.01) and major complications (RR: 3.67, 95% Cl: 1.63–8.24, P = 0.002), frequently demand for bladder neck reconstruction (RR: 5.46, 95% CI: 3.15–9.47, P < 0.001) and lower succeed in nerve sparing (RR: 0.73, 95% CI: 0.62–0.87, P < 0.001). In terms of quality of life, there are worse recovery of urinary continence (RR of incontinence rate: RR: 1.24, 95% CI: 1.02–1.52, P = 0.03) and potency (RR: 0.8, 95% CI: 0.73–0.89, P < 0.001) at 1 year in RARP with previous TURP. In addition, the RARP with previous TURP had greater percentage positive margins (RR: 1.24, 95% CI: 1.02–1.52, P = 0.03), while there is no difference in length of stay and biochemical recurrence rate at 1 year. RARP is feasible but challenging after TURP. It significantly increases the difficulty of operation and compromises surgical, functional and oncological outcomes. It is important for urologists and patients to be aware of the negative impact of TURP on subsequent RARP and establish treatment strategies to lessen the adverse effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most frequent cancer, and as the second leading cause of cancer-related mortality in men in western countries, is a global public health problem [1]. Radical prostatectomy is recommended as the standard treatment for localized prostate cancer. With the advances in robotic-assisted technique, robotic-assisted radical prostatectomy (RARP) has become the dominant prostatectomy approach [2].
Generally, prostate cancer is diagnosed by prostate biopsy on the basis of elevated prostate-specific antigen (PSA) or abnormal digital rectal examination. However, age is a risk factor for both benign prostatic hyperplasia (BPH) and prostate cancer, hence it is not uncommon for older men to be incidentally identified with prostate cancer during a transurethral resection of the prostate (TURP) performed to treat their BPH. This accounts for between 2 and 12% of all new cases of prostate cancer [3,4,5]. Patients incidentally discovered of prostate cancer during TURP are recommended to receive a consecutive radical prostatectomy after 3 months. It is anticipated that periprostatic inflammation, fibrosis, and adhesion of the surgical planes caused by perforation of the prostatic capsule and extravasation of blood and irrigation fluid during TURP would make future RARP more challenging. As a consequence, several studies have been published to evaluate the impact of prior TURP on RARP, however, showed controversial findings [4, 6,7,8,9].
In order to benefit the men who underwent RARP with a history of TURP, the internal association between TURP and RARP is of paramount importance. Hence, we performed a meta-analysis of the available literature to evaluate the surgical, functional or oncological outcomes between RARP with or not previous TURP. Moreover, we hypothesized that RARP with previous TURP offers undesirable outcomes, therefore, a literature review would be made to find out some strategies to mitigate the adverse effect of TURP on RARP.
Methods
Search strategy and study selection
Following the guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), a comprehensive review was conducted [10]. This study is registered at the INPLASY register (INPLASY202310062). For this purpose, we searched MEDLINE, EMBASE, and the Cochrane Library from 1998 to November 2022 that met our criteria for inclusion. The search terms were (‘‘TURP’’ OR ‘‘transurethral resection” OR “enucleation”) AND (‘‘robotic OR ‘‘robot’’ OR ‘‘robot assisted”) AND (“radical prostatectomy”). There were no linguistic constraints imposed. The references of retrieved articles were also searched for additional studies. The following requirements should be satisfied by the chosen studies: (1) randomized controlled trials, prospective or retrospective cohort study; (2) compared robot-assisted radical prostatectomy patients with previous TURP (TURP Group) to patients without TURP (no-TURP Group); (3) reported at least one surgical, functional or oncological outcomes of interest; (4) studies relied on a mixed surgical cohort (robot-assisted, laparoscopic, open) were excluded; (5) letters to the editor, reviews, case-series and case reports were not considered, and (6) in the event when studies focusing on the same population, the more informative of the information was included.
Data extraction and quality assessment
Two authors meticulously and independently retrieved data from relevant research, which may include demographics, surgical results, functional, or oncological outcomes. Statistical techniques were used to determine standard deviations (SDs) for research that provided continuous data as means and ranges [11]. The quality of individual included studies was assessed based on the Downs and Black tool [12] by two authors independently. All disagreements were resolved through discussions with another author. When necessary information was missing from the available studies, we contacted the study’s corresponding author for more details.
Outcomes of interest
The surgical outcomes of interest were operative time, estimated blood loss (EBL), time to catheter removal, length of hospital stay (LOS), overall complications, major complications, bladder neck construction and neurovascular bundle (NVB) sparing rate. The functional outcomes included urinary incontinence and potency at 1 year. Either incontinence or potency reported within 1 year or at the last follow-up were not extracted for analysis. The oncological outcomes were positive margin and biochemical recurrence rates (BCR).
Statistical analysis
Comparisons of continuous and dichotomous variables were performed using weighted mean difference (WMD) and risk ratio (RR), respectively, along with 95% confidence interval (95% CI). A P value < 0.05 was considered statistically significant. The presence of heterogeneity between studies were calculated by the χ2 based Q test and I2. An I2 value > 50% accompanied with P value < 0.05 was considered to indicate substantial heterogeneity, in which case, the pooled effect was calculated by a random-effects model (the DerSimonian and Laird method). Otherwise, the fixed effects model (Mantel–Haenszel method) was used for the meta-analysis [13]. For pooled outcomes with significant heterogeneity, sensitivity analyses were performed to explore the potential effect of heterogeneity by eliminating studies that did not use propensity scoring matching. Begg’s funnel plot and Egger’s test were used to evaluate the possibility of publication bias. All the statistical analyses were performed using Review Manager Version 5.4 (The Cochrane Collaboration, Oxford, London, United Kingdom) and STATA software (version 15.0; Stata Corporation, College Station, TX).
Results
Study selection and characteristics of studies
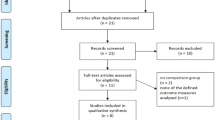
Figure 1 is a flowchart depicting the processes used to choose relevant literature. Our search of the literature yielded a total of 203 articles. After excluding the duplicates and articles not met the inclusion criteria based on the title, abstract scan and subsequent full-text scan, 10 articles with 683 and 4039 patients in TURP and no-TURP group were included in our meta-analysis [3,4,5,6,7,8,9, 14,15,16]. The characteristics and quality assessment of included studies are shown in Table 1. Both ten articles were retrospective cohort design and 3b in level of evidence. Among them, seven articles performed a propensity scoring matching (PSM) [6,7,8,9, 14,15,16], in which age, prostate-specific antigen (PSA) and Gleason score were the most frequent matching factors. According to the quality ratings, the majority of the articles were considered to be of a moderate standard (mean 17, SD 1.49).
Surgical outcomes
Results are summarized in Table 2 and Fig. 2. Compared to the No-TURP group, the operative time (seven articles extracted) of TURP Group is significant longer (WMD: 29.1 min, 95% CI: 13.3–44.8, P < 0.001; I2 = 81%, P < 0.001). In terms of the EBL (eight articles extracted), the TURP Group offered unfavorable outcomes than the No-TURP group (WMD: 49.3 ml, 95% CI: 8.8–89.7, P = 0.02; I2 = 93%, P < 0.001). Patients in TURP Group demonstrated longer time to catheter removal (WMD: 0.93 days, 95% CI: 0.41–1.44, P < 0.001; I2 = 39%, P = 0.16) and similar LOS (WMD: 0.03 days, 95% CI: − 0.31–0.37, P = 0.85; I2 = 0%, P = 0.71), as reported in five and three article, respectively. The overall (RR: 1.45, 95% CI: 1.08–1.95, P = 0.01; I2 = 27%, P = 0.24) and major complication rates (RR: 3.67, 95% CI: 1.63–8.24, P = 0.002; I2 = 19%, P = 0.3) was significantly higher in TURP group than no-TURP group. Regarding to rates of bladder neck reconstruction, 64.7% patients in TURP group received bladder neck reconstruction, which is much higher than that in no-TURP group (9.9%, RR: 5.46, 95% CI: 3.15–9.47, P < 0.001; I2 = 53%, P = 0.05). Six articles reported NVB sparing rate, among which one article [16] propensity scoring matched with NVB sparing, thus five articles were extracted for pooled analysis, and the results showed less patients in TURP group successfully received NVB sparing than that in no-TURP group (RR: 0.73, 95% CI: 0.62–0.87, P < 0.001; I2 = 49%, P = 0.1). Since the heterogeneity exist in pooled outcomes of operative time, EBL and bladder neck reconstruction, the sensitivity analyses were performed by excluding non-PSM studies. Both the operative time (WMD: 30.3 min, 95% CI: 13.6–47.1, P < 0.001) and bladder neck reconstruction rate (RR: 6.38, 95% CI: 2.6–15.6, P < 0.001) exhibited permanent significant differences. Though the TURP group had greater EBL (WMD: 44.2 ml, 95% CI: − 5.9–94.4, P = 0.08), the difference was not statistically significant (Supplemental Fig. 1).
Functional outcomes
Given the importance of long-term urinary and sexual function, only the data of incontinence or potency at 1 year were extracted for analysis. At 1-year follow-up, 16.4% patients in TURP group remained incontinence which was significantly higher than that in no-TURP group (9.6%) (RR: 1.54, 95% CI: 1.19–2, P < 0.001, Table 2 and Fig. 3). In addition, patients in the TURP group also reported lower sexual satisfaction (potency at 1 year: 49.4% vs. 59.1%, RR: 0.8, 95% CI: 0.73–0.89, P < 0.001, Table 2 and Fig. 3).
Oncologic outcomes
All ten articles reported positive margins, the pooled outcomes indicated a higher rate positive margin in TURP group compared with no-TURP group (RR: 1.24, 95% CI: 1.02–1.52, P = 0.03, Table 2 and Fig. 3). Only three articles [3, 4, 16] reported BCR at 1 year and one article [8] reported BCR at last follow-up, thus data of BCRs at 1 year were extracted for pooled analysis. There were no statistical differences in BCR at 1 year between groups (RR: 1.41, 95% CI: 0.87–2.29, P = 0.16, Table 2 and Fig. 3).
Publication bias
There was no discernible asymmetry in the Begg’s funnel plot of the results (Supplemental Fig. 1). Moreover, Egger’s test P values for each outcome were > 0.05, also indicating no substantial publication bias.
Discussion
Incidental cancer of the prostate is found in 3–16% of specimens from TURP [17] and these patients are recommended to receive radical prostatectomy after 3 months. The question of whether a previous TURP has an adverse impact on a future RARP stays debatable at now. To further elucidate these topics, we conducted a meta-analysis and systematic review of the relevant literature.
There are several concerns with respect to the post TURP scenario: (1) potential causes of periprostatic inflammation and fibrosis include infection of the prostate, capsular rupture, and extravasation of irrigation fluid after a TURP [18], (2) inflammation-induced increases in periprostatic adhesions following TURP recovery [19], (3) once the prostate is removed, the prostatovesical junction becomes lax and difficult to define [3], (4) an improper urethrovesical anastomosis is impeded by the surrounding fibrosis, which makes it difficult to identify and preserve appropriate residual urethral length [3], (5) identifying NVBs can be challenging because to periprostatic adhesions, which can make NVB sparing problematic, (6) when a TURP is performed, the ureteric orifices are pulled closer to the bladder neck, making it more difficult to distinguish between the two [19]. Collectively, these factors may exacerbate the difficulties of RARP following TURP, which is consistent with our findings. Consistent with this, the pooled results of our meta-analysis revealed that TURP group had worse surgical outcomes int terms of longer operative time, more blood loss, longer time to catheter removal, higher rates of overall and major complications, frequently demand for bladder neck reconstruction and lower succeed in nerve sparing.
Maintaining the quality of life is an important secondary goal after radical prostatectomy. Urinary incontinence and sexual dysfunction are the most frequent and distressing factors affecting the quality of life for men after radical prostatectomy. The cause of urinary incontinence after radical prostatectomy remains unknown. Pre-prostatectomy physical activity and obesity are important factors in post-prostatectomy continence levels [20]. Besides, surgical technique and surgeon experience are associated with postoperative urinary incontinence [21, 22]. Our results indicated prior TURP also had malign effect on subsequent RARP regarding to long-term incontinence. According to literature reports, selective deep dorsal vein complex division, puboprostatic-sparing techniques, nerve-sparing technique, and restoration of the pelvis space as well as anterior and posterior musculofascial reconstruction were advocated as surgical aspects potentially able to lessen the likelihood of urinary incontinence after RARP [23, 24]. In addition, recovery of continence is enhanced in the short-, intermediate-, and long-term with pelvic floor muscle training administered both pre- and post-operatively [25]. Taken together, patients who have undergone RARP, particularly those who have undergone prior TURP, benefit from a mix of surgical methods and rehabilitation in order to regain continence. Despite the fact that radical prostatectomy is primarily performed on the elderly, still many patients are concerned about their sexual function recovery. Almost half patients remain impotency at 1 year in TURP group, which is more prevalent than no-TURP Group. Both urologists and patients should be aware of this important information.
The presence of a positive margin adversely affects biochemical recurrence and cause specific survival in men with Pca [26]. In our study, positive margins were found to be significantly greater in TURP group compared with the no-TURP group. However, higher positive margins did not increase the biochemical recurrence rate at 1 year in our results. Actually, the rate of biochemical recurrence in each extracted studies [3, 4, 4, 16] is higher in TURP group than that in no-TURP group, despite statistically insignificant. Considering the paucity number of included patients and the relatively low incidence of short-term biochemical recurrence, it is plausible to suppose that RARP following TURP offers worse long-term oncologic outcomes. Nevertheless, future research using well-designed, large samples and extensive follow-up is needed to corroborate these findings.
Considering prior TURP compromises surgical, functional and oncological outcomes of subsequent RARP, any attempt to prevent the incidentally discovery of Pca by TURP should be accomplished. PSA screening is routinely recommend for men aged older than 50 years and is associated with an increased early detection of PCa [27]. However, foley catheterization [28] and larger prostate volume in BPH patients are associated with elevated PSA level, which may confused the urologists. Patients with BPH who are at risk of Pca should have a digital rectal exam [27]. Meanwhile, multiparametric magnetic resonance imaging undoubtedly facilitates the detection of clinical Pca [29]. Combining the PI-RADS score with the PSAD, as described in the published work by Wang et al. [30], has been shown to increase diagnostic certainty for prostate cancer and decrease the number of needless prostate biopsies. Furthermore, PSMA PET/CT can discriminate clinically significant prostate cancer from benign prostate diseases in patients with suspected prostate cancer [31]. Taken together, detailed assessment for elderly individuals with BPH can help them avoid unneeded TURP surgery.
There are some limitations that had to be taken into account. First, all included studies were retrospective. Improper randomization and lack of blinding were major sources of bias. Nevertheless, benefits of patients and ethical considerations prevent a randomized controlled trial from being conducted. Second, differences in surgical equipment and techniques between TURP and RARP might have an impact on the outcomes. Third, there was identified variability in a number of continuous variables. Consequently, the random-effects model was used to lessen the influence of heterogeneity, although it was unable to eradicate it entirely. Fourth, possibly due to its non-normal distribution properties, continuous variables were sometimes given as median and range in research. Statistical techniques were used in our calculations of the mean and standard deviation, which may introduce some degree of error.
In conclusion, RARP is feasible but challenging after TURP. It significantly increases the difficulty of operation and compromises surgical, functional and oncological outcomes. It is important for urologists and patients to be aware of the negative impact of TURP on subsequent RARP and establish treatment strategies perioperatively and post-operatively to lessen the adverse effects.
Data availability
Data will be made available for bona fide researchers on request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33. https://doi.org/10.3322/caac.21708
Gray PJ, Lin CC, Cooperberg MR, Jemal A, Efstathiou JA (2017) Temporal trends and the impact of race, insurance, and socioeconomic status in the management of localized prostate cancer. Eur Urol 71:729–737. https://doi.org/10.1016/j.eururo.2016.08.047
Gupta NP, Singh P, Nayyar R (2011) Outcomes of robot-assisted radical prostatectomy in men with previous transurethral resection of prostate. BJU Int 108:1501–1505. https://doi.org/10.1111/j.1464-410X.2011.10113.x
Hung CF, Yang CK, Ou YC (2014) Robotic assisted laparoscopic radical prostatectomy following transurethral resection of the prostate: perioperative, oncologic and functional outcomes. Prostate Int 2:82–89. https://doi.org/10.12954/PI.14046
Su YK et al (2015) Does previous transurethral prostate surgery affect oncologic and continence outcomes after RARP? J Robot Surg 9:291–297. https://doi.org/10.1007/s11701-015-0529-9
Garg H, Seth A, Kumar R (2022) Impact of previous transurethral resection of prostate on robot-assisted radical prostatectomy: a matched cohort analysis. J Robot Surg 16:1123–1131. https://doi.org/10.1007/s11701-021-01348-8
Tugcu V et al (2015) Robot-assisted radical prostatectomy after previous prostate surgery. JSLS 19:e2015 00080. https://doi.org/10.4293/JSLS.2015.00080
Gellhaus PT et al (2015) Robot-assisted radical prostatectomy in patients with a history of holmium laser enucleation of the prostate: feasibility and evaluation of initial outcomes. J Endourol 29:764–769. https://doi.org/10.1089/end.2014.0767
Zugor V, Labanaris AP, Porres D, Witt JH (2012) Surgical, oncologic, and short-term functional outcomes in patients undergoing robot-assisted prostatectomy after previous transurethral resection of the prostate. J Endourol 26:515–519. https://doi.org/10.1089/end.2011.0205
Shamseer L et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647. https://doi.org/10.1136/bmj.g7647
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Comm Health 52:377–384. https://doi.org/10.1136/jech.52.6.377
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Hampton L, Nelson RA, Satterthwaite R, Wilson T, Crocitto L (2008) Patients with prior TURP undergoing robot-assisted laparoscopic radical prostatectomy have higher positive surgical margin rates. J Robot Surg 2:213–216. https://doi.org/10.1007/s11701-008-0121-7
Abedali ZA et al (2020) Robot-assisted radical prostatectomy in patients with a history of holmium laser enucleation of the prostate: the Indiana university experience. J Endourol 34:163–168. https://doi.org/10.1089/end.2019.0436
Leyh-Bannurah SR et al (2021) Perioperative and postoperative outcomes of robot-assisted radical prostatectomy in prostate cancer patients with prior transurethral subvesical deobstruction: results of a high-volume center. J Urol 206:308–318. https://doi.org/10.1097/JU.0000000000001776
Merrill RM, Wiggins CL (2002) Incidental detection of population-based prostate cancer incidence rates through transurethral resection of the prostate. In: Urologic oncology: seminars and original investigations. Elsevier vol 7, no 5, pp 213–219
Colombo R et al (2006) Radical prostatectomy after previous prostate surgery: clinical and functional outcomes. J Urol 176:2459–2463. https://doi.org/10.1016/j.juro.2006.07.140
Rassweiler J, Teber D, Kuntz R, Hofmann R (2006) Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol 50:969–979. https://doi.org/10.1016/j.eururo.2005.12.042
Wolin KY, Luly J, Sutcliffe S, Andriole GL, Kibel AS (2010) Risk of urinary incontinence following prostatectomy: the role of physical activity and obesity. J Urol 183:629–633
Sandhu JS et al (2019) Incontinence after prostate treatment: AUA/SUFU guideline. J Urol 202:369–378
Cooperberg MR, Odisho AY, Carroll PR (2012) Outcomes for radical prostatectomy: is it the singer, the song, or both? J Clin Oncol Off J Am Soc Clin Oncol 30:476–478
Checcucci E et al (2021) The importance of anatomical reconstruction for continence recovery after robot assisted radical prostatectomy: a systematic review and pooled analysis from referral centers. Minerva Urol Nephrol 73:165–177. https://doi.org/10.23736/S2724-6051.20.04146-6
Mungovan SF et al (2021) Preoperative exercise interventions to optimize continence outcomes following radical prostatectomy. Nat Rev Urol 18:259–281. https://doi.org/10.1038/s41585-021-00445-5
Fernandez RA et al (2015) Improvement of continence rate with pelvic floor muscle training post-prostatectomy: a meta-analysis of randomized controlled trials. Urol Int 94:125–132. https://doi.org/10.1159/000368618
Yossepowitch O et al (2009) Positive surgical margins in radical prostatectomy: outlining the problem and its long-term consequences. Eur Urol 55:87–99. https://doi.org/10.1016/j.eururo.2008.09.051
Mottet N et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Anand A, Gupta S (2021) Prostate-specific antigen increase after urethral catheterisation: fact or myth. Afr J Urol 27:1–3
Johnson DC et al (2019) Detection of individual prostate cancer foci via multiparametric magnetic resonance imaging. Eur Urol 75:712–720. https://doi.org/10.1016/j.eururo.2018.11.031
Wang C et al (2022) Combination of PI-RADS score and PSAD can improve the diagnostic accuracy of prostate cancer and reduce unnecessary prostate biopsies. Front Oncol 12:1024204. https://doi.org/10.3389/fonc.2022.1024204
Jiao J et al (2021) Establishment and prospective validation of an SUV(max) cutoff value to discriminate clinically significant prostate cancer from benign prostate diseases in patients with suspected prostate cancer by (68)Ga-PSMA PET/CT: a real-world study. Theranostics 11:8396–8411. https://doi.org/10.7150/thno.58140
Funding
The author have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
LG: statistical analysis, data extraction, revised manuscripts. YL: statistical analysis, data extraction. XL: statistical analysis, data extraction. WL: study design, statistical analysis, data extraction, wrote the paper. All the authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflict of interest to declare. All the authors have no conflict of financial and non-financial interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gu, L., Li, Y., Li, X. et al. Does previous transurethral resection of the prostate negatively influence subsequent robotic-assisted radical prostatectomy in men diagnosed with prostate cancer? A systematic review and meta-analysis. J Robotic Surg 17, 1299–1307 (2023). https://doi.org/10.1007/s11701-023-01588-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01588-w