Abstract
Transoral robotic surgery (TORS) approach for the treatment of oropharyngeal cancer allows for reduced patient morbidity, amongst other advantages over the traditional lip-splitting mandibulotomy method. Free-flap reconstruction is commonly utilized in head and neck cancer surgeries; however, safety and outcomes of this technique in TORS procedures have not been well studied. The objective of this study was to perform a systematic review to evaluate the efficacy and safety of TORS with free-flap reconstruction (TORS-FFR) for oropharyngeal cancer. A systematic search of Scopus, EMBASE, CINAHL and PubMed databases was completed. Following PRISMA guidelines, case series/reports, retrospective and prospective cohort studies were included. Primary outcomes measured were deaths and complication rates associated with TORS-FFR for oropharyngeal cancers. Secondary outcomes included functional swallowing and airway outcomes, operative time and length of hospital stay. Twenty-one studies met the inclusion criteria comprising a total of 132 patients. The mean patient age was 58.4 years. The most frequent complication was infection (8.9%) followed by flap wound dehiscence (4.2%). The average total operative time was 710 min (n = 48), while average length of hospital stay was 13.5 days (n = 48). Reconstructions were most commonly fashioned from radial forearm free flaps (RFFF), with anterolateral thigh flaps (ALT) representing the second most common free-flap subtype. TORS-FFR procedures for oropharyngeal cancer are safe, with low serious complication rates. This surgical approach may be associated with decreased length of hospital stay; however, further studies are required to better characterize post-operative outcomes.
Level of evidence 1a.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Squamous cell carcinoma is the most common malignancy of the oropharynx, accounting for 90–95% of all oropharyngeal cancers [1, 2]. Risk factors for oropharyngeal cancers include alcohol consumption and tobacco smoking in a dose-related manner, with the role of human papillomavirus (HPV) emerging more recently [1,2,3,4,5]. The molecular driving force behind most oropharyngeal squamous cell carcinomas (OPSCCs) is attributed to tumorigenic changes by oncogenic HPV strains [6,7,8]. In North America, over 65% of OPSCCs are HPV-positive and this has increased by 20.6% worldwide since 1995 [3]. Patients with HPV-positive OPSCC have higher survival rates with both surgical and non-surgical approaches, as compared to non-HPV-positive pathologies; however, continued tobacco use has been shown to negate this survival benefit [9, 10]. While the incidence of oropharyngeal cancers has increased over the past 30 years, the 5-year survival of this disease has improved from 54.0% in 1992 to 71.4% in 2014 [11].
Traditional open surgical extirpation of oropharyngeal cancers frequently required an invasive, lip-splitting mandibulotomy approach to visualize tumors, often leading to significant post-operative speech, swallowing and respiratory dysfunction in addition to bone misalignment [12]. The development of transoral robotic surgery (TORS) has offered a novel surgical approach with improved tumor visualization and enhanced precision in the confined oropharyngeal space without sacrificing oncologic outcomes [13, 14]. The TORS approach has been shown to result in improved functional outcomes and cost effectiveness when compared to open procedures [9, 15, 16]. TORS has become a standard first-line treatment for early-stage OPSCC, and there is rising use of TORS for the surgical management of higher-stage OPSCC [15, 17].
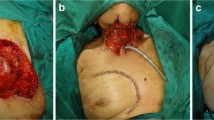
Soon after the FDA approval of TORS for T1 and T2 malignant and non-malignant tumors in 2009, pre-clinical investigations and the first report of using TORS for assisting reconstruction and microvascular anastomosis with free flaps were reported [18, 19]. Free flaps are frequently employed to reconstruct larger, more complex defects, or in salvage surgery in patients previously treated with chemoradiation [13, 16, 18, 20]. The bulk and larger surface area of free flaps can improve swallowing function while preventing velopharyngeal defects and fistula formation [16, 18, 21]. In recurrent OPSCC, free flaps provide healthy vascularized tissue with the ability to withstand the effects of adjuvant therapy [13, 20].
While much of the literature on TORS-FFR is presented as small case reports and case series, larger prospective studies focusing on TORS-FFR have been recently published [9, 20]. An updated review of the literature is required to better inform safety outcomes in TORS-FFR procedures. The aim of this study was to complete a comprehensive systematic review of the use of TORS-FFR for patients with oropharyngeal cancers to characterize patient selection, surgical and functional outcomes, and safety.
Methods
Study design and formulation of research question
This systematic review was prepared using a PICOS (population, intervention, comparison, outcome, and stud design) framework. The population of interest included adult patients over 18 years of age diagnosed with oropharyngeal cancer undergoing transoral robotic surgery with free flap reconstruction (TORS-FFR). The key outcomes of interest were intra- and perioperative complications of TORS-FFR. Secondary outcomes included determining length of hospital stay (LOHS), operative times and swallowing and airway functional results. Operative times included resection, neck dissection and reconstruction times. Flap in-setting and microvascular anastomosis times were included in the total operative times where provided. All observational and comparative studies were eligible to be included, along with case reports and case series. Abstracts, letters, narrative, and previous systematic reviews were not eligible for inclusion (Table 1).
Search strategy
With the assistance of a medical librarian (JK), a comprehensive search of Scopus, EMBASE, CINAHL and PubMed databases was completed on May 15, 2021. Gray literature was also searched through the Network Digital Library of Theses and Dissertations, ProQuest Dissertations and Theses. The full search strategy is detailed in Appendix A and was designed to identify all literature relating to TORS-FFR with appropriate key words and vocabulary. No date or language restrictions were applied. Reference lists of included studies were used to identify additional studies.
Study inclusion and exclusion criteria
Articles in all languages were reviewed and selected if the following criteria were met (Figure 1 and Table 1): (1) participants were diagnosed with oropharyngeal cancer; (2) transoral robotic surgery was utilized for tumour resection, and optionally included flap in-setting or anastomosis; (3) patients received free flap reconstruction; and (4) that all studies, including those incorporating other surgeries with TORS-FFR procedures, included at minimum perioperative complications and safety data (Table 2) that could be traced to TORS-FFR procedures.
Two authors (JP and DM) independently screened titles and abstracts and if the consensus was unclear, articles were moved to full-text screening. Full-text review and data extraction were completed by two independent reviewers. Any discrepancies were resolved through discussion and by a third party. When secondary analysis or long-term follow-up of the same patient cohort was identified, only the primary study was included with details from follow-up studies used to supplement the primary data. Authors of included studies were contacted up to three times to obtain missing data and additional information.
Analysis
For included studies that provided individual patient data, we calculated and reported the weighted mean operative times and weighted mean length of hospital stay. All operative times were converted into minutes for consistency. Data from studies that reported medians was utilized to estimate mean values using a validated equation [22]. Studies that also included non-TORS-FFR procedures in their summary statistics without individual patient data were not included. In one case, authors reported problems with calculated mean length of hospital stay, and this data was excluded. Only five studies included HPV testing/p16 staining and seven studies were published prior to the 8th edition of the American Joint Committee on Cancer Staging, thus the 7th edition was used to stage all tumors [23].
Quality assessment
Two authors independently assessed the quality of the studies using the National Institute of Health Study Quality Assessment of Case Series Studies (Table 3). Nine following domains were assessed: objective, population characteristics, consecutiveness of cases, comparability of subjects, intervention, outcomes, length of follow-up, description of statistical methods and results. For included cohort studies, these were assessed for risk of bias using the Methodological Index for Non-Randomized Studies (MINORS) [24]. There are 12 items on this validated index, with each scored as 0 when not reported, 1 when reported but not adequate, and 2 when reported and adequate. Studies with composite scores of 0 to 4 are considered to be of very low quality, 5 to 8 as of low quality, 9 to 12 are of moderate quality, 13 to 18 are of high quality and 19 to 24 are of very high quality.
Results
Our search retrieved 617 publications with two records being identified through references of included studies. After eliminating duplicates, 442 publications were identified for further review. After screening of titles and abstracts, 66 studies were considered for possible inclusion. Of 65, 23 met the inclusion criteria (Table 1). Reasons for exclusion included ineligible study design, ineligible patient diagnosis, no free flap reconstruction, no use of TORS-FFR, or no extractable data on TORS-FFR. The screening process of the review is shown in Fig. 1 (PRISMA flow chart). The group of eligible studies consisted of 12 case series and case reports, 8 retrospective cohort studies, and 3 prospective cohort studies [9, 18,19,20, 25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42] (Table 1).
The number of participants per study ranged from one to 42 patients, with a mean age of 58.4 years. Most patients were males (57%) with squamous cell carcinoma pathology (93%). Melanoma, adenoid cystic carcinoma, spindle cell carcinoma and histiocytic carcinoma each contributed to less than 3% of cases. The most common tumour subsite was tonsil (47%), followed by base of tongue (22%) and soft palate (15%). When reported, the majority of tumours were p16 positive (91%). All studies reporting margin status post-operatively had negative margins.
The most frequent complication was infection (n = 15), of which three were reported as abscesses [9, 20, 30] (Table 2). Post-operative flap wound dehiscence, fistulas, and flap necrosis were other reported complications (Table 2). Two partial flap failures were not originally reported by the authors as perioperative complications but were added due to the need for a reoperation for partial flap debridement [20]. There was one aborted flap procedure which occurred when a patient with prior laryngectomy was found to have no carotid branches intraoperatively that were suitable for anastomosis, with the defect subsequently sealed using a myocutaneous pectoralis flap [20].
Transfusions of packed red blood cells occurred in three patients [9]. Separately from those transfused, three patients (1.9%) had post-operative bleeding events. Pharyngeal bleeds occurred in two patients, of which one required a cauterization procedure (Tables 2 and 4). One perioperative death occurred from a tracheostomy stoma hemorrhage 9 days postoperatively that led to cardiac arrest and anoxic brain injury [20].
The placement of perioperative tracheostomies was reported in 14 studies, 11 of which provided specific data [9, 19, 20, 26, 28, 29, 33, 35, 37, 40, 41] (Table 4). Among studies reporting pre-operative tracheostomy, there was a tracheostomy placement rate of 95.9% (n = 98). Two patients had tracheostomies prior to TORS-FFR surgery [20]. In one case, a tracheostomy was performed post-operatively for 1 day [19]. Nine studies provided the overall mean airway decannulation time of 16.7 days with a range of 1 to 171 days (n = 93) [9, 19, 20, 26, 33, 35, 37, 40, 41]. One patient was decannulated after 1 day due to post-operative placement for airway maintenance following ventilation weaning [19].
Feeding and oral tolerance outcomes were described in nine studies, with a mean time to first oral intake of 29.1 days (n = 52), with a range of 5 to 274 days [19, 20, 26, 28, 29, 33, 37, 40, 41]. G-tube dependence rates for TORS-FFR patients at one month was reported to be 23.1% (n = 39) at 1 month [9, 20, 26, 27, 29, 37] and 3.8% at 1 year post-operatively (n = 80) [9, 20, 26, 27, 29, 37].
Patient-reported outcomes were documented using validated questionnaires in three studies [30, 39, 40]. Tsai et al. scored swallowing, speech, and chewing impairment using the Functional Intraoral Glasgow Scale (FIGS) and demonstrated improved functional status of TORS-FFR patients at 1- and three 3 months post-operatively when compared to patients who had undergone open procedures [39]. Two studies utilized M.D. Anderson Dysphagia Inventory (MDADI) scoring to assess patient swallowing outcomes. Williamson et al. demonstrated no differences in global or emotional scoring of swallowing when comparing pre- and post-operative scores [40]. However, there was a slight improvement in functional and physical scores following surgical treatment [40]. Haymerle et al. demonstrated extremely low to moderate functioning swallowing outcomes for all 1, 3, and 12 months post-operatively.
The mean operating time of 710 min was derived from eight studies (n = 48), ranging from 144 to 1132 min [9, 19, 26, 27, 30, 36, 38, 41] (Table 4). Two studies measured robot-assisted anastomosis times [31, 32]. One study found venous micro-anastomosis took 34.5 min with eight stitches for the single patient included in this analysis, while the robot-assisted flap insetting time of 26 min [31]. The second study reported a single patient micro-anastomosis time of 45 min [32]. Margin status was reported in seven studies totalling 32 patients, all of which had negative margins [9, 19, 26, 33, 34, 36, 40]. Mean flap size reported in four studies was 55 cm2 (42 flaps, range 24–105 cm2) [19, 20, 28, 38].
The mean LOHS of 13.5 days (means of studies between 6.5 and 22 days) was determined from 8 studies (n = 48) (Table 4). In one case only two patient cases documented discharge times [26] and five case studies included data with non-TORS-FFR procedures that had to be excluded from analysis [18, 25, 31, 34, 38]. Intensive care duration preceding ward transfer was inconsistently noted.
According to the NIH Quality Assessment of Case Series Studies tool, most of the 13 case series studies met the nine domains. The criterion for description of statistical methods was not applicable to the case series or case reports. Few studies reported the length of follow-up. For cohort studies, one was considered high quality, five were of moderate quality, and two were of low quality. Studies that were assessed to be of low quality generally lacked or did not report adequate follow-up. The quality assessment of each included study can be found in Appendix B.
Discussion
This is the first systematic review to investigate the safety and outcomes of TORS-FFR for oropharyngeal cancer. As this technique becomes more popular amongst head and neck surgeons globally, it is important to recognize areas for improvement in order to deliver the best possible outcomes for oropharyngeal cancer survivors. Free-flap reconstruction after TORS may enable surgeons to resect more advanced stage tumors while avoiding a mandibulotomy in carefully selected patients, provide safe coverage of exposed vessels, reduce salivary fistulas, and provide excellent function. The benefits of TORS can, therefore, be combined with the advantages of microvascular reconstruction. Although limited by the lack of high-quality studies, this review provides an initial assessment of the quality and outcomes associated with this surgical approach.
With the popularization of robotic surgery and the steady rise of oropharyngeal cancer, more investigation into TORS and free flap reconstruction is warranted to validate this approach. Although our current results suggest the procedure is relatively safe, larger randomized controlled trials comparing TORS with free flap reconstruction to alternative treatment modalities should be undertaken to strengthen the evidence for its utility in treating oropharyngeal cancer.
When further examining reported complications, the rates of hematomas (1.9%) and fistulas (3.1%) [9, 39, 41] were slightly higher with TORS-FFR than the reported rates of 0.4% and 2.5%, respectively, compiled from a systematic review of patients undergoing TORS without free-flap reconstruction [43]. However, many studies describing TORS-FFR include patients with more advanced disease, limiting historical comparisons to TORS alone. Our review of TORS-FFR found that two partial flap failures were not originally reported by the authors as perioperative complications but were added due to the need for a reoperation for partial flap debridement [20]. The aborted flap procedure occurred when a patient with prior laryngectomy was found intraoperatively to have no carotid branches suitable for anastomosis, with the defect subsequently sealed using a myocutaneous pectoralis flap [20].
Few studies beyond those included in this analysis have specific data on functional outcomes of TORS-FFR procedures, requiring comparisons to the most similar procedures that are performed. A study by Al-Khudari et al. on functional outcomes from TORS procedures showed a 44.4% gastrostomy tube (G-tube) dependence rate at 1 year for 9 TORS-FFR patients [44]. The higher rate of G-tube dependence may be explained by the small sample size, five of the nine patients receiving salvage therapy, and that all patients in the study underwent post-operative adjuvant chemotherapy [44]. While not statistically validated, TORS-FFR appears to share similar outcomes as non-TORS free-flap reconstructions and TORS without free-flap reconstructions.
A retrospective chart review by Skoner et al. compiled 20 patients who underwent non-TORS surgical resection of oropharyngeal carcinomas. The surgical defects were covered with free-flap reconstruction and each patient was given adjuvant radiation of 62.6 Gy at 1.8–2.6 Gy daily fractions for 6 to 8 weeks [45]. At 4 months following surgery, the rate of G-tube dependence increased to 50% of the cohort with 40% of those tube-dependent patients having no oral intake whatsoever. These reported values are much higher than those in this current study. While we expect that the G-tube dependence rates to be higher in the Skoner et al. study given the higher-grade and higher incidence of base of tongue disease in their cohort, newer data still suggest that swallowing outcomes may be more optimal with TORS-FFR when compared to the lip-splitting mandibulotomy. However, limitations in patient anatomy, available technology, and surgeon experience must be considered when selecting between open and TORS-FFR approaches. We identified two studies that investigated the Performance Scale Status on TORS without free flap reconstruction which demonstrated a similar trend as TORS-FFR, with an initial decreased oral function 2–6 months after surgery [16, 46]. As one could expect due to the common sequalae of adjuvant therapy, one of these studies reported a statistically significant decline in function at 6 months between TORS without radiation versus TORS with radiation [46].
A single case of patient death was reported due to tracheostomy stoma hemorrhage 9 days post-operatively, which did not appear to be due to microvascular reconstruction. Deaths from post-operative hemorrhage during TORS surgery have been previously reported but are rare complications [43]. Our review showed a higher LOHS compared with earlier TORS-FFR case series’ by Mukhija et al. and Bonawitz et al. [19, 26]. This increased LOHS could be due to prophylactic placement of tracheostomy tubes, which occurred in only the earlier reports or from selection bias from earlier smaller case series. A case-matched controlled study from our institution found a significant reduction of 5.3 days in LOHS in TORS-FFR versus lip-splitting mandibulotomy, at 14.4 versus 19.7 days, respectively [9]. The mean LOHS is significantly longer than reported outcomes for TORS procedures without reconstruction of 2.9 days from 45 patients [43]. However, this prior systematic review focused on T1 and T2 stage tumours, whereas, given the nature of TORS-FF, our analysis includes patients with more advanced disease.
While this review is comprehensive, it is not without its limitations. A notable problem encountered in several studies was including TORS-FFR procedures for oral cancer subsites alongside oropharyngeal subsites. This required us to exclude 17 patients from the study [25, 31, 32]. It is unclear whether these procedures were in fact oropharyngeal subsites that also invaded the oral tongue or if they were erroneously included in studies due to sub-optimal translation. Several studies also included conventional procedures alongside TORS procedures. The heterogeneity and variety of both data collection and presentation methods from the studies evaluated in the manuscript made data gathering on outcomes challenging. While adding further case series and reports to current literature is suboptimal compared with the benefit of a well-designed randomized controlled trial or case–control analysis, authors of reports or series should adopt CARE guidelines to reduce heterogeneity and improve overall quality [47]. Individual supplemental data in any study format should be made available for each patient in terms of safety and functional outcomes, to enable more detailed analyses and increase the likelihood of inclusion in future reviews.
Conclusion
Transoral robotic surgery with free-flap reconstruction for oropharyngeal cancer is an advantageous surgical approach for select patients with oropharyngeal cancer. It is a safe procedure with relatively low rates of major complications. This surgical approach may be associated with decreased length of hospital stay compared to traditional open procedure; however, more studies are required to better characterize post-operative outcomes.
Data availability
Available from corresponding author upon request.
Abbreviations
- ALT:
-
Anterolateral thigh flap
- EBL:
-
Estimated blood loss
- HPV:
-
Human papillomavirus
- LOHS:
-
Length of hospital stay
- MSFF:
-
Medial sural artery free flap
- OPSCC:
-
Oropharyngeal squamous cell carcinoma
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
- RFFF:
-
Radial forearm free flap
- TORS:
-
Transoral robotic surgery
- TORS-FFR:
-
Transoral robotic surgery with free flap reconstruction
- UFF:
-
Ulnar artery perforator free flap
- VLFF:
-
Vastus lateralis free flap
- G-tube:
-
Gastrostomy Tube
References
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR (2020) Head and neck squamous cell carcinoma. Nat Rev Dis Primers 6(1):92. https://doi.org/10.1038/s41572-020-00224-3
Leemans CR, Snijders PJF, Brakenhoff RH (2018) The molecular landscape of head and neck cancer. Nat Rev Cancer 18(5):269–282. https://doi.org/10.1038/nrc.2018.11
Stein AP, Saha S, Kraninger JL, Swick AD, Yu M, Lambert PF et al (2015) Prevalence of human papillomavirus in oropharyngeal cancer: a systematic review. Cancer J 21(3):138–146. https://doi.org/10.1097/PPO.0000000000000115
Di Credico G, Polesel J, Dal Maso L, Pauli F, Torelli N, Luce D et al (2020) Alcohol drinking and head and neck cancer risk: the joint effect of intensity and duration. Br J Cancer 123(9):1456–1463. https://doi.org/10.1038/s41416-020-01031-z
Jiang X, Wu J, Wang J, Huang R (2019) Tobacco and oral squamous cell carcinoma: a review of carcinogenic pathways. Tob Induc Dis 17:29. https://doi.org/10.18332/tid/105844
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35. https://doi.org/10.1056/NEJMoa0912217
Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C (2015) Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol 33(29):3235–3242. https://doi.org/10.1200/JCO.2015.61.6995
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L et al (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720. https://doi.org/10.1093/jnci/92.9.709
Biron VL, O’Connell DA, Barber B, Clark JM, Andrews C, Jeffery CC et al (2017) Transoral robotic surgery with radial forearm free flap reconstruction: case control analysis. J Otolaryngol Head Neck Surg 46(1):20. https://doi.org/10.1186/s40463-017-0196-0
Elhalawani H, Mohamed ASR, Elgohari B, Lin TA, Sikora AG, Lai SY et al (2020) Tobacco exposure as a major modifier of oncologic outcomes in human papillomavirus (HPV) associated oropharyngeal squamous cell carcinoma. BMC Cancer 20(1):912. https://doi.org/10.1186/s12885-020-07427-7
Institute NC: Surveillance, epidemiology, and end results program website. (2022). Accessed November 2022
Sansoni ER, Gross ND (2015) The role of transoral robotic surgery in the management of oropharyngeal squamous cell carcinoma: a current review. Curr Oncol Rep 17(3):432. https://doi.org/10.1007/s11912-014-0432-y
Longfield EA, Holsinger FC, Selber JC (2012) Reconstruction after robotic head and neck surgery: when and why. J Reconstr Microsurg 28(7):445–450. https://doi.org/10.1055/s-0032-1306376
O’Malley BW Jr, Weinstein GS, Snyder W, Hockstein NG (2006) Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 116(8):1465–1472. https://doi.org/10.1097/01.mlg.0000227184.90514.1a
Chung TK, Rosenthal EL, Magnuson JS, Carroll WR (2015) Transoral robotic surgery for oropharyngeal and tongue cancer in the United States. Laryngoscope 125(1):140–145. https://doi.org/10.1002/lary.24870
Genden EM, Kotz T, Tong CC, Smith C, Sikora AG, Teng MS et al (2011) Transoral robotic resection and reconstruction for head and neck cancer. Laryngoscope 121(8):1668–1674. https://doi.org/10.1002/lary.21845
Lorincz BB, Jowett N, Knecht R (2016) Decision management in transoral robotic surgery: indications, individual patient selection, and role in the multidisciplinary treatment for head and neck cancer from a European perspective. Head Neck 38(Suppl 1):E2190–E2196. https://doi.org/10.1002/hed.24059
Selber JC (2010) Transoral robotic reconstruction of oropharyngeal defects: a case series. Plast Reconstr Surg 126(6):1978–1987. https://doi.org/10.1097/PRS.0b013e3181f448e3
Mukhija VK, Sung CK, Desai SC, Wanna G, Genden EM (2009) Transoral robotic assisted free flap reconstruction. Otolaryngol Head Neck Surg 140(1):124–125. https://doi.org/10.1016/j.otohns.2008.09.024
Hatten KM, Brody RM, Weinstein GS, Newman JG, Bur AM, Chalian AA et al (2018) Defining the role of free flaps for transoral robotic surgery. Ann Plast Surg 80(1):45–49. https://doi.org/10.1097/SAP.0000000000001263
Kao SS, Peters MD, Krishnan SG, Ooi EH (2016) Swallowing outcomes following primary surgical resection and primary free flap reconstruction for oral and oropharyngeal squamous cell carcinomas: a systematic review. Laryngoscope 126(7):1572–1580. https://doi.org/10.1002/lary.25894
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 67(2):93–9. https://doi.org/10.3322/caac.21388
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Arora R, Verma VK, Mishra KS, Bhoye H, Kapoor R (2018) Reconstruction with free flaps in robotic head-and-neck onco-surgeries. Indian J Plast Surg 51(3):283–289. https://doi.org/10.4103/ijps.IJPS_35_18
Bonawitz SC, Duvvuri U (2012) Robot-assisted oropharyngeal reconstruction with free tissue transfer. J Reconstr Microsurg 28(7):485–490. https://doi.org/10.1055/s-0032-1313758
Duvvuri U, Bonawitz SC, Kim S (2013) Robotic-assisted oropharyngeal reconstruction. J Robot Surg 7(1):9–14. https://doi.org/10.1007/s11701-011-0326-z
Garfein ES, Greaney PJ Jr, Easterlin B, Schiff B, Smith RV (2011) Transoral robotic reconstructive surgery reconstruction of a tongue base defect with a radial forearm flap. Plast Reconstr Surg 127(6):2352–2354. https://doi.org/10.1097/PRS.0b013e318213a0e4
Ghanem TA (2011) Transoral robotic-assisted microvascular reconstruction of the oropharynx. Laryngoscope 121(3):580–582. https://doi.org/10.1002/lary.21428
Haymerle G, Charters EK, Froggatt C, Wykes J, Palme CE, Clark JR (2021) Transoral robotic free flap inset in oropharyngeal cancer. Clin Otolaryngol 46(3):642–644. https://doi.org/10.1111/coa.13696
Lai CS, Chen IC, Liu SA, Lu CT, Yen JH, Song DY (2015) Robot-assisted free flap reconstruction of oropharyngeal cancer–a preliminary report. Ann Plast Surg 74(Suppl 2):S105–S108. https://doi.org/10.1097/SAP.0000000000000464
Lai CS, Lu CT, Liu SA, Tsai YC, Chen YW, Chen IC (2019) Robot-assisted microvascular anastomosis in head and neck free flap reconstruction: preliminary experiences and results. Microsurgery 39(8):715–720. https://doi.org/10.1002/micr.30458
Meccariello G, Montevecchi F, Sgarzani R, Vicini C (2018) Defect-oriented reconstruction after transoral robotic surgery for oropharyngeal cancer: a case series and review of the literature. Acta Otorhinolaryngol Ital 38(6):569–574. https://doi.org/10.14639/0392-100X-1473
Paleri V, Fox H, Coward S, Ragbir M, McQueen A, Ahmed O et al (2018) Transoral robotic surgery for residual and recurrent oropharyngeal cancers: exploratory study of surgical innovation using the IDEAL framework for early-phase surgical studies. Head Neck 40(3):512–525. https://doi.org/10.1002/hed.25032
Parhar HS, Brody RM, Shimunov D, Rajasekaran K, Rassekh CH, Basu D et al (2021) Retropharyngeal internal carotid artery management in TORS using microvascular reconstruction. Laryngoscope 131(3):E821–E827. https://doi.org/10.1002/lary.28876
Park YM, Lee WJ, Yun IS, Lee DW, Lew DH, Lee JM et al (2013) Free flap reconstruction after robot-assisted neck dissection via a modified face-lift or retroauricular approach. Ann Surg Oncol 20(3):891–898. https://doi.org/10.1245/s10434-012-2731-6
Qassemyar Q, Aguilar P, Temam S, Kolb F, Gorphe P (2017) The thin ALT perforator flap for oropharyngeal robotic-assisted reconstruction. Ann Chir Plast Esthet 62(1):1–7. https://doi.org/10.1016/j.anplas.2016.11.003
Song HG, Yun IS, Lee WJ, Lew DH, Rah DK (2013) Robot-assisted free flap in head and neck reconstruction. Arch Plast Surg 40(4):353–358. https://doi.org/10.5999/aps.2013.40.4.353
Tsai YC, Liu SA, Lai CS, Chen YW, Lu CT, Yen JH et al (2017) Functional outcomes and complications of robot-assisted free flap oropharyngeal reconstruction. Ann Plast Surg 78(3 Suppl 2):S76–S82. https://doi.org/10.1097/SAP.0000000000001010
Williamson A, Haywood M, Awad Z (2021) Feasibility of free flap reconstruction following salvage robotic-assisted resection of recurrent and residual oropharyngeal cancer in 3 patients. Ear Nose Throat J 100(10_suppl):1113S–8S. https://doi.org/10.1177/0145561320937627
Hans S, Jouffroy T, Veivers D, Hoffman C, Girod A, Badoual C et al (2013) Transoral robotic-assisted free flap reconstruction after radiation therapy in hypopharyngeal carcinoma: report of two cases. Eur Arch Otorhinolaryngol 270(8):2359–2364. https://doi.org/10.1007/s00405-013-2566-1
Sgarzani R, Meccariello G, Montevecchi F, Gessaroli M, Melandri D, Vicini C (2020) Transoral robotic surgery (TORS) for head and neck squamous cell carcinoma: healing by secondary intention, local flap or free flap. Eur J Plast Surg 43:123–128. https://doi.org/10.1007/s00238-019-01586-y
de Almeida JR, Byrd JK, Wu R, Stucken CL, Duvvuri U, Goldstein DP et al (2014) A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review. Laryngoscope 124(9):2096–2102. https://doi.org/10.1002/lary.24712
Al-Khudari S, Bendix S, Lindholm J, Simmerman E, Hall F, Ghanem T (2013) Gastrostomy tube use after transoral robotic surgery for oropharyngeal cancer. ISRN Otolaryngol. https://doi.org/10.1155/2013/190364
Skoner JM, Andersen PE, Cohen JI, Holland JJ, Hansen E, Wax MK (2003) Swallowing function and tracheotomy dependence after combined-modality treatment including free tissue transfer for advanced-stage oropharyngeal cancer. Laryngoscope 113(8):1294–1298. https://doi.org/10.1097/00005537-200308000-00005
Leonhardt FD, Quon H, Abrahao M, O’Malley BW Jr, Weinstein GS (2012) Transoral robotic surgery for oropharyngeal carcinoma and its impact on patient-reported quality of life and function. Head Neck 34(2):146–154. https://doi.org/10.1002/hed.21688
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D et al (2013) The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv Health Med 2(5):38–43. https://doi.org/10.7453/gahmj.2013.008
Acknowledgements
We are grateful for the assistance of Janice Kung, librarian, who assisted with creating the search strategy.
Funding
Dr. Vincent Biron has received funding for salary support from the Alberta Head and Neck Cancer for Oncology and Reconstruction Foundation.
Author information
Authors and Affiliations
Contributions
DM, JMP: final project design, data acquisition, analysis and interpretation, manuscript drafting, revisions, final approval, agreement to be accountable. SM: data acquisition, analysis and interpretation, manuscript drafting, revisions, final approval, agreement to be accountable. RK, JY: initial project design, data acquisition, manuscript drafting, final approval, agreement to be accountable. VLB: project design, analysis and interpretation, manuscript drafting, revisions, final approval, agreement to be accountable.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Monroe, D., Pyne, J.M., McLennan, S. et al. Characteristics and outcomes of transoral robotic surgery with free-flap reconstruction for oropharyngeal cancer: a systematic review. J Robotic Surg 17, 1287–1297 (2023). https://doi.org/10.1007/s11701-023-01572-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01572-4