Abstract
Background
The goal of any oncological therapy should be to achieve long-term disease-free survival while minimising acute and late toxicities. One of the goals of transoral robotic surgery (TORS) resection is to obtain negative margins around the primary tumour with minimal functional morbidity. The aim of this study was to assess the functional morbidity of TORS and evaluate the post-operative pain and functional outcomes 6 months after TORS for head and neck squamous cell carcinoma (SCC) in reconstructed and non-reconstructed patients.
Methods
We retrospectively reviewed 64 patients with head and neck SCCs resected by TORS from 2008 to December 2017 in our institution. The tumour localisation, pathologic T classification, defect size, reconstructive method, wound healing time, complications, post-operative pain and functional outcomes at 6 months were statistically evaluated (Table 1).
Results
Fifty-four resections healed by secondary intention, and 4 patients were reconstructed with a local flap and 6 with a free flap. No flap loss was encountered, while two cases of flap dehiscence that needed surgical revision and one case of partial necrosis were recorded. Eight patients had post-operative oral bleeding from the primary tumour resection field with an average bleeding time of 6.2 days. All bleeding occurred in patients with secondary healing of the defect after tumour excision, while no oral bleeding was recorded in patients with flap reconstructions. The pain scores in the first 3 post-operative days were 8 ± 1.2 for the secondary healing wounds and 6.2 ± 1.5 for the flap reconstructions. From day 4 to day 10, the mean VAS score was 5.7 ± 1.2 for the secondary healing wounds and 5.5 ± 1.2 for the flap reconstructions. The average wound healing time was 21.3 days in the secondary healing wound patients and 14.5 days in the reconstructed patients. At the 6-month follow-up, 63 out of the 64 patients recovered oral feeding and comprehensive locution, and only one patient experienced severe post-operative dysphagia and needed a permanent tracheostomy tube and percutaneous endoscopic gastrostomy (PEG) feeding.
Conclusion
In this retrospective study, the functional morbidity and complications of TORS for head and neck squamous cell carcinoma resection were favourable in reconstructed and non-reconstructed patients.
Level of Evidence: Level III, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of transoral robotic surgery (TORS) has led to a resurgence in the role of transoral surgery in the management of patients with head-neck squamous cell carcinomas (SCCs). The goal of any oncological therapy should be to achieve long-term disease-free survival while minimising acute and late toxicities. The oncologic efficacy of TORS is clear, and for select patients, the functional outcomes are outstanding. Moreover, one of the goals of TORS resection is to obtain negative margins around the primary tumour with minimal functional morbidity [1]. TORS was approved by the United States Food and Drug Administration for benign and malignant tumours classified as T1–T2 in 2009 [2]. The NCCN guidelines recognise transoral surgery as a potentially useful tool in the treatment of these select patients [1]. Nevertheless, the use of TORS for select locoregionally advanced patients (cT3 or cN2–3) may improve the oncologic control over that achieved with chemoradiotherapy (CRT) alone [1]. Furthermore, TORS may be a valuable method for the de-intensification of locoregionally advanced patients in at least three ways: decreasing the dose of radiotherapy (RT), obviating the need for chemotherapy and decreasing the radiotherapy target volume [1]. Furthermore, TORS may be a valid option for locating the primary tumour in unknown cases. Once the primary tumour site is identified, radiation therapy may be delivered to a defined volume of tissue instead of total mucosal irradiation as reported by international guidelines. This reduces morbidity by minimising unnecessary radiation to sensitive normal structures, such as the pharyngeal constrictors and salivary glands [3].
The aim of this study was to assess the functional morbidity of TORS and evaluate the post-operative pain and functional outcomes 6 months after TORS for head and neck SCC in reconstructed and non-reconstructed patients.
Materials and methods
In this study, we retrospectively evaluated the medical charts of patients with head-neck SCC treated with TORS between January 2008 and December 2017 at our department.
The clinicopathologic features of interest included age at surgery, comorbidity, sex, HPV status, pathologic T classification, tumour localisation, size of the defect, reconstruction method, eventual tracheostomy time, complications, post-operative pain in the first 10 days, wound healing time (reported by the patients who were admitted to the outpatient clinic weekly in the post-operative period), pre-operative versus 6 months post-operative swallowing function, aspiration and dependency on percutaneous endoscopic gastrostomy (PEG) at 6 months.
Post-operative local pain was evaluated daily with a visual analogue scale (VAS) in the first 10 post-operative days before the administration of pain killers. The surgical approach has previously been described [4,5,6].
The MD Anderson Dysphagia Inventory (MDADI) Questionnaire was administered pre-operatively and 6 months post-operatively to all patients to evaluate swallowing function.
Functional endoscopic evaluation of swallowing (FEES) was performed for all of the patients at 6 months to evaluate aspiration. The collected data for the present study were “presence of aspiration” or “no aspiration”.
Statistical analysis
To test the differences amongst groups, Fisher’s exact tests were used for categorical data, while Student’s t tests were used for continuous data. Probability values lower than 0.05 were considered statistically significant. All analyses were performed with Stata 12.1 software (Stata Corp., College Station, TX, USA).
Results
As of December 2017, 514 TORS procedures had been performed. In the same period, a total of 64 head and neck SCCs were treated with TORS alone or in combination with adjuvant RT or CRT based on the pathologic cancer staging results. All patients were treated with intent-to-cure. The primary tumour was classified as cT1 (22/64; 34.3%), cT2 (25/64; 39%), cT3 (8/64; 12.5%) and cTx (9/64; 14%). The primary tumour arose in the base of the tongue (BOT) in 26 patients (40.6%), tonsils in 28 patients (43.7%), soft palate in 2 patients (3.1%), posterior pharyngeal wall in 3 patients (4.6%) and supra glottis in 3 patients (4.6%). Unfortunately, in 2 patients classified as cTx, the primary tumour was not found.
The size of the defect ranged from 1.5 cm × 2 cm to 4 cm × 8 cm. The localisation of the defect, not the size, was the main factor that guided the choice in reconstruction, according to the algorithm of de Almeida et al. [7]: patients with exposure of the internal carotid artery and those who underwent soft palate resection or oropharyngeal sphincter resection. Nevertheless, the size of the defect in secondary healing wounds ranged from 1.5 cm × 2 cm to 3 cm × 3 cm, while flap reconstructions were performed to repair wounds that ranged from 3 cm × 3 cm to 4 cm × 8 cm.
The reconstructive method consisted predominantly of secondary intention healing (84.3%; 54/64), while 10 patients (15.6%) underwent flap reconstruction. Local flaps were performed in 4 T2 patients, while 6 free anterolateral thigh (ALT) flaps were performed in 6 T3 patients.
One facial artery myomucosal (FAMM) flap and one buccinator-based myomucosal (BMM) flap were used to cover extensive carotid exposure in two different patients with tonsillar cancer (T2). One temporalis myofascial (TMF) flap was adopted to restore a competent velopharyngeal sphincter and a watertight seal between the pharynx and neck in a case of OPSCC involving part of the soft palate and the anterior tonsillar pillar (T2). One infrahyoid flap was used to reconstruct a posterior defect at the base of the tongue (T2).
In 6 patients with extensive tumours at the BOT involving the tonsil and soft palate (T3), the surgical defect was reconstructed with an ALT free flap. ALT flaps were carefully tailored before being inset according to the standard template method of Caliceti et al. [4], and robotic arms were used to inset the flap in 5 cases.
Tracheostomy was performed routinely in the first series of patients (15 patients until 2012). As our experience increased, tracheostomy was reserved only for difficult intubation cases, cT3 tumours or patients that needed reconstruction with free flaps. The average duration of tracheostomy use was 7.4 days ± 2.6 days.
Complications
We did not register any major or life-threatening intra-operative or post-operative complications. Only one patient, who had concurrent neck dissection, experienced post-operative bleeding into the neck. Eight (12.5%) patients had oral post-operative bleeding from the tumour resection field, 5 patients from the tonsil and 3 from the BOT. The average oral bleeding time was 6.2 days ± 3.7 days. All incidences of oral bleeding occurred in defects that were treated with secondary healing of the defect. No oral bleeding was registered in the flap reconstruction patients. The difference was not statistically significant (p = 0.33).
No total local or free flap failures were registered, while two cases of flap dehiscence (1 FAMM and 1 ALT) needed surgical revision, and a partial necrosis of the TMF flap healed by secondary intention.
Post-operative pain
In the first 3 days, the mean VAS score was 8 ± 1.2 for the secondary healing wounds and 6.2 ± 1.5 for the flap reconstructions (p < 0.01). From day 4 to day 10, the mean VAS score was 5.7 ± 1.2 for the secondary healing wounds and 5.5 ± 1.2 for the flap reconstructions (p = 0.63).
Time to wound healing and swallowing function at 6 months
The mean time to complete wound healing was 21.3 days ± 10.4 days in the secondary healing patients and 14.5 days ± 7.7 days in the flap reconstruction patients, with a minimum of 9 days and a maximum of 22 days. The difference was statistically significant (p = 0.05).
Within the secondary healing group, the mean pre-operative and post-operative MDADI scores were 4.6 ± 7 and 4.8 ± 5.9, respectively. The flap reconstruction group had pre-operative and post-operative scores of 5 ± 6.8 and 4.9 ± 6.2, respectively. The impact on swallowing function, which was related to the MDADI score, was not significant between patients who underwent secondary healing and those who underwent flap reconstructions (p = 0.96).
FEES showed that only one patient presented clear aspiration and dysphagia and was dependent on PEG as well as a tracheostomy tube at 6 months. The patient underwent surgery due to a pT3N2b tumour at the BOT that invaded the tonsil and soft palate and underwent ALT reconstruction; this was the same patient who presented post-operative neck bleeding and ALT flap dehiscence that needed surgical revision.
Discussion
The oncologic outcomes of TORS are a matter of debate. Recently, Moore et al. [8] reported excellent outcomes with 1-year, 3-year and 5-year OS rates of 98%, 91% and 86% and DFS rates of 99%, 96% and 94%, respectively, and a local or regional disease-free survival rate of 95%.
In a systematic review of surgical and non-operative therapy data for oropharyngeal SCC, Yeh et al. [9] found that TORS can achieve oncologic outcomes that compare favourably to those of primary RT, with an improved toxicity profile. In that review, the OS after TORS-based therapy was reported to range from 81 to 100% and DFS was reported to range from 85.7 to 96%.
TORS was approved by the United States Food and Drug Administration for benign and malignant tumours classified as T1–T2 in 2009 [2]. The majority of robotic surgeons favour leaving the oropharyngeal defects to heal by secondary intention following TORS. In T1–T2 resection with secondary healing wounds, TORS is associated with lower morbidity rates, lower blood loss and a shorter hospitalisation time than open surgical procedures. Our group advocates for the use of narrow-band imaging to obtain free margins and to reduce over-resections, consequently minimising the risks of functional impairments [4,5,6].
Our results show that the functional results at 6 months are comparable between the reconstructed and the non-reconstructed patients. Secondary healing wounds are more painful in the first three post-operative days and present a higher bleeding risk than reconstruction flaps, but they heal within 3 weeks and do not cause any delay for eventual adjuvant therapies. In our series, flap reconstruction presents a higher risk of complications requiring re-intervention (20%) than secondary healing wounds; on the other hand, flap reconstruction is less painful, has lower bleeding risk and heals more quickly.
A limitation of the study is that the patients were admitted to the outpatient clinic weekly in the post-operative period, and they were asked to report their scores on the day of wound healing. In addition, the group with flap reconstructions had larger defects than the non-reconstructive group, which makes comparisons between the 2 groups difficult.
Amongst the existing classification schemes for oropharyngeal defects, the reconstructive algorithm developed by de Almeida et al. [7] seems to be easily applied in the robotic surgery framework. The author’s indications for flap reconstruction are patients with exposure of the internal carotid artery and those who underwent soft palate resection or oropharyngeal sphincter resection. In cases of class IV defects, we used the ALT shaped according to the standard template method of Caliceti et al. [4] (Fig. 1). Flap insetting is the most challenging phase due to severely restricted physical access and visualisation. However, in our experience, an accurately shaped and measured flap allows us to thoroughly perform a manual inset, although the robot can be used to suture parts of the flap in deeper and narrower spaces [10,11,12].
The modified skin paddle of the ALT flap according to Caliceti et al. [4]; the flap design is centred on the best perforator and has three shaped petals in order to reconstruct the following: (1) the rear side of the palate, (2) the front side of the palate and the tonsillar fossa and (3) the base of the tongue. After TORS resection, the correct size and shape of the free flap is a key to allowing insetting
Hatten et al. [13] recently reported his experience with free flap reconstructions for TORS and added prior radiation therapy to the indications for free tissue transfer. The authors propose a template-based reconstruction; furthermore, they propose an additional transcervical pharyngotomy to complete the cancer resection and to inset the flap without robotic arms [13].
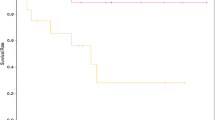
Regarding functional outcomes, Leonhardt et al. [14] demonstrated a decline in the eating, diet and speech domains from baseline to 6 months in the post-operative course, but these scores improved to the baseline levels for eating and diet at 12 months. Lee et al. [15] showed improved dysphagia scores between TORS and open mandibulotomy surgery for patients with T1–T3 tonsil SCC. Dziegielewski et al. [16] demonstrated a decline in all scores 3 weeks after surgery, with the lowest scores observed at 3 months in the post-operative course. Speech attitude, aesthetic, social and overall scores eventually returned to the baseline levels, but speech function and aesthetic scores only partially recovered and remained below the baseline scores at 12 months. In our series, the functional outcomes at 6 months post-operatively showed adequate MDADI and FEES scores both in patients with secondary healing wounds and in patients with flap reconstructions (Fig. 2). No aesthetic scoring and quality of life scoring systems were used.
Two studies included a comparison of quality of life (QOL) outcomes between TORS and RT. Moore et al. [17] found that the pre-operative and 3-month post-operative MDADI scores were similar between the two groups. However, by 6 months and 12 months post-operatively, patients treated with TORS and adjuvant therapy had significantly better MDADI scores than those treated with RT. In one of the largest prospective studies of patients undergoing TORS [18], post-operative dysphagia improved significantly more quickly in the TORS-only group than in patients who had adjuvant CRT. In summary, the TORS-only group had significantly better scores than the TORS + CRT group in the different QOL questionnaires. Similarly, Sethia et al. [19] showed that patients who underwent TORS alone had continued improvement in QOL in multiple domains shortly after surgery. These patients who underwent TORS alone reported higher QOL scores for eating 3 months and 6 months post-surgery than those who received adjuvant RT or CRT. The patients who underwent TORS alone or adjuvant RT reported less social disruption at 3 months than those who received adjuvant CRT, and patients who underwent TORS alone had higher speech scores at 3 months and 6 months than those who received adjuvant CRT and those who received adjuvant RT, respectively. Patients who received adjuvant CRT had lower overall QOL scores at baseline and 3 months, at 3 weeks and at 6 months than those who received adjuvant RT or underwent TORS alone, those who received adjuvant RT and those who underwent TORS alone, respectively.
Although many patients in this study underwent PEG, it is important to note that the total number of patients with PEG dependence greatly diminished from 3 to 12 months. Thus, the majority of patients underwent PEG prophylactically as recommended by their radiation oncologist or as a direct result of dysphagia due to adjuvant therapy. Regarding surgical complications, fistula formation was noted in the series from the Mayo Clinic in 6% of their cases. These patients underwent concurrent neck dissection at the time of TORS. In all four cases, the fistulae responded to treatment with daily packing and antibiotics [17, 20]. In our patients, no fistula formation was reported. Post-operative haemorrhage can be a life-threatening event in the case of TORS. Chia et al. [21] summarised the common complications in a 2013 multi-institutional survey of all TORS-trained surgeons in the USA. An electronic survey was sent to 300 TORS-trained surgeons. Forty-five surgeons responded to the survey and reported a post-operative haemorrhage rate of 3.1% requiring readmission. In total, 6 deaths occurred amongst 2015 procedures (0.3%). The other complications included temporary hypoglossal nerve injury (0.9%), lingual nerve injury (0.6%) and tooth injury (1.4%).
A limitation of the study is the number of reconstructed patients. Further data need to be collected prospectively to increase the level of evidence.
Final remarks
In conclusion, in this retrospective study, the functional morbidity and complications of TORS for head and neck squamous cell carcinoma resection were favourable in reconstructed and non-reconstructed patients. Flap reconstruction extends the benefits of TORS to patients with exposure of the internal carotid artery and those who underwent soft palate resection or oropharyngeal sphincter resection.
References
Ward MC, Koyfman SA (2016) Transoral robotic surgery: the radiation oncologist’s perspective. Oral Oncol 60:96–102
FDA 510(k) summary; 2009; http://www.accessdata.fda.gov/cdrh_docs/pdf9/K090993.pdf [accessed November 18, 2015]
Meccariello G, Cammaroto G, Ofo E, Calpona S, Parisi E, D'Agostino G, Gobbi R, Firinu E, Bellini C, de Vito A, Montevecchi F, Costantini M, Amadori E, Nuzzo S, Pelucchi S, Vicini C (2019) The emerging role of trans-oral robotic surgery for the detection of the primary tumour site in patients with head-neck unknown primary cancers: a meta-analysis. Auris Nasus Larynx 46(5):663–671
Caliceti U, Piccin O, Sgarzani R, Negosanti L, Fernandez IJ, Nebiaj A, Contedini F, Cipriani R, Ceroni AR (2013) Surgical strategies based on standard templates for microsurgical reconstruction of oral cavity and oropharynx soft tissue: a 20 years’ experience. Microsurgery. 33(2):90–104
Vicini C, Montevecchi F, D’Agostino G, DE Vito A, Meccariello G (2015) A novel approach emphasising intra-operative superficial margin enhancement of head-neck tumours with narrow-band imaging in transoral robotic surgery. Acta Otorhinolaryngol Ital 35(3):157–161
De Vito A, Meccariello G, Vicini C (2017) Narrow band imaging as screening test for early detection of laryngeal cancer: a prospective study. Clin Otolaryngol 42(2):347–353
de Almeida JR, Park RCW, Villanueva NL, Miles BA, Teng MS, Genden EM (2014) Reconstructive algorithm and classification system for transoral oropharyngeal defects. Head Neck 36:934–941
Moore EJ, Van Abel KM, Price DL, Lohse CM, Olsen KD, Jackson RS, Martin EJ (2018) Transoral robotic surgery for oropharyngeal carcinoma: surgical margins and oncologic outcomes. Head Neck. https://doi.org/10.1002/hed.25055
Yeh DH, Tam S, Fung K, MacNeil SD, Yoo J, Winquist E, Palma DA, Nichols AC (2015) Transoral robotic surgery vs. radiotherapy for management of oropharyngeal squamous cell carcinoma—a systematic review of the literature. Eur J Surg Oncol 41(12):1603–1614
Meccariello G, Montevecchi F, D’Agostino G et al (2019) Trans-oral robotic surgery for the management of oropharyngeal carcinomas: a 9-year institutional experience. Acta Otorhinolaryngol Ital 39(2):75–83
Meccariello G, Montevecchi F, Sgarzani R, Vicini C (2018) Defect-oriented reconstruction after transoral robotic surgery for oropharyngeal cancer: a case series and review of the literature. Acta Otorhinolaryngol Ital 38(6):569–574
Meccariello G, Montevecchi F, Sgarzani R, De Vito A, D’Agostino G, Gobbi R, Bellini C, Vicini C (2017) The reconstructive options for oropharyngeal defects in the transoral robotic surgery framework. Oral Oncol 66:108–111
Hatten KM, Brody RM, Weinstein GS, Newman JG, Bur AM, Chalian AA, O’Malley BW Jr, Rassekh CH, Cannady SB (2018) Defining the role of free flaps for transoral robotic surgery. Ann Plast Surg 80(1):45–49
Leonhardt FD, Quon H, Abrahao M, O’Malley BW, Weinstein GS (2012) Transoral robotic surgery for oropharyngeal carcinoma and its impact on patient-reported quality of life and function. Head Neck 34(2):146–154
Lee SY, Park YM, Byeon HK, Choi EC, Kim S-H (2014) Comparison of oncologic and functional outcomes after transoral robotic lateral oropharyngectomy versus conventional surgery for T1 to T3 tonsillar cancer. Head Neck 36(8):1138–1145
Dziegielewski PT, Teknos TN, Durmus K et al (2013) Transoral robotic surgery for oropharyngeal cancer. JAMA Otolaryngol Neck Surg 139(11):1099
Moore EJ, Olsen KD, Kasperbauer JL (2009) Transoral robotic surgery for oropharyngeal squamous cell carcinoma: a prospective study of feasibility and functional outcomes. Laryngoscope 119:2156–2164
Achim V, Bolognone RK, Palmer AD, Graville DJ, Light TJ, Li R, Gross N, Andersen PE, Clayburgh D (2017) Long-term functional and quality-of-life outcomes after transoral robotic surgery in patients with oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg. https://doi.org/10.1001/jamaoto.2017.1790
Sethia R, Yumusakhuylu AC, Ozbay I, Diavolitsis V, Brown NV, Zhao S, Wei L, Old M, Agrawal A, Teknos TN, Ozer E (2018) Quality of life outcomes of transoral robotic surgery with or without adjuvant therapy for oropharyngeal cancer. Laryngoscope 128(2):403–411
Moore EJ, Olsen SM, Laborde RR, García JJ, Walsh FJ, Price DL, Janus JR, Kasperbauer JL, Olsen KD (2012) Long-term functional and oncologic results of transoral robotic surgery for oropharyngeal squamous cell carcinoma. Mayo Clin Proc 87(3):219–225
Chia SH, Gross ND, Richmon JD (2013) Surgeon experience and complications with transoral robotic surgery (TORS). Otolaryngol Head Neck Surg 149(6):885–892
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rossella Sgarzani, Giuseppe Meccariello, Filippo Montevecchi, Manlio Gessaroli, Davide Melandri and Claudio Vicini declare that they have no conflict of interest.
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sgarzani, R., Meccariello, G., Montevecchi, F. et al. Transoral robotic surgery (TORS) for head and neck squamous cell carcinoma: healing by secondary intention, local flap or free flap. Eur J Plast Surg 43, 123–128 (2020). https://doi.org/10.1007/s00238-019-01586-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-019-01586-y