Abstract
Technical surgical skills are said to be acquired quicker on a robotic rather than laparoscopic platform. However, research examining this proposition is scarce. Thus, this study aimed to compare the performance and learning curves of novices acquiring skills using a robotic or laparoscopic system, and to examine if any learning advantages were maintained over time and transferred to more difficult and stressful tasks. Forty novice participants were randomly assigned to either a robotic- or laparoscopic-trained group. Following one baseline trial on a ball pick-and-drop task, participants performed 50 learning trials. Participants then completed an immediate retention trial and a transfer trial on a two-instrument rope-threading task. One month later, participants performed a delayed retention trial and a stressful multi-tasking trial. The results revealed that the robotic-trained group completed the ball pick-and-drop task more quickly and accurately than the laparoscopic-trained group across baseline, immediate retention, and delayed retention trials. Furthermore, the robotic-trained group displayed a shorter learning curve for accuracy. The robotic-trained group also performed the more complex rope-threading and stressful multi-tasking transfer trials better. Finally, in the multi-tasking trial, the robotic-trained group made fewer tone counting errors. The results highlight the benefits of using robotic technology for the acquisition of technical surgical skills.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Robotic systems such as the da Vinci surgical system (Intuitive Surgical Inc., Sunny Vale, California) are now used in over 1,000 hospitals across the USA [1]. Robotic technology is proposed to offer benefits to both the patient, including reduced post-operative pain and shorter stays in hospital [2], and the surgeon, including a more comfortable and ergonomic operating position, a high resolution three-dimensional field of view, and improved dexterity due to 6 degrees of freedom, motion scaling, and tremor filtering. These technological advances have been proposed to shorten the learning curve of technical surgical skills, an important benefit given the relatively extensive learning period required to acquire these skills using laparoscopic platforms [3]. However, to date, research exploring this proposition has been limited.
Only a handful of studies have examined the learning curves (the number of repetitions required to reach a certain level of proficiency when completing a specific task [4] ) of surgeons with considerable laparoscopic experience and no prior robotic experience. These studies have revealed mixed results [5–7]. For example, Hernandez and colleagues found that surgeons displayed a short learning curve and rapid improvement in performance when acquiring a new surgical skill using a robotic system [8]. In contrast, Heemskerk et al. [9] revealed a relatively flat learning curve and limited improvement in performance when surgeons performed multiple dexterity tasks with a robotic platform. However, it should be noted that the surgeons in this study performed the tasks more quickly and accurately using a robotic rather than laparoscopic system [9]. Thus, because the learning curve was calculated as the difference between the first and final trial, the flat learning curve is likely due to a floor effect caused by the surgeons performing better in the initial trial on the robotic system than the laparoscopic system.
Even less research has investigated the learning curves of novices with no prior surgical experience [4, 10]. This limited research has shown that novices can reach a higher level of proficiency quicker using a robotic rather than laparoscopic system. For example, Stefanidis et al. [11] found that medical students displayed better performance and a shorter learning curve on intracorporeal suturing on a robotic versus laparoscopic platform. However, a major limitation of this research is that only a small number of trials were employed (3–5 trials), meaning that only the beginning of the learning curve was assessed with no plateau in performance occurring. Additional limitations to this research include the failure to examine if any learning advantages accompanying the robotic device remained over an extended period of time via delayed retention trials. Moreover, studies have failed to employ transfer trials to identify if any performance benefits transferred to different and more difficult tasks or stressful conditions similar to those encountered in the operating room. Indeed, these are important criteria when assessing the effectiveness of learning and have been employed in previous laparoscopic training research [12–14].
Given the aforementioned knowledge gaps, the current study aimed to (1) compare the performance and learning curves of novice surgeons acquiring technical surgical skills using either a robotic or laparoscopic system and (2) investigate if any learning advantages were maintained over time and transferred to more difficult and stressful tasks. We predicted that novices using the robotic system would perform the task more quickly and accurately (i.e., fewer errors) during baseline, retention (immediate and delayed), and transfer (more difficult task and stressful multi-tasking conditions) trials compared to those using the laparoscopic system. Additionally, we predicted that the learning curves (i.e., number of trials) to reach the proficiency displayed in the immediate retention trial would be significantly shorter (for both completion time and number of errors) for the novices who acquired technical skills using the robotic system than those using the laparoscopic system.
Materials and methods
Participants
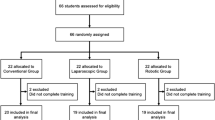
Forty participants (22 male, 18 female; mean age = 25.27 years; SD = 3.23) volunteered to take part in the study. All participants had no prior robotic or laparoscopic surgery experience and were thus considered novices (as [14]). Thirty-eight participants were right-hand dominant and two participants were left-hand dominant. Institutional ethical approval was gained prior to initiation of the study and all participants provided written informed consent prior to their first individual testing session.
Surgical systems and tasks
A da Vinci Si robotic system (Intuitive Surgical Ltd.) was employed throughout the study. This system had two main components: the control and viewing console and a moveable cart with three articulated robot arms. Participants sat in front of the console and viewed an enlarged three-dimensional image of the task while manipulating handles that controlled the robotic arms. An endoscope was attached to one of these arms, while laparoscopic tools were attached to the other two arms. A 3-Dmed (3-Dmed, Franklin, OH) standard minimally invasive laparoscopic training system with a joystick SimScope (a maneuverable webcam) was also used. Participants viewed the scene inside the training box on a monitor (via a webcam) and moved objects inside the box using surgical tools that were inserted through ports. Importantly, while predominately a training tool, this 3-Dmed laparoscopic system effectively mimics the ergonomic and perceptual difficulties associated with the laparoscopic techniques used in the operating room [12].
The participants performed two tasks at various points throughout the study on either the robotic or laparoscopic system. For the majority of the study, participants performed a ball pick-and-drop task in which they had to move six foam balls from stems of varying heights into a cup, using a single tool (with their dominant hand). The balls had to be grasped and dropped into the cup individually and in a pre-specified order. The participants were told to complete this task as quickly and as accurately (i.e., no dropped balls) as possible (as [14]). Additionally, the participants completed a rope-threading task in which they had to pass a rope through a succession of seven pre-specified metal hoops to create a P configuration, using two tools (with their dominant and non-dominant hands). The participants were asked to perform this task as quickly as possible (as [5]).
Procedure
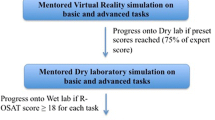
The participants were randomly assigned to one of two groups (robotic or laparoscopic trained) before being shown by the experimenter how their system worked and having one min to familiarize themselves with their system (this was standardized across all participants). They were then given some standardized instructions regarding the ball pick-and-drop surgical task that was taken from the fundamentals of laparoscopy curriculum [15]. Following a single baseline trial on the ball pick-and-drop task, participants performed 50 learning trials. These learning trials were divided into ten blocks of five trials and participants were given a few minutes break in between each block. Immediately after the learning trials, participants completed a retention trial on the ball pick-and-drop task and a transfer trial on the more difficult two-instrument rope-threading task. Approximately 1 month after the learning trials (mean = 30.85 days; SD = 3.50), participants performed a delayed retention trial on the ball pick-and-drop task and a stressful multi-tasking transfer trial during which participants completed a single trial on the ball pick-and-drop task while completing a secondary tone counting task. This task required participants to listen for a target sound (bell ring), count the number of times it was played, and ignore three other distracting sounds (buzzer, ping, and tone). The sounds were played to the participants in a randomized order using a laptop installed with Lab view software (National Instruments Inc.). Each participant was played the sounds for 30 s for familiarization purposes (as [12]).
Measures
Surgical task and tone counting performance
Performance on the ball pick-and-drop task was assessed in terms of both the time taken to complete each trial and the number of errors made during each trial (i.e., the number of balls dropped and/or knocked off) (as [14]). Furthermore, performance on the rope-threading task was measured by the time taken to complete the task (i.e., form the P configuration) (as [5]). The number of repetitions or trials taken to reach the proficiency level demonstrated at immediate retention was used to examine both groups’ learning curves for completion time and number of errors. Finally, tone counting performance was assessed by calculating an error score, by subtracting the actual number of target tones played during the task from participants’ estimate of the number of target tones played (as [12]).
Statistical analyses
A series of 2 (Group: robotic trained vs. laparoscopic trained) × 3 (Trial: baseline, immediate retention, delayed retention) mixed design ANOVAs with follow-up LSD t tests were conducted on the completion time and number of errors data. Furthermore, to compare differences between the groups, a series of independent t tests were conducted on the number of trials taken to reach proficiency for both completion time and number of errors (i.e., learning curves), the time taken to complete the more difficult complex transfer trial, and the completion time, number of errors, and tone counting performance data from the multi-tasking transfer trial. Partial eta squared (η 2p ) and Cohen’s d were employed to calculate effect sizes for omnibus and simple comparisons, respectively.
Results
Completion time
The 2 (Group) × 3 (Trial) ANOVA yielded significant main effects for Group (F(1, 38) = 8.37, p = 0.006, η 2p = 0.18) and Trial (F(2, 76) = 141.11, p < 0.001, η 2p = 0.79), but there was no significant interaction effect (F(2, 76) = 1.31, p = 0.275, η 2p = 0.03). Follow-up analyses revealed that the robotic-trained group completed the task significantly quicker than the laparoscopic-trained group across all trials (26.03 s vs. 36.38 s; p = 0.006). Moreover, both groups performed the task significantly quicker during the immediate retention trial than the baseline trial (15.96 vs. 52.76 s; p < 0.001), but significantly slower in the delayed retention trial compared to the immediate retention trial (24.89 vs. 15.96 s; p < 0.001). The completion time data are presented Fig. 1.
Number of errors
The 2 (Group) × 3 (Trial) ANOVA revealed significant main effects for Group (F(1, 38) = 25.60, p < 0.001, η 2p = 0.40), and Trial (F(2, 76) = 6.71, p = 0.002, η 2p = 0.15), but there was no significant interaction effect (F(2, 76) = 1.11, p = 0.336, η 2p = 0.03). Follow-up analyses revealed that the robotic-trained group made significantly fewer errors during the task than the laparoscopic-trained group across all trials (0.38 vs. 1.18; p < 0.001). Moreover, both groups made significantly fewer errors during the task in the immediate retention trial than the baseline trial (0.60 vs. 1.23; p = 0.016), but there was no significant difference in the number of errors made in the delayed retention trial compared to the immediate retention trial (0.53 vs. 0.60; p = 0.632). The error data are presented in Fig. 2.
Number of trials to proficiency
An independent t test revealed no significant difference between the robotic and laparoscopic-trained groups in terms of the number of trials performed to reach the completion time achieved during the immediate retention trial (34.40 vs. 30.40 trials; t(38) = −1.06, p = 0.295, d = 0.34). However, this analysis did reveal that the robotic-trained group performed significantly fewer trials to attain the accuracy level (i.e., number of errors) they exhibited during the immediate retention trial compared to the laparoscopic-trained group (1.80 vs. 4.20 trials; t(38) = 2.10, p = 0.043, d = 0.68). The learning curves for completion time and number of errors are displayed in Figs. 3 and 4, respectively.
Transfer, multi-tasking, and tone counting performance
Independent t tests revealed that the robotic-trained group was significantly quicker in completing the more difficult rope-threading task (90.95 vs. 205.18 s; t(38) = 3.55, p = 0.001, d = 1.15) and the multi-tasking trial (21.23 vs. 27.88 s; t(38) = 3.02, p = 0.004, d = 0.98) than the laparoscopic-trained group. They also performed marginally more accurately on the multi-tasking trial (0.35 vs. 0.90 errors; t(38) = 1.89, p = 0.067, d = 0.61) and made significantly fewer errors on the secondary tone counting task (0.00 vs. −1.05; t(38) = −2.17, p = 0.036, d = 0.70) compared to the laparoscopic-trained group.
Discussion
By offering better depth perception due to a high resolution three-dimensional field of view and improved dexterity due to 6 degrees of freedom, motion scaling, and tremor filtering, robotic technology addresses many of the limitations inherent in laparoscopy [4]. Subsequently, it has been suggested that the learning curve is likely to be much shorter when technical surgical skills are acquired using a robotic rather than laparoscopic system. However, to date, research examining this proposition has been scarce, with studies only employing a small number of trials (3–5 trials) and failing to use retention and transfer trials that are crucial in assessing skill acquisition and learning effectiveness. Thus, the aim of the current study was to address these issues and to compare the performance and learning curves of novices acquiring technical surgical skills using either a robotic or laparoscopic system. Furthermore, the present study aimed to investigate if any learning advantages were maintained over time and transferred to more difficult and stressful tasks that more closely replicate the demands inherent in the operating room.
The robotic-trained group performed the baseline trial more quickly and accurately (with fewer errors) than the laparoscopic-trained group, supporting previous research showing that novices can complete surgical tasks more proficiently on robotic rather than laparoscopic platforms [16–18]. Importantly, while both groups improved their performance over the learning period, the robotic-trained group maintained this performance advantage in an immediate retention test, suggesting that this group had reached a higher level of technical proficiency at the end of the learning period compared to the laparoscopic-trained group (see Figs. 1, 2). Although the learning curves for completion time were similar for both groups, with each group reaching a plateau in their performance after approximately 30 trials (block 7; Fig. 3), the learning curves for accuracy revealed an advantage for the robotic system. Specifically, the learning curve was shorter for the robotic-trained group than the laparoscopic-trained group , with the former achieving an error rate comparable to immediate retention after only two trials. Collectively, these results extend previous research [4, 10, 11], and offer support to the notion that novices can reach higher levels of proficiency quicker using robotic rather than laparoscopic systems. However, it should be noted that these results offer only limited support for this notion, as the learning curves of the groups were not substantially different (see Figs. 3, 4). This is likely due to a floor effect caused by the robotic-trained groups’ superior performance in the baseline trial, leaving them less ‘room’ for improvement. To overcome this issue, future research should examine learning curves by investigating the number of trials it takes to reach a set level of proficiency (e.g., a completion time of 30 s in the ball pick-and-drop task).
As temporary factors such as feedback, motivation, boredom, and fatigue can all influence performance, it is important to establish whether any improvements after a period of learning are relatively permanent [19]. This can be examined using delayed retention trials that are designed to allow a particular time interval to elapse after learning and can therefore reliably detect the stability of skill acquisition and effectiveness of learning [19]. In the present study, the robotic-trained group maintained their learning advantage over the laparoscopic-trained group, and completed the surgical task quicker and more accurately (fewer errors) in a delayed retention trial, 1 month after the learning period. The current study therefore extends previous research that only focused on the beginning of the learning curve [4, 10, 11] and suggests that the performance benefits associated with the robotic device are relatively permanent over time. However, it should be noted that while both groups maintained their accuracy in the delayed retention trial at immediate retention levels, both groups experienced some decay in their completion times, performing the task more slowly in the delayed retention trial compared to the immediate retention trial. Thus, the results imply that ‘top-up’ training sessions might be necessary in robotic training programs.
Another key step in assessing the effectiveness of skill acquisition is to examine the degree to which improvements in performance translate to different and more difficult tasks [14]. In the present study, both groups performed one transfer trial on a two-instrument rope-threading task, with the robotic-trained group able to complete the task in less than half the time it took the laparoscopic-trained group. This finding extends previous research [4, 10, 11] and confirms that the robotic-trained group acquired technical surgical skills to a higher level of proficiency. However, it is important to note that while the rope-threading task was more difficult than the ball pick-and-drop, it cannot be considered reflective of a real surgical procedure. While this is a limitation of the present study, it is likely that the benefits of the robotic system would have been exaggerated further had a more complex transfer task been employed (e.g., intracorporeal suturing).When examining how well skills have been acquired, it is also important to investigate if any improvements in performance transfer to stressful tasks that are more representative of the operating room [14]. Thus, in the current study, both groups completed one transfer trial in which they were required to perform a ball pick-and-drop task while performing a concurrent tone counting task. Importantly, as well as performing the surgical task more quickly and accurately, the robotic-trained group made fewer tone counting errors than the laparoscopic-trained group. This finding is interesting and suggests that the robotic-trained group were at a higher stage of learning, performing the task with greater automaticity and with more spare attentional resources than the laparoscopic-trained group [20].
Taken together, the findings of the present study have a number of important implications. Specifically, the faster and more robust skill acquisition demonstrated by the robotic-trained group should translate into shorter training durations as trainees can move onto acquiring other important skills (decision-making, communication etc.) sooner once they have mastered the technical surgical skills. This truncated learning curve might also lead to substantial cost savings that offset the higher recruitment and operational costs associated with the robotic system [21]. Although robotic training programs are rare due to issues regarding access to robotic systems, the results of the current study suggest that such programs might lead to the acquisition of technical surgical skills that can be maintained over time and under stressful multi-tasking conditions. This is an important finding given the important influence stress can have on surgical performance [22], and the frequency with which surgeons have to deal with auditory distractions in the operating room [23].
To conclude, the results of the present study highlight the benefits of using robotic technology for the acquisition of technical surgical skills. The novice participants were able to perform the surgical task more quickly and accurately using the robotic platform as well as showing transferability of surgical skills to a different and more difficult task. This learning advantage was also maintained over an extended period of time and while performing a surgical task under stressful multi-tasking conditions. Importantly, the expedited acquisition of technical surgical skills might lead to shorter training durations and thus reduced training costs relative to training laparoscopic skills.
References
Dulan G, Rege RV, Hogg DC, Gilbery-Fisher KM, Arain NA, Tesfay ST, Scott DJ (2012) Proficiency-based training for robotic surgery: construct validity workload and expert levels for nine inanimate exercises. Surg Endosc 26:1516–1521. doi:10.1007/s00464-011-2102-6
Reyes DA, Tang B, Cuschieri A (2006) Minimal access surgery (MAS)-related surgeon morbidity syndromes. Surg Endosc 20:1–13. doi:10.1007/s00464-005-0315-2
Smith CD, Farrell TM, McNatt SS, Metrevel RM (2001) Assessing laparoscopic manipulative skills. Am J Surg 181:547–550. doi:10.1016/S0002-9610(01)00639-0
Anderberg M, Larsson J, Kockum CC, Arnbjornsson E (2010) Robotics versus laparoscopy—an experimental study of the transfer effects in maiden users. Ann Surg Innov Res 4:3–9. doi:10.1186//1750-1164-4-3
Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Adult Urol 60:39–45. doi:10.1016/S0090-4295(02)01717-X
Chang L, Satava RM, Pellegrini CA, Sinanan MN (2003) Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc 17:1744–1748. doi:10.1007/s00464-003-8813-6
Sumi Y, Dhumane PW, Komeda K, Dallemagne B, Kuroda D, Marescaux J (2013) Learning curves in expert and non-expert laparoscopic surgeons for robotic suturing with the da Vinci® surgical system. J Robotic Surg 7:29–34. doi:10.1007/s11701-012-0336-5
Hernandez JD, Bann SD, Munz Y, Moorthy K, Datta V, Martin S et al (2004) Qualitative and quantitative analysis of the learning curve of a simulated surgical task on the da Vinci system. Surg Endosc 18:372–378. doi:10.1007/s00464-003-9047-3
Heemskerk J, van Gemert WG, de Vries J, Greve JW, Bouvy ND (2007) Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robot-assisted laparoscopic tasks compared with conventional laparoscopic tasks in experienced users. Surg Laparosc Endosc Percutan Tech 17:171–174. doi:10.1097/SLE.0b013e31805b8346
Narazaki K, Oleynikov D, Stergiou N (2006) Robotic surgery training and performance: identifying objective variables for quantifying the extent of proficiency. Surg Endosc 20:96–103. doi:10.1007/s00464-005-3011-3
Stefanidis D, Wang F, KorndorfferJr JR, Dunne JB, Scott DJ (2010) Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 24:377–382. doi:10.1007/s00464-009-0578-0
Wilson MR, Vine SJ, Bright E, Masters RSW, Defriend D, McGrath JS (2011) Gaze training enhances laparoscopic technical skill acquisition and multi-tasking performance: a randomized, controlled study. Surg Endosc 25:3731–3739. doi:10.1007/s00464-011-1802-2
Vine SJ, Masters RSW, McGrath JS, Bright E, Wilson MR (2012) Cheating experience: guiding novices to adopt the gaze strategies of experts expedites the learning of technical laparoscopic skills. Surgery 152:32–40. doi:10.1016/j.surg.2012.02.002
Vine SJ, Chaytor RJ, McGrath JS, Masters RSW, Wilson MR (2013) Gaze training improves the retention and transfer of laparoscopic technical skills in novices. Surg Endosc 27:3205–3213. doi:10.1007/s00464-013-2893-8
Ritter EM, Scott DS (2007) Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov 14:107–112. doi:10.1177/1553350607302329
Hubens G, Coveliers H, Balliu L, Ruppert M, Vaneerdeweg W (2003) A performance study comparing manual and robotically assisted laparoscopic surgery using the da Vinci system. Surg Endosc 17:1595–1599. doi:10.1007/s00464-002-9248-1
Blavier A, Gaudissart Q, Cadiere GB, Nyssen AS (2007) Perceptual and instrumental impacts of robotic laparoscopy on surgical performance. Surg Endosc 21:1875–1882. doi:10.1007/s00464-007-9342-5
Chandra V, Nehra D, Parent R, Woo R, Reyes R, Hernandez-Boussard T et al (2010) A comparison of laparoscopic and robotic assisted suturing performance by experts and novices. Surgery 147:830–839. doi:10.1016/j.surg.2009.11.002
Arthur W Jr, Bennet W Jr, Stanush PL, McNelly TL (1998) Factors that influence skill decay and retention: a quantitative review and analysis. Hum Perform 11:57–101. doi:10.1207/s15327043hup1101_3
Fitts PM, Posner MI (1967) Human performance. Belmont, CA
Dimitrios S, William WH, James RKJ, Sarah M, Daniel RS (2010) Initial laparoscopic basic skills training shortens the learning curve of laparoscopic suturing and is cost-effective. J Am Coll Surg 210:436–440
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147:318–330. doi:10.1016/j.surg.2009.10.007
Healey AN, Sevdalis N, Vincent CA (2006) Measuring intraoperativeinterference from distraction and interruption observed in the operating theatre. Ergonomics 49:589–604
Conflict of interest
This research was funded by Intuitive Surgical Ltd. through their, ‘Surgical Clinical Robotics Research Grant’ scheme. However, Intuitive Surgical Ltd. had no involvement in the design and execution of the research, or in the analysis or interpretation of the data presented. Therefore, Mr Lee Moore, Ms Elizabeth Waine, Dr Mark Wilson, Dr Rich Masters, Mr John McGrath, and Dr Samuel Vine have no conflicts of interest or financial ties to disclose.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moore, L.J., Wilson, M.R., Waine, E. et al. Robotic technology results in faster and more robust surgical skill acquisition than traditional laparoscopy. J Robotic Surg 9, 67–73 (2015). https://doi.org/10.1007/s11701-014-0493-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-014-0493-9