Abstract
Purpose
Sleeve gastrectomy (SG) is a common bariatric procedure that has been shown to be effective in both the short and long term, but it is not without risks, some of which necessitate revision or redo surgery (RS).
Materials and Methods
GBSR (German Bariatric Surgery Registry) data were evaluated in this multicenter analysis. Short-term results (1-year follow-up) of RS (Re-Sleeve gastrectomy, Roux-en-Y gastric bypass, RYGB, Omega-loop gastric bypass, OLGB, and duodenal switch, DS) following primary SG (n = 27939) were evaluated.
Results
Of PSG patients, 7.9% (n=2195) needed revision surgery. Nine hundred ninety-four patients underwent the aforementioned four surgical procedures (95 with R-SG, 665 with RYGB, 141 with OLGB, and 93 DS). Loss of follow-up within 1 year 52.44%. The most common reasons for RS were weight regain and/or a worsening of preexisting comorbidities. Regarding the operating time, R-SG was the shortest of the four procedures, and DS was the longest. In general, there were no significant advantages of one procedure over another in terms of complication incidence in these categories. However, certain complications were seen more often after R-SG and DS than with other redo procedures. There were significant differences in BMI reduction 1 year after surgery (RYGB: 5.9; DS: 10.1; OLGB: 9.1; and R-SG: 9.1; p<0.001). GERD, hypertension, and sleep apnea demonstrated statistically significant comorbidity remission. Diabetes exhibited non-significant differences.
Conclusion
According to the findings of our study, all revision surgeries effectively resolved comorbidities, promoted weight loss, and lowered BMI. Due to the disparate outcomes obtained by various methods, this study cannot recommend a particular redo method as the gold standard. Selecting a procedure should consider the redo surgery’s aims, the rationale for the revision, the patient’s current state, and their medical history.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity has recently been rising across all demographics globally despite advancements in medicine. This is also associated with an increase in the severity and prevalence of obesity-related diseases [1].
Consequently, several advancements in the non-surgical and surgical management of obesity have been documented in recent decades [2].
Sleeve gastrectomy (SG) is one of the most commonly performed bariatric surgical procedures used to treat obesity. Besides the treatment’s technical simplicity, the procedure’s outstanding short- and long-term outcomes distinguish it from other bariatric and metabolic surgeries [3]. However, results are not uniform and unpredictable in which the effects are not as predicted, either in the short or long term. These conditions necessitate constant monitoring of the affected individuals and, in severe stages, may require a revision surgery (RS) strategy adjustment [4, 5].
In recent years, numerous concepts related to this topic have been researched and evaluated. Surgical intervention is often the first line of treatment, coupled with other noninvasive methods [6].
In addition to re-sleeve gastrectomy (R-SG), other bariatric surgical procedures may be considered for patients whose original sleeve gastrectomy was unsuccessful [7,8,9]. Although sufficient information is available on the benefits of various surgical procedures as revision procedure (RP) following failed primary SG, determining which surgical RP is most appropriate in this case remains contentious and requires additional scientific investigation.
This study addresses and investigates the short- and long-term outcomes of Re-SG, duodenal switch (DS), Roux-en-Y gastric bypass (RYGB), and Omega-loop gastric bypass (OLGB) as RP following unsuccessful sleeve gastrectomy.
Material and Methods
Aim of the Study
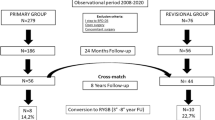
This study aims to compare different redo procedures after primary SG at 1-year follow-up, using both perioperative and 1-year follow-up data (182–547 days). Figure 1 summarizes the inclusion and exclusion criteria.
All patients with revision surgery (RS), DS, Re-SG, RYGB, and OLGB after failed SG between 2005 and 2021 were included in our analysis. Reasons for converting from SG to the above-mentioned bariatric procedures were weight regain, reflux disease, or persistence or worsening of comorbidities after primary SG.
Data Selection
Prospective data were collected from multiple centers in Germany using the German Bariatric Surgery Registry (GBSR).
From the processed data, patients are selected for analysis according to the following inclusion criteria:
-
All bariatric patients up to 04/08/2021 with the status “clean.”
-
Valid age of at least 18 years.
-
Redo procedure after primary SG.
-
Redo procedures: DS, RYGB, R-SG, or OLGB.
-
Presence of a valid 1-year follow-up.
During the outpatient presentation, preoperative data were gathered. A standardized questionnaire was used to obtain demographic data and comorbidities. During follow-up, data were collected either by presenting patients in person or by sending patients a questionnaire.
All data were collected in accordance with the principles of biomedical research outlined in the Declaration of Helsinki. Prior to prospective data collection, both patients and hospitals consented to the analysis of anonymized data in scientific studies.
Data Preparation and Definition of Variables
Individual target variables are each recorded individually as well as aggregated into one variable, for example, intraoperative complications are given if at least one intraoperative complication was selected.
Patients were assumed to have hypertension, sleep apnea (SA), or reflux if they had a documented preoperative diagnosis or were medicated for one or more of these conditions.
During follow-up, a complete remission of hypertension was observed if the patient had normal blood pressure after surgery and had stopped taking antihypertensive medications. The same was true for patients with diabetes mellitus type II (T2D), reflux, and SA.
Statistical Analysis
All analyses were performed using SAS 9.4 software. As this is an exploratory analysis, testing was deliberately performed at the full 5% significance level and any p-value ≤ 0.05 corresponds to a significant result.
Since the data came from GBSR as a multicenter registry study, it must also be considered that the cleanliness of the data cannot be assumed. In addition, only available data were analyzed. Therefore, bias due to incorrect values cannot be excluded.
If the target variable is categorical, the chi-square test was performed. For continuous target variables, an ANOVA (analysis of variance) was used. In the case of strong deviations of the distribution from the normal distribution (surgery duration, hospital length of stay, and postoperative length of stay), a transformation based on the root function is applied for the execution of the test to approximate a normal distribution.
Results
The registry included 27,939 patients with primary SG, of whom 2195 required revision surgery (7.9%). As this research focuses on the four most frequent revision procedures, data from 994 patients who underwent revisional surgery were analyzed. Loss of follow-up within 1 year was 52.44%. The most common RP performed was RYGB with 665 patients, followed by OLGB with 141, then R-SG with 95, and finally DS with 93 patients. Laparoscopy was the main method of revision. Conversion from laparoscopy to laparotomy was most commonly documented in DS (2.2%), RYGB (1.8%), R-SG, and OLGB (0%); p<0.001. Table 1 shows the distribution of RP and the type of procedure by access type.
Redo interventions were performed at various times after sleeve gastrectomy. The mean interval between PSG and redo procedures is displayed in Table 2.
Demographic and Preoperative Variables
All RPs showed substantial differences in demographic and preoperative variables. Females outnumbered males in all RPs. DS patients had the highest BMI and RYGB patients the lowest. OLGB patients were the oldest and R-SG patients the youngest. DS patients had the longest operating time and hospital stays. Table 3 presents a summary of the steady and preoperative parameters.
The distribution of comorbidities differed between the procedures and is demonstrated in Table 4.
Perioperative Adverse Events
Intraoperative complications showed no significant differences between the four RPs. However, a distinction existed between general and specific postoperative complications. Here, DS and R-SG had the greatest overall rate of complications. Regarding specific complications, the R-SG group had the greatest incidence of renal complications (2.1%; p=0.046). In contrast to RYGB and OLGB (4.3% and 4.2%, respectively; p=0.017), the prevalence of fever was highest in the group with DS and R-SG. The R-SG group had the highest documented rate (3.2%; p=0.004) of postoperative bleeding requiring transfusion. Moreover, anastomotic insufficiency and staple line leakage were most prevalent following DS and R-SG (6.5% and 6.3%, respectively; p=0.034). This also held true for sepsis, wound infections, and intraabdominal abscesses (p<0.001). In contrast, ileus occurred more frequently after DS than after RYGB (2.2% and 0.2%, respectively; p=0.008). Table 5 provides a summary of intra- and postoperative complications.
BMI and Weight Reduction
All groups experienced significant BMI and weight reductions 1 year after RS. Compared to the other groups, the DS group had the greatest average BMI reduction, followed by the R-SG group. Table 6 provides a comprehensive presentation of the evolution of weight, %EWL, and BMI.
Development of Comorbidities at 1-Year Follow-Up
One year after RS, significant differences were found for hypertension, SA, and reflux disease. Table 7 presents the results of the evolution of comorbidities following RS. There were no significant advantages in the development of T2DM between the four approaches used. However, it should be noted that more than 50% of NIDDM patients and more than 40% of IDDM patients experienced complete remission after undergoing any of the four procedures studied.
Discussion
Bariatric surgery is considered effective in achieving adequate weight loss and improvement of obesity-related comorbidities. Over the years, numerous bariatric and metabolic surgical procedures have been developed and modified. Nevertheless, certain surgical procedures are preferred due to their ability to achieve both better weight loss and adequate improvement of comorbidities.
Long-term weight loss and comorbidity improvement make sleeve gastrectomy (SG) a popular bariatric treatment. However, unfavorable outcomes may require revision or conversion surgery [10,11,12].
The most common reason for revision after SG was persistent obesity, gastroesophageal reflux disease, insufficient weight loss, and the persistence of comorbidities [4, 5, 13]. Several scientific papers have described a percentage of approximately 28% of patients with inadequate weight loss after primary SG and the need for RS or a redo operation [14, 15]. Additionally, other factors, such as strictures in the sleeve stomach or dilatation of the gastric sleeve, may contribute to the need for RS [16, 17]. In our analysis, the most common causes of RS were weight regain, the de novo or worsening of reflux disease, and the persistence or worsening of obesity-associated diseases. The percentages in this regard have not been studied in detail; rather, the work focuses on the outcome of revision procedures and the impact on the affected patient.
This analysis examined in depth a total of four revision procedures. RYGB was the most frequently performed procedure, followed by OLGB, R-SG, and DS. Although it was a revision treatment, laparoscopic surgeries were much more common than open procedures. Notably, the conversion rate from laparoscopy to laparotomy was highest after DS, followed by RYGB. Patient demographics, perioperative variables, and technical and anatomical complexity may affect these results. Depending on the revision approach, the average interval between RS and primary SG ranged from 18 to 36 months.
Our analysis and the existing literature are incapable of establishing a standard indication for the respective revision processes. Consequently, some studies characterize the possibility of using R-SG as an adequate RP if the weight loss is due to dilatation of the sleeve stomach [18]. In contrast, the literature suggests avoiding R-SG in the presence of reflux disease and opting instead for RYGB, OLGB, or DS [19,20,21,22]. This principle also pertains to the management of comorbidities, although the long-term efficacy of bariatric procedures is debatable and cannot be used to select a procedure.
Operating time can be influenced by several variables, such as patient demographics and the type of procedure. According to our analysis, patients with DS had the longest surgery time among the 4 procedures. This may be due to both the higher BMI and the technical aspects of the procedure. The available literature also supports this theory. This observation was particularly evident in patients with super obesity (BMI > 60 kg/m2) [23].
Literature indicates that an extended operating time can negatively affect perioperative outcomes [24]. DS had the longest operation duration among the four procedures analyzed. In addition to the technical complexity of the procedure and the health status of the patients, this may also explain the approximately negative intraoperative and postoperative outcomes of the procedure as well as the longer hospital stay than with other procedures. Considering this context, this factor should be considered when deciding whether or not to intervene. Nevertheless, it should not be decisive.
Our analysis revealed that DS achieved the highest BMI reduction and the highest rate of complete remission of SA among the procedures examined. However, the procedure’s complications and conversion rate were more severe, and hospital stays were the longest compared with other bariatric revision procedures. This, together with the technical complexity of the intervention, is in our opinion the reason why the intervention is much less common as a RP compared to OLGB, Re-SG, and RYGB.
According to the frequency of its use, RYGB is regarded as an attractive, sufficient, and effective RP following SG in both our analysis and other works of literature [4, 25]. In addition, the procedure resulted in fewer perioperative adverse events and sufficient comorbidity remission compared to DS. Interestingly, RYGB had the lowest reduction in BMI 1 year after surgery. Nonetheless, this outcome should not be the sole deciding factor, particularly since our analysis does not include long-term outcomes.
Re-SG ranks third among the four procedures in terms of application frequency. The analysis is unable to ascertain the low rate of secondary SG utilization. Nonetheless, we hypothesize that reflux disease was the primary reason why the operation was not employed as a revision method. However, 1 year after the procedure, Re-SG attained a significant BMI reduction and complete remission of SA in approximately 30% of patients and arterial hypertension in 22% of patients. According to the literature, R-SG is recommended for patients with dilatation of the sleeve stomach or weight loss failure [26, 27]. In the presence of reflux disease, other procedures such as RYGB should be used [28]. A study contrasted the outcomes of RYGB and DS following SG. Two years after revision surgery, the results of the two procedures were nearly identical in terms of BMI reduction and both procedures resulted in adequate remission of comorbidities [29].
In comparison to Re-SG and DS, OLGB is the preferable revision technique following SG. One year after surgery, OLGB obtained better BMI reduction than RYGB and practically similar results to DS and SG and it demonstrated better remission of reflux disease than Re-SG and DS. In one study, the outcome of RYGB was compared with OLGB as a revision procedure after SG. In terms of reflux disease, RYGB had better results than OLGB. Regarding remission of comorbidities and weight loss, the two procedures had the same results about 5 years after surgery [28]. The same results were obtained in another study that compared the two procedures (RYGB and OLGB) 2 years after surgery [21]. Given these findings, the strategy appears promising as a method for SG revision. Since the method is relatively new and long-term data are inadequately available in comparison to RYGB and SG, we infer that it has not yet been widely adopted and firmly established. The findings of future studies in this area should be anticipated, as it is currently impossible to forecast their direction.
Limitation of our study: as the data come from a registered study, we cannot presume its accuracy. The available data were the only ones analyzed. In addition, the analysis results should not be used to decide for or against intervention because they only provide short-term results. Consequently, the long-term data may differ from the medium-term outcomes, which may lead to radically different conclusions regarding specific interventions.
Conclusion
Based on our analysis, all four RP achieve sufficient results in various categories and contribute to addressing the root cause of revision following a primary SG. RYGB is one of the most prevalent revision methods, following SG. Due to the novel nature of OLGB, its use is not yet prevalent, even though the procedure provides adequate results in many categories following SG. Considering this, we anticipate the procedure to become more common over the next few years and it will be one of the most common bariatric procedures compared to RYGB and R-SG, including revision procedures. Re-SG, like the other procedures, reduces weight and comorbidities but is rarely performed after SG due to reflux disease, especially since the literature does not recommend it in the presence of these diseases. Compared to the other methods, DS had a greater effect on weight and specific comorbidities, but due to its technical complexity, it should only be performed by experienced surgeons in specialized centers, just like revision surgery in general.
Due to the short-term observation of affected individuals, it should be noted that the results of this analysis may differ from those reported in the available literature with long-term follow-up, particularly concerning the development of comorbidities. In case of ambiguity, the results from the existing literature should be considered alongside the results of our analysis to provide appropriate treatment to affected patients.
References
Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 21 Apr 2023.
Bray GA, Frühbeck G, Ryan DH, et al. Management of obesity. Lancet. 2016;387(10031):1947–56.
Howard R, Chao GF, Yang J, et al. Comparative safety of sleeve gastrectomy and gastric bypass up to 5 years after surgery in patients with severe obesity. JAMA Surg. 2021;156(12):1160–9.
Lazzati A, Bechet S, Jouma S, et al. Revision surgery after sleeve gastrectomy: a nationwide study with 10 years of follow-up. Surg Obes Relat Dis. 2020;16(10):1497–504.
Guan B, Chong TH, Peng J, et al. Mid-long-term revisional surgery after sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2019;29(6):1965–75.
Coblijn UK, Karres J, de Raaff CAL, et al. Predicting postoperative complications after bariatric surgery: the bariatric surgery index for complications, BASIC. Surg Endosc. 2017;31(11):4438–45.
Lacy A, Obarzabal A, Pando E, et al. Revisional surgery after sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2010;20(5):351–6.
Van Rutte PWJ, Smulders JF, De Zoete JP, et al. Indications and short-term outcomes of revisional surgery after failed or complicated sleeve gastrectomy. Obes Surg. 2012;22(12):1903–8.
Li S, Jiao S, Zhang S, et al. Revisional surgeries of laparoscopic sleeve gastrectomy. Diabetes Metab Syndr Obes. 2021;14:575–88.
Clapp B, Wynn M, Martyn C, et al. Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis. 2018;14(6):741–7.
Brunaldi VO, Galvao Neto M, Zundel N, et al. Isolated sleeve gastrectomy stricture: a systematic review on reporting, workup, and treatment. Surg Obes Relat Dis. 2020;16(7):955–66.
Kheirvari M, Dadkhah Nikroo N, Jaafarinejad H, et al. The advantages and disadvantages of sleeve gastrectomy; clinical laboratory to bedside review. Heliyon. 2020;6(2)
Gastric Sleeve Revision, WakeMed Health & Hospitals, Raleigh & Wake County, NC. https://www.wakemed.org/care-and-services/weight-loss/bariatric-surgery/procedures-we-offer/revisional-surgeries/gastric-sleeve-revision, Accessed 21 Apr 2023).
Arman GA, Himpens J, Dhaenens J, et al. Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(10):1778–86.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–72.
Disse E, Pasquer A, Pelascini E, et al. Dilatation of sleeve gastrectomy: myth or reality? Obes Surg. 2017;27(1):30–7.
Filip S, Hutopila I, Copaescu C. Re-sleeve gastrectomy - an efficient revisional bariatric procedure - 3 years results. Chirurgia (Bucur). 2019;114(6):809–23.
Hany M, Ibrahim M. Is re-sleeve gastrectomy after sleeve gastrectomy failure feasible? Egypt J Surg. 2018;37(1):5.
Biertho L, Thériault C, Bouvet L, et al. Second-stage duodenal switch for sleeve gastrectomy failure: a matched controlled trial. Surg Obes Relat Dis. 2018;14(10):1570–9.
Kapoulas S, Sahloul M, Singhal R. Laparoscopic conversion of sleeve gastrectomy to one anastomosis gastric bypass in a hostile abdomen. Obes Surg. 2021;31(6):2845–6.
Hany M, Zidan A, Elmongui E, et al. Revisional Roux-en-Y gastric bypass versus revisional one-anastomosis gastric bypass after failed sleeve gastrectomy: a randomized controlled trial. Obes Surg. 2022;32(11):3491–503.
Rayman S, Assaf D, Azran C, et al. Sleeve gastrectomy failure-revision to laparoscopic one-anastomosis gastric bypass or Roux-n-Y gastric bypass: a multicenter study. Obes Surg. 2021;31(7):2927–34.
Sanford JA, Kadry B, Brodsky JB, et al. Bariatric surgery operating room time--size matters. Obes Surg. 2015;25(6):1078–85.
Inaba CS, Koh CY, Sujatha-Bhaskar S, et al. Operative time as a marker of quality in bariatric surgery. Surg Obes Relat Dis. 2019;15(7):1113–20.
Marti-Fernandez R, Cassinello-Fernandez N, Cuenca-Ramirez MD, et al. Roux-en-Y gastric bypass as an effective bariatric revisional surgery after restrictive procedures. Obes Facts. 2020;13(3):367.
Noel P, Nedelcu A, Eddbali I. Five-year results after resleeve gastrectomy. Surg Obes Relat Dis. 2020;16(9):1186–91.
Noel P, Nedelcu M, Nocca D, et al. Revised sleeve gastrectomy: another option for weight loss failure after sleeve gastrectomy. Surg Endosc. 2014;28(4):1096–102. https://doi.org/10.1007/S00464-013-3277-9.
Felsenreich DM, Steinlechner K, Langer FB, et al. Outcome of sleeve gastrectomy converted to Roux-en-Y gastric bypass and one-anastomosis gastric bypass. Obes Surg. 2022;32(3):643–51.
Shimon O, Keidar A, Orgad R, et al. Long-term effectiveness of laparoscopic conversion of sleeve gastrectomy to a biliopancreatic diversion with a duodenal switch or a Roux-en-Y gastric bypass due to weight loss failure. Obes Surg. 2018;28(6):1724–30.
Acknowledgements
We would like to thank Mr. Martin Hukauf for his contributions to the statistical analysis of our data.
Author information
Authors and Affiliations
Contributions
Omar Thaher and Juan Fernando Mesa Daza: study concept, literature review, manuscript writing. Christine Stroh and Roland Croner: study concept, preparation of data for statistical analysis, revision of manuscript, final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics Approval
For this type of retrospective study, no formal consent was required. All data were gathered and analyzed in accordance with the privacy and ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. Despite the advantages of sleeve gastrectomy (SG), insufficient weight loss, complications, or the persistence of comorbidities may necessitate revision surgery (7.9% documented in GBSR).
2. Depending on the revision procedure, revision surgery after a failed sleeve gastrectomy results in varying degrees of adequate weight loss and remission of comorbidities.
3. Although certain revision surgical procedures were linked with an increased complication rate, revision surgery appears to be a safe and effective therapeutic option following failed SG.
4. Patients deciding to undergo a bariatric revision surgery should be informed of the procedure’s intermediate and long-term risks.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thaher, O., Daza, J.F.M., Croner, R.S. et al. Outcome of Revisional Bariatric Surgery After Failed Sleeve Gastrectomy: a German Multicenter Study. OBES SURG 33, 3362–3372 (2023). https://doi.org/10.1007/s11695-023-06834-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06834-6