Abstract
Background
Sleeve gastrectomy (SG) is the most common primary bariatric surgery. Long-term, up to 20% of patients may need revisional surgery. We aimed to evaluate the short-term outcomes of various revisional bariatric surgeries after a failed primary SG.
Methods
This is a single-center retrospective study of a prospectively collected database of obese patients who underwent revisional bariatric surgery during 2010–2018 for a failed previous SG. Failure was defined as inadequate weight loss (< 50% excess weight loss), ≥ 20% weight regain of the weight lost, and presence of refractory non-reflux obesity-related comorbidities ≥ 1 year after SG. Revisions included were re-sleeve, Roux en-Y gastric bypass (RYGB), biliopancreatic diversion with duodenal switch (BPD/DS), and single-anastomosis duodenal switch (SADS). The primary outcome was weight loss after revision. Secondary outcomes included postoperative complications. Due to varying follow-up rates, short-term outcomes (≥ 6 and ≤ 18 months) were assessed. Descriptive statistics are expressed as count(percentage) or median(interquartile range).
Results
Ninety-four patients met inclusion criteria. Forty-one underwent conversion to RYGB, 33 had BPD/DS, 7 had SADS, and 13 underwent re-sleeve surgery. Median interval between SG and revision was 31(27) months. At a median of 14(18) months, follow-up rate was 76% for the study cohort. Prior to revision, median BMI was 41.9(11.7) kg/m2 and 1 year after decreased by 6.3(5.1) kg/m2. BPD/DS resulted in the largest total weight loss of 21.8(10.9) kg followed by RYGB 13.2(11.3), SADS 12.2(6.1), and re-sleeve 12.0(11.9) kg; p = 0.023. Major 90-day and long-term complications occurred only after RYGB and BPD/DS and were similar (7.3% vs. 3.0%; p = 0.769 and 9.8% vs. 24.2%; p = 0.173, respectively).
Conclusions
At 1 year, revisional procedures offer further weight loss after a failed primary SG. Bypass-type revisions are preferred over re-sleeve surgery. In the absence of refractory reflux symptoms, duodenal switch-type procedures are safe and effective options especially in patients with severe obesity before SG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the past decade, sleeve gastrectomy (SG) has become the most frequently performed primary bariatric surgery in North America and worldwide [1, 2]. SG is technically easier to perform compared to bypass-type procedures and is the procedure of choice in patients with complex medical histories, e.g., renal transplant candidates or patients with chronic kidney disease or immunosuppressant therapy [3,4,5]. In addition to its safety profile, the popularity of SG is also driven by the satisfactory long-term outcomes [6, 7].
Although SG is easier to perform and is the most frequent bariatric procedure, reported reoperation rates after a primary SG due to chronic complications such as refractory reflux or weight recidivism range between 3 and 34%, with a long-term average up to 20% [8, 9]. Moreover, as we get into more than a decade past the introduction of SG as a stand-alone procedure especially long-term outcomes of pre-standardized SG [10, 11], there is a need to identify the best revisional surgical options to tailor therapy for a given patient. Historically, Roux en-Y gastric bypass (RYGB) and biliopancreatic diversion with duodenal switch (BPD/DS) have been presumed second-stage or rescue procedures after a failed sleeve. Over the past decade, emerging procedures including single-anastomosis duodenal switch (SADS) procedures have shown great promise and gained popularity as potential candidates [12, 13].
There are various revisional surgical options available after a failed primary SG. However, we need to identify the most optimal revisional procedure for a given patient driven by their individualized needs, e.g., inadequate weight loss, persistent obesity-related comorbidity, and presence of chronic complications like refractory gastroesophageal reflux disease (GERD). Moreover, the comparative data on various revisional surgical options including some newly emerging procedures such as SADS are either scarce or from small case series and in need of further studies [14,15,16]. Hence, we aimed to evaluate the short-term outcomes of various revisional bariatric surgeries (re-sleeve, RYGB, BPD/DS, SADS) after a failed primary SG.
Materials and methods
After approval from the institutional Ethics Review Board, we carried out a retrospective study of a prospectively collected database at a single academic tertiary institution. The study cohort included all patients who underwent a revisional bariatric surgery between 2010 and 2018 and after a failed prior SG. Not all prior primary SGs were performed at our institution. The revisional surgeries included re-sleeve gastrectomy and conversions to RYGB, BPD/DS, and SADS. We excluded patients who underwent a planned second-stage procedure when this was decided prior to the initial SG. We also excluded patients that required a conversion to RYGB primarily due to refractory GERD after SG. As part of the inclusion criteria we defined a failed prior SG when any of the following was present at least 1 year after SG: (1) < 50% excess weight loss (EWL); (2) ≥ 20% weight regain of the weight lost; and (3) presence of any non-GERD obesity-related comorbidity.
At our institution, the RYGB is constructed with a 50–70 cm biliopancreatic limb and a 100 cm-long anti-colic Roux limb. For BPD/DS, Roux limb and the common channel limb lengths are constructed at 150 and 100 cm, respectively. Since late 2016 and as part of a prospective study, we have also been performing SADS, which is carried out as single-anastomosis duodeno-ileal bypass (SADI) with a 250 cm common channel length as described by Sanchez-Pernaute et al. [12] In terms of mesenteric defects, we routinely close the defect at the mesentery of the small bowel anastomosis in both RYGB and BPD/DS but, the closure of the Peterson defect is not universally performed. All SGs and re-sleeve gastrectomies are performed with a 40-60Fr bougie catheter. All procedures were performed laparoscopically and without routine drainage. In addition, at our institution, the choice of surgical procedure is a joint decision derived from the patient’s preference and surgeon’s recommendation based on medical indications. Moreover, in Quebec, Canada, there is a single-payer universal healthcare system in place, which does not restrict access to any established type of bariatric surgery.
The information on patients’ demographic characteristics, Body Mass Index (BMI), and obesity-related comorbidities were obtained. Comorbidities accounted for were GERD, obstructive sleep apnea (OSA), and metabolic syndrome including diabetes mellitus type 2 (DM2), hypertension (HTN), and dyslipidemia (DLP). Operative characteristics including the American Society of Anaesthesiologists (ASA) classification, operative time, and length of stay (LOS) were also documented.
The primary outcome was weight loss after revision and described as both absolute and percent total weight loss (TWL), change in BMI, and percent EWL. Due to varying follow-up rates after each revisional procedure and the recent addition of SADS as an option at our institution (since late 2016), only short-term outcomes (≥ 6 months and ≤ 18 months) were assessed. The latest weight recorded prior to revisional bariatric surgery was used as the reference to calculate various weight loss metrics after revision. Ideal body weight was set for BMI 25 kg/m2. Composite postoperative complications were used as secondary outcomes. 90-day and long-term postoperative complications were reported as minor/major according to the established standardized reporting recommendations for bariatric surgery [17].
Descriptive statistics are presented as count (frequency) or median (interquartile range). Fisher's exact or Chi-square tests were used to compare categorical variables and Mann–Whitney U or Kruskal–Wallis tests were used for continuous variables where applicable. Data analysis was performed using R version 3.5.1 (R Foundation for Statistical Computing). Inference was based on a two-sided 5% level.
Results
During the study period, there were 1,937 primary SGs performed at our center. Among the patients included in the study cohort, 4 had their SG surgeries done at outside institutions. Over the same time period, we performed a total of 112 BPD/DS procedures from which 26% (N = 29) were done as planned second-stage procedures and not included in our study cohort. There were also 5 patients that underwent conversions to RYGB primarily due to refractory GERD symptoms after SG and were also excluded from the study cohort. The study cohort included 94 patients, who underwent revisional bariatric surgery after a failed prior SG at our institution during 2010–2018. Most patients were female (N = 77; 81.9%) and median age and BMI were 49 (17) years and 41.8 (11.7) kg/m2, respectively. OSA and HTN were the most prevalent non-GERD obesity-related comorbidities (N = 19; 20.2%), respectively. Forty-one patients (44%) underwent conversion to RYGB, 33 (35%) had BPD/DS, 7 (7%) had SADS, and the rest underwent a re-sleeve. Table 1 shows the detailed list of baseline characteristics of the study cohort stratified based on the revisional procedure.
Table 2 provides the detailed list of indications for revisional surgery. While each patient may have had more than one indication to undergo revisional surgery, primary inadequate weight loss (< 50% EWL) at 1 year was the most common reason to qualify followed by weight recidivism (≥ 20% regaining of the weight lost). Patients who underwent BPD/DS mainly suffered from inadequate weight loss followed by persistent comorbidities. However, those patients that had re-sleeve surgery rarely had residual obesity-related comorbidities.
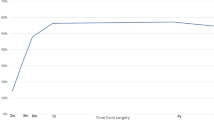
Only 71 patients had complete ≥ 6 and ≤ 18-month follow-up (76%) and were subsequently used to assess the primary outcome. The median follow-up time for this cohort was 14 (18) months. The median interval delay between primary SG and revision was 31 (24.5) months. Median BMI for the study cohort was 41.9 (11.7) kg/m2 prior to revision with the highest estimates belonging to the BPD/DS subgroup at 46.8 (12.3) kg/m2 (p = 0.013). One year after revision, median percent TWL was 12.0% (13.1); largest change in BMI was achieved after BPD/DS (8.0 [3.2], p = 0.043) and highest percent EWL was observed after SADS (55.1% [22.1], p = 0.707). Table 3 provides further details on short-term weight-related outcomes after revisional bariatric surgery along with procedure-dependent weight loss trajectories.
Changes in obesity-related comorbidities were also reviewed in detail. However, there was significant amount of missing information on the status of such comorbidities both prior to and after revisions (up to 33% and 49%, respectively). Hence, the respective data were not formally tabulated and analyzed.
Table 4 reports details on the operative characteristics and postoperative complications both early (90-days) and long-term after revisional surgery. The shortest procedure was re-sleeve and the longest was BPD/DS with median operative times of 128 (48) and 215 (49) minutes, respectively (p < 0.001). The median LOS was 2 days irrespective of the revisional procedure. In total, 7 patients experienced 90-day complications (7.4%) and all major 90-day morbidities occurred after either RYGB (N = 3) or BPD/DS (N = 1).
The details regarding patients who suffered any major 90-day morbidity were as follows: One patient required readmission on postoperative day (POD) 17 for pulmonary embolism (PE), and was started on therapeutic anticoagulation; one patient had persistent dysphagia soon after RYGB with LOS > 7 days, requiring an endoscopic dilatation on POD 14 without any adverse events prior to discharge; one patient underwent diagnostic laparoscopy on POD 4 after RYGB for symptoms suggestive of leak that confirmed a leak from the gastrojejunostomy (GJ) anastomosis that was washed out and drained with a subsequent unremarkable hospital stay; and one patient presented on POD 6 after BPD/DS and was found to have an acute small bowel obstruction due to an incarcerated incisional hernia (near umbilicus at previous extraction site of SG) and underwent a laparotomy and primary closure of the hernia without a need for bowel resection. In addition, during the 90-day period after revisions, 2 patients presented to the Emergency Department (ED) with dehydration after RYGB and received intravenous fluids and did not require any hospital readmission. Another patient presented to ED on POD 21 after RYGB and was diagnosed with a urinary tract infection and discharged on oral antibiotics (no foley was inserted at the time of revisional surgery).
There were 15 long-term complications beyond 90 days after revisional surgeries. Once again, virtually all of them occurred after either RYGB (N = 6) or BPD/DS (N = 8) and at similar rates (p = 0.453; Table 4). Long term after BPD/DS, 2 patients suffered from refractory steatorrhea and severe protein-calorie malnutrition: one patient required a laparoscopic lengthening of the common channel by at least 100 cm nearly 1.5 years after BPD/DS; another patient suffered from refractory hypoglycemic episodes in addition to severe protein-calorie malnutrition and nearly 6 years after revision underwent a complete reversal of BPD/DS laparoscopically. Previously (nearly 4 months after BPD/DS), this same patient had undergone a negative diagnostic laparoscopy for chronic abdominal pain. Moreover, 3 patients presented with internal hernia after BPD/DS requiring surgical intervention: 2 patients were found to have internal hernias through the mesenteric defect of the small bowel anastomosis and 1 patient through the Peterson defect; all three patients presented between 4 and 10 months after revision and had their internal hernias repaired laparoscopically without any bowel resection. Another 2 patients complained from chronic abdominal pain post-BPD/DS and underwent negative diagnostic laparoscopies between 4 and 6 months after revision.
Six patients experienced long-term complications after RYGB. Two patients developed GJ stricture: one required multiple endoscopic dilatations, which eventually resolved the problem; another patient underwent laparoscopic revision/redo of the GJ anastomosis. Three patients developed symptomatic internal hernias after RYGB requiring surgical interventions: 2 of them were through the Peterson defect approximately 4 months post-revision and were repaired laparoscopically without any bowel resection; also around 4 months after revision, another patient presented with acute small bowel obstruction due to an internal hernia through the jejuno-jejunostomy (JJ) mesenteric defect, which was repaired laparoscopically but needed bowel resection and redoing of the JJ anastomosis. Finally, nearly 9 months after RYGB, an active smoker was diagnosed with a marginal ulcer by gastroscopy and was successfully treated with smoking cessation, twice daily proton pump inhibitors (PPIs) and sucralfate.
In addition, while considered a minor long-term morbidity, there was one patient that underwent re-sleeve surgery despite a known diagnosis of non-dysplastic Barrett esophagus (BE) subsequent to the primary SG. This patient continues to undergo close endoscopic surveillance of the BE which so far has not progressed and has remained non-dysplastic.
Discussion
To our knowledge and albeit at short-term follow-up, this is the largest study that compares outcomes of multiple revisional bariatric surgeries after a prior failed SG, which, in addition to RYGB and classic BPD/DS, provides comparative outcomes on re-sleeve that has previously been discussed as an option [14, 18] and SADS which has recently gained significant popularity and is now endorsed by prominent international bariatric societies [15, 16, 19].
In a recent study, Amiki et al. described their institutional medium-term outcomes of revisional bariatric surgery for inadequate weight loss (< 50% EWL at 1 year; N = 15) and intractable GERD (N = 9) over a 12 year period (2006–2107) [20]. While more than half of patients in their study had a failed original SG, other primary procedures like adjustable gastric banding and vertical banded gastroplasty were also included. Looking only at those with inadequate weight loss who had revisions after a primary SG (N = 10), and despite the 12-year study period, outcomes were compared irrespective of the different mean follow-up times among procedures (33 to 48 months, re-sleeve to RYGB, respectively). Also, no follow-up rates were reported and the sample size for each revision-arm was very small (BPD/DS or duodenojejunal bypass, N = 6; RYGB, N = 2; re-sleeve, N = 2) [20]. Moreover, while they did not report the time interval between the original surgery and the revision, they demonstrated a mean TWL of nearly 30 kg and an 11-unit decrease in BMI. Revisions to BPD/DS or duodenojejunal bypass were most effective and re-sleeve surgery yielded the least weight loss [20]. In our study, at a median interval time greater than two and a half years (31 months) between SG and the revision and among individuals that had complete follow-up (≥ 6 and ≤ 18 months; N = 71) we found that revisional surgery allowed for another 12% TWL and more than a 6-unit drop in BMI. Furthermore, BPD/DS was the most effective among the revisional procedures and allowed for an additional median 14% TWL and an 8-unit drop in BMI. Although weight loss outcomes of RYGB, SADS and even re-sleeve were similar, only patients that underwent SADS achieved a median BMI < 30 kg/m2. However, this finding is in part explained by the fact that the median BMI prior to revisions was the lowest in the SADS subgroup (38 kg/m2). In addition, when comparing the change in BMI between SADS and BPD/DS subgroups as the two switch-type procedures, the latter revisional surgery yielded nearly double the change in BMI during the short-term follow-up. This difference in BMI change was also despite patients in BPD/DS subgroup having the highest pre-revision BMI (47 kg/m2). Moreover, one must not forget that these weight outcomes may be similar at 1 year but could very well diverge out at long-term follow-up after revision. Regardless, these results are important as revisional surgeries are often viewed as such that they will not allow for the same expected weight loss as a primary procedure or when there is a planned two-stage approach [21, 22].
In our study, inadequate weight loss (< 50% EWL) at 1 year was the most common reason to qualify for revisional bariatric surgery. Achieving this target in the context of severe obesity with BMI ≥ 50 kg/m2 is a major challenge and a main reason for advocating a two-step surgical approach especially in patients with super-super obesity (BMI ≥ 60 kg/m2) [23, 24]. Hence, one could argue that in the context of super-super obesity a purely restrictive procedure is destined to fail. Combined restrictive/malabsorptive or bypass-type procedures such as RYGB or classic BPD/DS are shown to result in greater weight loss and improvement in comorbidities when compared to purely restrictive procedures like SG or re-sleeve especially in patients suffering from severe obesity (BMI ≥ 50 kg/m2) [8, 25]. Moreover, among patients with severe obesity, classic BPD/DS is shown to be significantly more effective than RYGB for weight loss and resolution of comorbidities such as DM2 [26, 27]. At our institution choosing the surgical procedure is a joint decision derived from the patient’s preference and surgeon’s recommendation based on medical indications. Yet, in our study the patients who underwent SADS and BPD/DS suffered from severe obesity (BMI ≥ 50 kg/m2) prior to their SG. In fact, after grouping switch-type procedures (BPD/DS and SADS) together, the head-to-head comparison with RYGB subgroup revealed a significantly higher weight loss (median absolute TWL: 22 versus 13 kg; p = 0.007 and median BMI change: 8 versus 5 kg/m2; p = 0.015, respectively). This observation was despite our efforts to include only patients that were not originally planned for a two-step approach with median interval delays of 14 (SADS) and 20 (BPD/DS) months. In addition, the individuals with a heavier burden of their obesity syndrome in the absence of intractable GERD were more likely to undergo the more aggressive duodenal switch-type procedures.
In terms of improvements in persistent obesity-related comorbidities, as previously mentioned, due to significant missing information on the status of the comorbid conditions especially after revisions (up to 49%), we did not formally analyze the data or consider it as a secondary endpoint. However, among those with complete data on comorbid conditions pre- and post-revision, we observed improvement or resolution of obesity-related comorbidities to be as follows: for DM2 60–83%, for HTN 40–60%, for DLP 60–63%, and for OSA 40–50% (results not shown). Despite the significant missing information, these findings are consistent with the existing literature [25, 27]. In our study, the patients that received SADS as their revisional surgery and had adequate follow-up (≥ 6 and ≤ 18 months) were only a few (N = 3), who were not heavily burdened by metabolic syndrome before revision. Thus, the respective small sample size did not allow us to gage the impact of SADS on related comorbidities. However, SADS is shown to have a similar impact on obesity-related comorbidities especially cardiometabolic conditions at medium-term follow-up compared to both RYGB and BPD/DS [28, 29].
In our study cohort, we observed a 7.4% 90-day complication rate and a 4.3% rate of major morbidity after revisional surgery. All major 90-day morbidities occurred after either RYGB (N = 3/41) or BPD/DS (N = 1/33) which included one leak that was from the GJ anastomosis after RYGB; there were no mortalities. Our overall 90-day complication rate after revisional bariatric surgery is comparable to what is reported for revisional surgeries after SG (6.7–31.5%) and superior to rates referenced for revisional surgeries irrespective of original bariatric surgery including adjustable gastric banding or vertical banded gastroplasty [20, 22,23,24]. Moreover, our observed rate for 90-day major morbidity appeared to be comparable or superior to reported estimates from other large case series of revisional bariatric surgeries including two-stage BPD/DS where major morbidity ranged from 6.4–10% with a leak rate between 4.5 and 8.3% [20, 23, 24, 30]. Surprisingly, with a median follow-up of 11 months, we did not encounter any major complications among patients that had SADS. However, the sample size was small in the SADS group and only 3 out of 7 patients had follow-up ≥ 6 and ≤ 18 months, which could in part explain the observed statistics. Nevertheless, Sanchez-Pernaute et al., in their reporting of outcomes in patients that underwent SADS as a second-stage surgery and at a mean follow-up time of 21 months (N = 16), also did not observe any complications [16]. Despite the total number of subjects in our study cohort, the procedures were done at a single center and our sample size is still relatively small to make the observed complication rates generalizable. Nevertheless, better 90-day major morbidity profiles especially for more complex bypass-type procedures maybe an indirect consequence of surgeries being performed at higher-volume centers by higher-volume surgeons as was recently shown in large population-level study [31].
As for long-term complications beyond 90 days, the observed rate in our study cohort was 15.9%. Most of the long-term morbidities were categorized as major (12.8%; N = 12) and again all of those belonged to either the RYGB (N = 4/41) or BPD/DS (N = 8/33) group. Our observed internal hernia rates after either RYGB or BPD/DS were 7.3% and 9.1%, respectively. At our center, we routinely close the mesenteric defect of the small bowel anastomoses, but the closure of the Peterson defect is not universally performed. Half of observed internal hernias were through the mesenteric defect of the small bowel anastomosis despite the routine closure, which could be an advantage of SADS procedures where such mesenteric defect is not created. However, given that the other half were internal hernias through to the Peterson defect, these findings may further advocate for its routine closure. Furthermore, while the need for closure of such defect in SADS surgery is up for debate, symptomatic internal hernia through the Peterson defect has been observed even after SADS [32]. Regardless, our observed major morbidity including internal hernia rates is compatible with what was shown in a large multicenter study evaluating complications among 1,328 patients who underwent SADS procedures and compared with BPD/DS and RYGB [33]. Moreover, while the quality literature on long-term complications after revisional bariatric surgery with high follow-up rates is scarce, our results are also compatible with other reported literature [21, 34, 35].
Although the presence of non-GERD obesity-related comorbidities was used as an inclusion criterion in our study, nearly 28% (N = 26) of our cohort were taking PPIs to treat GERD symptoms prior to revision and nearly two-third of them underwent RYGB as their revisional surgery. However, 3 of these patients underwent a re-sleeve surgery one of whom was known to have developed non-dysplastic BE after the primary SG. While the patient continues to undergo close endoscopic surveillance of the BE, this observation is very important to note. This is especially true in the current era where SG is the most common bariatric procedure and de novo GERD post-SG and potential progression to dysplastic BE and adenocarcinoma is a very serious concern [36]. Perhaps re-sleeve surgery as a repeat reflux-prone procedure in someone suffering from GERD after a previous SG is not a wise choice. Although a case could be made when the primary SG is not performed properly with a large retained fundus documented on endoscopy and upper gastrointestinal series as was the case for the re-sleeve gastrectomies included in our study cohort. Nevertheless, patients requiring any form of therapy for their refractory GERD symptoms after an SG should undergo proper surveillance to rule out dysplastic BE and a subsequent conversion to RYGB as the revisional procedure of choice.
Certain limitations also need to be considered when interpreting our results. Clearly, the retrospective nature of the study from a single institution may limit the generalizability and conclusions that can be drawn. The small sample size also limits the possibility of detailed statistical analyses to interpret various independent predictors of outcome after revisional surgery and carry out stratified analyses (for instance between BPD/DS and SADS patients). As mentioned previously, while our study period spanned 9 years, the medium- to long-term follow-up rates were poor (< 50%) which led to us analyzing short-term outcomes up to 18 months after revisional surgery. When comparing the indications for the switch-type procedures (BPD/DS and SADS) with the RYGB, we found that inadequate weight loss (< 50% EWL) at 1 year was nearly twice more frequent in the former group (60% [N = 24/40] versus 34% [N = 14/41], respectively). Moreover, patients who underwent switch-type procedures suffered from severe obesity prior to their SG (median BMI for BPD/DS = 64.7 kg/m2 and for SADS = 53.3 kg/m2) compared to RYGB (median BMI = 49.5 kg/m2). This observation may indicate that the individuals who suffered from severe obesity were more likely to receive the duodenal switch-type procedures, which could be a source of selection bias. In addition, the different interval delays between primary SGs and the four surgical subgroups could also introduce selection bias. There may also be the possibility of confounding from missing data or some un-measured variables, but this should likely be distributed evenly for all 4 procedures and hence the potential bias is likely toward the null value. Furthermore, even among those with short-term follow-up, the completeness of the data on all obesity-related comorbidities was poor and did not allow for any meaningful comparative analyses among various procedures. Therefore, prospective multicenter studies that can allow for a larger sample size and longer follow-up time are needed. In addition, it would be important to know the long-term differences in absorption of vitamins, micronutrients, and other nutritional parameters including protein levels among various bypass-type procedures.
Conclusions
Revisional procedures offer further weight loss short-term after a failed primary SG. Bypass-type revisional procedures are more effective compared to re-sleeve surgery. In the absence of refractory GERD symptoms, duodenal switch-type procedures are both safe and effective revisional options especially in patients with severe obesity prior to their SG. Further long-term studies are needed to evaluate outcomes after various revisional surgeries in order to identify the optimal revisional bariatric procedures for patients with weight recidivism or refractory comorbidities after a primary SG.
References
Khorgami Z, Shoar S, Andalib A, Aminian A, Brethauer SA, Schauer PR (2017) Trends in utilization of bariatric surgery, 2010–2014: sleeve gastrectomy dominates. Surg Obes Relat Dis 13:774–778
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, Scopinaro N (2017) Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes Surg 27:2279–2289
Bouchard P, Tchervenkov J, Demyttenaere S, Court O, Andalib A (2020) Safety and efficacy of the sleeve gastrectomy as a strategy towards kidney transplantation. Surg Endosc 34:2657–2664
Andalib A, Aminian A, Khorgami Z, Navaneethan SD, Schauer PR, Brethauer SA (2016) Safety analysis of primary bariatric surgery in patients on chronic dialysis. Surg Endosc 30:2583–2591
Andalib A, Aminian A, Khorgami Z, Jamal MH, Augustin T, Schauer PR, Brethauer SA (2016) Early postoperative outcomes of primary bariatric surgery in patients on chronic steroid or immunosuppressive therapy. Obes Surg 26:1479–1486
Aminian A (2020) Bariatric procedure selection in patients with type 2 diabetes: choice between Roux-en-Y gastric bypass or sleeve gastrectomy. Surg Obes Relat Dis 16:332–339
Aminian A, Brethauer SA, Andalib A, Punchai S, Mackey J, Rodriguez J, Rogula T, Kroh M, Schauer PR (2016) Can sleeve gastrectomy "Cure" Diabetes? Long-term metabolic effects of sleeve gastrectomy in patients with type 2 diabetes. Ann Surg 264:674–681
Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev 8:CD003641
Clapp B, Wynn M, Martyn C, Foster C, O'Dell M, Tyroch A (2018) Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis 14:741–747
Lauti M, Kularatna M, Hill AG, MacCormick AD (2016) Weight regain following sleeve gastrectomy—a systematic review. Obes Surg 26:1326–1334
Regan JP, Inabnet WB, Gagner M, Pomp A (2003) Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 13:861–864
Sanchez-Pernaute A, Rubio Herrera MA, Perez-Aguirre E, Garcia Perez JC, Cabrerizo L, Diez Valladares L, Fernandez C, Talavera P, Torres A (2007) Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg 17:1614–1618
Mitzman B, Cottam D, Goriparthi R, Cottam S, Zaveri H, Surve A, Roslin MS (2016) Stomach intestinal pylorus sparing (SIPS) surgery for morbid obesity: retrospective analyses of our preliminary experience. Obes Surg 26:2098–2104
Nedelcu M, Noel P, Iannelli A, Gagner M (2015) Revised sleeve gastrectomy (re-sleeve). Surg Obes Relat Dis 11:1282–1288
Brown WA, Ooi G, Higa K, Himpens J, Torres A, SADI-S, OADS IF-atfrtlo (2018) Single anastomosis duodenal-ileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS) IFSO Position Statement. Obes Surg 28:1207–1216
Sanchez-Pernaute A, Rubio MA, Conde M, Arrue E, Perez-Aguirre E, Torres A (2015) Single-anastomosis duodenoileal bypass as a second step after sleeve gastrectomy. Surg Obes Relat Dis 11:351–355
Brethauer SA, Kim J, El Chaar M, Papasavas P, Eisenberg D, Rogers A, Ballem N, Kligman M, Kothari S, Committee ACI (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg 25:587–606
Noel P, Nedelcu M, Nocca D, Schneck AS, Gugenheim J, Iannelli A, Gagner M (2014) Revised sleeve gastrectomy: another option for weight loss failure after sleeve gastrectomy. Surg Endosc 28:1096–1102
Kallies K, Rogers A (2020) American Society for Metabolic and Bariatric Surgery updated statement on single-anastomosis duodenal switch. Surg Obes Relat Dis 16:825–830
Amiki M, Seki Y, Kasama K, Hashimoto K, Kitagawa M, Umezawa A, Kurokawa Y (2020) Revisional bariatric surgery for insufficient weight loss and gastroesophageal reflux disease: our 12-year experience. Obes Surg 30:1671–1678
Qiu J, Lundberg PW, Javier Birriel T, Claros L, Stoltzfus J, El Chaar M (2018) Revisional bariatric surgery for weight regain and refractory complications in a single MBSAQIP accredited center: what are we dealing with? Obes Surg 28:2789–2795
Abdelgawad M, De Angelis F, Iossa A, Rizzello M, Cavallaro G, Silecchia G (2016) Management of complications and outcomes after revisional bariatric surgery: 3-year experience at a bariatric Center of Excellence. Obes Surg 26:2144–2149
Dapri G, Cadiere GB, Himpens J (2011) Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg Obes Relat Dis 7:703–708
Iannelli A, Schneck AS, Dahman M, Negri C, Gugenheim J (2009) Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc 23:2385–2389
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Risstad H, Sovik TT, Engstrom M, Aasheim ET, Fagerland MW, Olsen MF, Kristinsson JA, le Roux CW, Bohmer T, Birkeland KI, Mala T, Olbers T (2015) Five-year outcomes after laparoscopic gastric bypass and laparoscopic duodenal switch in patients with body mass index of 50 to 60: a randomized clinical trial. JAMA Surg 150:352–361
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, Castagneto M, Bornstein S, Rubino F (2015) Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 386:964–973
Torres A, Rubio MA, Ramos-Levi AM, Sanchez-Pernaute A (2017) Cardiovascular risk factors after single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S): a new effective therapeutic approach? Curr Atheroscler Rep 19:58
Surve A, Zaveri H, Cottam D, Belnap L, Cottam A, Cottam S (2017) A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis 13:415–422
Landreneau JP, Strong AT, Rodriguez JH, Aleassa EM, Aminian A, Brethauer S, Schauer PR, Kroh MD (2018) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg 28:3843–3850
Bouchard P, Demyttenaere S, Court O, Franco EL, Andalib A (2020) Surgeon and hospital volume outcomes in bariatric surgery: a population-level study. Surg Obes Relat Dis 16:674–681
Surve A, Cottam D, Horsley B (2020) Internal hernia following primary laparoscopic SADI-S: the first reported case. Obes Surg 30:2066–2068
Surve A, Cottam D, Sanchez-Pernaute A, Torres A, Roller J, Kwon Y, Mourot J, Schniederjan B, Neichoy B, Enochs P, Tyner M, Bruce J, Bovard S, Roslin M, Jawad M, Teixeira A, Srikanth M, Free J, Zaveri H, Pilati D, Bull J, Belnap L, Richards C, Medlin W, Moon R, Cottam A, Sabrudin S, Cottam S, Dhorepatil A (2018) The incidence of complications associated with loop duodeno-ileostomy after single-anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. Surg Obes Relat Dis 14:594–601
Shimizu H, Annaberdyev S, Motamarry I, Kroh M, Schauer PR, Brethauer SA (2013) Revisional bariatric surgery for unsuccessful weight loss and complications. Obes Surg 23:1766–1773
Brethauer SA, Kothari S, Sudan R, Williams B, English WJ, Brengman M, Kurian M, Hutter M, Stegemann L, Kallies K, Nguyen NT, Ponce J, Morton JM (2014) Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis 10:952–972
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H (2020) Does sleeve gastrectomy expose the distal esophagus to severe reflux?: A systematic review and meta-analysis. Ann Surg 271:257–265
Acknowledgments
Drs. Zvi Perry and Ali Aboalsaud are both acknowledged for their participation in the data collection.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Amin Andalib, Hussam Alamri, Yousef Almuhanna, Philippe Bouchard, Sebastian Demyttenaere, and Olivier Court have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andalib, A., Alamri, H., Almuhanna, Y. et al. Short-term outcomes of revisional surgery after sleeve gastrectomy: a comparative analysis of re-sleeve, Roux en-Y gastric bypass, duodenal switch (Roux en-Y and single-anastomosis). Surg Endosc 35, 4644–4652 (2021). https://doi.org/10.1007/s00464-020-07891-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07891-z