Abstract
Introduction/Purpose
One anastomosis gastric bypass (OAGB) and single anastomosis duodenoileostomy with sleeve (SADI-S) are two highly effective bariatric procedures that have been recently endorsed by the American Society of Metabolic and Bariatric Surgery (ASMBS). We compared the outcomes and safety profiles of SADI-S and OAGB using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database.
Materials and Methods
Retrospective analysis on patients who underwent SADI-S or OAGB obtained from the MBSAQIP database 2020–2021. Patients who underwent concurrent procedures (besides EGD) or had missing data were removed. Variables included age, sex, body mass index, American Society of Anesthesiologists (ASA) class, and pertinent medical comorbidities. Data were analyzed for 30-day postoperative morbidity, mortality, reoperation, reintervention, and readmissions. p values were calculated using Student’s t-test or Fisher analysis.
Results
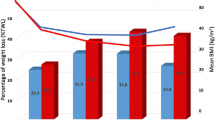
A total of 694 and 1068 patients respectively underwent SADI-S or OAGB. Statistically significant comorbidities included age (42.2 ± 10.8 vs. 43.7 ± 12.2), BMI (50.6 ± 9.1 vs. 45.3 ± 7.1), ASA 2 (66 (9.5%) vs. 165 (15.4%)), ASA 4 [69 (9.9%) vs. 20 (1.9%)], and immunosuppressive therapy [24 (3.5%) vs. 17 (1.6%)]. Clavien-Dindo-based analysis highlighted that SADI-S had higher grade 2 (p = 0.005) and grade 4b (p = 0.001) complications. Patients who underwent SADI-S were twice as likely to be readmitted within 30 days (3.7% vs. 1.9%; p = 0.021).
Conclusion
SADI-S had higher readmission rates and higher Clavien-Dindo grade 2 and 4b complications. To note, SADI-S patients had higher BMIs. Further studies are needed to determine the long-term complications and efficacy of both operations.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The American Society of Metabolic and Bariatric Surgeons (ASMBS) has recently endorsed the single anastomosis duodenoileostomy with sleeve (SADI-S) in 2021 [1] and the one anastomosis gastric bypass (OAGB) in 2022 [2]. The OAGB was originally described by Dr. Robert Rutledge in 2001 and has been adopted worldwide [3]. In some countries, it is already the most commonly performed bariatric operation, surpassing sleeve gastrectomy (SG) [4]. SADI-S was described by Dr. Antonio Torres more than 10 years ago as a safer alternative to the biliopancreatic diversion with duodenal switch (BPD-DS) and is gaining global popularity [5, 6]. However, there are several possible reasons that have led to the slow adoption of these surgeries in the USA including a delay in endorsement by the ASMBS. Additionally, the lack of Current Procedural Terminology (CPT) codes and the inability of US surgeons to get reimbursed by insurance companies might also be a contributing factor [7]. The recent endorsements of these procedures by the ASMBS may finally increase the volume of these two bariatric procedures.
The 30-day safety of OAGB compared to sleeve gastrectomy (SG) and to Roux-en-Y gastric bypass (RYGB) was described recently using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MBSAQIP) Participant Use File (PUF) for the year 2020 [8]. Our group has previously reported on the comparative safety of SADI-S to SG, RYGB, and BPD-DS using the same database [9]. There are also emerging reports of OAGB and SADI-S as revisional procedures after SG that show very good outcomes [10, 11]. To our knowledge, no comparative study of primary OAGB and SADI-S has been performed as yet in the USA. The rationale for comparing these two procedures is threefold. First, both OAGB and SADI-S have been recently endorsed by the ASMBS; thus, we sought to compare these two procedures to further encourage their adoption in the USA and guide the surgical community about the comparative risks and benefits. Additionally, both OAGB and SADI-S are hypo-absorptive procedures that offer comparable weight loss benefits. Finally, the shared loop configuration and one anastomosis nature of the procedures makes a side-by-side comparison reasonable. We used the MBSAQIP PUF to compare outcomes of the OAGB and SADI-S for the years 2020–2021. Our main goal was to compare the 30-day outcomes of the two operations. Our hypothesis was that the SADI-S and OAGB have comparable safety outcomes.
Methods
The MBSAQIP PUF for the years 2020–2021 were evaluated using patient baseline characteristics and comorbidities and 30-day outcomes, which included complications based on the Clavien-Dindo classification, readmissions, reoperations, and reinterventions.
Subjects were separated into two cohorts: one undergoing SADI-S and the other undergoing OAGB. Patients who underwent concurrent procedures (other than EGD) or had missing data were removed from this analysis. Major characteristics that were analyzed include, but are not limited to, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, diabetes mellitus, hypertension, prior deep venous thrombosis, smoking status, immunosuppressive therapy, and functional status. The American College of Surgeons MBSAQIP and the centers participating in the ACS MBSAQIP are the sources of the data used herein; they have not been verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. This project was approved by our Institutional Review Board.
Qualitative variables were summarized using frequencies and percentages while quantitative variables were summarized using mean and standard deviation (SD), using Fisher and unpaired t-tests, respectively. p values were considered significant at < 0.05. We classified complications into the Clavien-Dindo classification scheme. We have previously described how we fit reported complications from the MBSAQIP into the Clavien-Dindo classification [9] (Supplemental Table 1). Data analysis and data management were conducted using Stata v.17 and SAS v.9.4.
Results
There were 694 SADI-S and 1068 OAGB procedures recorded within the 2020 and 2021 PUF files. Table 1 highlights the preoperative characteristics of patients. Patients who underwent an OAGB were on average older (43.7 years vs. 42.2 years, p < 0.005) than their SADI-S counterparts, as well as more frequent ASA 2 classification (15.4% vs. 9.5%, p < 0.001). On the other hand, SADI-S patients had a much higher preoperative BMI (50.6 kg/m2 vs. 45.3 kg/m2, p < 0.001) and more ASA 4 (9.9% vs. 1.9%, p < 0.001) and were on immunosuppressive therapy (3.5% vs. 1.6%, p < 0.0146). Furthermore, operative times in the SADI-S cohort were significantly longer than those in the OAGB group (129.8 ± 54.0 vs. 93.3 ± 52.7 min, p < 0.001).
Clavien-Dindo grades were calculated based on recorded 30-day outcomes and are shown in Table 2. Statistically significant differences were observed with SADI-S patients having higher grade 2 (2.6% vs. 0.8%, p < 0.005) and grade 4b (2.9% vs. 0.7%, p < 0.001) complications. Further analysis identified that SADI-S patients were five times more likely to develop pneumonia (grade 2, p < 0.03) as well as at an increased risk for developing sepsis (grade 4B, p < 0.02) (Supplemental Table 1). The risk for developing grade 1, grade 3, grade 4A, and grade 5 Clavien-Dindo-based complications was equal between the two procedures. Patients who underwent SADI-S were also twice as likely to be readmitted within 30 days (3.7% vs. 1.9%; p < 0.021) compared to their OAGB counterparts (Table 3).
Discussion
The main finding of our study is that the SADI-S has higher rates of 30-day complications (pneumonia and sepsis) and a higher readmission rate than the OAGB. However, leak rates were similar. There were some notable differences in patients’ characteristics, chiefly that SADI-S patients had a higher BMI and also were twice as likely to be on immunosuppressive therapy (3.5% vs. 1.6%).
SADI-S and OAGB are both hypo-absorptive procedures. SADI-S and OAGB have been proposed and described as “simpler” but highly effective alternatives to RYGB and BPD-DS, respectively. Additionally, they both share a loop configuration instead of Roux-en-Y anatomy. We expected that these procedures would be offered to the same patient population. SADI-S has shown in a recent study to have more TWL than OAGB in a retrospective study published in 2021 (23.7% vs. 18.7% at 1-year follow-up) [10]. This may be why surgeons offered it to patients with higher BMIs in the USA. In fact, the above study was in a revisional setting after sleeve and contradicts the comparative study by Dr. Antonio Torres showing similar outcomes [5]. While SADI-S has been offered to patients with higher BMIs, both OAGB and SADI-S offered significant and comparable weight loss in patients with BMI > 50 kg/m2 in individual studies in the literature [12, 13]. Due to the MBSAQIP only reporting 30-day outcomes, long-term weight loss was not a variable that we used to better understand the aforementioned selection bias.
On the other hand, offering SADI-S in the setting of immunosuppressive therapy is reasonable since a duodenoileostomy is less prone to ulcers than a gastrojejunostomy. Cottam et al. reported 13 ulcers in 798 SADI-S cases, a very low percentage relative to gastrojejunostomy procedures [14]. As for the leak rates, there is no robust data on leak rates in SADI-S or OAGB in patients who are on immunosuppressants. Extrapolating from the data from Roux-en-Y anatomy (gastric bypass and duodenal switch), the leak rates are not significantly higher when performed by expert hands in this patient population [15]. However, in patients who are not on immunosuppressive therapy, similar leak rates between both operations were noted in larger series. Parmar et al. reported leak rates of around 0.86% in OAGB patients [16] while Surve et al. estimated that rate to be 0.6% in SADI-S patients [17].
We also found that pneumonia and sepsis were higher in the SADI-S cohort in the MBSAQIP. Despite the statistical differences in these complications, it should be stressed that these were still exceedingly rare events with pneumonia occurring for SADI-S and OAGB at 1.0% and 0.2%, respectively, and sepsis at 0.6% for SADI-S and with no occurrences for OAGB. (These low rates of complications highlight the safety of either procedure and they both have comparable complication rates to what has been reported for the RYGB [8, 9].) A potential explanation for this increased pneumonia risk in the SADI-S cohort could be the statistically significant longer operative time in that patient group (129.8 ± 54.0 vs. 93.3 ± 52.7 min, p < 0.001) [18]. Another critical finding of this paper was the higher rate of readmission for the SADI-S. The rate of readmission (3.7%) for the SADI-S was almost twice the rate for the OAGB. This may reflect the complexity of the procedure. It is important to note that increased BMI and immunosuppressive therapy might have contributed to this increased complication risk. Increased BMI has not been shown to increase complications in sleeve gastrectomy (SG), RYGB, and duodenal switch (DS); however, this study was done on a single-institutional level and did not include OAGB or SADI-S [19]. Similarly, immunosuppression can be associated with increased complications after sleeve and bypass [20, 21]. No specific studies have addressed the risk of immunosuppressive therapy on SADI-S and OAGB. This range still falls into favorable comparison with the other two main operations of SG (1.2% readmission) and RYGB (2.8% readmission) [22].
While our study reports on the early complication rates, the ultimate adoption and acceptance of these procedures require long-term follow-up with favorable outcomes. Protein-caloric malnutrition is a major concern in bariatric procedures that induces a state of malabsorption [23]. The SADI-S is a hypo-absorptive technique that is derived from the BPD-DS with the occurrence of nutritional deficiencies being uncommon when compared to procedures such as RYGB [12, 24]. OAGB is also described as a hypo-absorptive technique, with the true incidence of protein malabsorption and malnutrition yet to be fully established in the literature. Despite that, there is still enough evidence to suggest that patients respond well to nutritional supplementation [25].
Limitations
This study has potential limitations. Given that the procedures described were only recently endorsed by the American Society of Metabolic and Bariatric Surgery, the data we obtained spanned back only 2 years, with the earliest being 2021. Nevertheless, even with this limited time frame, our sample size of 1762 patients undergoing both procedures was still enough for comparison purposes. Due to the rarity of some of the complications, the small sample size available makes it difficult to assess for statistically significant differences in the occurrence of some complications between both procedures. The technical aspects of the operations (length of biliopancreatic limb or common channel) are not part of the MBSAQIP database. Nevertheless, we do not expect that this would affect the short-term outcomes of the procedure.
As these two procedures are performed more commonly in the future, the differences between these two studies may increase or decrease. This study will provide a good baseline for future analyses with larger sample sizes. There will also need to be longer-term studies conducted outside the MBSAQIP as the follow-up is only 30 days.
Conclusions
The SADI-S had a higher readmission rate and higher rates of Clavien-Dindo grade 2 and 4b complications. To note, the SADI-S patients had a higher BMI. Further study is needed to determine the long-term complication profile and efficacy of both operations.
References
Kallies K, Rogers AM. American Society for Metabolic and Bariatric Surgery updated statement on single-anastomosis duodenal switch. Surg Obes Relat Dis. 2020;16(7):825–30.
ASMBS endorsed procedures and FDA approved devices. 2019 2022 [cited 2022 November 24th]; Available from: https://asmbs.org/resources/endorsed-procedures-and-devices.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80.
Kaplan U, et al. Trends in bariatric surgery: a 5-year analysis of the Israel National Bariatric Surgery Registry. Obes Surg. 2020;30(5):1761–7.
Torres A, et al. Cardiovascular risk factors after single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S): a new effective therapeutic approach? Curr Atheroscler Rep. 2017;19(12):58.
Clapp B, et al. American Society for Metabolic and Bariatric Surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2022;18(9):1134–40.
Clapp B, et al. Reluctance in duodenal switch adoption: an international survey among bariatric surgeons. Surg Obes Relat Dis. 2021;17(10):1760–5.
Jung JJ, et al. Comparison of short-term safety of one anastomosis gastric bypass to Roux-en-Y gastric bypass and sleeve gastrectomy in the United States: 341 cases from MBSAQIP-accredited centers. Surg Obes Relat Dis. 2022;18(3):326–34.
Clapp B, et al. Single-anastomosis duodenoileal bypass with sleeve in the United States: a first comparative safety analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis. 2022;19(1):11–7.
Bashah M, et al. Single anastomosis duodeno-ileostomy (SADI-S) versus one anastomosis gastric bypass (OAGB-MGB) as revisional procedures for patients with weight recidivism after sleeve gastrectomy: a comparative analysis of efficacy and outcomes. Obes Surg. 2020;30(12):4715–23.
de la Cruz M, et al. Short- to medium-term results of single-anastomosis duodeno-ileal bypass compared with one-anastomosis gastric bypass for weight recidivism after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2020;16(8):1060–6.
Surve A, et al. Long-term outcomes of primary single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Surg Obes Relat Dis. 2020;16(11):1638–46.
Parmar CD, et al. One anastomosis gastric bypass in morbidly obese patients with BMI ≥ 50 kg/m(2): a systematic review comparing it with Roux-En-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2019;29(9):3039–46.
Cottam A, et al. An analysis of mid-term complications, weight loss, and type 2 diabetes resolution of stomach intestinal pylorus-sparing surgery (SIPS) versus Roux-En-Y gastric bypass (RYGB) with three-year follow-up. Obes Surg. 2018;28(9):2894–902.
Maroun J, et al. Impact of chronic immunosuppression on short-, mid-, and long-term bariatric surgery outcomes. Obes Surg. 2022;33(1):240–6.
Parmar CD, Mahawar KK. One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28(9):2956–67.
Surve A, et al. The incidence of complications associated with loop duodeno-ileostomy after single-anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. Surg Obes Relat Dis. 2018;14(5):594–601.
Sparn MB, et al. Risk factors and outcomes of postoperative aspiration pneumonia in abdominal surgery patients: an exact matching and weighting analysis. Surgery. 2021;170(5):1432–41.
Badaoui JN, et al. Does BMI matter? A 10-year single institutional experience on 571 bariatric surgery patients with BMI >50 kg/m2. Surg Laparosc Endosc Percutan Tech. 2022;32(4):466–71.
Hefler J, et al. Effects of chronic corticosteroid and immunosuppressant use in patients undergoing bariatric surgery. Obes Surg. 2019;29(10):3309–15.
Vahibe A, et al. Diabetes remission after bariatric surgery in patients on glucocorticoids: a pilot study. Surg Laparosc Endosc Percutan Tech. 2021;32(2):236–40.
Chaar ME, Lundberg P, Stoltzfus J. Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass: first report based on Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis. 2018;14(5):545–51.
Vahibe A, et al. Safety and efficacy of revisional surgery as a treatment for malnutrition after bariatric surgery. J Am Coll Surg. 2022;236(1):156–66.
Sánchez-Pernaute A, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up Obes Surg. 2010;20(12):1720–6.
Mahawar KK, et al. Impact of biliopancreatic limb length on severe protein-calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14(1):37–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent does not apply.
Conflict of Interest
Dr. Benjamin Clapp, Dr. Kamal Abi Mosleh, Dr. John Corbett, and Dr. Karl Hage declare no conflicts of interest. Dr. Rachel L. Moore is a consultant for Allurion and a speaker for Olympus and Medtronic. Dr. Helmuth Billy is a consultant for Lexion and a speaker for Medtronic, W. L. Gore, Lexington, Arthrex, and GT metabolic. Dr. Jaime Ponce is a consultant for W. L. Gore, Olympus, Medtronic, and Reshape Lifesciences and a speaker for W. L. Gore, Olympus, and Medtronic. Dr. Omar M. Ghanem declares no conflict of interest. These disclosures have no effect on the results of this submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• SADI-S was offered in patients with higher BMI and on immunosuppressive therapy.
• SADI-S had slightly higher complication rates compared to OAGB.
• Thirty-day readmission rates were twice as high in SADI-S compared to OAGB.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clapp, B., Mosleh, K.A., Corbett, J. et al. One Anastomosis Gastric Bypass Versus Single Anastomosis Duodenoileostomy with Sleeve: Comparative Analysis of 30-Day Outcomes Using the MBSAQIP. OBES SURG 33, 720–724 (2023). https://doi.org/10.1007/s11695-023-06452-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06452-2