Abstract
Purpose
Patients undergoing bariatric surgery are at particular high risk of postoperative nausea and vomiting (PONV). Few studies have shown the superiority of opioid-free anesthesia (OFA) over general anesthesia with opioids in bariatric surgery. The aim was to investigate the potential advantages of the OFA in bariatric surgery.
Materials and Methods
This is a retrospective study on a prospectively collected database that included bariatric patients over a 3-year period. All patients who underwent bariatric surgery at our institution were included and divided into opioid-free or standard anesthesia. The primary endpoint was the length of hospital stay. Data was collected and analyzed using a propensity score.
Results
We included 344 patients, of these 209 (60.8%) received opioid-free and 135 (39.2%) received a standard anesthesia. Mean age was 46.2 ± 11.2 years, 265 (77.0%) patients were female, and 238 (69.2%) had at least one associated medical problem. The two groups were similar in terms of age, gender, BMI, associated medical problems, and type of operations. Postoperatively, we observed no significant difference in opioid requirement, while significantly less doses of antiemetics were administered in the OFA group at postoperative day 1 (0.4 ± 0.7 vs. 0.7 ± 1.0 doses, p = 0.006) and 2 (0.1 ± 0.4 vs. 0.2 ± 0.6 doses, p = 0.022). Length of stay was significantly shorter in the OFA group (2.8 ± 0.9 vs. 3.5 ± 2.0 days, p < 0.001) both in the overall and in the propensity score–matched analyses.
Conclusion
OFA is effective for patients undergoing bariatric surgery. Perioperative outcomes are similar, while OFA patients required less antiemetics and were discharged earlier from hospital.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is the most effective treatment for obesity [1]. With hundreds of thousands of operations performed worldwide [2], many anesthesia protocols have been developed to optimize pre- and post-surgical pathways of treatment [3, 4]. Particularly, patients that are at high risk of postoperative nausea and vomiting (PONV), and despite prophylaxis, up to 50% of patients require antiemetic rescue medication (AERM) [5, 6].
The use of volatile anesthetics can attribute to the increased risk of developing PONV [7], whereas total intravenous anesthesia (TIVA) with propofol can reduce this risk. However, propofol is highly lipophilic and its clearance prolonged in bariatric patients [8, 9]. The combined use of opioids during the anesthesia is directly attributed to increase the risk of PONV [10]. To date, several studies have investigated PONV management in pediatric and adult populations for general surgery [11], while no guidelines are available for bariatric surgery [6, 12]. There are only a few studies that have shown the superiority of opioid-free anesthesia (OFA) over general anesthesia with opioids in bariatric surgery [5, 8].
The present study aims to investigate the potential advantages of the OFA in patients undergoing bariatric surgery.
Materials and Methods
Study Design and Patient Selection
This is a retrospective single-center study on a prospectively maintained dataset that included bariatric patients. Patients who were deemed eligible for bariatric surgery [13] were treated according to the standard of care [4]. Patients’ consents were obtained before the inclusion and ethic committee approved the study (2021–01,374 CE3911).
From January 2019 to November 2021, all patients who underwent bariatric surgery at our institution were retrospectively assessed for eligibility. Inclusion criteria were the following: bariatric operations and age ≥ 18 years. No exclusion criteria were applied. Patients were divided into two groups according to the type of anesthesia they underwent, either OFA or standard anesthesia with opioids. The anesthesia type was chosen according to the anesthesiologists’ personal preference and experience only, with no institutional change in anesthesia policy. No other factors (e.g., surgeon preference, insurance system issues) influenced such a decision.
The primary endpoint we considered to be the length of stay. Secondary endpoints are the requirement of opioids and antiemetics, recovery room time, and complications.
Collected data included the following: age, gender, body mass index (BMI, expressed in kg/m2), Apfel score, associated medical problems (e.g., hypertension, obstructive sleep apnea, dyslipidemia, diabetes, depression, reflux), type of surgery, intraoperative complications, operative time, recovery room time, length of hospital stay, requirement of both opioids and antiemetic medication, postoperative complications according to the Clavien-Dindo classification [14]. The Apfel score was calculated to predict the likelihood of PONV on four parameters: female gender, history of motion sickness or PONV, nonsmoking, and opioid use within 24 h after surgery [15]. Operative time was defined as the “skin to skin” time, while recovery room time was defined as the time spent after successful tracheal extubation before admission to the surgical ward. Antiemetic medications were calculated as the number of single antiemetic doses required, either metoclopramide, ondansetron, or granisetron. Opioids as required were calculated as cumulative dose of morphine milligram equivalents (morphine mg-eq) [16].
All patients were pre-assessed in a multidisciplinary manner, evaluated by bariatric surgeons, physician nutrition specialists, dieticians, anesthesiologists, and/or pulmonologists, cardiologists, and endocrinologists if required. Patients were placed in a supine position with both legs in an open position, compressive pneumatic stocking, antibiotic prophylaxis, and using laparoscopic technique. Postoperative care included basis analgesia, rescue medications, and regular respiratory physiotherapy. All patients started drinking the day of surgery and could eat on the first postoperative day. Patients were discharged from hospital once adequate mobilization, feeding, and pain control were achieved.
Opioid-Free and Standard Anesthesia with Opioids
We developed a very standard protocol using a multimodal anesthesia technique. All patients received double PONV prophylaxis with dexamethasone 0.1 mg/kg and ondansetron 8 mg (or metoclopramide 10 mg in case of known allergy or side effects to ondansetron).
OFA protocol included the following: an infusion of dexmedetomidine with a bolus of 0.5µcg/kg followed by an infusion of 0.1–1µcg/kg, a lignocaine bolus of 1.5 mg/kg with an infusion running at 1–2 mg/kg, magnesium sulfate 20% given as a bolus of 40–60 mg/kg followed by an infusion of 5 mg/kg, and a ketamine bolus of 0.25–0.5 mg/kg, followed by an infusion of 0.25 mg/kg/h. Ideal body weight was used to calculate medication doses.
Standard anesthesia protocol included the following: an infusion of propofol with a bolus of 2–3 mg/kg followed by an infusion of 6–8 mg/kg and an infusion of rocuronium with a bolus of 0.9–1.2 mg/kg followed by an infusion of 0.5 mg/kg. Finally, repeatable boluses of fentanyl 100µcg were also administered.
Statistical Analysis
Descriptive statistics were presented as absolute frequencies for categorical variables and mean with standard deviation (SD) for continuous variables. The comparison of dichotomous values was performed with the chi-square test, while continuous variables were compared with the Student t-test. A propensity score–matched (PSM) analysis [17] with 1:1 ratio was carried out according to age, sex, BMI, associated medical problems, type of surgery, associated surgical procedures, and postoperative complications. A p-value < 0.05 was considered statistically significant. MedCalc® Statistical Software version 20.014 (Ostend, Belgium; 2021) was used.
Results
Demographics and Clinical Characteristics
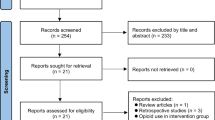
Over a 3-year period, 344 consecutive patients underwent bariatric surgery at our institution. They were assessed for eligibility and included in the present study (Fig. 1). Of these, 265 (77.0%) were female, mean age was 46.2 ± 11.2 years, and 238 (69.2%) patients had at least one associated medical problem. In our study population, 209 (60.8%) patients received OFA and 135 (39.2%) received a standard anesthesia. In Table 1, reported demographics and clinical characteristics of the two study populations resulted similar in terms of age, gender, BMI, associated medical problems, smoking status, and Apfel score.
Performed operations were as follows: 150 (43.6%) sleeve gastrectomy (SG), 137 (39.8%) Roux-en-y gastric bypass (RYGB), 5 (1.5%) single anastomosis duodenal switch (SADI-S), 33 (9.6%) cases of conversional surgery (mainly from SG to RYGB), and 29 (8.4%) cases of revisional surgery. Associated procedures were performed in 90 (26.2%). The analysis showed that the distribution of operations and associated procedures was uniform between OFA and standard anesthesia groups. Similarly, other perioperative results such as operative time, conversion to open surgery, anesthesia and time for preparation of the patient, recovery room time, and opioid administration in the recovery room were similar (details in Table 2).
Postoperative Results
Postoperatively, we observed no significant difference in opioid use the day of surgery or at postoperative days 1, 2, and 3 (details in Table 3), while significantly less doses of antiemetics were administered in the OFA group at postoperative days 1 (0.4 ± 0.7 doses vs. 0.7 ± 1.0 doses, p = 0.006) and 2 (0.1 ± 0.4 doses vs. 0.2 ± 0.6 doses, p = 0.022). The overall rate of postoperative antiemetic use was also lower in the OFA group. Subgroup analyses showed that the antiemetics were used similarly between groups in patients undergoing SG (40.0% vs. 46.2%, p = 0.481), conversional surgery (31.6% vs. 50.0%, p = 0.292), and revisional surgery (50.0% vs. 40.0%, p = 0.708), while significantly less antiemetics were used in patients undergoing RYGB (47.7% vs. 66.1%, p = 0.026).
Overall, 7 complications graded I Clavien-Dindo occurred (stomatitis, dysphagia, pancreatitis, epigastralgia, anemia, bronchospasm, and superficial wound infection). Five complications graded II Clavien-Dindo included two cases of pneumonia (in the OFA group), two self-limiting hemorrhages, and one case of pulmonary edema. Four complications graded III Clavien-Dindo included two cases of gastric leak treated endoscopically, one hemorrhage, and one bowel occlusion which were managed laparoscopically. Finally, three complications graded IV Clavien-Dindo occurred: two hemorrhagic and one septic shock which required re-operations and admission in intensive care unit.
The overall length of hospital stay was 3.1 ± 1.5 days. In the OFA group, it was significantly shorter than in the standard anesthesia group (2.8 ± 0.9 days vs. 3.5 ± 2.0 days, p < 0.001). Subgroup analyses showed that the length of hospital stay was shorter in the OFA group both in patients receiving RYGB (3.0 ± 1.0 days vs. 3.4 ± 1.6 days, p < 0.001) and SG (2.7 ± 0.9 days vs. 3.2 ± 1.8 days, p < 0.001).
Propensity Score–Matched Analysis
As reported in tables, there were no differences in patients’ characteristics and many perioperative outcomes. Anesthesia and time for surgery preparation were slightly prolonged in the OFA group (87 ± 20 min vs. 81 ± 22 min, p = 0.017) in the PSM analysis.
The two groups were also matched for postoperative complications, which could influence the use of opioids and antiemetics and the length of hospital stay. The PSM analysis did not show any significant difference in opioid use. On the contrary, the requirement for antiemetics was significantly less in the OFA group in the first (0.4 ± 0.7 doses vs. 0.6 ± 1.0 doses, p = 0.016) and the second postoperative day (0.1 ± 0.3 doses vs. 0.2 ± 0.5 doses, p = 0.030). Finally, the length of hospital stay was significantly shorter in the OFA group also in the PSM analysis (2.7 ± 0.9 days vs. 3.0 ± 0.9 days, absolute difference 0.3 days, 95% confidence interval for the mean 0.1–0.5 days, p = 0.009).
Discussion
In our study, the use of OFA reduced the length of hospital stay and antiemetics requirement in patients undergoing bariatric surgery, while no difference in the other peri- and postoperative outcomes was demonstrated.
Patients undergoing bariatric surgery are particularly at risk of PONV and the incidence can reach up to 50% of the patients [5, 6]. The best evidence suggest a multimodal pharmacological approach to PONV, including multi-agent antiemetic prophylaxis with dexamethasone in combination with lignocaine, ondansetron, droperidol, dexamethasone, metoclopramide, scopolamine, opioid-free analgesia, and TIVA [18]. However, even the recent evidence regarding OFA in bariatric surgery is concluded on small sample size studies. In our cohort, TIVA was the technique of choice in all cases either without or in combination with intraoperative opioids. We administered systematically double PONV prophylaxis. The overall incidence of PONV in our cohort was 163/344 (47.4%) patients, which is similar to other studies in the literature [5, 6, 8, 18].
Since the implementation, years ago, of the enhanced recovery after surgery (ERAS) for patients undergoing bariatric surgery at our institution [19], we observed improved postoperative courses and shorter length of hospital stay. As shown by our results, we believe a step further might be the implementation of opioid-free protocols for all type of bariatric surgery patients. The effectiveness of OFA in bariatric surgery was also demonstrated by the significantly lower incidence of antiemetic use. In fact, 42.6% of patients in the OFA and 54.8% in the standard anesthesia group required antiemetics despite good intraoperative prophylaxis. Ziemann-Gimmel et al. [8] reported an incidence of PONV of 37.3% in patients undergoing bariatric surgery and receiving inhalation anesthetics with opioids vs. 20.0% in patients receiving opioid-free TIVA. Another study of Ziemann-Gimmel et al. [5] reported that 34.8% of patients receiving hydromorphone patient-controlled analgesia required antiemetics vs. 20.2% of patients receiving intravenous acetaminophen and ketorolac. The higher rate of antiemetic use in our cohort could be justified by the fact that we did not apply systematically the intraoperative triple PONV prophylaxis [18]. As opposed to the study of Ziemann-Gimmel et al. [8], subgroup analyses showed that patients undergoing RYGB seem to require more antiemetics than patients undergoing SG and they may be the patients who profit the most from OFA.
Having said that, the intraoperative avoidance of opioid use did not affect the requirement of opioid and pain perception in the postoperative period. Interestingly, Ziemann-Gimmel et al. [8] found similar results. In addition, the rate of anesthesia-related complications was extremely low. In the OFA group, no patient suffered from severe or relevant events. Interestingly, two cases of pneumonia occurred in the OFA group, but given the mechanism of opioid-related respiratory depression, we would have expected this complication in the standard anesthesia group. This finding did not result statistically significant and may be due to chance, but further studies would be needed to address this topic.
One of the most criticized aspects of OFA at our institution was the additional time needed to prepare and manage perfusions, e.g., lignocaine. Although it was perceived by our team to have an impact, it did not actually affect operating theater schedule or any change over time. Anesthesia and patient preparation time resulted slightly shorter in the standard anesthesia group (6 min difference in the PSM analysis). Such difference is hard to be interpreted as clinically relevant, and also the time spent in recovery room was similar in OFA and standard anesthesia groups.
In our study, the overall length of hospital stay was shortened in patients receiving OFA in the overall analysis, in the PSM analysis, and in subgroup analyses performed according to the type of surgery. It seems that patients undergoing all types of bariatric surgery may profit from OFA. It seems reasonable as these patients experienced less PONV, similar complications, and pain and could be discharged earlier. Our results are consistent with other studies published in the literature in regard to the length of hospital stay [19,20,21]. The overall hospital stay was reduced by 0.7 days in the unmatched analysis and 0.3 in the PSM analysis. According to hospital cost calculation in Switzerland [22], the average potential saving is about 300 Swiss franc per patient (ca. 323 US dollars) and 32,300 US dollars/100 patients. A thorough economic analysis is needed to assess this aspect and will be the topic of our future research.
Our study has some limitations. First of all, the retrospective analysis on a prospectively maintained database of bariatric surgery which collected a large number of patients. The lack of randomization and the choice of OFA or standard anesthesia that was based on anesthesiologists’ personal preference and experience may represent a selection bias. All anesthesia cases were reviewed and also the statistical analysis did not show any reliable criteria for choosing between OFA and standard anesthesia. However, the thorough PSM analysis we performed should be considered the best option for our study design and should minimize the inherent bias. During the study period, no institutional change in anesthesia policy was decided; indeed, OFA and standard anesthesia patients were uniformly distributed over the time. Also, the surgeons did not take part in this decision process and patients did incur in the same costs. In fact, the diagnosis-related group-based reimbursement provided is exactly the same for OFA and standard anesthesia. Another limitation is the lack of blinding procedure with regard to the OFA or standard anesthesia by the caretakers (i.e., surgeon, anesthesiologists, and nurses). No scale (visual analogue scale, Likert scale) to assess severity of PONV was retrievable from the database. Heterogeneity is an important limitation that exists among group allocation, operations, associated procedures, and chosen day of discharge. However, such differences should be minimized in the PSM analysis. We decided to match also for postoperative complications, which has to be considered with utmost importance when aiming at comparing length of hospital stay and antiemetic use.
Conclusion
Our study showed that OFA is effective for patients undergoing bariatric surgery. Intra- and perioperative outcomes are similar, while OFA patients required less antiemetics and were discharged earlier from hospital.
References
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73. https://doi.org/10.1016/s0140-6736(15)00075-6.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29(3):782–95. https://doi.org/10.1007/s11695-018-3593-1.
Nishiyama T, Kohno Y, Koishi K. Anesthesia for bariatric surgery. Obes Surg. 2012;22(2):213–9. https://doi.org/10.1007/s11695-011-0406-1.
Thorell A, MacCormick AD, Awad S, et al. Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg. 2016;40(9):2065–83. https://doi.org/10.1007/s00268-016-3492-3.
Ziemann-Gimmel P, Hensel P, Koppman J, et al. Multimodal analgesia reduces narcotic requirements and antiemetic rescue medication in laparoscopic Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2013;9(6):975–80. https://doi.org/10.1016/j.soard.2013.02.003.
Sinha AC, Singh PM, Williams NW, et al. Aprepitant’s prophylactic efficacy in decreasing postoperative nausea and vomiting in morbidly obese patients undergoing bariatric surgery. Obes Surg. 2014;24(2):225–31. https://doi.org/10.1007/s11695-013-1065-1.
Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109(5):742–53. https://doi.org/10.1093/bja/aes276.
Ziemann-Gimmel P, Goldfarb AA, Koppman J, et al. Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth. 2014;112(5):906–11. https://doi.org/10.1093/bja/aet551.
Wang JJ, Ho ST, Tzeng JI, et al. The effect of timing of dexamethasone administration on its efficacy as a prophylactic antiemetic for postoperative nausea and vomiting. Anesth Analg. 2000;91(1):136–9. https://doi.org/10.1097/00000539-200007000-00025.
Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350(24):2441–51. https://doi.org/10.1056/NEJMoa032196.
Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118(1):85–113. https://doi.org/10.1213/ane.0000000000000002.
Mendes MN, Monteiro Rde S, Martins FA. Prophylaxis of postoperative nausea and vomiting in morbidly obese patients undergoing laparoscopic gastroplasties: a comparative study among three methods. Rev Bras Anestesiol. 2009;59(5):570–6. https://doi.org/10.1016/s0034-7094(09)70081-9.
Di Lorenzo N, Antoniou SA, Batterham RL, et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC. EASO and ESPCOP Surg Endosc. 2020;34(6):2332–58. https://doi.org/10.1007/s00464-020-07555-y.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Apfel CC, Läärä E, Koivuranta M, et al. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. https://doi.org/10.1097/00000542-199909000-00022.
Rennick A, Atkinson T, Cimino NM, et al. Variability in opioid equivalence calculations. Pain Med. 2016;17(5):892–8. https://doi.org/10.1111/pme.12920.
Haukoos JS, Lewis RJ. The Propensity Score. JAMA. 2015;314(15):1637–8. https://doi.org/10.1001/jama.2015.13480.
Naeem Z, Chen IL, Pryor AD, et al. Antiemetic prophylaxis and anesthetic approaches to reduce postoperative nausea and vomiting in bariatric surgery patients: a systematic review. Obes Surg. 2020;30(8):3188–200. https://doi.org/10.1007/s11695-020-04683-1.
Zhou J, Du R, Wang L, et al. The application of Enhanced Recovery After Surgery (ERAS) for patients undergoing bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2021;31(3):1321–31. https://doi.org/10.1007/s11695-020-05209-5.
Bertoni MV, Marengo M, Garofalo F, et al. Robotic-assisted versus laparoscopic revisional bariatric surgery: a systematic review and meta-analysis on perioperative outcomes. Obes Surg. 2021;31(11):5022–33. https://doi.org/10.1007/s11695-021-05668-4.
Groene P, Eisenlohr J, Zeuzem C, et al. Postoperative nausea and vomiting in bariatric surgery in comparison to non-bariatric gastric surgery. Wideochir Inne Tech Maloinwazyjne. 2019;14(1):90–5. https://doi.org/10.5114/wiitm.2018.77629.
La Regina D, Di Giuseppe M, Lucchelli M, et al. Financial impact of anastomotic leakage in colorectal surgery. J Gastrointest Surg. 2019;23(3):580–6. https://doi.org/10.1007/s11605-018-3954-z.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The local ethic committee approved the study (2021–01374 CE3911).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Few studies showed the superiority of opioid-free anesthesia in bariatric surgery.
• Perioperative complications are similar in opioid-free and standard anesthesia.
• Opioid-free anesthesia reduces the postoperative requirement of antiemetics.
• Length of hospital stay is shorter in patients receiving opioid-free anesthesia.
Rights and permissions
About this article
Cite this article
Torre, A., Marengo, M., Ledingham, N.S. et al. Opioid-Free Anesthesia in Bariatric Surgery: a Propensity Score–Matched Analysis. OBES SURG 32, 1673–1680 (2022). https://doi.org/10.1007/s11695-022-06012-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06012-0