Abstract
Background
Some studies have suggested that bariatric surgery improves pulmonary function in patients with obesity, but whether it alleviates pulmonary ventilation disorders in patients with obesity, type 2 diabetes mellitus (T2DM), and restrictive ventilatory dysfunction(RVD) is unclear. To evaluate the effect of laparoscopic sleeve gastrectomy (LSG) in improving pulmonary ventilation function in patients with obesity, T2DM, and RVD.
Methods
We studied patients with T2DM and RVD (forced vital capacity (FVC) predicted < 80%, forced expiratory volume in one second/forced vital capacity (FEV1/FVC) > 70%) who underwent LSG from March 2018 to January 2020. Baseline data was recorded and follow-up visits were made at 3, 6, 9, and 12 months after surgery to evaluate glucose, hemoglobin A1c (HbA1c), body mass index (BMI), and pulmonary ventilation function. We used multivariate analyses to assess the remission of RVD (reversion of FVC to ≥80% of the predicted value).
Results
We enrolled 33 patients (mean age 46.9±5.2 years, 21 males). Two patients were lost to follow-up and another patient died. Thirty patients completed follow-up; 24 had remission of RVD (24/33, 72.7%). Multivariate Cox regression analysis showed that lower HbA1c (HR=0.35 (0.16 ~ 0.76), p=0.008), reduced waist size (0.9 (0.83 ~ 0.98), p=0.017), and shorter duration of diabetes (0.67(0.47~0.97), p=0.033) were associated with alleviation of pulmonary ventilation function.
Conclusions
LSG not only controls the body weight and T2DM; it may also relieve pulmonary ventilation dysfunction in patients with obesity, T2DM, and RVD. The waist size, duration of diabetes, and HbA1c before LSG negatively affect recovery of pulmonary ventilation dysfunction.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a global chronic epidemic and serious public health problem. The prevalence of adult patients with obesity in the world is 12% and is gradually increasing [1]. T2DM is a common complication of obesity, characterized by glucose metabolism disorders and multisystem organ damage [2], including effects on the cardiovascular and cerebrovascular system, the peripheral nervous system, the lung, the kidney, and others. Bariatric surgery is an effective treatment procedure for obesity-related T2DM [3]. After surgery, many patients are able to eliminate or reduce the use of antidiabetic drugs and still maintain normal blood glucose [4].
Restrictive ventilatory dysfunction (RVD) is a ventilation disorder caused by limited lung volume, which reduces lung volume without a decrease in the gas flow rate. Forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) decrease, but FEV1/FVC has no significant deterioration. RVD is a common manifestation caused by a variety of factors, which can lead to a decline in lung or chest compliance [5]. T2DM is also a risk factor for RVD. A prospective study showed that after 5 years of follow-up, the risk of RVD in patients with T2DM is 1.6 times greater than that of patients without T2DM [6]. In turn, RVD independently increases the risk of prediabetes or T2DM [7]. Therefore, there may be a risk of mutual deterioration of T2DM and RVD. In addition, obesity also causes RVD [8, 9]. Based on the recent European Community Respiratory Health Survey, during the 20 years of follow-up, a weight gain of greater than 0.25 kg/year was associated with an accelerated decline of FVC and FEV1 [10].
Bariatric surgery can alleviate obesity and T2DM but whether it also alleviates pulmonary ventilation disorders in patients with obesity, T2DM, and RVD is not as yet clear from the available data. Previous studies have shown that bariatric surgery improves pulmonary function in patients with obesity [11,12,13]. However, it is unclear whether the patients included in these studies had RVD before surgery. Among the procedures of bariatric surgery, LSG has become the most commonly used surgical method because of its simplicity, low risk profile, and positive anti-diabetic and weight loss outcomes [14, 15]. A meta-analysis showed that the excess weight loss at 1 and 3 years after LSG was 72.6% and 67.1% [16]. LSG is more suitable for patients with a higher risk of complications during the perioperative period [17]. Therefore, in this study, we performed LSG on patients with obesity, T2DM, and RVD; analyzed the metabolic indices and pulmonary ventilation function before and after surgery; and evaluated alleviation of RVD and factors that might influence the alleviation of pulmonary dysfunction.
Methods
Patients
The subjects were patients with obesity who underwent LSG in the Affiliated Hospital of North Sichuan Medical College and the First Affiliated Hospital of Jinan University from March 2018 to January 2020. This study was approved by the Ethics Committee of the Affiliated Hospital of North Sichuan Medical College and the First Affiliated Hospital of Jinan University. Inclusion criteria included patients with obesity (BMI≥27.5, waist size ≥90 cm for males, waist size ≥85 cm for females) [18], T2DM, and RVD (FVC < 80% predicted, FEV1/FVC > 70%). We excluded (1) patients with spinal and thoracic deformities, a history of thoracic surgery, respiratory infection, space-occupying lesion in lung, acute T2DM complications, severe alcohol or drug dependence, mental disorders, type 1 diabetes, secondary diabetes, and gestational diabetes; (2) patients with severe cardiovascular diseases who could not withstand the stress of surgery; (3) patients with active digestive tract ulcer or tumor found during preoperative examination; (4) patients who could not undergo pulmonary function tests.
LSG Surgery
After the completion of general anesthesia and endotracheal intubation, the operating space for laparoscopic surgery was established. The surgeon separated the omentum and the posterior wall of the greater curvature of the stomach along the vascular arch on the gastric antrum and the greater curvature of the stomach. A 36F gastric tube was inserted as an indicator. Sleeve gastrectomy was performed by excising the gastric body in the greater curvature of the stomach from about 3 cm from the pylorus to the His angle. The margin of the remnant stomach was sutured and embedded via absorbable sutures. After placing the drainage tube, the operation was completed.
Pulmonary Ventilation Function Examination
The pulmonary ventilation function of each patient was evaluated using the MasterScreen PFT System (Jaeger, Germany) with the patient in a sitting position. After the nasal airflow was blocked, the patient exhaled with maximum strength and speed after a deep inhalation. Preoperative FVC, FEV1, and FEV1/FVC were measured. The test was then repeated. If the difference between the highest and second highest FVC and FEV1 values was within 5%, the result was considered reliable. A bronchial provocation test and bronchodilation test were not performed.
Evaluation Parameters
Age, sex, duration of diabetes, smoking history, preoperative FVC, FEV1/FVC, BMI, blood pressure, waist size, aspartate transaminase (AST), alanine aminotransferase (ALT), albumin (ALB), glomerular filtration rate (GFR), cystatin, uric acid (UA), hemoglobin A1c (HbA1c), C-peptide, glucose, triglyceride (TG), very low-density lipoprotein (VLDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), total cholesterol (TC), natriuretic peptide, and testosterone and result of liver ultrasound were recorded before surgery. BMI, glucose, HbA1c, and pulmonary ventilation function were evaluated at 3, 6, 9, and 12 months after surgery. When the FVC reversed to ≥ 80% of the predicted value, RVD was considered relieved, and the pulmonary ventilatory function test was not performed in subsequent follow-up visits.
Statistical Analysis
R software (version 4.1.0) was used for statistical analysis and data visualization. Continuous variables are expressed by median (interquartile range) or mean ± standard deviation; categorical variables are expressed as frequency (percentage). Univariate Cox regression analysis was used to evaluate the influence of preoperative indicators on the remission of pulmonary ventilation function within 1 year after surgery. The variables with p<0.1 in the univariate analysis were included in the multivariate Cox regression analysis to assess the independent effects of these indicators on the remission of pulmonary function within 1 year after surgery. Pearson correlation analysis was performed to assess whether changes in BMI and HbA1c correlated with the change of FVC% predicted at 3, 6, 9, and 12 months after operation. p <0.05 was considered statistically significant.
Results
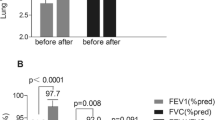
The 33 patients enrolled in this study included 21 males and 12 females. The average age was 46.9±5.2 years. Seventy percent of patients had hypertension before surgery; 87.9% of patients had fatty liver based on ultrasound imaging. On the day of surgery, a calf length pneumatic compression device was used for thromboprophylaxis until the patient started ambulating. Most (90.9%) ambulated on the first postoperative day and the remainder on the second postoperative day. The number of hospitalization days was 4 for most patients (87.9%), and 5 (6.1%), and 6 (6.1%) for others. Two patients were lost to follow-up at the 9th and 12th months. Another patient died unexpectedly due to a drowning accident unrelated to hospital care in the 12th month after surgery. At 3, 6, 9, and 12 months after surgery, 6, 14, 19, and 24 patients had remission of RVD, respectively. As shown in Fig. 1, LSG significantly reduced HbA1c, BMI, and glucose at 3, 6, 9, and 12 months. Table 1 shows the baseline characteristics of the 33 patients.
Univariate Cox regression analysis was performed with preoperative indicators as independent variables and alleviation status of RVD as the dependent variable (Table 2). The p values for HbA1c, BMI, waist size, duration of diabetes, natriuretic peptide, FVC% predicted, and FEV1/FVC were all less than 0.1. These indices were then included in the multivariate Cox regression (Table 3, Fig. 2), which showed that elevated HbA1c, increased waist size, and increased duration of diabetes were independent risk factors for remission of pulmonary ventilation function. That is, a larger preoperative waist size, a longer duration of diabetes, and poorer control of diabetes were not conducive to remission of pulmonary ventilation function after surgery.
The changes in HbA1c and BMI (Δ HbA1c, Δ BMI), by FVC% predicted from baseline values at 3, 6, 9, and 12 months after surgery, are represented by the change in FVC% predicted (ΔFVC% predicted). The ΔHbA1c at the 6th and 9th months after surgery was negatively correlated with ΔFVC% predicted (R=0.48, p=0.011; R=0.051, p=0.037). Although there was a negative correlation between ΔBMI and ΔFVC% predicted at the 6th, 9th, and 12th month after surgery, the change was not statistically significant (Fig. 3).
Discussion
Patients with obesity, T2DM, and RVD may have an increased incidence of perioperative complications with some forms of bariatric surgery [19]. Because minimally invasive surgery with LSG has a lower surgical risk, we performed LSG on these patients in order to control body weight and T2DM and avoid the more serious complications of obesity. Our study found that LSG reduced BMI, blood glucose, and HbA1c in patients within 1 year after surgery, and at the same time, it significantly alleviated RVD in 72.7% of patients. In addition, a greater preoperative waist size, a longer duration of diabetes, and poorer control of diabetes were associated with nonalleviation of RVD within 1 year after surgery. Previous studies have shown that restrictive ventilatory dysfunction increases the risk of cardiovascular disease and lung squamous cell carcinoma [20, 21], and is also associated with pulmonary hypertension [22]. Therefore, reversing the effects of RVD by bariatric surgery may help reduce these risks.
In addition to deteriorating kidney and retinal function, T2DM causes excess fat to accumulate in the lungs [23]. Hyperglycemia leads to the formation of advanced glycation end products, which will aggravate the damage to the microvascular system [24]. Therefore, the alveolar capillary reserve of patients with T2DM is reduced, and the degree of reduction is related to the control of blood glucose and damage to the systemic vasculature; the reduction in capillary reserve is also aggravated by obesity [25].
In a rat study, the secretion of surfactant by type II alveolar epithelial cells decreased after T2DM was induced by streptozotocin [26], which increased the resistance of the inspiratory phase. The morphological and functional changes induced by hyperglycemia worsen pulmonary compliance and cause RVD. However, the change can be reversed by insulin. For example, insulin is beneficial in alleviating the thickening of the vascular basement membrane in obese and diabetic rats [27, 28]. After in vivo insulin treatment, the abnormal secretion of type 2 alveolar epithelial cells also returned to a physiological state [26].
A large number of studies have shown that bariatric surgery controls T2DM significantly [29]. Our study also found that glucose and HbA1c decreased significantly after LSG. These effects are beneficial in improving RVD. Our study found that a longer course and poorer control of T2DM are associated with a greater risk of not alleviating RVD after surgery. This may be due to a long-term and fluctuating hyperglycemic state, which can cause irreversible lung damage, such as interstitial fibrosis. However, further research is needed to confirm this long-term effect of fluctuating hyperglycemia. In addition, correlation analysis showed that a large decrease in HbA1c was accompanied by a large increase in FVC% predicted at 6 and 9 months after surgery. Therefore, control of T2DM after bariatric surgery may play an important role in the remission of RVD.
Our study also found that the greater the waist size before surgery, the greater the risk of not alleviating RVD after surgery. This may be because this study involved a Chinese population, which is characterized by abdominal obesity with excessive visceral fat accumulation [30]. Excessive intra-abdominal fat is not conducive to the contraction of the diaphragm, which leads to a decrease in thoracic compliance in patients with obesity, which then leads to RVD. Although LSG reduces intra-abdominal fat content significantly [31], the time required to return to a stable state in patients with a larger preoperative waist circumference is probably longer than that in patients with smaller waistlines. Therefore, in our study, preoperative waist size was a risk factor for delaying non-remission of RVD within 1 year after operation. Further follow-up will be conducted in future studies to assess the effect of preoperative waist size on remission of RVD.
Our study has the following limitations: (1) our sample size was small and may not have detected other unknown confounding factors; (2) our study involved Chinese people with abdominal obesity, and therefore the results may not be applicable to Europeans and others; (3) we only evaluated RVD remission 1 year after surgery. Longer term follow-up is still necessary to confirm conclusions and fully evaluate risk factors. Therefore, in future studies, we will increase our sample size, increase the follow-up time, and expand the population to peoples other than Han Chinese.
In summary, LSG not only controls obesity and T2DM; it may also relieve RVD. Decreased postoperative HbA1c, waist size, and duration of diabetes were associated with alleviation of preoperative RVD. Our research should be confirmed in a larger sample including subjects other than Han Chinese in a prospective clinical study. The results will have far-reaching value in expanding the clinical application of metabolic surgery.
References
Matta J, Carette C, Rives LC, et al. French and worldwide epidemiology of obesity. Presse Med. 2018;47(5):434–8.
Anagnostis P, Paparodis RD, Bosdou JK, et al. Risk of type 2 diabetes mellitus in polycystic ovary syndrome is associated with obesity: a meta-analysis of observational studies. Endocrine. 2021;74(2):245–53.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess (Winchester, England). 2009;13(41):215–357.
Frachetti KJ, Goldfine AB. Bariatric surgery for diabetes management. Curr Opin Endocrinol Diabetes Obes. 2009;16(2):119–24.
Kim HK, Kim CH, Jung YJ, et al. Association of restrictive ventilatory dysfunction with insulin resistance and type 2 diabetes in Koreans. Exp Clin Endocrinol Diabetes. 2011;119(1):47–52.
Sonoda N, Morimoto A, Tatsumi Y, et al. A prospective study of the impact of diabetes mellitus on restrictive and obstructive lung function impairment: the Saku study. Metabolism. 2017;82:58–64.
Kim CH, Kim HK, Kim EH, et al. Association of restrictive ventilatory dysfunction with the development of prediabetes and type 2 diabetes in Koreans. Acta Diabetol. 2015;52(2):357–63.
Leone N, Courbon D, Thomas F, et al. Lung function impairment and metabolic syndrome: the critical role of abdominal obesity. Am J Respir Crit Care Med. 2009;179(6):509–16.
Kwack WG, Kang YS, Jeong YJ, et al. Association between thoracic fat measured using computed tomography and lung function in a population without respiratory diseases. J Thoracic Dis. 2019;11(12):5300–9.
Peralta GP, Marcon A, Carsin AE, et al. Body mass index and weight change are associated with adult lung function trajectories: the prospective ECRHS study. Thorax. 2020;75(4):313–20.
Campos EC, Peixoto-Souza FS, Alves VC, et al. Improvement in lung function and functional capacity in morbidly obese women subjected to bariatric surgery. Clinics. 2018;73:1–8.
Zavorsky GS, Kim DJ, Sylvestre JL, et al. Alveolar-membrane diffusing capacity improves in the morbidly obese after bariatric surgery. Obes Surg. 2008;18(3):256.
Tu Y, Yu H, Bao Y, et al. Baseline of visceral fat area and decreased body weight correlate with improved pulmonary function after Roux-en-Y Gastric Bypass in Chinese obese patients with BMI 28–35 kg/m2 and Type 2 diabetes: a 6-month follow-up. BMC Endocr Disord. 2015;15:1 (2015-06-09), 2015, 15(1):1-8).
English WJ, Demaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis. 2018;14(3):259.
Javanainen M, Penttilä A, Mustonen H, et al. A Retrospective 2-year follow-up of late complications treated surgically and endoscopically after laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG) for morbid obesity. Obes Surg. 2018;28(4):1055–62.
Jaruvongvanich V, Wongjarupong N, Vantanasiri K, et al. Midterm outcome of laparoscopic sleeve gastrectomy in Asians: a systematic review and meta-analysis. Obes Surg. 2020;30(4):1459–67.
Nasser H, Ivanics T, Carlin AM. Factors influencing the choice between laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Endosc. 2020;35(8):4691–9.
Wang Y, Wang Cu, Zhu S, et al. Guidelines for surgical treatment of obesity and type 2 diabetes in China (2019 Edition). Chin J Pract Surg. 2019;39(04):301–306.
Huisstede AV, Biter LU, Ronald L. Pulmonary function testing and complications of laparoscopic bariatric surgery. Obes Surg. 2013;23(10):1596–603.
Johnston AK, Mannino DM, Hagan GW, et al. Relationship between lung function impairment and incidence or recurrence of cardiovascular events in a middle-aged cohort. Thorax. 2008;63(7):599–605.
Purdue MP, Gold L, Järvholm B, et al. Impaired lung function and lung cancer incidence in a cohort of Swedish construction workers. Thorax. 2007;62(1):51–6.
Choudhary G, Jankowich M, Wu WC. Prevalence and clinical characteristics associated with pulmonary hypertension in African-Americans. PLoS ONE. 2013;8(12):e84264.
Yilmaz C, Ravikumar P, Bellotto DJ, et al. Fatty diabetic lung: functional impairment in a model of metabolic syndrome. J Appl Physiol. 2010;109(6):1913–9.
Hsia C, Raskin P. The diabetic lung: relevance of alveolar microangiopathy for the use of inhaled insulin. Am J Med. 2005;118(3):205–11.
Chance WW, Rhee C, Yilmaz C, et al. Diminished alveolar microvascular reserves in type 2 diabetes reflect systemic microangiopathy. Diabetes Care. 2008;31(8):1596–601.
Lou A, Longmore WJ. Altered phospholipid secretion in type II pneumocytes isolated from streptozotocin-diabetic rats. Biochim Biophys Acta. 1986;878(2):258–65.
Ruze R, Li J, Xu Q, et al. Sleeve gastrectomy ameliorates alveolar structures and surfactant protein expression in lungs of obese and diabetic rats. Int J Obes (Lond). 2020;44(12):2394–404.
Chakrabarti S, Sima A. Effect of aldose reductase inhibition and insulin treatment on retinal capillary basement membrane thickening in BB rats. Diabetes. 1989;38(9):1181–6.
Alison, H, Affinati, Oral EA, Kraftson AT. Bariatric surgery in the treatment of type 2 diabetes. Curr Diabetes Rep. 2019;19(12):1–10.
Du P, Wang HJ, Zhang B, et al. Prevalence of abdominal obesity among Chinese adults in 2011. J Epidemiol. 2017;27(6):282–6.
Mizrahi I, Beglaibter N, Simanovsky N, et al. Ultrasound evaluation of visceral and subcutaneous fat reduction in morbidly obese subjects undergoing laparoscopic gastric banding, sleeve gastrectomy, and Roux-en-Y gastric bypass: a prospective comparison study. Obes Surg. 2015;25(6):959–66.
Acknowledgements
We thank John T. Cathey for English language assistance (Peerwith, John Cathey, https://goo.gl/MSJTA7).
Funding
This study was supported by the National Natural Science Foundation of China (82070535), and the Nanchong Government and North Sichuan Medical College Cooperation Project (20SXQT0312).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Bariatric surgery has improved pulmonary ventilation in patients with obesity.
• Whether it alleviates pulmonary ventilation in patients with obesity, T2DM, and RVD is unknown.
• In this study, RVD was alleviated in 80% (24/30) of patients with obesity, T2DM, and RVD.
• Increased HbA1c, increased waist size, and longer duration of diabetes may prevent remission.
Xiaodong Lv, Jingge Yang, and Yin Xian contributed equally to this work and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Lv, X., Yang, J., Xian, Y. et al. Multiple Beneficial Effects of Laparoscopic Sleeve Gastrectomy for Patients with Obesity, Type 2 Diabetes Mellitus, and Restrictive Ventilatory Dysfunction. OBES SURG 32, 1016–1023 (2022). https://doi.org/10.1007/s11695-022-05898-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-05898-0